Abstract
The implementation of a new paradigm for caries management is necessary for the profession to respond effectively to changing population health needs. The FDI Global Caries Initiative (GCI) is a 10 year programme aimed at developing and implementing a new paradigm for caries management, one that would contribute to a common vision of health. The article reviews the global health policy landscape and examines how it might influence and shape the implementation of the GCI.
Key words: Global, caries, matrix, oral health
BACKGROUND
A recent editorial in The Journal of the American Dental Association notes that the predominant model of dental care based on G.V. Black’s1 caries lesion classification and disease management system is more than 100 years old and ‘although many of its principles still hold true, the system increasingly is unable to meet the needs and demands of our patients2.
In 2009 the FDI World Dental Federation established the Global Caries Initiative (GCI)3, a profession led 10 year programme aiming at developing and implementing a new paradigm for caries management, one that would contribute to a common vision of health. The GCI is now at the end of its first phase (2009–11) and has achieved political consensus towards establishing a comprehensive framework that includes caries classification and management systems4.
In this article we examine how the global health policy context might influence and shape the implementation of the GCI, as well as identifying some of the challenges and opportunities that lie ahead.
The global risk landscape
The 2011 Global Risks Landscape report by World Economic Forum5 (WEF) maps the perceived likelihood of issues occurring in the next 10 years against the impact in billions of US dollars. The report concludes that the increasingly interconnected nature of systems will require an understanding of the systems behind risks, as well as the risk context. Governments are beginning to adopt a comprehensive ‘whole government’ approach to many issues, recognising that effective solutions lie in engaging many sectors and involving multiple agencies, as well as civil society.
With this in mind we review four global initiatives that are very likely to affect the implementation of the Global Caries Initiative and have wider implications for shaping the future of dental medicine and oral health.
Non-communicable diseases
The statistics around non-communicable diseases (NCDs) are staggering; over the next 20 years NCDs will cost more than 47 trillion US dollars, with 63% of all deaths worldwide currently stemming from NCDs. The highest burden will be carried by low- and middle-income countries6.
The urgency and need for global action was recognised by the United Nations (UN) High Level meeting on Control and Prevention of NCDs held in New York (September 2011), which is only the second time the UN has dedicated a meeting to health, the first being HIV AIDS pandemic. The meeting approved the UN Political Declaration on Prevention and Control of NCDs7, which sets out member states’ response. The political declaration recognised the significance of oral diseases, with paragraph 19 stating that ‘renal, oral and eyes diseases pose a major health burden for many countries and that these diseases share common risk factors and can benefit from common responses to NCDs’. Paragraphs 61, 62 and 63 mandated the World Health Organisation (WHO) to develop a Global Monitoring Framework (GMF)8 along with a set of targets and indicators.
It is very likely that these targets and indicators will focus on the four main NCDs; cardiovascular diseases, chronic respiratory diseases, diabetes, and cancer as well as on the common risk factors, such as unhealthy diet, tobacco use, physical inactivity and harmful alcohol use.
Dental caries affects most adults in the world and is the most common chronic disease of children. Oral diseases have a significant psychosocial, socio-economic and developmental impact on individuals and health systems of all countries. All the four main NCDs are related to oral conditions and further, they share the same risk factors including unhealthy diet, tobacco use, and harmful alcohol use. Hence a common risk factors approach will enable multiple health conditions to be prevented, controlled and managed by focusing on risk factors common to all of them.
Health related behaviours are modifiable, particularly if introduced early in life. The most effective way to change behaviours is to change the environment. Healthy lifestyles need to be an integral part of the development and surroundings of every child as recommended by the WHO’s Commission on the Social Determinants of Health (SDH)9. This will require a multi sectoral approach to engage sectors outside health, for example transport, urban planning, infrastructure in promoting physical activity and healthy living.
The NCD agenda will determine health and development priorities over the next 20 years. Dental caries is acknowledged as a major global public health issue. The GCI allows national dental associations and dentists to engage in national NCD policy debates and advocate for the strengthening health systems through emphasis on primary health care, including primary oral health care. By prioritising infants, the GCI places oral health within the spectrum of maternal and child health programmes, opening new avenues of collaborative practice and strengthening our role in the multi sectoral approach.
Public health, dental practice and the environment
The WHO report, Healthy Hospitals, Healthy Planet, Healthy People10, addresses climate change in health care settings and notes that ‘global climate change is no longer an ominous future threat, but a dawning reality, one that is already creating disturbing shifts in the natural and human environment and eroding the delicate balance of our planet’s ecosystem and the species that depend on it’.
WHO details seven aspects that underpin a climate friendly hospital and calls for urgent comprehensive multi-sectoral action. This shift in political thinking towards a whole government approach and the reframing of health within a wider development context is increasingly reflected in UN and WHO policy initiatives, such as the Health Environment Linkage Initiative (HELI)11, which is a ‘global effort by WHO and UNEP to support action by developing country policymakers on environmental threats to health, encouraging countries to address health and environment linkages as integral to economic development’.
Challenges exist in developing technologies, techniques and materials to support the new paradigm of caries management, but the adoption of a green dentistry approach will align GCI and the profession with wider health and environment policy.
UN Rio+20; support for the Strategic Approach to International Chemical Management (SAICM)
The Rio+20 meeting in Brazil in June 2012 involved world leaders, governments, the private sector, NGOs and other groups in an effort to address ways to ‘reduce poverty, advance social equity and ensure environmental protection on an ever more crowded planet to get to the future we want12.
A key focus is sustainable development, which is defined as ‘meeting the needs of the present without compromising the ability of future generations to meet their own needs13. It is viewed as the guiding principle for long-term global development and consists of three pillars: economic development, social development and environmental protection.
The Strategic Approach to Chemical Management (SAICM)14 is emerging as an area of consensus within the Rio +20 discussions. SAICM was developed to ensure that, by the year 2020, chemicals are produced and used in ways that minimise significant adverse impacts on the environment and human health. Current areas include nanomaterials, with the third International Conference on Chemicals Management15 likely to witness endocrine disruptor chemicals being added as an emerging global issue. SAICM has produced a draft strategy for the engagement of the health sector in SAICM implementation16.
United Nations Environmental Programme (UNEP) Intergovernmental negotiating committee process; the future use of materials for dental restoration
Probably one of the most important political processes in relation to dentistry has been taking place over the last 4 years. In the 2009 UNEP Governing Council was mandated by its member states to develop a legally binding instrument (LBI) on mercury17. Due to be finalised by February 2013, the LBI (Treaty/Convention) is highly relevant to oral health, as it will include provisions for dental amalgam, which is under the section products and processes, where it is currently classed as mercury-added product.
At the first session of the UNEP Intergovernmental Negotiating Committee to prepare a global legally binding instrument on Mercury18, WHO gave a presentation at a technical briefing session noting that ‘a global near term ban on amalgam would be problematic for public health and the dental sector, but phase down should be pursued by promoting disease prevention and alternatives to amalgam, research and development of cost-effective alternatives and education of dental professionals and raising public awareness’.19 This approach was subsequently reflected in the report from the WHO Experts Consultation20.
FDI General Assembly approved a resolution in 2010, which clearly stated that dental amalgam was a safe and effective restorative material and should remain without restrictions as a clinical treatment option21. The General Assembly resolution also recognises the LBI (Treaty) as an unique opportunity to implement a new paradigm for caries management (GCI) and called upon governments to ‘foster and ensure the phase up of effective prevention for dental caries and associated health promotion programmes. This should be linked to preventive disease management, which will result in the phase down of the use of all restorative materials, including dental amalgam’21.
The management of caries is included with the scope of several global initiatives; WHO NCD policy and global monitoring framework, UN climate change and development and the environment (SAICM, UNEP mercury treaty). A key element in GCI implementation will be developing a strong communications plan that articulates and explains its objectives to different stakeholder groups; policy makers, public health, researchers, educators, clinicians, business and the public.
WHO transformational scale up of health profession education; a question of quantity, quality and relevance
In 2009 WHO and US Presidents Emergency Plan for AIDS Relief (PEPFAR) began work to address the global crisis in health workforce, the lack of access to quality health services faced by a billion people worldwide and the failure of health systems to adapt to changes in population health. While an increase in the numbers of health professionals was cited as an imperative, so was the need to strengthen their impact on population health outcomes.
In its review paper Transformative Scale up of Health Professional Education22, WHO identifies three dimensions that are to be considered in education and health system reform, the quality, quantity and relevance of health care providers. Health profession leadership is required to help improve health system performance and outcomes. Health professions have already begun to examine the issues, for example through the Medical and Nursing Education Partnership Initiatives (MEPI23 and NEPI24).
At the same time governments are encouraging health professions to move towards collaborative practice and inter-professional education to build more flexible workforces and allow for best use of scarce human and financial resources.
GLOBAL CARIES INITIATIVE, PHASE 1 ACHIEVEMENTS AND RESULTS
The Global Caries Initiative was created conceptually in 2008 to address the global public health challenge of dental caries. FDI, the principal representative body for more than 1 million dentists worldwide, launched the Global Caries Initiative at the Rio Caries Conference in Rio de Janeiro, Brazil in 2009. Its aim was to facilitate the implementation of a new paradigm for caries management through a broad alliance of key influencers and decision-makers from research, education, clinical practice, public health, government, and industry, partnering in a common goal: to effect fundamental change in health systems and individual behaviour to STOP* Caries by 2020 (*initiation and progression)25.
The GCI Rio Caries Conference was held in collaboration with FDI member, the Brazilian Dental Association (ABO) and partners International Association for Dental Research and the International Federation of Dental Educators and Associations. Key outcomes were:
-
•
Prioritisation of the 0–3 age group
-
•
Eradication of early childhood caries in children under 3 years of age
-
•
Prioritising primary and secondary prevention and health promotion for caries management
-
•
Need for consensus on caries terminology
-
•
Need to establish a new common language for caries classification and management.
This conference was followed up with other regional meetings in Singapore, during the FDI Annual World Dental Congress; in New York, during the Greater New York Dental meeting; and in 2010 it was introduced in Dubai during the AEEDC meeting; Durban at the South African Dental Association conference (October 2010); and in Brisbane at the Australian National Dental Conference (April 2011).
These regional consultations enabled FDI to establish political consensus and develop evidence based policy to support the GCI vision and its activities in advocacy and communication. From the outset the GCI sought to actively engage all stakeholders in a multi-stakeholder partnership optimised at a world level. This partnership included five leading global oral healthcare companies, who formed the GCI founding partners; Procter and Gamble (gold), Colgate Palmolive and Unilever (silver) and GlaxoSmithKline and WM Wrigley Jr Company (bronze).
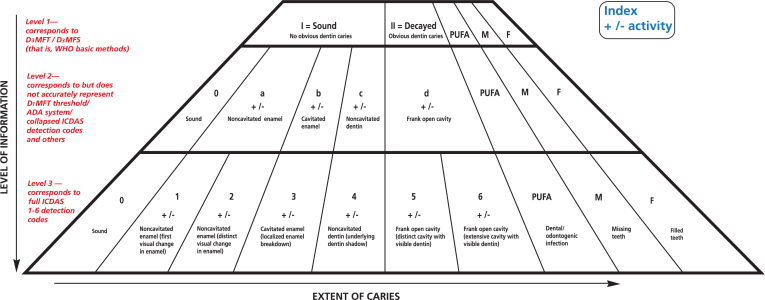
A key milestone was the development of the FDI Caries Matrix2 led by the FDI Science Committee. The Caries Matrix is the first step to integrating current science into dental practice, while recognising that it will need further development and refinement (Figure 1).
Figure 1.
FDI Caries Matrix under development by FDI Science Committee.
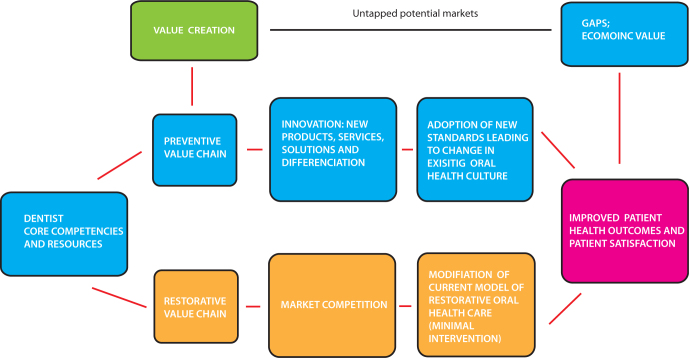
It is important to be clear that the vision of the GCI is not to move from a surgical and restorative model of care to a preventive one i.e. replacement. Rather it seeks to encompass appropriate restorative care within a prevention based model of oral health to expand value and contribute to health outcomes. Although technical developments around the FDI Caries Matrix and caries management pathways are important, consistent feedback has been the need to look at both the health and economic case with respect to moving to a prevention based model of oral health care.
GLOBAL CARIES INITIATIVE BUSINESS PLAN; ADDING VALUE TO HEALTH AND CONTRIBUTING TO DEVELOPMENT
The GCI business plan25 is founded on the principle of adding value to health and contributing to sustainable development.
The oral health care chain involves a series of complex partnerships and relationships. The GCI preventive health value chain works by optimising all preventive and restorative activities throughout the whole value chain to create bundles of innovative products, services and solutions, rather than focusing on maximising the interests of one player or component.
A major element of the qualitative aspect of this value chain is knowledge management and dissemination. The use of information technology to support relationships through co-ordinating and combining web based technologies and mobile applications will expand opportunities for patient centred care. Similarly, adopting a public health centred approach will add value to the preventive dental practice business model. For example practice based research networks, practice outreach programmes and services to the community will provide richer flow of information, ensure good communication and underpin the cost effective delivery of these innovative products, services and solutions.
The quantitative aspect uses a market/usage/dosage gap analysis to highlight how dental practitioners can implement a preventive dental practice business model to generate positive health outcomes without upsetting core competencies and existing revenue streams.
The GCI preventive health value chain aims to deliver improved patient health outcomes and satisfaction by creating additional value and modifying the approach to restorative care (Figure 2). Those who do not have necessary core competencies will need to invest in the additional step of value creation and model alignment before passing though the GCI preventive health value chain.
Figure 2.
The GCI Preventive health value chain.
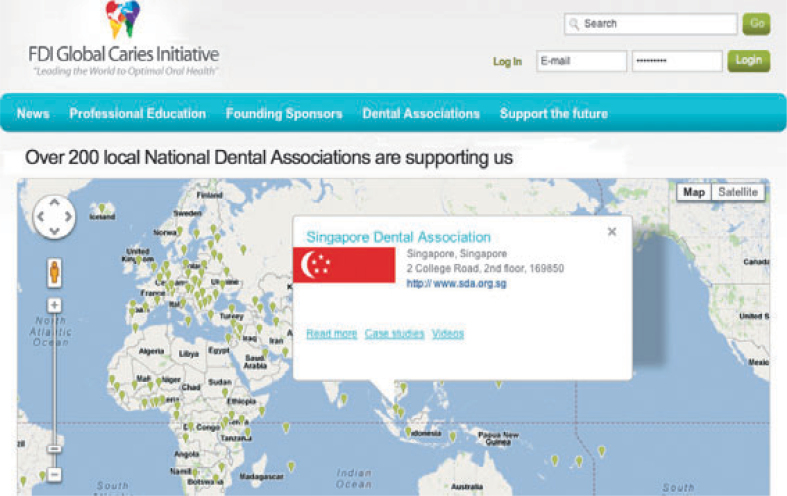
GCI website: mapping implementation
The dissemination and exchange of information and experiences are at the heart of the design of the GCI website26. The world map registering FDI’s membership of 130 national dental associations will create a communication and education matrix; associations to their individual members and between associations (Figure 3). Education around GCI will out of necessity be a learning continuum, in time building collaborative partnerships, mentoring opportunities and establishing practitioner and student exchange networks.
Figure 3.
NDA support worldwide.
GLOBAL CARIES INITIATIVE; DEVELOPMENTS AND CHALLENGES
The first phase of the GCI has established both a broad policy base in support of the new paradigm of caries management and developed instruments that will enable its implementation, including the FDI Caries Matrix. There has been significant progress in defining new pathways for caries management with the Caries Management Pathways (CMP) conference27 in June 2012, providing the foundation for future work.
However, in parallel to these efforts, there is a need to map the global policy landscape and assess how best to implement GCI within the current set of global health policy initiatives, taking into account their timelines and objectives.
As trusted health professionals it is our responsibility to deliver an effective, efficient and sustainable model of oral care based on the best available evidence, one that addresses health inequalities and improves health outcomes worldwide.
The success of the GCI depends on the leadership of individual dentists working with oral health care leaders around the world to implement the new model into national policy, public health care and daily general dental practice.
Acknowledgements
The authors are grateful for the contributions and support from the International Association for Dental Research, Dr A Alvi, Dr P Cooney, Dr J Cottrell, Dr C Fernandes, Dr S Hancocks, Prof. LJ Jin, Prof M Kambara, Prof. G Meyer, Dr D Meyer, Dr PE Petersen, Dr H-S Selikowitz, Prof. M Tyas, and Dr T Yücel.
REFERENCES
- 1.Black GV. Medico-Dental Publishing; Chicago: 1917. A Work on Operative Dentistry: The Technical Procedures in Filling Teeth. [Google Scholar]
- 2.Fisher J, Glick M. A new model for caries classification and management, FDI World Dental Federation Caries Matrix. JADA. 2012;143:546–551. doi: 10.14219/jada.archive.2012.0216. [DOI] [PubMed] [Google Scholar]
- 3.FDI World Dental Federation. Global Caries Initiative. http://www.fdiworldental.org/global-caries-initiative (Accessed 4th June, 2012)
- 4.FDI General Assembly resolution. The Principle of the Caries Classification and Management Matrix. http://www.fdiworldental.org/c/document_library/get_file?uuid=0b872daa-5d02-4d21-a408-fcef4205bd66&groupId=10157 (Accessed 4th June, 2012)
- 5.World Economic Forum. Global Risks 2011 Sixth Edition. An Initiative of the Risk Response Network. 2011. http://reports.weforum.org/global-risks-2011/ (Accessed June 4th, 2012)
- 6.World Economic Forum. The Global Economic Burden of Non-communicable Diseases. 2011. http://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf (Accessed 4th June, 2012)
- 7.United Nations. United Nations Political Declaration of the High-level Meeting of the General Assembly on the Prevention and Control of Non-communicable Diseases. 2011. http://www.un.org/ga/search/view_doc.asp?symbol=A/66/L.1 (Accessed 4th June, 2012)
- 8.World Health Organisaton Global Monitoring Framework. 2011. http://www.who.int/nmh/events/2011/consultation_dec_2011/WHO_Discussion_Paper_FINAL.pdf (Accessed 4th June, 2012)
- 9.World Health Organisaton. Commission on Social Determinants of Health 2005–2008. http://www.who.int/social_determinants/thecommission/en/ (Accessed 4th June, 2012)
- 10.World Health Organisaton. Healthy hospitals, healthy planet, healthy people: addressing climate change in healthcare settings. 2009. http://www.who.int/globalchange/publications/climatefootprint_report.pdf (Accessed 4th June, 2012)
- 11.United Nations Environmental Programme, World Health Organisation. The Health and Environment Linkages Initiatives. http://www.who.int/heli/en/ (Accessed 4th June, 2012)
- 12.United Nations Conference on Sustainable Development Rio + 20. 2012. http://www.uncsd2012.org/rio20/index.html (Accessed 4th June, 2012) [DOI] [PubMed]
- 13.Oxford University Press; 1987. World Commission on Environment and Development’s (the Brundtland Commission) report; Our Common Future. [Google Scholar]
- 14.Strategic Approach to International Chemicals Management. http://www.saicm.org/index.php?ql=h&content=home (Accessed 4th June, 2012)
- 15.Third International Conference on Chemicals Management. 2012. http://www.saicm.org/index.php?content=meeting&mid=147&def=1&menuid=50 (Accessed 4th June, 2012)
- 16.Third Latin America and Caribbean regional meeting on the Strategic Approach to International Chemicals Management. Draft Strategy for strengthening the engagement of the health sector in SAICM implementation. http://www.saicm.org/documents/meeting/grulac/Panama%202011/Meeting%20documents/LAC3_INF7_health%20strategy.pdf (Accessed 4th June, 2012)
- 17.United Nations Environmental Governing Council mandate part III of decision 25/5. 2009. http://www.unep.org/hazardoussubstances/Portals/9/Mercury/Documents/GC25Report_English_25_5.pdf (Accessed 4th June, 2012)
- 18.First session United Nations Environmental Programme Intergovernmental Negotiating Committee. 2010. http://www.unep.org/hazardoussubstances/Mercury/Negotiations/INC1/tabid/3324/Default.aspx (Accessed 4th June, 2012)
- 19.Vickers CM. Mercury and the Health Care Sector. 2010. http://www.unep.org/hazardoussubstances/Mercury/Negotiations/INC1/Technicalbriefingpresentations/tabid/4118/language/en-US/Default.aspx (Accessed 4th June, 2012)
- 20.Petersen PE. Future Use of Materials for Dental Restoration. World Health Organisation. 2009. http://www.who.int/oral_health/publications/dental_material_2011.pdf (Accessed 4th June, 2012)
- 21.FDI World Dental Federation General Assembly resolution on Dental Amalgam. 2010. http://www.fdiworldental.org/c/document_library/get_file?uuid=4e418f83-20ff-41eb-9d46-3c64b891bf30&groupId=10157 (Accessed 4th June, 2012)
- 22.World Health Organisation Transformational scale up of health professional education; an effort to increase the numbers of health professionals and strengthen their impact on population health. 2011. http://whqlibdoc.who.int/hq/2011/WHO_HSS_HRH_HEP2011.01_eng.pdf (Accessed 4th June, 2012)
- 23.Medical Education Partnership Initiative (MEPI). http://www.mepinetwork.org/ (Accessed 4th June, 2012)
- 24.Nursing Education Partnership Initiative (NEPI). http://www.pepfar.gov/initiatives/nepi/programs/index.htm (Accessed 4th June, 2012)
- 25.FDI Global Caries Initiative Business plan. 2010. http://www.fdiworldental.org/documents/10157/eaa2d8ad-70c4-4750-bca2-6d25f450fd34 (Accessed 4th June, 2012)
- 26.FDI Global Caries Initiative website. 2012. http://www.globalcariesinitiative.org/ (Accessed 4th June, 2012)
- 27.Caries Management Pathways, A Roadmap for Clinicians and Educators. An International Conference to Define a Common Language and New Pathways for Caries Management. Temple University Maurice H. Kornberg School of Dentistry. http://templecmp.org/ (Accessed 4th June, 2012)