Abstract
Objective: To evaluate the novel assessment of gingival contour volume measurement from digital impressions compared with traditional clinical indices (Modified Gingival Index and Bleeding Index) and oral microflora following a dental prophylaxis. Methods: Following baseline examinations and full mouth digital impression using the LAVA™ Oral Chairside Scanner (COS), subjects had one maxillary quadrant and the contra-lateral mandibular quadrant randomly allocated to receive a complete dental prophylaxis. Subjects then brushed twice daily at home using a standard toothpaste. After 1, 2, 4, 6 and 12 weeks gingivitis examinations and digital impressions of the maxillary and mandibular arches were taken. Results: Significant improvements in gingivitis for the prophylaxis versus no prophylaxis quadrants were observed up to six weeks using both the traditional gingivitis indices and the assessment of change in gingival contour volume from the digital impressions. Conclusion: The assessment of changes in gingival contour volume may be a promising technique for the objective and quantitative clinical evaluation of products or procedures used to treat gingivitis. The effects of a dental prophylaxis were demonstrated by both this novel measure and traditional clinical indices.
Key words: Digital impressions, gingival contour volume measurement
INTRODUCTION
Numerous gingival indices have been utilised over the years for the purpose of studying the relationship between plaque and gingivitis, conducting epidemiology studies and assessment of product efficacy1. These indices have been based on assessment of clinical features of gingivitis including oedema, colour, contour, bleeding and gingival crevicular fluid. The limitations of these indices are that they are not quantitative and rely on subjective assessment by a trained examiner using non linear numerical scales (i.e. where a score of 2 does not necessarily indicate twice the severity of a score of 1) and are subject to inter-examiner variability2. Bleeding indices are often considered to be more objective with greater clinical relevance than assessments of gingival appearance as a measure of gingivitis. However, even this measure has subjective elements which include the angle, depth and pressure applied during probing, all of which can influence the number of bleeding sites observed3.
Therefore, it is highly desirable to have an objective, quantitative technique for assessing gingival condition. Recently researchers have evaluated the use of imaging techniques to assess gingivitis4., 5., 6.. The major limitation of this technique is that it only includes the assessment of the facial surfaces of the anterior teeth. When compared to the entire mouth this accounts for only a small proportion of the sites which are treated, and does not allow for assessment of those areas of the mouth that have higher levels of disease, and are more difficult for the patient to clean to achieve changes in the gingival condition.
Rosin et al.7 investigated the suitability of measuring volume differences in gingival papillae for monitoring changes in the inflammatory status of the gingivae. This study demonstrated that a laser scanner could be used to provide reproducible measurements of papillary gingival oedema in an induced gingivitis model. The method used from both a clinical and laboratory perspective was quite simple but time consuming. Gingival oedema was measured on a number of test teeth by taking impressions and then obtaining replicas from the impressions. The replicas were then scanned with a 3-D laser scanner to assess volume changes. Rosin et al. found that there was an increase in volume during the induced gingivitis phase followed by a subsequent decrease in volume when a normal oral hygiene regime was resumed. High-precision scanners have also been used for three-dimensional measurements of wear of restorative materials8 and plaque9.
A potential source of error in the Rosin study is introduced during the preparation of the impression and replicas. The volume changes observed are relatively small therefore poor quality impressions could have a significant impact on the data.
The Lava™ Chairside Oral Scanner (COS) (3M) is a digital impression system that replaces traditional impression materials and utilises continuous 3D video images to create a digital impression. The COS ‘wand’ is a circular digital camera head containing an optical system comprised of multiple lenses and blue LED cells. The optical system can capture approximately 20, 3D data sets per second, or close to 2,400 data sets per arch, for an accurate and high speed scan. The processing algorithms use the 3-D coordinates of selected points from the video stream in real time to rebuild a 3-D image.
While primarily designed for in-office use, in this study it was used to investigate changes in the gingival contours over time. The teeth and gingivae were first scanned to create a digital impression, and the 3D co-ordinates from the digital impression were then transferred to specialised software to directly compare changes in gingival volume. Using this technique eliminated some of the potential error introduced in the Rosin study from the physical impressions which have changes in dimensions in both the negative (impression) replica of the arch and the positive replica (cast(s)). As compared to other techniques noted previously a significant benefit of creating digital impressions from the Lava™ Chairside Oral Scanner is that the all surfaces (anterior and posterior, facial and lingual surfaces) can be evaluated rather than only the facial surfaces of the anterior teeth as previously investigated using digital photography.
The objectives of this study were to evaluate the assessment of gingival contour volume from digital impressions compared with traditional clinical indices (Modified Gingival Index and Bleeding Index) and oral microflora following a dental prophylaxis.
MATERIALS AND METHODS
Clinical study design
This was a single examiner, single centre, exploratory, split-mouth, randomised, examiner blind (including laboratory measures) clinical study conducted at University Park Research Center, Indiana, USA using a prophylaxis model to establish changes in the gingival condition over time. The following were measured: Modified Gingival Index (MGI)10 and Bleeding Index (BI)11, Lava COS digital impressions to establish gingival contours and oral micro-flora following a dental prophylaxis over a 12 week period.
The study protocol and consent form were reviewed and approved by an Institutional Review Board. After providing written informed consent, 38 healthy adult subjects between the ages of 18–65 years were enrolled into the study if they had:
-
•
Good oral health with at least 20 natural teeth and mild to moderate gingivitis at baseline (mean whole mouth MGI score 1.50–2.50).
Subjects were excluded from the study if they:
-
•
Were pregnant or breast feeding
-
•
Were smokers
-
•
Had dental conditions requiring immediate treatment, sensitivity to oral care products, severe periodontitis or gingivitis, severe recession, partial dentures, orthodontic appliances or fixed retainers, restorations on surfaces where plaque would be collected from or oral or peri-oral ulceration including herpetic lesions.
Subjects were also screened for the use of any systemic medications which would have an effect on gingival conditions within 14 days of any gingivitis assessment.
A total of 38 subjects were randomised and 37 subjects completed the study (a subset of 21 subjects underwent plaque sampling for assessment of oral microflora).
At the screening visit, after written consent, subjects received an oral soft tissue examination (OST) and gross gingivitis examination. Subjects brushed at home with their own toothpaste and toothbrush between screening and baseline visits (1–7 days).
At the baseline visit subjects underwent an oral soft tissue examination, dental plaque sampling (for a sub-set of 21 subjects only), MGI and BI examinations. Each index had a single examiner throughout the study (two different examiners). A digital impression was taken of the maxillary and mandibular arches using the Lava™ COS (following MGI and prior to BI assessment). Subjects then had one maxillary quadrant and the contra-lateral mandibular quadrant randomly allocated to receive a complete dental prophylaxis. Subjects were provided with a standard toothpaste (Aquafresh® Advanced) and an Aquafresh® Clean Control toothbrush for twice daily use throughout the study.
After 1, 2, 4, 6 and 12 weeks subjects returned to the site to undergo a full OST examination, dental plaque sampling, MGI and BI examinations followed by a digital impression of the maxillary and mandibular arch taken using the LAVA™ COS. At the end of the study, all subjects received a complete professional prophylaxis.
Lava™ chairside oral scan of gingival contours
A digital impression of both arches was taken by a trained operator using the Lava™ COS system. The teeth and gums were coated with a thin layer of titanium dioxide to prevent high surface reflectivity prior to scanning. The digital impressions were evaluated using a specialised software (Geomagic Qualify, 3d Inspection/ comparison software, version 12) to measure gingival volumetric changes over time by analysing 3D coordinates from the scanned images. Data from the hard tissue (teeth) was used to align the images from the same subject at baseline and subsequent visits as any changes that occurred over this study time would be minimal. Indeed, from the comparison data this was the case with most teeth showing little or negligible deviations from baseline.
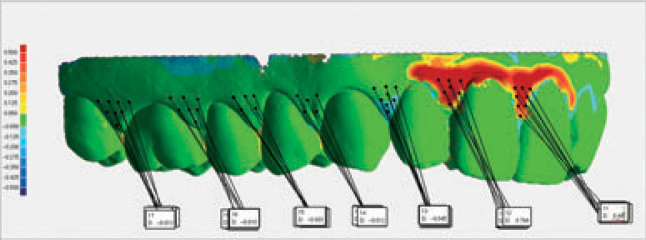
Once the hard tissue alignment was finalised, the difference between the superimposed baseline and each subsequent visit image was measured as the average deviation (d) in millimetres over a specific area around the gingival margin and papilla for each tooth (facial and lingual aspects). Average deviations were calculated over circular areas know as Bomb Radii (BR) so that error due to rogue points of scan data were minimised. Multiple BR were used to cover the entire region as illustrated in Figure 1.
Figure 1.
Example of bomb radii used to calculate gingival volume changes – each single black dot represents a bomb radii.
Modified Gingival Index
The MGI10 is a non-invasive evaluation of early visual changes in severity and extent of gingivitis. The MGI was assessed on the facial and lingual surfaces at two sites on each tooth (papillae and margin) by a single examiner. These assessments were performed on all evaluable teeth. The scoring of the MGI was performed under dental office conditions using a standard dental light for illuminating the oral cavity. The MGI scoring system was as follows:
0 = absence of inflammation
1 = mild inflammation; slight change in colour, little change in colour; little change in texture of any portion of the marginal or papillary gingival unit
2 = mild inflammation; criteria as above but involving the entire marginal or papillary gingival unit
3 = moderate inflammation; glazing, redness, oedema, and/or hypertrophy of the marginal or papillary gingival unit
4 = severe inflammation; marked redness, oedema and/or hypertrophy of the marginal or papillary gingival unit, spontaneous bleeding, congestion, or ulceration.
Bleeding Index
The Bleeding Index11 (modification to the index of Saxton) was performed by a single examiner using a colour coded periodontal probe. The probe was engaged approximately 1 mm into the gingival crevice. A moderate pressure was used whilst sweeping from interproximal to interproximal along the sulcular epithelium.
The BI scoring system was as follows:
0 = no bleeding after 30 seconds
1 = bleeding upon probing after 30 seconds
2 = immediate bleeding observed
Plaque sampling
Plaque samples were collected from the same test site at each visit. Immediately before dental plaque collection, the collection area was dried using a light stream of air. Dental plaque samples were collected from three teeth in each quadrant, on buccal and lingual/palatal surfaces, next to the gingival margin. The teeth to be sampled were: lateral incisor (alternatively central incisor), first premolar (alternatively second premolar) and first molar (alternatively second molar). Pooled plaque samples were collected from all tooth surfaces up to the interproximal sites (but not deep in the interproximal spaces) and up to the gingival margin (but above the gum line) using a stainless steel periodontal scaler (Gracey® 13/14).
The pooled plaque sample was transferred to a pre-weighed sterile cryovial containing 2.0 ml of reduced transport fluid (RTF)12 vortexed for 30 seconds and immediately placed in an ice-bath and transported to the microbiology laboratory for analysis. Samples in RTF were held in the ice bath for no greater than 4.5 hours prior to culturing.
Analysis of oral bacteria
Following receipt at the microbiology laboratory, the plaque sample in RTF was vortexed vigorously for 30 seconds followed by one-10 second burst of sonic energy and then immediately serially decimally diluted in RTF from 10−1 to 10−6 dilutions. All dilutions were spread plated in duplicate on pre-reduced Schaedler Anaerobic Blood Agar supplemented with haemin and menadione (SABA) (Difco) and Schaedler Blood Agar (SBA) (Difco). SABA was incubated anaerobically (85% nitrogen, 10% hydrogen, 5% carbon dioxide) at 37 °C for five days; SBA was incubated aerobically at 37 °C for two days. Bacterial colonies were counted after appropriate incubation. When no colonies were observed on a culture plate, a zero count was replaced by half the nominal limit of detection. Log10 aerobic and anaerobic bacterial counts per plaque sample were calculated.
Statistical methods
Gingival contour volume change
The volume changes for each Bomb Radius (BR) were calculated using the following equation:
The total volume change in a tooth site (papillae or margin) was calculated by summing all the volume changes for each BR at a tooth site. The treatment value was based on the average of the total volume change across all the tooth sites in the appropriate quadrants (one maxillary quadrant and the contra-lateral mandibular quadrant) for a subject. The total volume change in a tooth site was calculated, rather than the average, because there was the possibility of fitting in more or less BRs in a tooth site at different visits due to change in the inflammation of the gum tissue. Averaging BRs would lose the effect of the more or less BRs in a tooth site. The average across all sites in two quadrants for a treatment was taken as opposed to the total value due to the possibility of different numbers of teeth.
MGI and BI
The MGI and BI were calculated taking the average over all tooth sites in the two relevant quadrants per subject. The difference at the tooth site level between the visit and the baseline visit was calculated first and then averaged over the relevant quadrants to calculate change.
Teeth that were missing or not gradable were excluded from all calculations. The midline papillae was not included in the average scores as this site was shared between both treatments (prophylaxis and non- prophylaxis).
Oral bacteria
A single value was recorded for each treatment group to evaluate Total Anaerobes and Total Aerobes. Each bacterial count was log transformed (log10) prior to analysis and the change from pre- prophylaxis was the difference in the log values.
Analysis of variables
Results of the change from pre-prophylaxis at each time-point were compared using an analysis of covariance/variance (ANCOVA/ANOVA) with a factor for treatment (prophylaxis, no prophylaxis), subject (random effect) and a covariate for the pre-prophylaxis (baseline) level of the variable under analysis where appropriate.
The relationship between the MGI and change in gingival contour volume and bacterial counts was explored using correlation. The change in MGI and BI was tabulated against the summary of the change in gingival contour volume.
RESULTS
A total of 38 subjects were included in the intent to treat and safety populations. A summary of the gender and age of the population which completed the study are presented in Table 1.
Table 1.
Summary of age and gender of study population
| Number of Subjects | Age | ||||
|---|---|---|---|---|---|
| Male | Female | Total | Mean | Range | |
| Population* | 18 | 20 | 38 | 37.1 | 20–60 |
Plaque samples were collected from a subset of 21 subjects only
Comparison of change in gingival contours and volume
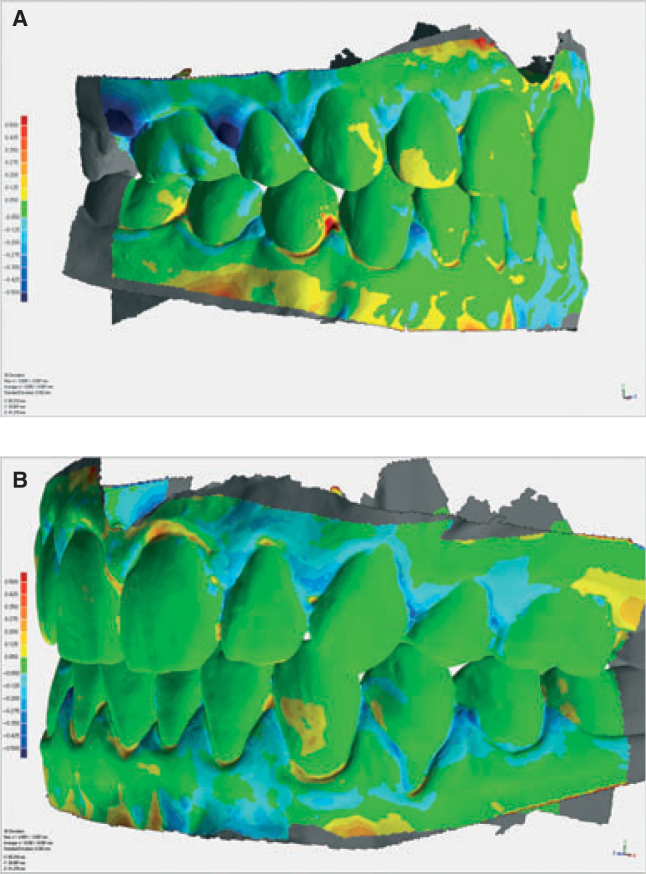
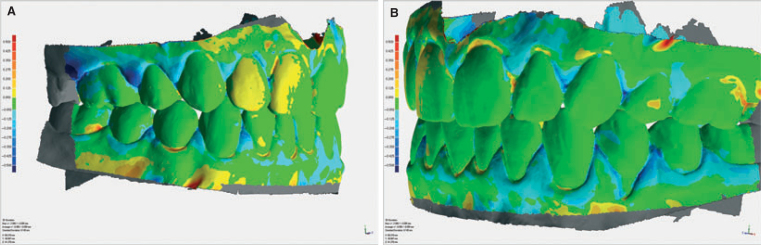
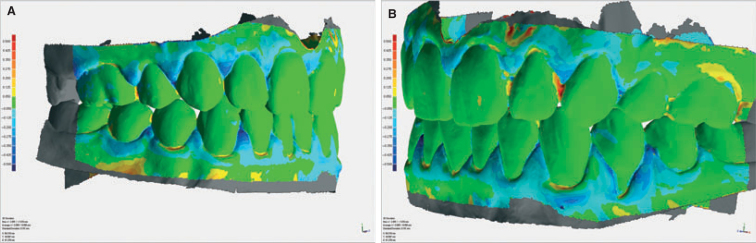
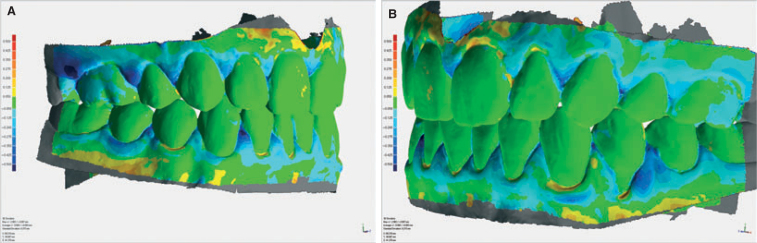
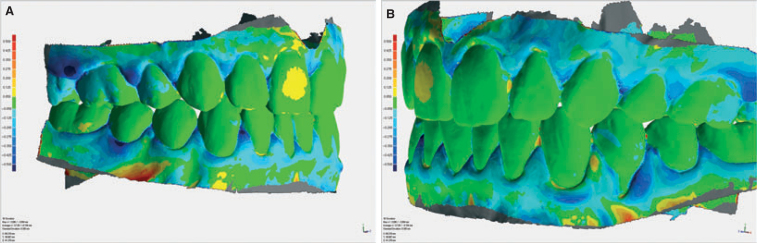
Images of example changes in gingival contour scans from baseline for each visit for one subject (subject 10) are provided in Figure 2., Figure 3., Figure 4., Figure 5., Figure 6.. This subject underwent a prophylaxis in the upper right and lower left quadrants at baseline. The change in contour volume from baseline is represented by colour changes on the image where green indicates no change from baseline, red represents an increase in volume and blue a decrease from baseline.
Figure 2.
Change in contour volume from baseline for Subject 10, week 1 (a) right side, upper prophylaxis, (b) left side, lower prophylaxis.
Figure 3.
Change in contour volume from baseline for Subject 10, week 2 (a) right side, upper prophylaxis, (b) left side, lower prophylaxis.
Figure 4.
Change in contour volume from baseline for Subject 10, week 4 (a) right side, upper prophylaxis, (b) left side, lower prophylaxis.
Figure 5.
Change in contour volume from baseline for Subject 6, week 6 (a) right side, upper prophylaxis, (b) left side, lower prophylaxis.
Figure 6.
Change in contour volume for Subject 6 week 12 (a) right side, upper prophylaxis, (b) left side, lower prophylaxis.
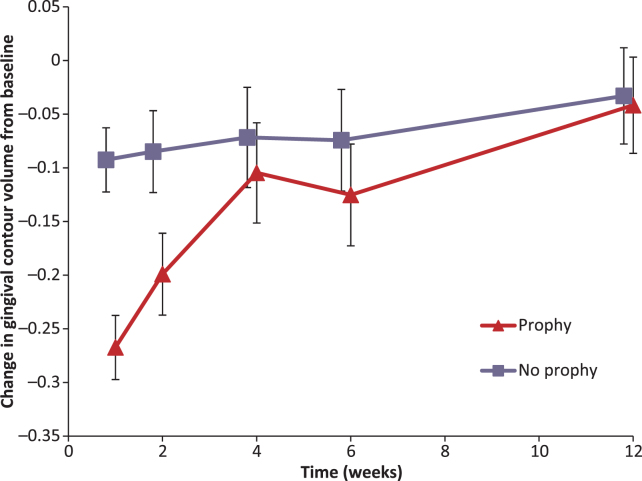
The numerical results of the gingival contour change from baseline are presented in Tables 2 and 5 and Figure 7. A greater reduction in contour volume was observed in the arches which underwent dental prophylaxis as compared to those sites which did not receive a prophylaxis, This difference was statistically significant at weeks 1, 2 and 6. There was also a small non significant reduction in gingival contour volume for the sites which did not receive a prophylaxis compared to baseline.
Table 2.
Summary of change from baseline gingival contour volume over time
| Timepoint | N | Prophylaxis | No Prophylaxis | ||
|---|---|---|---|---|---|
| Mean Change from baseline ± SD | P-value* | Mean Change from baseline ± SD | P-value* | ||
| Week 1 | 38 | −0.27 ± 0.18 | <0.0001 | −0.09 ± 0.19 | 0.0032 |
| Week 2 | 38 | −0.20 ± 0.23 | <0.0001 | −0.08 ± 0.24 | 0.0307 |
| Week 4 | 37 | −0.10 ± 0.30 | 0.0304 | −0.07 ± 0.27 | 0.1324 |
| Week 6 | 37 | −0.13 ± 0.29 | 0.0117 | −0.07 ± 0.29 | 0.1248 |
| Week 12 | 37 | −0.04 ± 0.26 | 0.3588 | −0.03 ± 0.28 | 0.4667 |
P-value from adjusted mean.
Figure 7.
Change in gingival contour volume from baseline over time.
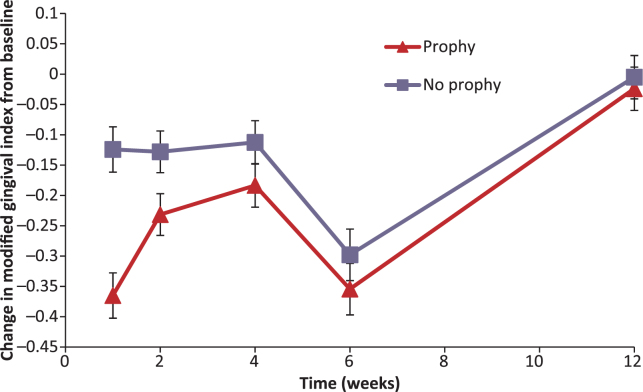
Comparison of mean Modified Gingival Index scores
The results of the Modified Gingival Index are presented in Tables 3 and 5 and Figure 8. A greater reduction in MGI was observed in the arches which underwent dental prophylaxis as compared to those sites which did not receive a prophylaxis. This difference was statistically significant at weeks 1, 2, 4 and 6. There was also a small reduction in MGI for the sites which did not receive a prophylaxis compared to baseline (except at week 12).
Table 3.
Summary of mean and change from baseline Modified Gingival Index over time
| Timepoint | N | Prophylaxis | No Prophylaxis | ||||
|---|---|---|---|---|---|---|---|
| Mean MGI ± SD | Mean Change from baseline MGI ± SD | P-value* | Mean MGI ± SD | Mean Change from baseline MGI ± SD | P-value* | ||
| Baseline | 38 | 2.00 ± 0.26 | 2.03 ± 0.29 | ||||
| Week 1 | 38 | 1.63 ± 0.38 | −0.36 ± 0.26 | <0.0001 | 1.91 ± 0.33 | −0.12 ± 0.19 | 0.0014 |
| Week 2 | 38 | 1.76 ± 0.32 | −0.23 ± 0.19 | <0.0001 | 1.91 ± 0.39 | −0.13 ± 0.23 | 0.0004 |
| Week 4 | 37 | 1.82 ± 0.33 | −0.18 ± 0.24 | <0.0001 | 1.93 ± 0.35 | −0.11 ± 0.19 | 0.0028 |
| Week 6 | 37 | 1.65 ± 0.36 | −0.35 ± 0.25 | <0.0001 | 1.74 ± 0.43 | −0.30 ± 0.26 | <0.0001 |
| Week 12 | 37 | 1.98 ± 0.34 | −0.02 ± 0.23 | 0.5050 | 2.03 ± 0.33 | −0.01 ± 0.18 | 0.8896 |
P-value from adjusted mean.
Table 5.
Summary of mean differences from baseline in gingival contour, Modified Gingival Index and Bleeding Index between prophylaxis and no prophylaxis
| Variable | Time (week) | Change from baseline | 95% Confidence Interval | P-value | |||
|---|---|---|---|---|---|---|---|
| Prophylaxis | No Prophylaxis | Difference | Lower | Upper | |||
| Gingival Contour (mm3) | 1 | −0.27 | −0.09 | −0.17 | −0.23 | −0.12 | <0.0001 |
| 2 | −0.20 | −0.08 | −0.11 | −0.17 | −0.06 | 0.0003 | |
| 4 | −0.10 | −0.07 | −0.03 | −0.09 | 0.02 | 0.2224 | |
| 6 | −0.13 | −0.07 | −0.05 | −0.10 | −0.01 | 0.0299 | |
| 12 | −0.04 | −0.03 | −0.01 | −0.06 | 0.04 | 0.7415 | |
| Modified Gingival Index | 1 | −0.37 | −0.12 | −0.24 | −0.34 | −0.14 | <0.0001 |
| 2 | −0.23 | −0.13 | −0.10 | −0.17 | −0.03 | 0.0053 | |
| 4 | −0.18 | −0.11 | −0.07 | −0.13 | −0.01 | 0.0270 | |
| 6 | −0.35 | −0.30 | −0.06 | −0.11 | 0.00 | 0.0392 | |
| 12 | −0.02 | 0.00 | −0.02 | −0.06 | 0.02 | 0.3110 | |
| Bleeding Index | 1 | −0.17 | −0.07 | −0.10 | −0.14 | −0.06 | <0.0001 |
| 2 | −0.09 | 0.00 | −0.09 | −0.16 | −0.02 | 0.0111 | |
| 4 | 0.01 | 0.09 | −0.09 | −0.15 | −0.03 | 0.0050 | |
| 6 | −0.04 | 0.02 | −0.05 | −0.11 | 0.00 | 0.0666 | |
| 12 | 0.08 | 0.12 | −0.04 | −0.09 | 0.01 | 0.0986 | |
Prophylaxis and No Prophylaxis means are adjusted means from ANOVA/ANCOVA.
Difference is prophylaxis minus no prophylaxis. A negative difference favours prophylaxis.
Figure 8.
Change in Modified Gingival Index from baseline over time.
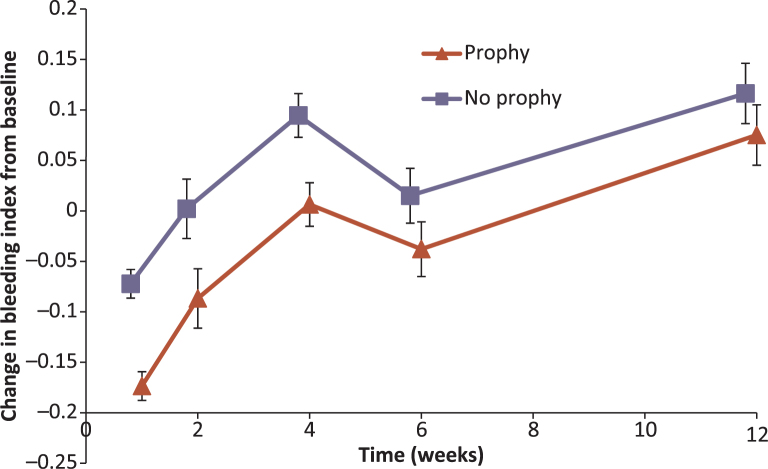
Comparison of Bleeding Index scores
The results of the Bleeding Index are presented in Tables 4 and 5 and Figure 9. A greater reduction in BI was observed in the arches which underwent dental prophylaxis as compared to those sites which did not receive a prophylaxis. This difference was statistically significant at weeks 1, 2 and 4.
Table 4.
Summary of mean and change from baseline Bleeding Index over time
| Timepoint | N | Prophylaxis | No Prophylaxis | ||||
|---|---|---|---|---|---|---|---|
| Mean BI ± SD | Mean Change from baseline BI ± SD | P-value* | Mean BI ± SD | Mean Change from baseline BI ± SD | P-value* | ||
| Baseline | 38 | 0.32 ± 0.25 | 0.31 ± 0.20 | ||||
| Week 1 | 38 | 0.14 ± 0.13 | −0.17 ± 0.16 | <0.0001 | 0.24 ± 0.18 | −0.07 ± 0.09 | <0.0001 |
| Week 2 | 38 | 0.23 ± 0.17 | −0.09 ± 0.18 | 0.0045 | 0.31 ± 0.29 | 0.00 ± 0.20 | 0.9441 |
| Week 4 | 37 | 0.33 ± 0.18 | 0.00 ± 0.15 | 0.7700 | 0.41 ± 0.19 | 0.10 ± 0.17 | <0.0001 |
| Week 6 | 37 | 0.28 ± 0.19 | −0.04 ± 0.19 | 0.1679 | 0.33 ± 0.24 | 0.02 ± 0.17 | 0.5813 |
| Week 12 | 37 | 0.40 ± 0.24 | 0.07 ± 0.16 | 0.0156 | 0.43 ± 0.27 | 0.12 ± 0.20 | 0.0003 |
P-value from adjusted mean.
Figure 9.
Change in Bleeding Index from baseline over time.
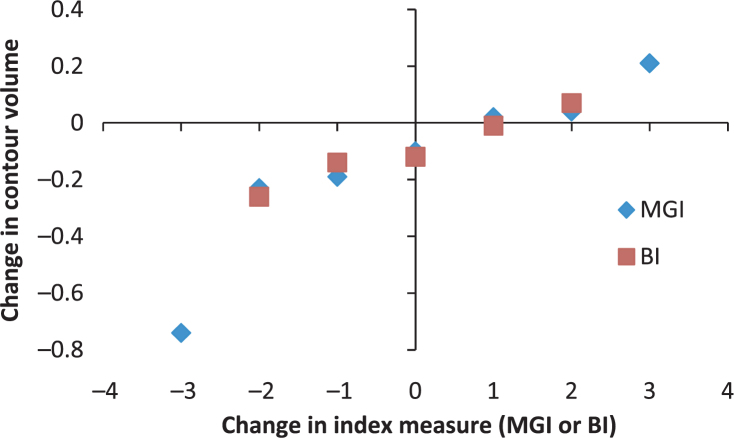
Relationship between gingival contours and traditional indices
The relationships between variables are depicted in Table 6 and Figure 10. There was some correlation in change in gingival contour volume against the change in MGI (ρ = 0.36) and BI (ρ = 0.33). In general there is a corresponding increase in gingival contour volume with an increase in MGI and BI.
Table 6.
Summary of relationship between change in gingival contour volume and change in MGI and BI
| Change in index score (MGI or BI) | Mean change in contour volume in relation to: | |
|---|---|---|
| MGI | BI | |
| −3 | −0.74 | |
| −2 | −0.23 | −0.26 |
| −1 | −0.19 | −0.14 |
| 0 | −0.10 | −0.12 |
| 1 | 0.02 | −0.01 |
| 2 | 0.04 | 0.07 |
| 3 | 0.21 | |
| Correlation | 0.36 | 0.33 |
Figure 10.
Plot of change in MGI or BI relative to change in contour volume.
Evaluation of oral microflora
The results of the mean log10 bacterial counts from the plaque samples are presented in Table 7. There were some statistically significant reductions in Total Aerobe and Total Anaerobes in both the prophylaxis and non prophylaxis groups, there were no statistically significant differences between the prophylaxis and non prophylaxis groups.
Table 7.
Summary of mean bacterial counts over time
| Measurement | Treatment | Summary of Bacterial Counts (mean log10 ± SD) | |||||
|---|---|---|---|---|---|---|---|
| Baseline (N = 21) | Week 1 (N = 21) | Week 2 (N = 21) | Week 4 (N = 20) | Week 6 (N = 20) | Week 12 (N = 20) | ||
| Mean Total Anaerobes (log10)* | Prophylaxis | 7.47 ± 0.512 | 7.11 ± 0.824† | 6.98 ± 0.633† | 7.37 ± 0.748 | 7.85 ± 0.965 | 7.14 ± 0.446† |
| Non Prophylaxis | 7.56 ± 0.514 | 7.27 ± 0.664 | 7.02 ± 0.375† | 7.49 ± 0.639 | 7.73 ± 0.748 | 7.21 ± 0.338† | |
| Mean Total Aerobes (log10)* | Prophylaxis | 7.04 ± 0.482 | 6.81 ± 0.487 | 6.67 ± 0.495† | 6.87 ± 0.468† | 8.28 ± 1.497† | 6.68 ± 0.474† |
| Non Prophylaxis | 7.16 ± 0.434 | 7.05 ± 0.957 | 6.68 ± 0.391† | 7.07 ± 0.590 | 8.31 ± 1.409† | 6.60 ± 0.517† | |
Plaque samples were collected from a subset of 21 subjects only
Statistically significant reduction from baseline (p < 0.05)
There were no statistically significant differences (p < 0.05) between prophylaxis and no prophylaxis
DISCUSSION
The improvement in gingival health for the areas which underwent a dental prophylaxis was evident from both the traditional gingivitis indices (MGI and BI) and from the change in gingival contour volume up to six weeks following dental prophylaxis. The effect of the prophylaxis was no longer observed after 12 weeks in either the examiner assessments or the gingival contour assessment. The areas which did not undergo a dental prophylaxis also showed significant reductions from baseline at some timepoints, this may have been due to the effect of timed twice daily brushing required by the clinical study protocol.
The 6-week data for the examiner based indices were out of trend with the other timepoints in the study, there was a greater improvement in gingival health for both the prophylaxis and the non prophylaxis areas than observed at the 4-week timepoint. This anomaly was not observed for the gingival contour volume assessment. This was observed for both the MGI and the BI indices which were assessed separately by different examiners and therefore is likely to be a real phenomenon. The objective measure of gingival contour volume did not display the same trend however this measurement did not take into account colour, texture or bleeding and therefore this may be a limitation of the technique. The anomalous results of the 6-week data may also have had an influence on the overall correlation between the MGI and BI with the gingival contour measurements. There was a trend of an increase in change of index score as the contour volume changes (Table 6 and Figure 10).
The results of the change in gingival contour volume suggest that this technique may have future value for assessment of gingivitis in clinical studies. The benefits of this technique are that it is quantitative and does not rely on examiner interpretation of a non-linear index. This technique enables assessment of the entire mouth unlike previously reported techniques in digital photography which are significantly limited by access to only facial surfaces of the anterior teeth. Potential drawbacks of this technique are that it requires specialised equipment and software and the scanning process and data analysis is time consuming. In order to assess the subjects’ condition other parameters such as colour, texture and bleeding should be included.
CONCLUSION
This exploratory study shows that the assessment of gingival contour volume may be a promising technique for the objective and quantitative clinical evaluation of changes in gingival conditions due to treatment. The effects of a dental prophylaxis were demonstrated by both this novel measure and traditional clinical indices.
CONFLICT OF INTEREST AND SOURCE OF FUNDING
The work described in this manuscript was funded by GlaxoSmithKline Consumer Healthcare. The authors external to GSK received no additional fee for the preparation of this manuscript. The remaining authors are employed by GSK but confirm no potential conflicts of interest.
REFERENCES
- 1.Ciancio S. Current status of indices of gingivitis. J Clin Periodontol. 1986;13:375–378. doi: 10.1111/j.1600-051x.1986.tb01476.x. [DOI] [PubMed] [Google Scholar]
- 2.McClanahan SF, Bartizek RD, Biesbrock AR. Identification and consequences of distinct Loe-Sillness gingival index examiner styles for the clinical assessment of gingivitis. J Periodontol. 2001;73:383–392. doi: 10.1902/jop.2001.72.3.383. [DOI] [PubMed] [Google Scholar]
- 3.Newburn E. Indices to measure gingival bleeding. J Periodontol. 1996;67:555–561. doi: 10.1902/jop.1996.67.6.555. [DOI] [PubMed] [Google Scholar]
- 4.Smith RN, Lath DL, Rawlinson A, et al. Gingival inflammation assessment by image analysis: measurement and validation. Int J Dent Hygiene. 2008;6:137–142. doi: 10.1111/j.1601-5037.2008.00294.x. [DOI] [PubMed] [Google Scholar]
- 5.Biesbrock AR, Rubush ME, Dunavent JM et al. Evaluating gingivitis image analysis and Laser Doppler imaging. IADR/AADR/CADR 87th General Session and Exhibition, Miami, April 1-4, 2009 Abstract 1355
- 6.Biesbrock AR, Gibb R, Rubush ME et al. Concurrent clinical and image analysis assessment of gingivitis natural history. IADR 88th General Session, Barcelona, July 14-17, 2010 Abstract 4742
- 7.Rosin M, Splieth C, Hesser M, et al. Quantification of gingival edema using a new 3-D laser scanning method. J Clin Periodontol. 2002;29:240–246. doi: 10.1034/j.1600-051x.2002.290310.x. [DOI] [PubMed] [Google Scholar]
- 8.Mehl A, Gloger W, Kunzelmann K, et al. A New Optical 3-D Device for the Detection of Wear. J Dent Res. 1997;76:1799–1807. doi: 10.1177/00220345970760111201. [DOI] [PubMed] [Google Scholar]
- 9.Yeganeh S, Lynch E, Jovanovski V, et al. Quantification of root surface plaque using a new 3-D laser scanning method. J Clin Periodontol. 1999;26:692–697. doi: 10.1034/j.1600-051x.1999.261009.x. [DOI] [PubMed] [Google Scholar]
- 10.Lobene RR. A Modified Gingival Index for Use in Clinical Trials. Clin Prev Dent. 1986;8:3. [PubMed] [Google Scholar]
- 11.Saxton C, Van der Ouderara FGJ. The Effect of a Dentifrice Containing Zinc Citrate & Triclosan on Developing Gingivitis. J Periodont Res. 1989;24:75. doi: 10.1111/j.1600-0765.1989.tb00860.x. [DOI] [PubMed] [Google Scholar]
- 12.Syed SA, Loesche WJ. Survival of human dental plaque flora in various transport media. Appl Microbiol. 1972;24:638–644. doi: 10.1128/am.24.4.638-644.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]