Abstract
Objective: To analyse the demographics surrounding and the sustainability of a course in Emergency Dental Care and Health Promotion developed and taught by a team of dentists from the United States to refugee camp health-care workers in two long-term refugee camps in Western Tanzania. Methods: Refugee camp dental patient log books from Mtabila and Nyarugusu camps Kigoma, Tanzania were analysed and demographic data collected on each patient visit from the programme inception in November 2007 until August 2009. Data collection included information relevant to 1961 patient visits. Data were entered into SPSS Statistics 17.0 using the Freq application. Outcomes: Patient visit data included demographics involving both the resident camp populations and the surrounding communities. The distribution of patients treated by nationality was: 58% Burundian (Mtabila), 14% Congolese (Nyarugusu), and 28% Tanzanian citizens residing near both camps. Extractions accounted for 95.5% of procedures performed. Recorded incidences of post-operative complications were 1 > % of patient visits. Patient visits were steady over time and a referral system was implemented for complex cases. Health promotion sessions were held in both camps. Conclusion: This dental programme has been self-sustaining and is providing some access to care where none existed previously. Programmes such as this may be one solution to the access to dental care problem in long-term refugee camps.
Key words: Refugees, oral health care, health promotion, access to care
INTRODUCTION
Under the United Nations Convention Relating to the Status of Refugees from 1951, a refugee is a person who (according to the formal definition in article 1A of this Convention), owing to a well-founded fear of being persecuted on account of race, religion, nationality, membership of a particular social group or political opinion, is outside the country of their nationality, and is unable to or, owing to such fear, is unwilling to avail him/herself of the protection of that country1. There are currently about 10 million refugees under the auspices of the United Nations High Commissioner for Refugees (UNHCR) worldwide2. The United Republic of Tanzania has been host to Africa’s largest concentration of refugees since its independence in 1964; currently close to half a million people3.
The realities of life in such places can be difficult on many levels. Although most refugees arriving to these camps receive health screenings by the UNHCR, and health care is provided through international agencies and local Non-Government Organisations (NGO), this does not include dental care. In developing countries, oral health services are severely lacking. In Africa, for instance, the dentist to population ratio is approximately 1:150,0004.
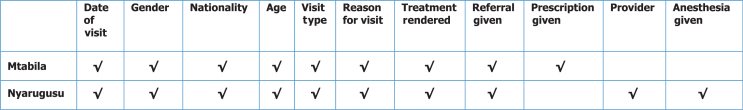
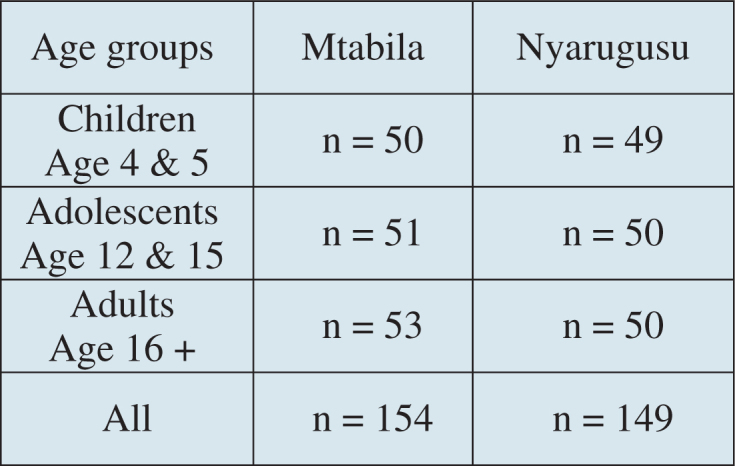
In February 2006, an initial site and oral health assessment was conducted in two long-term camps in the Kigoma region of Tanzania; Mtabila (Burundians n = 40,000), and Nyarugusu (Congolese n = 20,000). Refugees from each of three target groups were selected; children adolescents and adults (Figure 1). Intra-oral examinations were performed within the medical facilities in the camps using modified CDC and WHO protocols5., 6.. The prevalence of dental caries among children, adolescents and adults was 64%, 31% and 70% respectively (Figure 2), with many complaints of previous or current pain and infection5. According to the literature, one of the key differences between refugees and populations from developing countries, migrants, and internally displaced persons (IDP) in terms of health care, is that refugees do not control their own destinies and are confronted with new, possibly hostile environments that in many cases differ in language, background, culture, climate and food7. Newly arriving refugees and asylum seekers may experience poor oral health due to these and other factors8. As the above statistics indicate, dental disease is highly prevalent among this particular population of refugees and intervention was needed.
Figure 1.
Initial site assessment 2006 population sampling.
Figure 2.
Camp caries prevalence in 2006.
In November 2007 a team of four volunteer dentists from the United States arrived at Mtabila and Nyarugusu refugee camps to establish a small dental clinic in each camp and provide a 2 week training course in Emergency Dental Care and Health Promotion to a group of 12 refugee health-care workers, similar to a programme described in 2000 by Ogunbodede et al9. Logistical support on site was provided by the Tanzania Red Cross (TRC) who had selected 12 students to participate in the course. Ten of the students were working in at least one of the above camps as health care providers in some capacity, although none had any formal dental training. Two of the students were from the nearby Kabanga Hospital which, until this team arrived, had no formal association with the camps. The training course consisted of topics focusing on health promotion and the relief of dental pain and infection with the following three goals in mind; to train and teach dental health care providers in the camps to:
-
•
Provide safe, emergency dental care in the field
-
•
Know their limits and know when to refer patients to the hospital
-
•
Teach community based dental health promotion
The initial 2 weeks course had a lecture and clinical component. Translation was provided from English to Swahili and Kirundi through the TRC. Donated dental chairs, surgical instruments and educational materials were utilised in the training and were left for use after the team departed. Access to anaesthetics and disposables such as gauze, gloves, masks, and medications are available on an ongoing basis in the camps through the medical supply system.
The following topics were taught and put to immediate use in the training:
-
•
Preparing the clinic
-
•
Triage techniques
-
•
Patient management
-
•
Dental and medical history taking
-
•
Intra-oral examination
-
•
Knowing when to treat or refer
-
•
Extraction techniques
-
•
Simple treatment of periodontal problems
-
•
Preventing and treating post-operative complications
-
•
Patient dismissal
-
•
Sterilisation
-
•
Health promotion.
Training topics were selected based on the following: the observed level of care that was being provided, the oral health assessment data described above, and other dental training programmes9., 10..
Another goal of the establishment of this programme was to initiate a referral system with the local civilian hospital to enable the refugee dental providers a means of referral for complex cases. Though the hospital dental clinic is itself rudimentary, it staffs a dental therapist and assistant with formal dental training who were also participants in the initial training course in November 2007. Arrangements were made to allow for the referral of patients from the camps to the hospital dental clinic if cases were too complex for the trainees to treat.
August 2008, another team of volunteer dentists, two of whom had participated in the first training, arrived back at the camps to evaluate the progress of the students from the first training and provide a 2 week refresher course. Ten of the original 12 students participated in the second training. In this second session, all of the topics listed above were reviewed in detail and expanded upon as necessary.
METHODS
In August 2009, 22 months into the programme, an evaluation was done. After obtaining clearance from The Tanzania Ministry of Home Affairs, data were collected from the dental clinic log books of the two camps on each patient visit from the onset of the programme. The major research questions were:
-
•
What was the demographic make-up of patients being treated?
-
•
What was the incidence of post-operative complications?
-
•
How many patients were referred to the hospital?
-
•
How were health promotion sessions being conducted?
-
•
Is the programme sustainable over time?
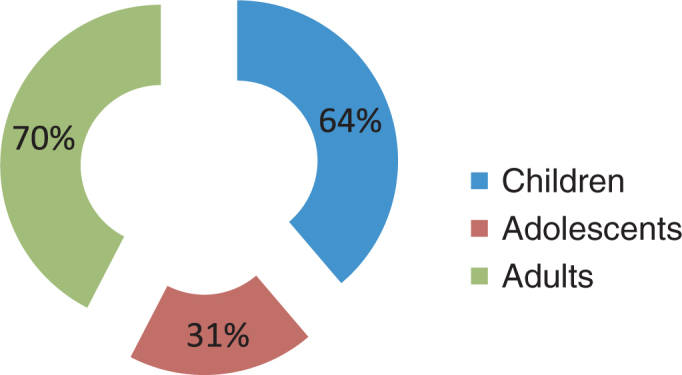
Each camp keeps written records of every patient visit which includes demographic and procedure specific information. However, the two camps varied slightly on some of the information that was being collected (Figure 3). Translation from Swahili to English was provided by a TRC employee now working in Mtabila camp as one of the dental providers; however most of the documentation in the log books was written in English. Some information was irrelevant and not recorded in the programme assessment. Patient names and addresses were also collected in the log books but not recorded in this data to respect patient confidentiality and to de-identify the data. Sixteen data categories collected from both camps used for each patient visit are shown in Table 1 and were analysed for the demographic portion of this study.
Figure 3.
Data variables available in log books per camp.
Table 1.
Data categories recorded for the study
| General demographics |
| 1. Gender |
| 2. Nationality |
| 3. Age |
| 4. Visit type |
| a. Primary |
| b. 1 week post-operative |
| c. 2 week post-operative |
| Reason for visit |
| 5. Pain |
| 6. Swelling |
| 7. Periodontal disease |
| 8. Retained root |
| 9. Bleeding |
| 10. Other |
| Treatment rendered |
| 11. Rx antibiotic |
| 12. Rx pain |
| 13. Rx other |
| 14. Extraction |
| 15. Referral to hospital |
| 16. Month of service |
Since one of the goals of this research was to assess the established dental programme’s sustainability over time, the specific demographics of the populations served were looked at as well as the incidence of patients returning after initial treatment with complications resulting from the care provided; i.e. post-operative complications. Patients returning within 1 or 2 weeks with a chief complaint pertaining to previous treatment provided were considered to have experienced a post-operative complication. The referral system to the local hospital for complex cases was also evaluated. This hospital also maintains log books containing the records of patients treated and referral sources. Referrals made per camp were compared with actual patients seen at the hospital.
Since health promotion was an important part of the training of the health care providers, the approximate number of health promotion sessions held was also collected. For this data, the providers from both camps were questioned as to how health promotion sessions were carried out and the frequency with which they were occurring.
RESULTS
There were a total of 1,961 patient visits, 1,532 at Mtabila and 429 at Nyarugusu, from November 2007 when the first training occurred to August 2009 when the formal evaluation was completed. Dental care was provided 1 day/week at Mtabila and 2 day/week at Nyarugusu. As in 2006, Mtabila camp houses Burundian refugees (n = 35,000) while Nyarugusu (n = 38,000) houses refugees of Congolese decent (note: population numbers have changed since 2006). Both camps also treat Tanzanian citizens on a limited basis. The overall gender/ethnic breakdown of patients treated is: in all groups, Burundian, Congolese and Tanzanian, females were treated more frequently than males; 63%, 57% and 63% respectively. The overall distribution of ethnicity of patients treated was Burundian 58%, Tanzanian 28% and Congolese 14% (Figure 4). Since the Burundian population was the most frequently treated (58%), the author acknowledges that data may be biased to this population. Patient visits were slowly increasing over time (Figure 5).
Figure 4.
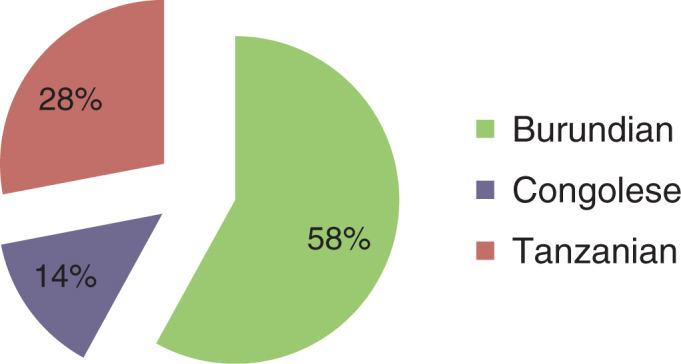
Ethnic distribution of patients treated in both camps.
Figure 5.
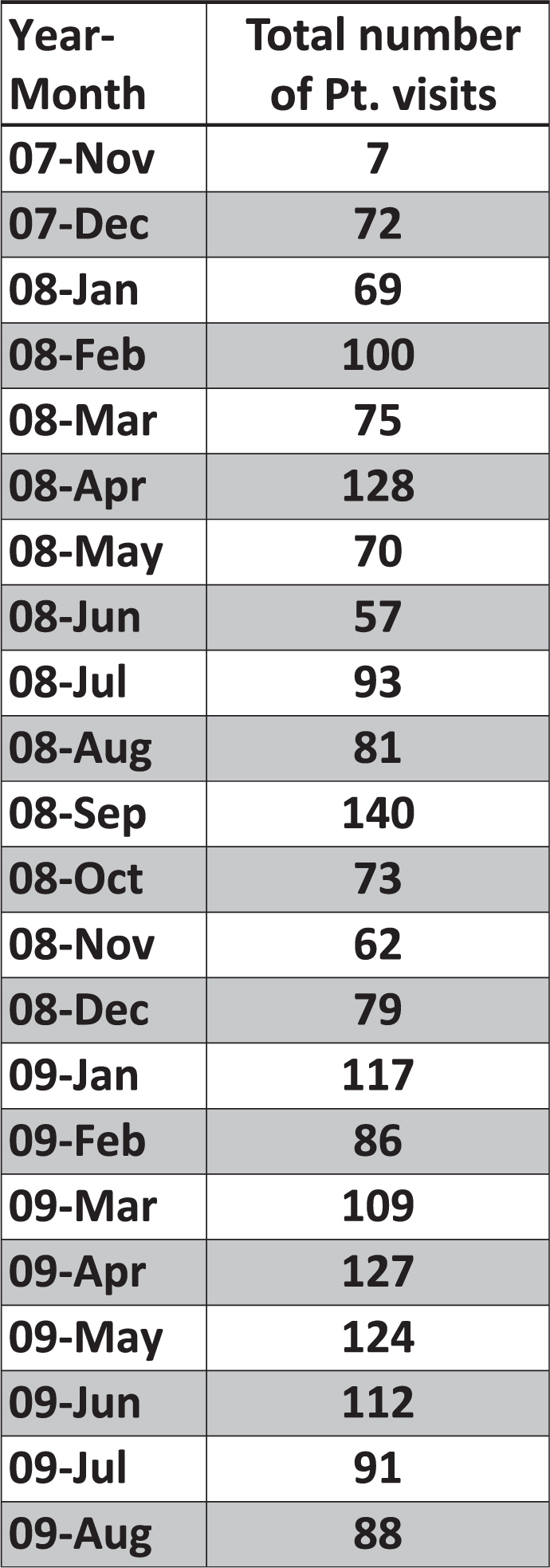
Patient visits per month.
The mean age of all patients treated was 29.4 years (range 2–87 years). The overall age distribution by percentage is illustrated in Figure 6. By far the main reason patients sought dental care was because they were experiencing pain; n = 1,944 patients (99%). Swelling was the second most common reason with n = 53 patients or 2.7% while periodontal disease followed at n = 10 patients, 0.5%. Note that some patients had multiple reasons for visiting the dental clinic; there being 2,014 reasons for the 1,961 patient visits. Bleeding was a category that was originally tracked independently in the data collection process. There were no incidences recorded where bleeding was the reason for a dental visit, therefore, it was dropped as an individual category in the data presented in Figure 7. The initial site assessment found the rate of dental caries to be the highest in the adult group (70%), followed by children under 12 (64%) then adolescents at (31%)3. This study demonstrates the distribution of patients treated as: adults 75.2%, children under 12 18.8% and adolescents 12–15, 4.8%. In 1.2% of patients treated, age was unknown. Note that the age classification in this study differs slightly from the initial site and oral health assessment of 2006 (Figures 1 and 6). The majority of patients, n = 1,876 (95.5%), received dental extractions. Other treatments rendered included prescriptions for antibiotics and pain medications, periodontal treatment, and hospital referrals (Figure 8).
Figure 6.

Percentage age distribution of patients treated.
Figure 7.
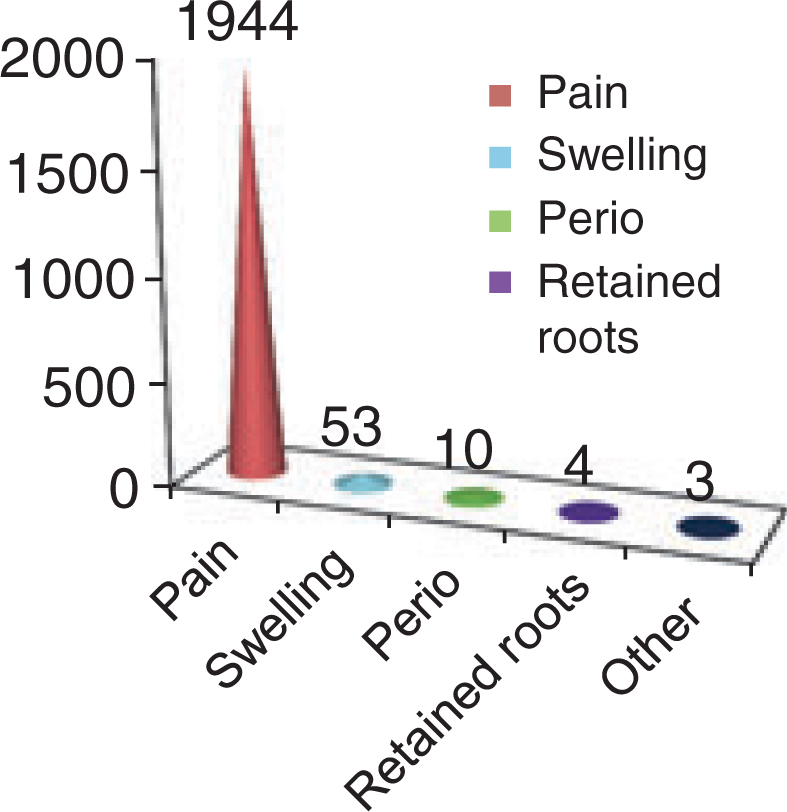
Reasons for dental visits.
Figure 8.
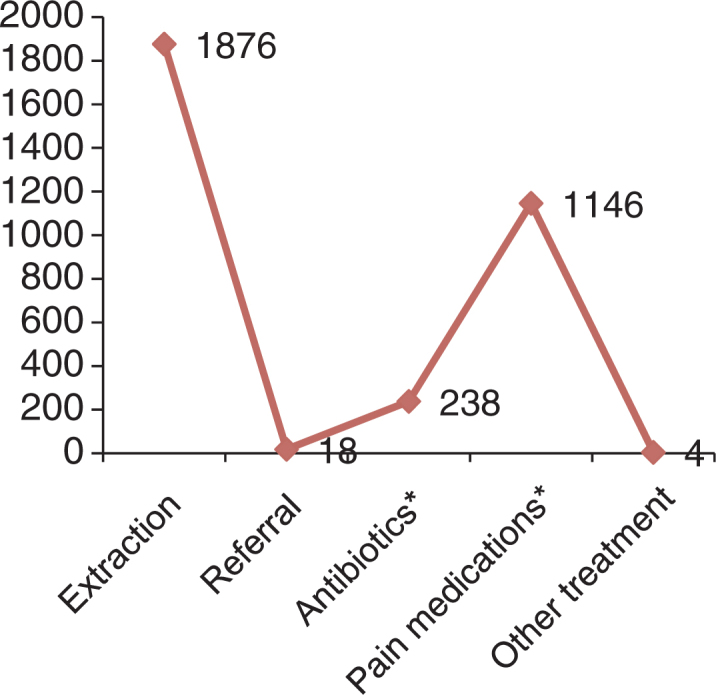
Treatments rendered. ‘*’ Medications were only recorded in Mtabila log, no data for Nyarugusu.
One area that the author was particularly interested in was the incidence of post-operative complications. Only eight patients returned to the clinic within 1 or 2 weeks of initial treatment with complaints of pain, swelling or retained root tips after initial treatment. The reason for this is not completely clear, but it may be inferred that if they were experiencing pain or other complications post-operatively, they might have returned to the dental clinic to seek additional care since they sought care initially. This cannot be proven, however, and many other reasons might prevent patients from being able to return. For example, the clinics maintain limited hours of operation which could be a barrier in itself. Also, although these are long-term camps, residents do repatriate to their native countries. The populations are not constant. On food distribution days in the camps, priority is given to collecting allotted food rations for residents which may take a majority of the day. As a result, dental care, if available that day, may not be a priority. The most common reason for returning to the clinic after the initial visit was continued pain or swelling.
Documented patient referrals to the hospital were four Burundians, seven Congolese and seven Tanzanians. Free transportation to the hospital for the refugees was provided by the TRC, however, treatment rendered was not free of charge. There was a $3,000 TSh fee imposed per visit which translates to approximately US$3 per refugee. This cost may be prohibitive to most refugees. According to Kabanga hospital records, over the 22-month period in question, only 9 (50%) of referrals made, were actually treated; eight from Mtabila and one from Nyarugusu.
Health promotion sessions varied by camp. The Nyarugusu staff conducted health promotion sessions at the onset of every clinic day, (twice per week) for waiting patients and their accompanying families. They also teamed up with the health educators in the camp and periodically went out into the community talking about oral health to the residents. They also conducted four sessions for the camp schools over the studied time period. The Mtabila staff conducted one session per week at the onset of the clinic day for waiting patients and their accompanying families. In both camps, health promotion sessions consisted of discussing oral hygiene, healthy diet, and demonstrating tooth brushing technique with models.
DISCUSSION
This programme, to date, has proven to be sustainable over time. The data suggest that at least some of the oral health needs of both camp populations as well as a small segment of the native population in the area are being addressed and are ongoing at the time of this publication. The incidence of post-operative complications was negligible (>1%). Various treatments were rendered successfully though the vast majority of patients received dental extraction(s) (Figure 8). The author acknowledges that since the data collection was limited to the factors listed above some patients may have experienced post-operative complications and chose not to or were unable to return to the clinic for subsequent treatment. Others may have repatriated or not returned to the clinic for various other reasons. Further data collection is indicated.
There were three times more patients treated at Mtabila (n = 1,532) than Nyarugusu (n = 429) despite Nyarugusu providers working 2 day/week compared with Mtabila’s one. It is notable that in the original site assessment of 2006, the incidence of caries was higher overall in the Burundian population5. There may or may not be a correlation here and the data collected in this study cannot determine this.
Other issues that could be researched further are the referral system and total costs of the training programme. Only 50% of the patients referred to the hospital were actually treated. This could be due to the fee that the hospital charged patients, as discussed above, which may be cost prohibitive for many refugees. A cost benefit analysis of the entire programme should be completed to determine the actual costs of equipping the clinics, travel for the volunteer trainers, training materials, costs incurred per patient treated as well as costs of patient referrals both to the TRC and referral hospital. The author believes that quantifying a dollar figure on this programme may help to determine the feasibility of the funding of such programmes in the future.
The next clinical training objective would be to incorporate the technique of Atraumatic Restorative Treatment (ART) into the treatment options and armamentarium of the providers within the camps, giving them another treatment option for patients. This technique has been proven to work in field settings where environmental resources are limited and economic and living conditions are difficult11., 12.. ART training could be conducted in a similar manner as the rest of the course.
The author acknowledges that there are currently no specific WHO guidelines for evaluating oral health promotion and disease prevention programmes such as the one described above, though some guidelines are in development13. Petersen and Kwan state that the science of such evaluations in general is ‘poorly developed and documented and more research needs to be done in this area’. This makes it difficult to quantify the success of this programme. That being said, however, oral health care should be an integral part of the health care system within long-term refugee camps9. The UNHCR recognises the value of providing health services to refugees to minimise morbidity and mortality14. As part of the primary health care approach in long-term refugee camps, camp health-care workers, many of whom are refugees themselves, can provide a basic level of dental care by gaining the basic knowledge, skills and instrumentation needed9., 10.. In theory, oral health care for refugees should not differ from what is being provided for people living in developing countries. Basic emergency dental treatment for pain relief, infection, and treatment of maxillo-facial injuries should be provided. Oral manifestations of systemic diseases like those associated with HIV/AIDS, and suspected cases of oral cancer should be recognised. Treatment outside the realm of practice for such dental care providers should be referred to local hospitals when available10.
Programmes such as the one described above could be instituted in other refugee camps if site assessments determine need. Variations in geographical movements, diet, cultural background, political and socio-economic status all play a role in determining the needs of a particular population. Programmes developed in one site may or may not be appropriate for another6. If a programme such as this were implemented at another site, data collection post-training would be appropriate to ascertain similarities or differences to the findings of this study. It is the opinion of the author that this training, though rudimentary in nature, has provided some level of safe, emergency dental care and oral health promotion education to refugee camp residents and surrounding native peoples where none existed before. Programmes such as this may be a feasible way to address the oral health care needs of refugees in other long-term camp environments.
Acknowledgements
This paper was written as a result of active participation in the Health Volunteers Overseas Kigoma Tanzania project in 2007, 2008 and 2009 (Figure 9., Figure 10., Figure 11.). The author wishes to recognise the American Dental Association’s Center for International Development and Affairs, Health Volunteers Overseas and the Tanzania Red Cross for the logistical and human resources support provided. Thanks to Drs. Freder Jaramillo, Jack Levine, Christine Lathuras and Richard Heidemann for their contribution to curriculum development and teaching. Thanks to Dr. Joseph Vitolo, Dr. Evelyn Donate-Bartfield and Dr. Alexis Dye for their organisational and statistical support. Last but not least, she acknowledges the valuable help and dedication of Father Paul Flamm whose lifework of helping refugees in these camps brought us to Tanzania in the first place.
Figure 9.
A typical refugee dental patient with severe caries and periodontal disease.
Figure 10.
Giving clinical instruction on extraction technique while the students look on.
Figure 11.
One of the students offering health promotion instruction as waiting dental patients look on.
REFERENCES
- 1.UNHCR Convention and Protocol Relating to the Status of Refugees 1951 Article 1, p. 16 Available from: http://www.unhcr.org/3b66c2aa10.html. Accessed 19 April 2011
- 2.UNHCR Refugee Figures. Available from: http://www.unhcr.org/pages/49c3646c1d.html. Accessed 19 April 2011
- 3.Central Intelligence Agency, World Fact Book Tanzania. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/tz.html. Accessed 19 April 2011
- 4.Peterson PE. Improvement of oral health in Africa in the 21st century – the role of the WHO Global Oral Health Program. Developing Dent. 2004;5:17. [Google Scholar]
- 5.Beltran E, Cherrett H, Hobdell M et al.Tanzania Site Assessments. Refugee Camps. Faculty of Dentistry, Muhimbili University, Tanzania Dental Association. CDC Release, March 2006.
- 6.World Health Organization . 4th edition. WHO; Geneva: 1997. Oral Health Surveys – Basic Methods. [Google Scholar]
- 7.Medecins Sans Frontieres . MacMillan Education Ltd; London: 1997. Refugee Health: An Approach to Emergency Situations. [Google Scholar]
- 8.Victorian Refugee Health Network. Oral Health. Available from: http://www.refugeehealthnetwork.org.au/projects-and-programs/OralHealth. Accessed 19 April 2011
- 9.Ogunbodede EO, Michenautsch S, Rudolph J. Oral health care in refugee situations: Liberian refugees in Ghana. J Refug Stud. 2000;13(3):328–335. [Google Scholar]
- 10.Htoon HM, Mickenautsch S. World Health Organisation; Geneva: 2000. Oral Health Care in Camps for Refugees and Displaced Persons. Oral Health Programme, Management of Noncommunicable Diseases. WHO/NMH/ORH/00.1. [Google Scholar]
- 11.Frencken JE, Makoni F, Sithole WD. Atraumatic restorative treatment and glass-ionomer sealants in a school oral health programme in Zimbabwe: evaluation after 1 year. Caries Res. 1996;30:428–433. doi: 10.1159/000262355. [DOI] [PubMed] [Google Scholar]
- 12.Phantumvanit P, Songpaisan Y, Pilot T, et al. Atraumatic restorative treatment (ART): a three-year community field trial in Thailand – survival of one-surface restorations in the permanent dentition. J Public Health Dent. 1996;56:141–145. doi: 10.1111/j.1752-7325.1996.tb02424.x. discussion 161–163. [DOI] [PubMed] [Google Scholar]
- 13.Petersen PE, Kwan S. Evaluation of community-based oral health promotion and oral disease prevention – WHO recommendations for improved evidence in public health practice. Community Dent Health. 2004;21(Suppl.):319–329. [PubMed] [Google Scholar]
- 14.UNHCR/M.Pearson, September 2005. Available from: http://www.unhcr.org/pages/49c3646cdd.html. Accessed 19 April 2011
FURTHER READING
- 15.Dickson M. Hesperian; Berkely, CA: 2009. Where there is no Dentist. ISBN: 978-0-942364-05-7. [Google Scholar]