Abstract
Objectives: To analyse dental caries-related quality of life (QoL) in adolescent (15–19-year-old) subjects in a suburban area (SA) and a downtown area (DA) of Bauru, São Paulo, Brazil, in 2009. Methods: This was a cross-sectional, randomised study. The sample consisted of 185 and 147 adolescents from the SA and DA, respectively. The caries index used was that for decayed, missing and filled teeth (DMFT) (World Health Organization criteria). The 14-item Oral Health Impact Profile (OHIP-14) was used to assess QoL. The non-parametric Mann–Whitney test, Spearman’s correlation coefficient and chi-squared test were used in the statistical analysis. Results: The DMFT index, Significant Caries (SiC) Index and percentage of caries-free students were similar (P > 0.05) between these populations, but findings on the Care Index differed (P < 0.05). There was a correlation between the DMFT index and OHIP-14 score in SA subjects (mean DMFT index = 3.01) in the dimensions of physical pain (r = 0.25; P < 0.01) and psychological disability (r = 0.17; P = 0.02). The DMFT index in DA subjects (mean DMFT index = 2.95) showed a correlation with functional limitation (r = 0.19; P = 0.02). The correlation in SA subjects between the caries component (mean = 1.22) of the DMFT index and OHIP-14 was significant only for the physical pain dimension (r = 0.16; P = 0.03). In DA subjects, correlations between the caries component (mean = 0.37) and all dimensions of OHIP-14 were statistically significant (P < 0.05). Conclusions: Despite the similarities in means in the DMFT index, the SiC Index and the caries-free percentage of subjects in both localities, access to dental treatment proved to be less effective for SA adolescents. Physical pain and psychological disability were the most frequent negative manifestations of impact on QoL. The SA adolescents were more negatively affected by dental caries in terms of QoL.
Key words: Dental caries, quality of life, oral epidemiology, dental public health
INTRODUCTION
The World Health Organization (WHO) definition of health1, presented in the preamble to its constitution of 1948, signalled a major step towards the enhancement of the quality of life (QoL) of individuals and populations around the world. Health was no longer considered an isolated and tightly defined concept: its definition included not only the absence of disease or illness, but a state of complete physical, mental and social well-being. This was an obvious inclusion of the incipient concept of QoL. In 1973, the PubMed and MEDLINE databases contained only five papers that included the term ‘quality of life’ in their keyword lists2. By March 2011, that number had risen to 159,402, and included 33,937 literature reviews. This new concept has been refined considerably over time in a process that has included the development of measures for the evaluation of physical, mental and social well-being related to QoL in individuals and populations. It has been discussed in the literature with reference to various age groups, including children3., 4., adolescents5., 6., adults7., 8. and the elderly population9., 10., and for specific treatments11., 12.. Its development is becoming easier to apply in research, even when the discussion refers to standards of validity, sensitivity and reliability13.
In 1980, in order to classify the effects of disease on the daily lives of individuals and populations in terms of parameters such as pain, discomfort, disability, physical disability, psychological and social effects, the WHO published the ‘International Classification of Impairments, Disabilities and Handicaps’ (ICIDH)14. Under this classification, disability is a characteristic caused by disease or congenital malformation or by another cause of harm to health. Disability causes the subject to have an eminently personal and disadvantageous relationship to the social context. According to the WHO, there is a logical consequence of a disease or disorder in the health–disease process, which causes a deficiency, a disability and, finally, a social disadvantage.
In 1989, Locker15 proposed an improved model of the ICIDH, which included, in addition to the original variables, death, pain and discomfort and functional limitation. This model is more dynamic and does not present a continuous line of evolution between the variables. According to Locker, the line of reasoning in the classification of impairment, disability and handicap is not complete. He argues that pain and discomfort can be consequences of disability, and can themselves cause physical disability, and psychological or social disadvantage, and that this outcome represents the maximum degree of consequence of a disturbance in the health–illness process15.
In 1994, Slade and Spencer16 presented the Oral Health Impact Profile (OHIP), which comprises 49 items on perceptions of oral health as it relates to QoL. Seven dimensions described by Locker15 in 1989 represented the basis for the formulation of questions: functional limitation; physical pain; psychological discomfort; physical disability; psychological disability; social disability, and handicap. In 1997, Slade17 described the notion that these dimensions can be ordered in a hierarchy according to their impact on QoL and people’s daily lives. The first dimension, functional limitation, relates to the individual’s own problems, as well as to physical pain and psychological discomfort. The dimensions relating to physical, psychological and social disability refer to the impact of oral health on daily life. Finally, the dimension of disadvantage represents the extent of the disadvantage caused by the oral health condition. Slade17 also reported that OHIP-49 may be used by dimension or generically. Oral health problems, such as tooth loss, dental caries, periodontal attachment loss and dental care problems have been shown to have increasing levels of impact on the welfare of people10., 18..
The OHIP questionnaire is intended to capture the impact of oral health conditions on QoL. However, in its complete form, some research may present implementation difficulties. Some population groups, such as groups that do not use artificial dentures, do not permit the use of the full battery of questions, and other contexts may impose time constraints on field research, such as in health services research. For these reasons, in 1997 Slade17 proposed a short version of the questionnaire, using 14 questions, two for each dimension.
In 2006, Pires et al.19 translated into Portuguese and culturally adjusted and validated the OHIP questionnaire in its full version for use with 60 elderly subjects. The questionnaire presented in this research used the 14 questions of the short version of the OHIP (OHIP-14), which were translated, validated and culturally adapted into Portuguese.
Despite the important and well-documented decline in prevalences of dental caries in children and adolescents in Brazil since the 1980s20, as well as in other industrialised and developing countries, incidences of caries in the interstices between 12-year-old children and adolescents aged 15–19 years are significant in Brazil, as observed in the national surveys of 200321 and 201022. However, little has been published regarding the oral health status of adolescents23 and their perceptions about it.
This cross-sectional, randomised study aimed to investigate the impact of tooth decay on the QoL of adolescents aged 15–19 years in a central district and in a district on the outskirts of the city of Bauru, São Paulo, Brazil.
METHODS
Ethical aspects
This paper was submitted for consideration and approved by the Ethics Committee of the Bauru Dental School, University of São Paulo (process no. 132/2008), in accordance with resolution 196/96 of the Brazilian National Health Board. This research was conducted in full accordance with the World Medical Association Declaration of Helsinki. All participants or their legal guardians signed informed consent before participating in any part of the research.
Population
The city of Bauru is located in the midwest of the Brazilian state of São Paulo and has 347,601 inhabitants24. The public water supply has been fluoridated since 197525 and fluoride levels in the water have been externally controlled since 200426.
Study design
A district on the outskirts of Bauru and a district in the city centre were selected to participate in this research. First, one area was randomly selected from each peripheral region of the city (north, south, east and west). The neighbourhood of Parque Santa Edwirges was selected from among the four areas previously identified. This neighbourhood includes two state-run public schools attended by students aged 15–19 years, the Vereador Antônio Ferreira de Menezes School and the Parque Santa Edwirges School. These two schools took part in this research. The city centre neighbourhood selected to represent the downtown area (DA) was Jardim Estoril, where the only school to include students aged 15–19 years is the state-run Professor Christino Cabral School. All of the 442 adolescent students enrolled in the suburban area (SA) schools and all of the 398 students enrolled in the DA school were invited to participate in the study. Thus, a total of 840 students were invited to participate in the research. Of these, 185 students in the SA schools and 147 students in the DA school met the inclusion criteria.
Inclusion criteria
The inclusion criteria adopted for this research required all subjects to be aged 15–19 years at 31 December 2009, to be enrolled in a participating public school, and to submit informed consent signed by the participant or by his or her legal guardian if the student was a minor aged < 18 years, as required by Brazilian law.
Examinations
Participating adolescents were examined by one calibrated examiner (kappa statistic = 0.98) in order to ensure uniform interpretation, understanding, reproducibility and application of WHO criteria. Examinations were performed in an outdoor setting using natural light, with the examiner and the adolescent sitting in chairs. The examiner used a dental mirror and a Community Periodontal Index (CPI) ballpoint probe.
For evaluation of dental caries, the WHO criteria for decayed, missing and filled teeth (DMFT) were used. These data provide the information needed to calculate the Significant Caries (SiC) Index, as well as the Care Index. The polarisation of dental caries was analysed according to the percentage of caries-free adolescents.
Impact on QoL
To assess the impact of oral health on the adolescent’s QoL, the OHIP-14 was used to evaluate the experiences of the subject in the 12 months prior to the dental caries epidemiological examination. The dimensions assessed by this questionnaire were functional limitations, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. Two questions applied to each dimension. Response codes were: 0 = never; 1 = rarely; 2 = sometimes; 3 = often, and 4 = always. Because the total maximum score could range from 0 to 28, total scores were classified as indicating no impact (0), low impact (0 < OHIP-14 ≤ 9), medium impact (9 < OHIP-14 ≤ 18) and strong impact (18 < OHIP-14 ≤ 28).
Statistical analysis
The Mann–Whitney test and chi-squared test were used to compare findings in the two populations on the DMFT index and its components, the SiC Index27 and Care Index. Spearman’s correlation coefficient was used to estimate the correlations between the DMFT and its components, the caries-free percentage and the SiC Index, and the OHIP-14. All statistical procedures adopted a significance level of 0.05 and tests were performed using statistica Version 9.1 (StatSoft, Inc., Tulsa, OK, USA).
RESULTS
Voluntary participants
The decision to study an adolescent age group (15–19 years) reflected a historic choice influenced by findings in epidemiological surveys of oral health conditions in Brazil. In all schools, students from eighth grade through to the third year of high school, who met the criteria for inclusion in the survey, were invited to participate. Numbers of students, by category of age, are listed in Table 1. Most SA volunteers were aged 15–16 years. A more uniform distribution was found in the DA participants. However, both groups included a small sample of students aged 19 years. In general, the age group comprising the highest percentage of the sample consisted of students aged 15–17 years, which is characteristic of the Brazilian high school population. The presence of a dichotomy between White and non-White students drew particular attention. The first group constituted 50.81% of the SA sample and included mostly females. In the DA sample, the vast majority of students were White (78.91%) and the gender distribution of the sample was evenly balanced. In the total sample, the ethnic group most represented was White and female participants outnumbered male (Table 1).
Table 1.
Sample distribution according to age, sex, locality and ethnic group
| Suburban area group | Downtown area group | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male, n | Female, n | Total, n | % | Male, n | Female, n | Total, n | % | Male, n | Female, n | Total, n | % | |
| Age, years | ||||||||||||
| 15 | 36 | 52 | 88 | 47.57 | 8 | 20 | 28 | 19.05 | 44 | 72 | 116 | 34.94 |
| 16 | 18 | 38 | 56 | 30.27 | 29 | 22 | 51 | 34.69 | 47 | 60 | 107 | 32.23 |
| 17 | 12 | 18 | 30 | 16.22 | 22 | 29 | 51 | 34.69 | 34 | 47 | 81 | 24.40 |
| 18 | 1 | 8 | 9 | 4.86 | 11 | 5 | 16 | 10.88 | 12 | 13 | 25 | 7.53 |
| 19 | 0 | 2 | 2 | 1.08 | 1 | 0 | 1 | 0.68 | 1 | 2 | 3 | 0.90 |
| Total | 67 | 118 | 185 | 55.72 | 70 | 76 | 147 | 44.28 | 137 | 194 | 332 | 100 |
| Ethnic group | ||||||||||||
| I | 0 | 2 | 2 | 1.08 | 0 | 0 | 0 | 0.00 | 0 | 2 | 2 | 0.60 |
| II | 33 | 61 | 94 | 50.81 | 54 | 62 | 116 | 78.91 | 87 | 123 | 210 | 63.25 |
| III | 17 | 23 | 40 | 21.62 | 8 | 8 | 16 | 10.88 | 25 | 31 | 56 | 16.87 |
| IV | 17 | 32 | 49 | 26.49 | 9 | 6 | 15 | 10.20 | 26 | 38 | 64 | 19.28 |
| Total | 67 | 118 | 185 | 55.72 | 70 | 76 | 147 | 44.28 | 137 | 194 | 332 | 100 |
I, subjects of East Asian descent; II, subjects of White European descent; III, subjects of African descent; IV, subjects of White European and African descent.
Dental caries epidemiology
Dental caries were studied using the DMFT index (WHO criteria). Table 2 presents descriptive statistics for this index and its components, the percentage of caries-free students and the Care Index. The SA adolescents presented a mean ± standard deviation (SD) DMFT index of 3.01 ± 2.99, and mean ± SD indices for decayed and filled teeth of 1.22 ± 1.63 and 1.67 ± 2.63, respectively. In the DA group, the mean ± SD DMFT index was 2.95 ± 3.09 and the mean ± SD index for filled teeth was 2.52 ± 2.93. The mean ± SD DMFT index in the entire study sample was 2.98 ± 2.35. Findings on the SiC Index, introduced by Bratthall27 in 2000, were similar between the two populations, at 6.73 ± 2.73 in the DA group and 6.84 ± 2.00 in the SA group, and represented the average of the upper third of the DMFT index. The Care Index was lower in the SA group (39.01%) than in the DA group (62.84%). The percentage of caries-free participants did not statistically differ between the groups (P = 0.52), at 29.73% in the SA group and 26.53% in the DA group.
Table 2.
Distribution of mean findings on the index for decayed, missing and filled teeth (DMFT) and its components, the Significant Caries (SiC) Index, the caries-free percentage and the Care Index (%) in Brazilian adolescents, by neighbourhood of Bauru, São Paulo, in 2009
| DT (SD) | DFT (SD) | FT (SD) | MT (SD) | DMFT (SD) | SiC Index (SD)* | Caries -free, % | Care Index, %† | |
|---|---|---|---|---|---|---|---|---|
| SA | 1.22 (1.63) | 0.08 (0.40) | 1.67 (2.63) | 0.05 (0.24) | 3.01 (2.99) | 6.84 (2.00) | 29.73 | 44.49 |
| DA | 0.37 (0.82) | 0.05 (0.27) | 2.52 (2.93) | 0.01 (0.12) | 2.95 (3.09) | 6.73 (2.73) | 26.53 | 81.74 |
| P-value | < 0.01‡ | 0.51‡ | < 0.01‡ | 0.12‡ | 0.84‡ | 0.82‡ | 0.52§ | < 0.01 |
SiC Index = mean DMFT (1/3 higher).
Care Index (%) = (FT/DMFT) × 100, DMFT > 0.
Mann–Whitney test.
Chi-squared test.
P-values in bold are significant at P < 0.01.
DT, decayed teeth; DFT, decayed filled teeth; MT, missing teeth; SD, standard deviation; SA, suburban area group; DA, downtown area group.
Dental caries related to QoL
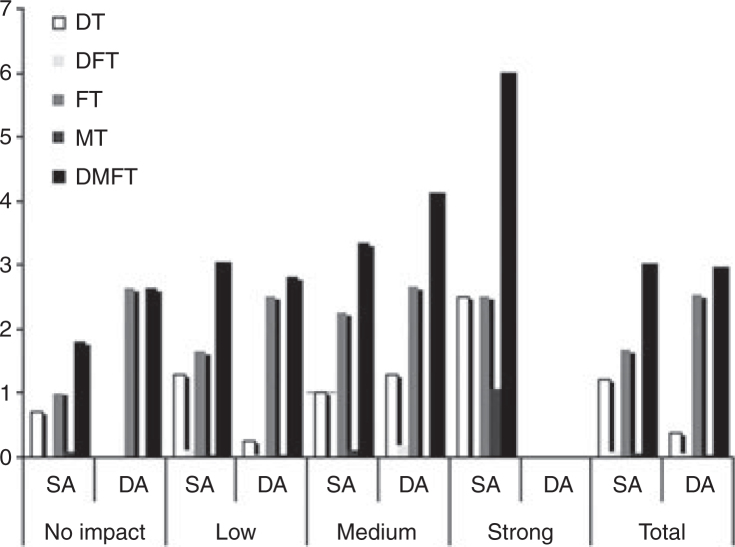
In this study, the negative impact on QoL measured by the assessment instrument OHIP-14 generally tended to increase as the DMFT index increased (Figure 1).
Figure 1.
Incidences of dental caries components in Brazilian adolescents in Bauru, by neighbourhood and impact types, in 2009. SA, suburban area group; DA, downtown area group; DT, decayed teeth; DFT, decayed filled teeth; FT, filled teeth; MT, missing teeth; DMFT, decayed, missing and filled teeth.
Table 3 shows the correlation between the DMFT index and its components, as well as the SiC Index and each dimension assessed in OHIP-14.
Table 3.
Correlations of mean findings on the index for decayed, missing and filled teeth (DMFT) and its components with findings on the 14-item Oral Health Impact Profile (OHIP-14) using Spearman’s correlation coefficient (r), by dimension, in Brazilian adolescents in Bauru, São Paulo, by neighbourhood, in 2009
| OHIP-14 dimensions, r | ||||||||
|---|---|---|---|---|---|---|---|---|
| Functional limitation | Physical pain | Psychological discomfort | Physical disability | Psychological disability | Social disability | Handicap | OHIP-14 | |
| Decayed teeth | ||||||||
| SA | 0.02 | 0.16* | −0.01 | −0.03 | 0.10 | −0.01 | 0.00 | 0.04 |
| DA | 0.28* | 0.31* | 0.24* | 0.20* | 0.23* | 0.22* | 0.27* | 0.31* |
| Decayed filled teeth | ||||||||
| SA | 0.04 | −0.01 | 0.04 | −0.04 | −0.10 | −0.04 | −0.03 | −0.02 |
| DA | 0.07 | 0.04 | 0.10 | 0.01 | 0.02 | 0.13 | 0.11 | 0.06 |
| Filled teeth | ||||||||
| SA | 0.12 | 0.15* | 0.15* | 0.06 | 0.15* | 0.02 | 0.05 | 0.18* |
| DA | 0.11 | −0.04 | −0.05 | 0.01 | 0.01 | 0.00 | 0.00 | 0.01 |
| Missing teeth | ||||||||
| SA | 0.09 | 0.16* | 0.04 | 0.13 | 0.12 | 0.02 | 0.12 | 0.09 |
| DA | 0.03 | 0.08 | −0.06 | 0.13 | 0.14 | −0.10 | −0.06 | 0.05 |
| Decayed, missing and filled teeth | ||||||||
| SA | 0.09 | 0.25* | 0.10 | 0.03 | 0.17* | −0.01 | 0.05 | 0.16* |
| DA | 0.19* | 0.04 | 0.00 | 0.03 | 0.06 | 0.08 | 0.07 | 0.07 |
P < 0.05.
SD, standard deviation; SA, suburban area group; DA, downtown area group.
DISCUSSION
Instruments of oral health-related QoL were developed in order to quantify the extent to which oral health problems interfere in daily life and the well-being of people and to assess the impact of oral health on physical and psychosocial development. Adolescence represents a period of life during which particular characteristics are associated with the social and psychological needs of people in this age group, but the impacts of health and disease-related problems on QoL in this age group have not been much researched28. Adolescents, as well as children and adults, are affected by many oral health problems, which may potentially compromise their well-being and QoL29. Dental caries, like other diseases that affect human beings, have a positive association with increasing age.
The DMFT index was similar between the two populations, as was the SiC Index and the percentage of caries-free adolescents (P > 0.05). However, the prevalences of decayed teeth (DT) in the SA group (P < 0.01) and filled teeth (FT) in the DA group (P < 0.01) were higher, as evidenced by the respective Care Indices of these populations (P < 0.01). These data clearly show that access to dental services was higher among DA adolescents because these students were of higher socioeconomic status (P < 0.01). The respective findings on the Care Index show a disparity in access to oral health care between the two populations; such a disparity can be avoided and is unfair28.
The present study found the dental caries component (DT) at low levels to have no negative impact on QoL. In addition, restorative treatment (indicated by FT) was so effective that the FT index was able to represent the DMFT in the DA group, although this group demonstrated a higher incidence of dental caries. This result shows the impact of the lack of required dental care and is evidence of the lower rates of care provided in schools in the city outskirts compared with those in the city centre. Thus, the impact was greater in subjects with untreated dental caries (in the DA group), recurrent caries in FT or caries on another surface of a filled tooth (DFT), or teeth that had been extracted as a result of caries [missing teeth (MT)]. For MT, respondents reported a short period of pain and discomfort caused by the need for extraction or the empty space left by the extraction. It is important to remember that students completing the OHIP-14 questionnaire were instructed to report their feelings over the year prior to the examination. The epidemiological differences observed were strongly related to access to dental services in the respective groups. Assessment of the impact of tooth decay on QoL showed that when the need for dental care for tooth decay is met, any negative impact on QoL becomes irrelevant. Similar DMFT indices emerged in both groups of adolescents, but the FT component in the DA group resulted in the absence of any strong impact on QoL. However, this was not true in SA adolescents because their needs, represented by the FT index, had not been met. These findings also imply that sensations of pain can significantly affect QoL in adolescents.
An evaluation of the correlations between the dimensions of the OHIP-14 and the dependent variables of the DMFT index and its components shows that the impact of tooth decay on QoL was manifested differently in the two groups (Table 3). Although the DT component of the DMFT index was lower in the DA group, its impact on QoL was statistically significant in all dimensions of the OHIP-14 (P < 0.05). This did not occur in the SA group, except with reference to the physical pain dimension. The FT component was shown to be less representative in the SA than in the DA group; however, the degree of virulence of dental caries, as represented by deeper cavities and thus greater postoperative pain, may impact on the physical pain dimension (r = 0.15; P = 0.04).
The second important aspect of findings in this research refers to the psychological issues related to the presence of restorations, which were evident in the dimensions of psychological discomfort and psychological disability (Table 3). In this aspect, data for the DA group on the FT component in the DMFT index were more significant (Table 2). However, this study did not investigate the quality of restoration in terms of its form, the type of restorative material used and its relation to the aesthetics of the smile. Mean scores for perceptions of the aesthetic appeal of teeth [the upper anterior teeth (canines and central and lateral incisors)] were 0.20 in the DA group and 0.07 in the SA group, which are unimpressive in view of the prevalences of FT in these groups (2.52 and 1.67, respectively). It would not be reasonable to consider that the aesthetic appeal of inadequate restorations in anterior and upper teeth would counteract the negative impact of the fillings on the dimensions of psychological discomfort and psychological disability. However, we suspect that the quality of restoration, in general, may have influenced these correlations of negative impact, especially in terms of a significant negative impact on QoL in the SA group (OHIP-14, r = 0.18; P = 0.02). The MT component of the DMFT index is obviously closely related to episodes of severe pain caused by decay. This component was more strongly represented in the SA group; although its value was low (SA group MT = 0.05), it was five times more prevalent in the SA than the DA group and its impact on QoL was statistically more significant for participants in the SA group (Table 2).
Adolescents in the city centre (DA group) reported a greater impact of the DT component in terms of the functional limitation dimension, which may reflect characteristics of social life in the community in which they live. However, the DMFT index in this group did not differ statistically from that in the SA group (Table 2) and did not impact negatively on QoL in other dimensions.
In the SA group, the composition of the DMFT index was shared by components related to pain (DT and MT; Table 2). Table 3 shows the trend for increasing physical pain and dental caries in the SA group. The physical pain and psychological disability caused by dental caries and, more specifically, the pain caused by decay and by extractions, contributed to this significant difference in the dimensions of physical pain and psychological disability in the overall impact observed on the OHIP-14 (Table 3). The trend towards a negative impact of the DMFT index on QoL (OHIP-14) was significant in the SA group, especially with regard to the greater need for dental care in this group than in the DA group.
The SiC Index27 is intended to identify the worst one-third of DMFT index distribution. This calculation is important to establish variability in mean DMFT indices30, as well as percentages of caries-free individuals. However, the SiC Index, as well as its predecessor, the DMFT index, is incapable of identifying the depth of dental caries lesions. Its only objective is to establish the third worst percentage. This index assesses only the presence of caries and does not assess the progression of caries in a tooth. For the purpose of this particular research, the International Caries Detection Assessment System (ICDAS)31., 32. is a proper assessment. The SiC Index was higher and statistically significant only for the physical pain dimension in the SA group (Mann–Whitney test, P < 0.01). It might also be expected to be significant in the DA group; however, despite the general negative impact of the DT component among DA adolescents and the similar SiC Indices in both groups (Table 2), only in the SA group did the SiC Index show significance. Both the DMFT and the SiC Index focus on the overall condition of a tooth and not on dental caries lesion progression. These results may be explained by the lesser access of SA students to dental health care, as indicated by differences in the DT and FT components of the DMFT data (Table 2). This lack of care would result in deepening dental caries lesions in SA adolescents, despite the similarities in the DMFT data and SiC Index between the groups.
The DMFT index represents the intensity of the attack of dental caries and its relation to the care needs of a population. Correlating this important index with a QoL indicator can help policymakers to better understand how to create dental policy plans that are specifically designed to meet people’s needs rather than to fulfil the normative criteria of dentists. In this research, it is important to note that the impacts of tooth decay on the QoL of adolescents in a central and a suburban area of the same city differ. Thus, the actions required of policymakers also differ and must take into account the intrinsic biological factors related to results on the DMFT index and the abstract factors related to QoL in these different populations.
Traditional methods of oral health evaluation focus on clinical parameters in the absence or presence of disease. Such tests only evaluate conditions based on the judgement of clinical professionals (normative assessment) and do not consider psychosocial consequences, information about the welfare of the subjects, their feelings about their oral health or their ability to chew.6 Thus, measures of QoL have been developed to help assess the psychosocial impact of oral health on people’s lives in addition to the normative assessment. These measures aim to quantify the extent to which oral health problems interfere in daily life and well-being to provide data that can complement the results of clinical studies29. Because assessing changes in the QoL of individuals requires the subjects of study to use a measure of self-awareness, including this concept in new programmes that are cost-effective in terms of both human and financial resources is challenging.
CONCLUSIONS
Despite the similarities in mean DMFT and SiC Index data and in the percentage of caries-free individuals in both groups in this study, dental treatment proved to be less accessible to adolescents in the SA group. The physical pain and psychological disability dimensions bore the most frequent negative impact of dental caries on QoL (OHIP-14). Adolescents in the SA group were more negatively affected by dental caries in terms of QoL. Further research on oral health conditions in relation to QoL, including biological variables, is required to improve community dentistry assessment, planning and attendance.
Acknowledgements
The authors wish to thank the directors of the participating schools, their teachers and staff, and the study participants and their parents and guardians. Without such cooperation, this research could not have been accomplished. We also acknowledge the financial support of Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil.
Conflicts of interest
None declared.
REFERENCES
- 1.World Health Organization . WHO; New York, NY: 1946. Constitution of the World Health Organization. [Google Scholar]
- 2.Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–840. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 3.Gherunpong S, Tsakos G, Sheiham A. Developing and evaluating an oral health-related quality of life index for children: the CHILD-OIDP. Community Dent Health. 2004;21:161–169. [PubMed] [Google Scholar]
- 4.Kolawole KA, Otuyemi OD, Oluwadaisi AM. Assessment of oral health-related quality of life in Nigerian children using the Child Perceptions Questionnaire (CPQ 11-14) Eur J Paediatr Dent. 2011;12:55–59. [PubMed] [Google Scholar]
- 5.Thelen DS, Bårdsen A, Astrøm AN. Applicability of an Albanian version of the OIDP in an adolescent population. Int J Paediatr Dent. 2011;21:289–298. doi: 10.1111/j.1365-263X.2011.01122.x. [DOI] [PubMed] [Google Scholar]
- 6.Peres KG, Peres MA, Araujo CL, et al. Social and dental status along the life course and oral health impacts in adolescents: a population-based birth cohort. Health Qual Life Outcomes. 2009;7:95. doi: 10.1186/1477-7525-7-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leao A, Sheiham A. The development of a socio-dental measure of dental impacts on daily living. Community Dent Health. 1996;13:22–26. [PubMed] [Google Scholar]
- 8.Bernabe E, Marcenes W. Periodontal disease and quality of life in British adults. J Clin Periodontol. 2010;37:968–972. doi: 10.1111/j.1600-051X.2010.01627.x. [DOI] [PubMed] [Google Scholar]
- 9.Atchison KA, Dolan TA. Development of the geriatric oral health assessment index. J Dent Educ. 1990;54:680–687. [PubMed] [Google Scholar]
- 10.Slade GD, Spencer AJ. Social impact of oral conditions among older adults. Aust Dent J. 1994;39:358–364. doi: 10.1111/j.1834-7819.1994.tb03106.x. [DOI] [PubMed] [Google Scholar]
- 11.Brook PH, Shaw WC. The development of an index of orthodontic treatment priority. Eur J Orthod. 1989;11:309–320. doi: 10.1093/oxfordjournals.ejo.a035999. [DOI] [PubMed] [Google Scholar]
- 12.Locker D, Jokovic A, Tompson B, et al. Is the Child Perceptions Questionnaire for 11–14-year-olds sensitive to clinical and self-perceived variations in orthodontic status? Community Dent Oral Epidemiol. 2007;35:179–185. doi: 10.1111/j.1600-0528.2006.00324.x. [DOI] [PubMed] [Google Scholar]
- 13.Locker D, Allen F. What do measures of ‘oral health-related quality of life’ measure? Community Dent Oral Epidemiol. 2007;35:401–411. doi: 10.1111/j.1600-0528.2007.00418.x. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . WHO; Geneva: 1980. International Classification of Impairment, Disabilities and Handicaps. [Google Scholar]
- 15.Locker D. Tavistock; London: 1989. An Introduction to Behavioural Sciences and Dentistry; p. 259. [Google Scholar]
- 16.Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 17.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–290. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 18.Hunt RJ, Slade GD, Strauss RP. Differences between racial groups in the impact of oral disorders among older adults in North Carolina. J Public Health Dent. 1995;55:205–209. doi: 10.1111/j.1752-7325.1995.tb02371.x. [DOI] [PubMed] [Google Scholar]
- 19.Pires CP, Ferraz MB, de Abreu MH. Translation into Brazilian Portuguese, cultural adaptation and validation of the Oral Health Impact Profile (OHIP-49) Braz Oral Res. 2006;20:263–268. doi: 10.1590/s1806-83242006000300015. [DOI] [PubMed] [Google Scholar]
- 20.Ministry of Health (Ministério da Saúde) MoH; Brasilia: 1988. Secretaria Nacional de Programas Especiais de Saúde. Divisão Nacional de Saúde Bucal. Fundação de Serviços de Saúde Pública. Levantamento Epidemiológico em Saúde Bucal: Brasil, Zona Urbana. 1986. [Google Scholar]
- 21.Ministry of Health (Ministério da Saúde) MoH; Brasilia: 2004. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Coordenação Nacional de Atenção à Saúde Bucal. Projeto SB Brasil 2003: Condições de Saúde Bucal da População Brasileira 2002–2003: Resultados Principais. [Google Scholar]
- 22.Roncalli AG. [The SB Brazil 2010 Project: a key strategy for developing an oral health surveillance model] Cad Saude Publica. 2010;26:429. doi: 10.1590/s0102-311x2010000300001. [DOI] [PubMed] [Google Scholar]
- 23.Pattussi MP, Olinto MT, Hardy R, et al. Clinical, social and psychosocial factors associated with self-rated oral health in Brazilian adolescents. Community Dent Oral Epidemiol. 2007;35:377–386. doi: 10.1111/j.1600-0528.2006.00339.x. [DOI] [PubMed] [Google Scholar]
- 24.Instituto Brasileiro de Geografia e Estatística (IBGE) Ministério do Planejamento, Orçamento e Gestão; Rio de Janeiro: 2007. Contagem da População 2007. [Google Scholar]
- 25.da Silva Bastos R, Olympio KP, Bijella VT, et al. Trends in dental caries prevalence in 12-year-old schoolchildren between 1976 and 2001 in Bauru, Brazil. Public Health. 2005;119:269–275. doi: 10.1016/j.puhe.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 26.Ramires I, Maia LP, Rigolizzo DoS, et al. [External control over the fluoridation of the public water supply in Bauru, SP, Brazil] Rev Saude Publica. 2006;40:883–889. doi: 10.1590/s0034-89102006000600019. [DOI] [PubMed] [Google Scholar]
- 27.Bratthall D. Introducing the Significant Caries Index together with a proposal for a new global oral health goal for 12-year-olds. Int Dent J. 2000;50:378–384. doi: 10.1111/j.1875-595x.2000.tb00572.x. [DOI] [PubMed] [Google Scholar]
- 28.Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22:429–445. doi: 10.2190/986L-LHQ6-2VTE-YRRN. [DOI] [PubMed] [Google Scholar]
- 29.Barbosa TS, Gavião MB. Oral health-related quality of life in children: part II. Effects of clinical oral health status. A systematic review. Int J Dent Hyg. 2008;6:100–107. doi: 10.1111/j.1601-5037.2008.00293.x. [DOI] [PubMed] [Google Scholar]
- 30.Mapengo MA, Marsicano JA, Garcia de Moura P, et al. Dental caries in adolescents from public schools in Maputo, Mozambique. Int Dent J. 2010;60:273–281. [PubMed] [Google Scholar]
- 31.Mendes FM, Braga MM, Oliveira LB, et al. Discriminant validity of the International Caries Detection and Assessment System (ICDAS) and comparability with World Health Organization criteria in a cross-sectional study. Community Dent Oral Epidemiol. 2010;38:398–407. doi: 10.1111/j.1600-0528.2010.00557.x. [DOI] [PubMed] [Google Scholar]
- 32.Ormond C, Douglas G, Pitts N. The use of the International Caries Detection and Assessment System (ICDAS) in a National Health Service general dental practice as part of an oral health assessment. Prim Dent Care. 2010;17:153–159. doi: 10.1308/135576110792936177. [DOI] [PubMed] [Google Scholar]