Abstract
Objective: To assess the use of self medication in oral health problems in Cameroon. Methods: This multi-regional cross-sectional survey was conducted in three towns; Bamenda, Yaounde and Buea over a 10 month period. The questionnaire elicited information on demography, oral problem for self medication, substance used for self medication, source of the substance, duration of self medication, reason for self medication, source of advice of the drugs or those products used, opinion about the substance, effect and duration. Results: The prevalence of self medication for oral health problems was 67.8% which was significantly associated with age, marital status and location. The most frequently self medicated oral health problem was toothache (54.7%). The majority (64.5%) of the respondents used pharmaceutical products while a minority (7.7%) used dangerous substances such as petrol and vinegar for self medication. Sources of substances of self medication included pharmacy (55.6%), road side vendors (26.1%), native healers (7.8%), mobile drug vendors in buses (5.3%), and others (5.3%). The choice of substances used for self medication was mostly guided by the advice from relatives. Conclusion: The majority of the respondents self-medicated for oral health problems. Unmarried, urban residents, aged 21–30 years reported significantly increased self-medication for oral health problems. Evidently dangerous substances were utilised for self-medication in this study, necessitating awareness and other forms of intervention.
Key words: Access, behavioural science, oral health, pain, outcomes
INTRODUCTION
Health seeking behaviour is a typical response in the presence of a disease condition or an infective process. This response, geared towards optimal wellness, recovery, and rehabilitation, is usually a function of individual, societal and environmental factors1., 2., 3.. In developing countries, self medication is the commonest chosen pathway. The underlying reasons are inadequate health care, poverty, illiteracy, drug abuse, poor access to health services due fewer trained physicians and easy availability of traditional herbal medicines4. Cost has been cited as a major reason why many low income households opt for the self-care option5.
Previous studies have cited oral health problems as one of the commonest reasons for self medication with antibiotics6., 7.. Recent evidence from developing countries indicates an inverse trend: an increasing prevalence of oral health problems, yet low visits to dental healthcare facilities; a trend which seems to suggest that many individuals from these regions resort to obtaining and consuming medications for oral health problems without a prescription from a dentist. Granted that self medication is considered acceptable in some health condition8., 9., there could be some associated negative effects. These may include poor self diagnosis and use of contraindicated medications, drug resistance, adverse drug reactions, taking expired drugs, taking of wrong doses, and drug dependence or addiction10., 11., 12., 13. especially when using opioids and tranquilisers. The economic, health, social and other impacts of self medication qualify it as a public health problem. Available literature shows the link between self medication and socioeconomic status. For example, self-care strategies for toothache usually take precedence over professional health services among low income adults in Maryland14 and individuals seeking care in a rural dental clinic in north Florida15 Kouame et al.16 reported self medication to be one of the most frequent causes of late odontostomatologic consultations. The unrestricted access to all forms of medications due to poor legislation, bizarre and unenforced official policies on self medication in many African countries favours widespread self-medication with orthodox and traditional medication. Although self medication is common place in Sub-Saharan African, there appears to be a paucity of data quantifying rates or prevalence of self medication for oral health problems. The only previous studies available were hospital based research17., 18.. However, it is common knowledge that the majority of residents in developing countries have poor access to healthcare facilities. This scenario justifies the need for a community based survey to ascertain the actual magnitude of this form of health seeking behaviour. The objective of the study was to assess the use of self medication in oral health problems in Cameroon.
MATERIALS AND METHODS
This multi-regional cross-sectional survey was conducted in three towns; Bamenda, Yaounde and Buea which represent three out 10 regions in Cameroon. Bamenda represents the North West region,Yaounde represents the Central regions while Buea represents the South West regions. The study was conducted over a 10 month period (October 2009–August 2010). The calculated sample size for was 73 for each of the three regions based on the fact that the mouth and teeth accounted for 5% of self medication19, 95% confidence interval and 5% error margin. Participants were both customers and traders in the respective markets which were selected randomly from the different parts of the market. Informed consent was obtained from the participants before administration of the questionnaire. Individuals, who have not experienced oral health problems and those who understood neither French nor English were excluded. The tool of data collection was a pretested, 17-item semi-structured questionnaire. The questionnaires were self-administered to literate respondents and interviewer administered to the illiterate respondents. The questionnaire elicited information on demography, oral problem for self medication, substance used for self medication, source of the substance, duration of self medication, reason for self medication, source of advice of the drugs or those products used, opinion about the substance, effect and duration. Ethical approval was obtained from the respective regional delegates of public health in the three provinces. Data analysis was done using Epi-info 3.5.1 and data were presented in tabular and graphic form. Test of significance was done using chi square statistics with P < 0.05 considered as significant.
RESULTS
A total of 283 individuals participated in the survey with 94 (33.2%) from North West region, 95 (33.6%) from Central regions and 94 (33.2%) from South West regions. The majority of the respondents were 21–30-years-old (37.8%), females (51.9%), single (67.1%) urban residents (56.5%) and belonged to a low income group (78.8%). The prevalence of self medication was 67.8%.
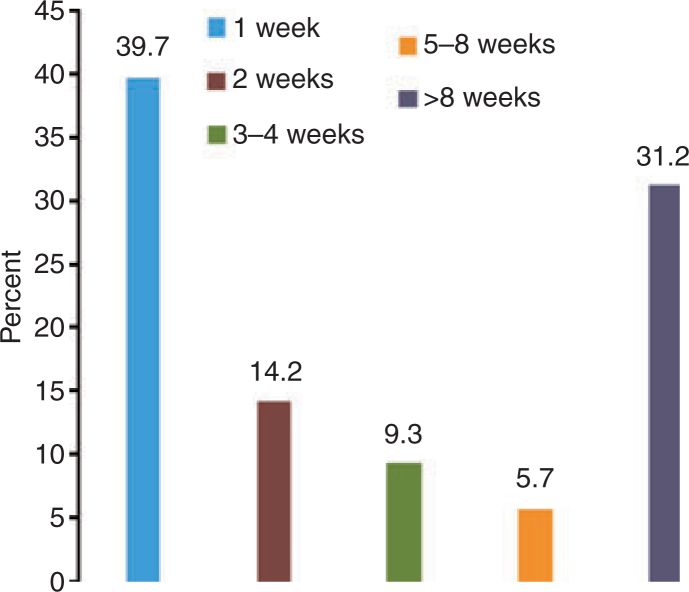
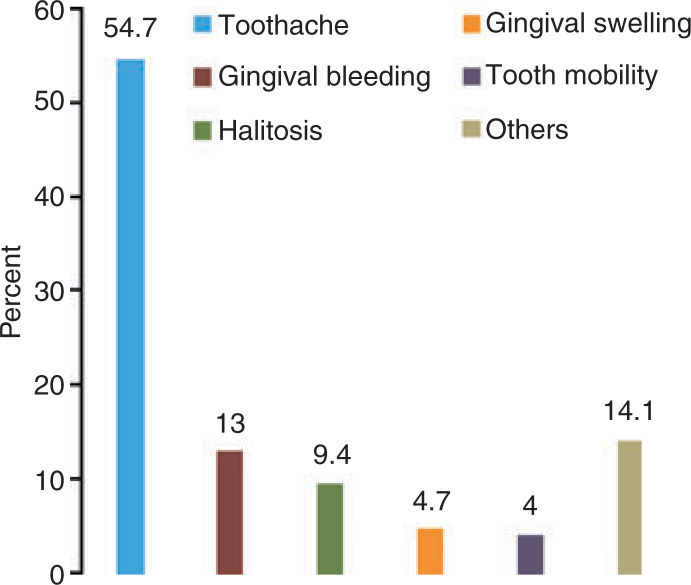
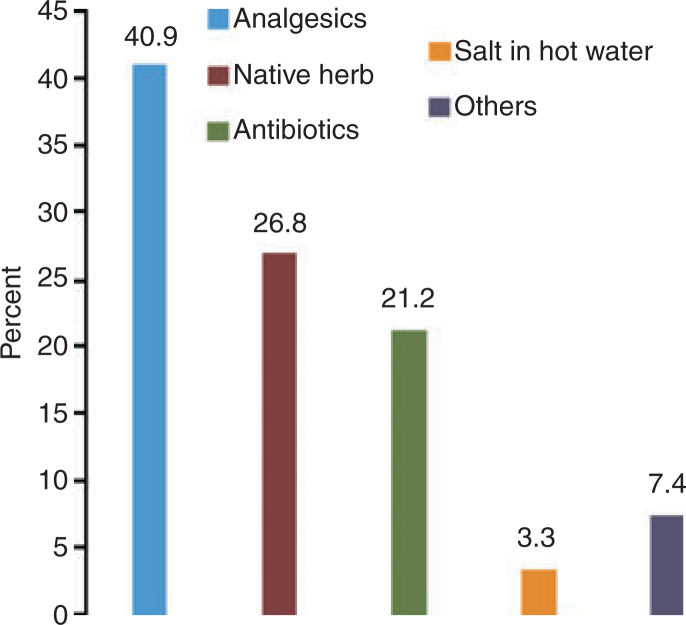
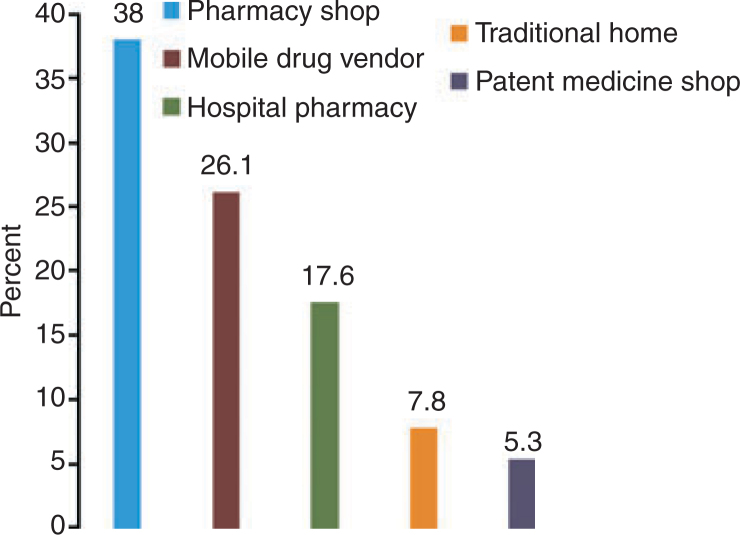
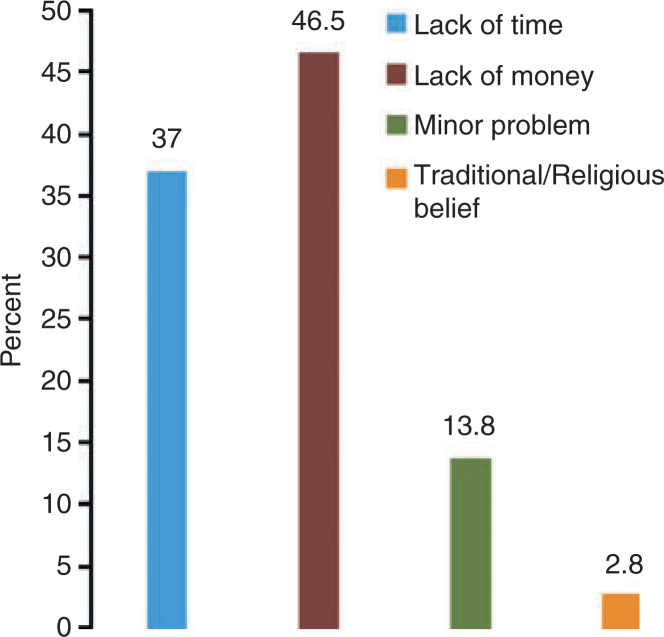
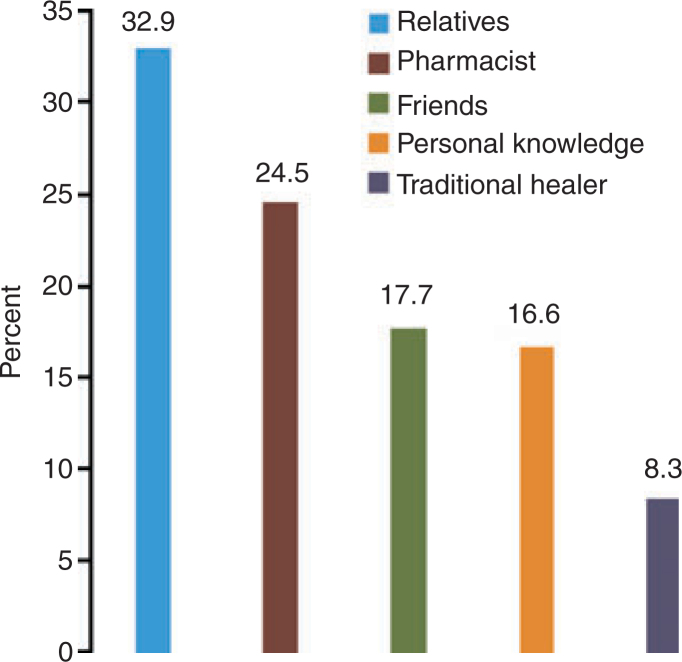
Age, marital status, highest educational level, income status were significantly associated with self medication for oral health problems (Table 1). The majority of respondents (86.4%) felt better after using the medications; out of which, 39.7% and 31.2% experienced the beneficial effect in 1 week and after 4 months respectively (Figure 1). Self medicated oral health problems were toothache (54.7%), bleeding gums (13%), bad breath (9.4%), gum swelling, cheek problems (4.7%), tooth mobility (4%) and other dental treatment 14% (Figure 2); out of which 64.5% used pharmaceutical products, 27.8% herbal products and 7.7% other products such as petrol etc. (Figure 3). Sources of the self-medication were a pharmacy (38.0%), hospital pharmacy (17.6%), native healers (7.8%), mobile drug vendors in buses (5.3%), road side vendors (26.1%) and others (5.3%) (Figure 4). The reasons for indulgence in self medication were lack of time (37%), lack of money (46.5%) perception of problem as minor (13.8%) and tradition and religious belief (2.8%) (Figure 5). The choice of self-medicament was guided by advice from relatives in 32.9% of the respondents (Figure 6). About four-tenths (43.2%) of the respondents believed the medications gave temporary pain relief, while under a quarter (20.7%) believed that they are effective, 16.2% useful in stressful situations, 9.9% didn’t know about their effects and 4.1% believed that it cures illnesses (Table 2).
Table 1.
Relationship between demography characteristics and self medication for oral health problems
| Characteristics | Yes | No | Total | P-value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age (years) | ||||
| <20 | 59 (67.8) | 28 (32.2) | 87 (100) | 0.001* |
| 21–30 | 82 (76.6) | 25 (23.4) | 107 (100) | |
| 31–40 | 25 (73.5) | 9 (26.5) | 34 (100) | |
| 41–50 | 13 (61.9) | 8 (38.1) | 21 (100) | |
| >50 | 13 (38.2) | 21 (61.8) | 34 (100) | |
| Sex | ||||
| Female | 99 (67.3) | 48 (32.7) | 147 (100) | 0.852 |
| Male | 93 (68.4) | 43 (31.6) | 136 (100) | |
| Marital status | ||||
| Single | 139 (73.2) | 51 (26.8) | 190 (100) | 0.021* |
| Married | 48 (57.8) | 35 (42.2) | 83 (100) | |
| Divorced | 5 (50.0) | 5 (50.0) | 10 (100) | |
| Income class | ||||
| Low income | 145 (65.0) | 78 (35.0) | 223 (100) | 0.144 |
| Middle income | 27 (79.4) | 7 (20.6) | 34 (100) | |
| High income | 20 (76.9) | 6 (23.1) | 26 (100) | |
| Residence | ||||
| Rural | 70 (56.9) | 53 (43.1) | 123 (100) | 0.001* |
| Urban | 122 (76.3) | 38 (23.7) | 160 (100) | |
Statistically significant.
Figure 1.
Duration at experiencing symptom alleviation among the respondents.
Figure 2.
Oral health problem that triggered self medication among respondents.
Figure 3.
Type of substance used for self medication among the respondents. Other include vinegar, petrol, urine, alum, snuff, ice pack, ‘Touch and Go’.
Figure 4.
Source of substance used for self medication among the respondents.
Figure 5.
Reason for self medication among the respondents.
Figure 6.
Source of advice on substance used for self medication among the respondents.
Table 2.
Respondents’ attitude about self medication practices
| Opinion | Frequency (n) | Percent |
|---|---|---|
| Temporary pain relief | 96 | 43.2 |
| Effective | 46 | 20.7 |
| Useful in stressful situations | 36 | 16.2 |
| Don’t know about their effects | 22 | 9.9 |
| Curative in nature | 9 | 4.1 |
| Natural products | 5 | 2.3 |
| Previous properly prescribed | 2 | 0.9 |
| They are cheaper option | 1 | 0.5 |
DISCUSSION
The prevalence of self medication for oral health problem in this study was 67.8%. This was higher than 37.3% and 42.0% previously reported in hospital based research in the Ivory Coast and Nigeria respectively17., 18., and 48% documented in Burkina Faso20. The higher prevalence implies that community based surveys are more valid than hospital based research in quantifying the actual magnitude of oral health behaviour. This is because not all oral health problems are eventually brought to the dentist’s attention as an earlier study revealed that as much as one quarter of the population gives up care despite experiencing pain or embarrassment due to oral health problem20., 21.. Age was significantly associated with self medication for oral health problems. The prevalence increased with increasing age climaxing at 21–30 years and decreased thereafter with the lowest level among the elderly. A similar assertion has been made by Yousef et al.22 in Jordan. Residence in an urban area was significantly associated with self medication for oral health problems in this study. The higher frequency of self medication among urban residents documented in previous study may be the explanation23.
Toothache affects diet, diet choices, disturbs sleep and impairs overall health motivating individuals to seek urgent help. Available literature shows that the main reasons for self medication is pain17., 18.. However, the use of self-medication by an individual in the clinical state of acute orofacial pain associated with lack of, or inadequate, care to relieve the symptoms24. Pain is distress in nature, thereby posing as a driving force for self medication in individuals to alleviate symptoms or avoid the need for dental attendance25. Gingival bleeding, gingival swelling and tooth mobility which are manifestations of periodontal disease result in chronic discomfort leading to self medication. Halitosis is a disturbing oral symptom that hampers personal and social relations thus necessitating attention seeking by individual sufferers in the form of self medication and others.
The majority of respondents (86.4%) felt better after using the medications. About one-third (31.2%) experienced the perceived beneficial effect after 4 months. The long duration before experiencing the perceived beneficial effect attest to chronicity of self medication which may be associated with adverse consequences like addiction, reversible and irreversible deformities, antibiotics resistance, bleeding tendencies, peptic ulcer and analgesics nephropathy.
Earlier studies indicated that reported poverty and lack of information are barriers to buccodental consultation services26. In this study, lack of money and lack of time were the most frequent reasons for using self medication for health problems. Other reasons included traditional belief, religious belief and perception of the problem as minor. The lack of financial means has been cited as the first obstacle in the accessibility of oral care20., 21. and one of the main reasons of self-medication17. Time saving, financial reason and individual perception of the severity of the health condition have also been documented as the reason for self medication in Jordan7., 22. and Nigeria27.
Analgesics were the most commonly used substances for self medication. This was similar to Souaga et al.’s17 finding in the Ivory Coast and Afolabi et al.’s18 finding in Nigeria. It could be explained by the fact that toothache was the most common oral health problem. Native herbs were the second most frequent utilised substances. High prevalence of consultation with traditional healers and local herb use for toothache among individuals living in the Tanga Region of Tanzania have been reported with 40% relief for more than 6 months28. It confirms the fact that individual in Africa that rely on self-medication for oral health problem are more likely to use modern medicines than traditional ones20. The disposition to utilise lay sources of care like native healers hampers the effectiveness of modern professional health agents and delivery system. There is evident reliance on traditional healers and plant products when dealing with a broad range of oral health concerns29 from ethnomedicine survey use of plants in the treatment of oral ailments like toothache, plaque and caries, pyorrhea and aphthae30. The role of the traditional healer in healthcare delivery and the belief in unorthodox care may have resulted in a high frequency of native herbs for self medication. One-fifth of the respondents used antibiotics for oral health problems, confirming the unrestricted access to antibiotics with its attendant complication in developing countries. Dangerous substances like vinegar, petrol, tobacco, alum and touch and go which are corrosive and unorthodox chemicals were used by 7.4% of the respondents. Such dangerous substances used for an oral health problem have also been reported in studies in the southern parts of Nigeria31., 32.. There is a need for reorientation as complications emanating from the use of these dangerous substances may either be reversible or irreversible. For example, some topically applied substances when taken for tooth pain relief have been reported to cause oral chemical burns24.
In this study, the sources of substances for self medication were mainly pharmacies, followed by roadside vendors (general provision shops and kiosks along the road), native healers, mobile drug vendors in buses and others, like hawkers, village markets etc. In parallel, a large number of pharmacies, street-market traders and traditional healers play a significant role in providing oral health care20. The unrestricted access and readily availability of drugs on demand from hospitals, pharmacies; patient medicine stalls, roadside stalls, and hawkers in developing countries account for the diversity of substances for self medication33., 34., 35., 36..
In this study, half (50.6%) of respondents reported receiving their advice from relatives and friends, 24.5% from pharmacists, 17.7% from personal knowledge, and 8.3% from traditional healers. This is similar to the findings of Yousef et al.22 in Jordan. Significant others were a veritable source of advice as they serve an important role in caring for sick family members or relatives. Pharmacists and patient medicine dealers in developing countries are consulted for any form of health problem because of their ease accessibility, fast services and no consultation fee. The utilisation of a traditional healer in an oral health problem among the respondents was 16.7% reported by a community dwelling adult Chinese people in Hong Kong experiencing orofacial pain37 but lower than the 1.3% reported in a household survey in Burkina Faso20. The role of the traditional healer in dental care in developing countries28., 38. may also explain their relevance in perpetuating self medications for oral health problem among the respondents.
The description of respondents experiences with self medication for oral health problems include temporary reliever of pain, useful in a stressful situation, natural product, cheaper alternative, effective, curative in nature and no felt effect. The varied nature of respondents’ experiences with self medication for oral health problems may be explained by the diversity of oral health conditions, reasons and utilised substance for self medication. Some of the participants correctly described self medication as a step in self care behaviour39. Lay measures in tooth pain relief, resulted in limited and uncertain benefits40 fitting the descriptors like temporary reliever of pain and no felt effect. Cheaper alternative, effective and curative in nature, descriptions may have guided respondents into falsely believing that self medication for oral health problem are appropriate thus perpetuating the behaviour39.
CONCLUSION
The majority of the respondents self-medicated for oral health problems with pharmaceutical products, herbs, corrosive substances and unorthodox chemicals. Unmarried, urban residents, aged 21–30 years reported significantly increased self-medication for oral health problems. The high prevalence of self-medicated and the use of corrosive unorthodox chemicals reported in this study necessitate awareness creation and introduction of preventive and mitigating interventional programmes. Development of an official government policy on prescription and over-the-counter medications is also recommended.
REFERENCES
- 1.Sule SS, Ijadunola KT, Onayade AA, et al. A study on the utilization of primary health care facilities in a rural community. Niger J Med. 2008;17:98–106. doi: 10.4314/njm.v17i1.37366. [DOI] [PubMed] [Google Scholar]
- 2.MacKian S. Complex cultures: rereading the story between health and social capital. Crit Soc Policy. 2002;22:203–225. [Google Scholar]
- 3.Katung PY. Socio-economic factors responsible for poor utilisation of the primary health care services in a rural community in Nigeria. Niger J Med. 2001;10:28–29. [PubMed] [Google Scholar]
- 4.Okonkwo JEN, Ngene JN. Determinants of poor utilization of orthodox health facilities in a Nigerian rural community. Niger J Clin Pract. 2004;7:74–78. [Google Scholar]
- 5.Amaghionyeodiwe LA. Determinants of the choice of health care provider in Nigeria. Health Care Manag Sci. 2008;11:215–227. doi: 10.1007/s10729-007-9038-3. [DOI] [PubMed] [Google Scholar]
- 6.Ilhan MN, Durukan E, Ilhan SO, et al. Self-medication with antibiotics: questionnaire survey among primary care center attendants. Pharmacoepidemiol Drug Saf. 2009;18:1150–1157. doi: 10.1002/pds.1829. [DOI] [PubMed] [Google Scholar]
- 7.Sawair FA, Baqain ZH, Abu Karaky A, et al. Assessment of self-medication of antibiotics in a Jordanian population. Med Princ Pract. 2009;18:21–25. doi: 10.1159/000163041. [DOI] [PubMed] [Google Scholar]
- 8.Wingate D, Phillips SF, Lewis SJ, et al. Guidelines for adults on self-medication for the treatment of acute diarrhoea. Aliment Pharmacol Ther. 2001;15:773–782. doi: 10.1046/j.1365-2036.2001.00993.x. [DOI] [PubMed] [Google Scholar]
- 9.Hernandez-Juyol M, Job-Quesada JR. Dentistry and self-medication: a current challenge. Med Oral. 2002;7:344–347. [PubMed] [Google Scholar]
- 10.Schlenker T, Raedsch R, DeVries JX, et al. Self-medication for abdominal discomfort resulting in life-threatening consequences. Clin Investig. 1993;72:74–75. doi: 10.1007/BF00231122. [DOI] [PubMed] [Google Scholar]
- 11.Reeves DS, Finch RG, Bax RP, et al. Self medication of antibacterials without prescription (also called ‘over-the-counter’ use). A report of a Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother. 1999;44:163–177. doi: 10.1093/jac/44.2.163. [DOI] [PubMed] [Google Scholar]
- 12.Indermitte J, Reber D, Beutler M, et al. Prevalence and patient awareness of selected potential drug interactions with self-medication. J Clin Pharm Ther. 2007;32:149–159. doi: 10.1111/j.1365-2710.2007.00809.x. [DOI] [PubMed] [Google Scholar]
- 13.Ouma F. All Africa Global Media; Kampala: 2007. Uganda: Self Medication Causing Drug Resistance. New vision. [Google Scholar]
- 14.Cohen LA, Bonito AJ, Akin DR, et al. Toothache pain: behavioral impact and self-care strategies. Spec Care Dentist. 2009;29:85–95. doi: 10.1111/j.1754-4505.2008.00068.x. [DOI] [PubMed] [Google Scholar]
- 15.Stoller EP, Gilbert GH, Pyle MA, et al. Coping with tooth pain: a qualitative study of lay management strategies and professional consultation. Spec Care Dentist. 2001;21:208–215. doi: 10.1111/j.1754-4505.2001.tb00256.x. [DOI] [PubMed] [Google Scholar]
- 16.Kouame P, Amantchi D, Samba M, et al. Causes of late odontostomatologic consultations in Ivory Coast. Odontostomatol Trop. 1998;21:24–26. [PubMed] [Google Scholar]
- 17.Souaga K, Adou A, Amantchi D, et al. Self medication during orodental diseases in urban Ivory Coast. Results of a study in the region of Abidjan. Odontostomatol Trop. 2000;23:29–34. [PubMed] [Google Scholar]
- 18.Afolabi AO, Akinmoladun VI, Adebose IJ, et al. Self-medication profile of dental patients in Ondo State, Nigeria. Niger J Med. 2010;19:96–103. doi: 10.4314/njm.v19i1.52488. [DOI] [PubMed] [Google Scholar]
- 19.Lam CLK, Tse MHW, Munro C. A survey on the use of self medication over a period of two weeks. HK Pract. 1989;11:371–375. [Google Scholar]
- 20.Varenne B, Petersen PE, Fournet F, et al. Illness-related behaviour and utilization of oral health services among adult city-dwellers in Burkina Faso: evidence from a household survey. BMC Health Serv Res. 2006;6:164. doi: 10.1186/1472-6963-6-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Samba M, Guinan JC, Sangare A, et al. Oral health care practices in Abidjan. Odontostomatol Trop. 2004;27:37–40. [PubMed] [Google Scholar]
- 22.Yousef AM, Al-Bakri AG, Bustanji Y, et al. Self-medication patterns in Amman, Jordan. Pharm World Sci. 2008;30:24–30. doi: 10.1007/s11096-007-9135-x. [DOI] [PubMed] [Google Scholar]
- 23.Shankar PR, Partha P, Shenoy N. Self-medication and non-doctor prescription practices in Pokhara valley, Western Nepal: a questionnaire-based study. BMC Fam Pract. 2002;3:17. doi: 10.1186/1471-2296-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Antunes LAA, Kuchler EC, de Andrade Risso P, et al. Oral chemical burns caused by self-medication in a child: case report. J Burn Care Res. 2009;30:740–743. doi: 10.1097/BCR.0b013e3181ac0571. [DOI] [PubMed] [Google Scholar]
- 25.Preshaw PM, Meechan JG, Dodd MD. Self-medication for the control of dental pain: what are our patients taking? Dent Update. 1994;21:299–304. [PubMed] [Google Scholar]
- 26.Eya’Ane M, Toure B, Ngono E, et al. Poverty and ignorance: the cause of late consultation in odontostomatology at the University Hospital Center in Yaounde. Odontostomatol Trop. 2001;24:11–14. [PubMed] [Google Scholar]
- 27.Fasina O, Ubah JN. Pattern of pre-hospital consultation among ophthalmic patients seen in a tertiary hospital in South West Nigeria. Afr J Med Med Sci. 2009;38:173–177. [PubMed] [Google Scholar]
- 28.Ngilisho LA, Mosha HJ, Poulsen S. The role of traditional healers in the treatment of toothache in Tanga Region, Tanzania. Community Dent Health. 1994;11:240–242. [PubMed] [Google Scholar]
- 29.Tapsoba H, Deschamps JP. Use of medicinal plants for the treatment of oral diseases in Burkina Faso. J Ethnopharmacol. 2006;104:68–78. doi: 10.1016/j.jep.2005.08.047. [DOI] [PubMed] [Google Scholar]
- 30.Hebbar SS, Harsha VH, Shripathi V, et al. Ethnomedicine of Dharwad district in Karnataka, India – plants used in oral health care. J Ethnopharmacol. 2004;94:261–266. doi: 10.1016/j.jep.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 31.Omogbai EKI, Ehikhamenor EE, Ojo MA. Effects of some patients’ perceptions and practices on the treatment of dental diseases – a study of the situation in Benin City, Edo State, Nigeria. West Afr J Pharmacol Drug Res. 2005;20:44–47. [Google Scholar]
- 32.Sofola OO, Uti OG. Coping with oral pain: lay management strategies adopted by patients prior to presentation. Nig Q J Hosp Med. 2009;19:59–62. doi: 10.4314/nqjhm.v19i1.50210. [DOI] [PubMed] [Google Scholar]
- 33.Obaseiki-Ebor EE, Akerele JO, Ebea PO. A survey of antibiotic outpatient prescribing and antibiotic self-medication. J Antimicrob Chemother. 1987;20:759–763. doi: 10.1093/jac/20.5.759. [DOI] [PubMed] [Google Scholar]
- 34.Lansang MA, Lucas-Aquino R, Tupasi TE, et al. Purchase of antibiotics without prescription in Manila, the Philippines. Inappropriate choices and doses. J Clin Epidemiol. 1990;43:61–67. doi: 10.1016/0895-4356(90)90057-v. [DOI] [PubMed] [Google Scholar]
- 35.Kafle KK, Gartoulla RP, Pradhan YM, et al. Drug retailer training: experiences from Nepal. Soc Sci Med. 1992;35:1015–1025. doi: 10.1016/0277-9536(92)90241-h. [DOI] [PubMed] [Google Scholar]
- 36.Wolff MJ. Use and misuse of antibiotics in Latin America. Clin Infect Dis. 1993;17(Suppl 2):S346–S351. doi: 10.1093/clinids/17.supplement_2.s346. [DOI] [PubMed] [Google Scholar]
- 37.Zheng J, McMillan AS, Wong MC, et al. Investigation of factors associated with treatment-seeking in Southern Chinese with orofacial pain. J Orofac Pain. 2010;24:181–188. [PubMed] [Google Scholar]
- 38.Ogunbodede E. Dental care: the role of traditional healers. World Health Forum. 1991;12:443–444. [PubMed] [Google Scholar]
- 39.Bartlomé JA, Bartlomé P, Bradham DD. Self-care and illness response behaviors in a frontier area. J Rural Health. 1992;8:4–12. doi: 10.1111/j.1748-0361.1992.tb00322.x. [DOI] [PubMed] [Google Scholar]
- 40.Cohen LA, Harris SL, Bonito AJ, et al. Coping with toothache pain: a qualitative study of low-income persons and minorities. J Public Health Dent. 2007;67:28–35. doi: 10.1111/j.1752-7325.2007.00005.x. [DOI] [PubMed] [Google Scholar]