Abstract
Objective: This study aimed to evaluate the progression of sealed non-cavitated dentinal occlusal caries in a randomised controlled clinical trial. Materials and methods: Sixty teeth with non-cavitated dentinal occlusal caries were selected in patients with a high risk for caries. Patients were randomly divided into two groups so that each group included 30 teeth. Patients in the experiment group were given oral hygiene instructions and a fissure sealant. Patients in the control group were given oral hygiene instructions only. Caries progression and sealant loss were monitored over a period of 36 months by clinical and radiographic examinations. Results: Clinical and radiographic progression of caries was significantly more frequent in the control group than in the experiment group. Three teeth lost their sealant and showed caries progression, but this was apparent only at the 12-month follow-up. At the 24- and 36-month recall appointments, neither sealant loss nor caries progression were observed. Conclusion: The pit and fissure sealant utilised in this study was shown to be effective in arresting carious lesions at 36 months.
Key words: Dental caries, dentine, prevention
INTRODUCTION
In restorative dentistry, the treatment of carious lesions has been reviewed many times. Minimally invasive dentistry, the goal of which is to preserve the greatest amount possible of tooth structure, is intended to replace conventional procedures1. When an open cavity is diagnosed, the option of restoration tends to be unquestionable. However, it should be noted that caries involving dentine may be present in non-cavitated lesions and that there may be a layer of intact enamel2.
Given the lack of evidence indicating that dentinal caries can be arrested, some investigators have recommended more invasive treatment to manage non-cavitated dentinal lesions3., 4.. By contrast, other researchers5., 6. have demonstrated that non-surgical interventions are capable of arresting cavitated dentinal caries. Recently, a 12-month follow-up clinical trial7 showed that the sealing of pits and fissures halted the progression of non-cavitated dentinal occlusal caries. Although such short-term results7 highlighted the possibility of treating non-cavitated dentinal occlusal caries using a non-surgical approach, longterm follow-up investigations remain scarce in the literature. For this reason, this study aimed to investigate the clinical and radiographic outcomes of sealing non-cavitated dentinal occlusal caries over a period of 36 months.
MATERIALS AND METHODS
This randomised controlled clinical trial was approved by the ethics committee of the Federal University of Rio Grande do Norte (Natal, RN, Brazil) (protocol no. 121/05) and was conducted in full accordance with the World Medical Association’s Declaration of Helsinki. Before enrolling patients in the trial, informed consent was obtained by asking prospective patients to read and sign a form containing all information regarding the risks and benefits entailed in the treatment.
Study population
This 36-month randomised controlled clinical trial was conducted according to the criteria defined in the CONSORT statement. All procedures were conducted in the city of Natal (RN, Brazil), which is devoid of a fluoridated water supply. Patients with high risk for caries8 who attended the National Health Service (Federal University of Rio Grande do Norte) for dental care were selected.
Over a period of 3 months (intake period), 60 (n = 30 per group) molars in 35 individuals (10–22 years of age) were selected. A sample size of 30 per research treatment is recognised as adequate to afford levels of variability that enable a pertinent conclusion9., 10.. The criterion for inclusion was the presence of visually non-cavitated lesions between the enamel–dentine junction and the middle one-third of dentine. Exclusion criteria were the presence of restorations and white spot lesions or cavitations on other tooth surfaces. Teeth with reported sensitivity to any type of stimulus were also excluded. All visual and radiographic examinations were performed by one calibrated operator.
Each eligible tooth was assigned a number; these numbers were noted on individual pieces of paper which were subsequently put into a sealed opaque envelope. An external examiner withdrew one paper at a time and allocated 30 teeth to each group. Patients in the experiment group received: (i) instructions on oral hygiene, and (ii) an opaque pit-and-fissure sealant. The control group received oral hygiene instructions only. Background and demographic variables of subjects are displayed in Table 1.
Table 1.
Demographic data for the subjects included in this study
| Variables | Experiment group (n = 30 teeth) |
Control group (n = 30 teeth) |
|---|---|---|
| Age, years, median (IQ range) | 16 (12.0–19.5) | 13 (12.0–15.0) |
| Gender, n (%) | ||
| Male | 16 (51.6) | 15 (48.4) |
| Female | 14 (48.3) | 15 (51.7) |
| Tooth position, n (%) | ||
| Lower | 22 (56.4) | 17 (43.6) |
| Upper | 8 (38.1) | 13 (61.9) |
| Occlusion, n (%) | ||
| Contact with antagonist tooth | 3 (100) | 0 |
| Infraocclusion | 27 (47.4) | 30 (52.6) |
IQ range, interquartile (25th–75th) range.
Examiner calibration
Before the study began, one blinded examiner was calibrated to analyse the radiographs. During the calibration process, 104 radiographs obtained in a previous study were used; 52 of these were baseline radiographs and 52 were taken at follow-up at 1 year. The examiner paired the radiographs and evaluated them blindly in a dark room using a negatoscope, a 2× magnifying glass (Maped do Brasil Ltda, São Paulo, SP, Brazil), and a millimetre ruler (Prisma Instrumentos Odontológicos, São Paulo, SP, Brazil). Another person took note of outcomes of increase, decrease or no change in the radiolucent area (occlusoapical and/or mesiodistal directions, in mm). After 15 days, the same examiner re-evaluated 39.1% of the radiographs to determine intra-examiner agreement (kappa coefficient: 0.9).
Clinical procedures (experiment and control groups)
To confirm the absence of clinically visible cavitation on the occlusal surfaces, one operator carried out a prophylaxis with pumice and water, as well as a clinical examination with a flat mirror (SS White Duflex, Rio de Janeiro, RJ, Brazil), triplex syringe and headlight (Gnatus Equipamentos Médico-Odontológicos Ltda, Araraquara, SP, Brazil). In order to standardise the bitewing radiographs, silicone bite records and a positioner (Indusbello, Londrina, PR, Brazil) were utilised. On all occasions, the same X-ray source [Timex 70C mobile column (exposure time: 0.64 seconds); Gnatus Equipamentos Médico-Odontológicos Ltda] was used to expose Kodak E-Speed films (Eastman Kodak Co., New York, NY, USA). The films were manually processed in Kodak developing and fixative solutions using the following temperature and time protocol: 2 minutes in the developing solution and 4 minutes in the fixative solution at a temperature of 26 °C.
All patients received oral hygiene instructions that included the Fones technique11 for daily tooth brushing and the use of dental floss after meals. In addition, the operator recorded all possible fluoride sources used.
Clinical procedures (experiment group)
After placement of a rubber dam (Indústria e Comércio de Artefatos de Látex, São José dos Campos, SP, Brazil), a prophylaxis was carried out with a Robison brush containing pumice and water (Microdont, São Paulo, SP, Brazil). The occlusal surface was etched with 37% phosphoric acid for 30 seconds, washed for 1 minute with an air/water spray, and dried with an air stream immediately thereafter. The next step consisted of applying a fluoride-releasing, resin-based sealant (Dentsply/Caulk, Milford, DE, USA) with a dental probe (SS White Duflex) in order to secure a better flow of the material throughout the pits and fissures. The sealant was photoactivated for 20 seconds with a light-curing device (Optilight LD MAX; Gnatus Equipamentos Médico-Odontológicos Ltda), which gives a radiance of 600 mW/cm2), and checked for complete sealant coverage by visual inspection with the aid of a dental probe. Occlusal contacts were examined with an articulating paper and any premature contact was eliminated.
Observation periods
The experiment8 and control groups were followed up at intervals of 4 months over a period of 1 year to allow intervention in the event of caries progression. After 8 months, caries progression was observed in the control group either by clinical or by radiographic examination. Because these teeth had to be restored, they were not included in the subsequent follow-ups. After 1 year, the experiment group was assessed at intervals of 12 months up to 36 months. At each time-point, the same operator collected a dental history and also performed both clinical and radiographic examinations. Patients were asked to report the presence of any sensitivity to any type of stimulus and to report on the use of fluoride during the time preceding the appointment. Clinical examination consisted of an evaluation of the presence of visible cavitation and (in the experiment group only) of the marginal integrity of the sealant. Full retention, partial retention and complete loss were the expected outcomes.
One experienced and calibrated examiner evaluated the radiographs at 12, 24 and 36 months. Clinical progression was defined by the presence of visible cavitation and/or sensitivity during follow-up. To assess radiographic progression, baseline radiographs were compared with control radiographs using a negatoscope and a magnifying glass. Caries progression was defined as an increase in the size of lesions in any of the directions considered (occlusoapical and mesiodistal). Caries arrest was defined by the occurrence of either no change or a reduction in one or both dimensional planes at 12, 24 and 36 months.
Sealant was replaced whenever loss of material was observed in the absence of caries progression. In both groups, restorations with composite resin (Filtek P-60; 3M ESPE Division, St Paul, MN, USA) were carried out in the presence of any sign of caries progression (tooth sensitivity, occurrence of visible cavitation, increase in the radiolucent area).
Statistical analysis
Data were entered into a Windows Microsoft Excel 2007 datasheet and analysed using BioEstat Version 5.0 (Sociedade Civil Mamiraruá, Belém, PA, Brazil) to generate descriptive statistics and Fisher’s exact tests to draw comparisons. A level of significance of 5% was considered.
RESULTS
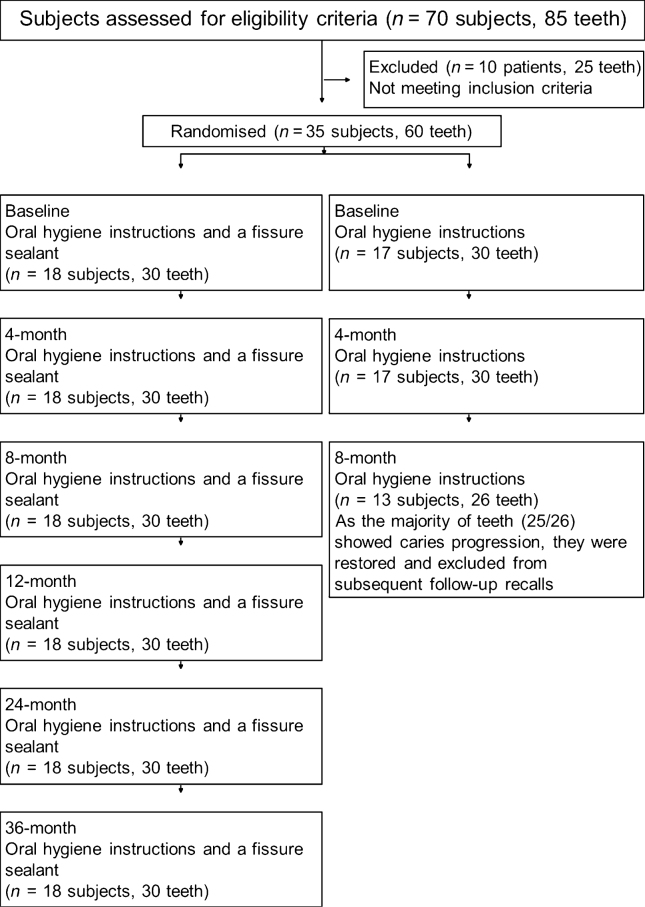
Four participants (four teeth) were lost at the 12-month recall appointment from the experiment group and at the 8-month recall appointment from the control group. At the 8-month follow-up, the majority of teeth (25/26) that had been allocated to the control group showed caries progression. These were restored and excluded from subsequent follow-up recalls. At 24 months and 36 months, all 26 teeth in the experiment group were re-evaluated (Figure 1). During recalls, patients reported the use of fluoridated toothpastes only; these included: Colgate Máxima Proteção Anticáries (Colgate-Palmolive Ldta, São Paulo, SP, Brazil), 1500 ppm fluoride; Tandy Morango (Colgate-Palmolive Ldta), 1100 ppm fluoride; Tandy Uva (Colgate-Palmolive Ldta), 1100 ppm fluoride, and Colgate Total 12 Clean Mint (Colgate-Palmolive Ldta), 1450 ppm fluoride.
Figure 1.
Flowchart of the trial.
With regard to sealant retention, full retention was observed in 23 of the 26 teeth evaluated at 12, 24 and 36 months. Partial retention was noticed in two teeth and complete loss was observed in one of the 26 teeth evaluated at 12, 24 and 36 months. Material loss was apparent only at the 12-month recall appointment.
At the 12-month recall appointment, a statistically significant difference was detected by Fisher’s exact test between teeth allocated to the experiment and control groups, respectively. Caries progression was present in three teeth with sealant loss (either partial or complete). These lesions were restored and excluded from future assessments. Subsequently from 12 months, the incidence of teeth presenting with caries progression was null (Table 2).
Table 2.
Number of teeth with clinical and/or radiographic caries progression in the experiment and control groups at each follow-up appointment
| Follow-up appointment | ||||
|---|---|---|---|---|
| 12 months* (n = 26) |
24 months (n = 23) |
36 months (n = 23) |
P-value | |
| Experiment group, n (%) | 3 (11.5%) | 0 | 0 | – |
| Control group, n (%) | 25 (96.1%) | – | – | – |
| P-value† | < 0.001 | – | – | |
8 months in the control group.
Fisher’s exact test.
DISCUSSION
The results of this work show that the progression of non-cavitated dentinal occlusal caries can be arrested by sealing pits and fissures. Although this finding had been previously indicated at 12 months7, this length of follow-up may be too short to provide the clinician with sufficient evidence to seal non-cavitated dentinal occlusal caries. By contrast, the results from the present 36-month clinical trial should be of major impact because this follow-up time is relatively long and thereby provides stronger evidence in favour of this approach.
It is interesting to note that the procedures to restore decayed teeth have evolved considerably in recent years. Some years ago, the predominant treatment was much more focused on operative intervention12. Recently, a minimally invasive approach has received great attention worldwide. This more conservative philosophy is based on sound science that spans the breadth of the disease continuum and includes the non-surgical management of early non-cavitated carious lesions13 and the use of effective conservative interventions for dentinal caries14. It is also recognised that the appropriate management of dental caries must include the improved diagnosis of early non-cavitated lesions, and measures for their prevention and arrest. However, some dentists continue to recommend surgical intervention for non-cavitated dentinal occlusal caries3., 4.. This normally puts the affected tooth into a repetitive restorative cycle, increasing the risks for adverse effects to the pulp and adjacent teeth14. All these factors contribute to a reduction in the longevity of the tooth and the restoration. By contrast, the adoption of a non-invasive treatment is expected to minimise the chances of secondary caries and early failures of restorations, and thereby to reduce the incidence of tooth fracture caused by extensive restoration and to maintain pulp vitality for longer15. Thus, the results obtained in this 36-month follow-up study support the adoption of non-surgical treatment for non-cavitated dentinal occlusal caries by the sealing of pits and fissures with a resin-based material.
Since the introduction of pit and fissure sealing in the 1960s16, dentists have assumed that caries, especially that affecting dentine, may progress beneath sealants. However, in a 10-year follow-up study, Mertz-Fairhurst et al.5 confirmed that composite restorations placed over frankly cavitated lesions were capable of arresting caries progression. Alves et al.6 obtained similar results in caries arrest when they partially removed carious dentine from deep caries lesions. Given these findings, we decided to investigate the efficacy of sealing pits and fissures in teeth with non-cavitated dentinal occlusal caries in an attempt to achieve caries arrest as a secondary preventive approach. Previous 12-month follow-ups involving either deciduous17 or permanent7 teeth, together with the results from the present investigation, confirm that the progression of non-cavitated dentinal occlusal caries can be arrested by sealing pits and fissures. A connection between caries progression and sealant loss at 12 months was also apparent. This leads to the assumption that the blocking of the nutritional supply to infected dentine may be the most plausible explanation for the lack of caries progression observed in these studies7., 17. and in others reported elsewhere.5., 6. When the sealant bond is disrupted, the infected dentine resumes its nutritional supply, thus favouring bacterial growth and caries progression. Therefore, regular professional follow-up is necessary when sealing caries and patients must have easy access to regular recall appointments.
The protective barrier provided by the sealant, which precludes the passage of stimuli, may well explain the lack of sensitivity in teeth with full material retention during recall appointments7. In the present investigation, a resin-based, fluoride-releasing sealant with an opaque colour was chosen because it could be easily distinguished from the tooth structure. Resin-based sealants have relatively good adherence to tooth structure and have increased resistance to wear18, and thus act as mechanical obstacles to the formation of biofilm on the occlusal surface. In addition, the fluoride that is released within a short period of time exerts a cariostatic effect on the enamel surface, thereby increasing the effectiveness of treatment19. However, as caries arrest is highly dependent upon sealant retention, researchers must seek ways to improve the mechanical strength of sealants. The use of flowable composite as a fissure sealant may be an interesting option in teeth with non-cavitated dentinal occlusal caries as its physical properties are superior to those of traditional fissure sealants20., 21.. An extended period of photoactivation can improve physical properties20., 21.. Further clinical trials should be carried out to confirm the clinical benefits to be derived from the use of flowable composites and extended periods of photoactivation.
Possible limitations of this study include the absence of a power calculation, the sample size of 60 teeth and the loss of some of the sample at 12 months, which may have decreased the internal and external validity of the present investigation. However, the remarkable difference in caries progression observed between the two groups at the 12-month recall appointment indicates that the sample size was satisfactory for the analysis and that the observation period was appropriate to detect distinct differences in the outcomes of the two procedures. Indeed, the lack of caries progression at 12-, 24- and 36-month recall appointments observed in teeth with intact sealant clearly confirmed that this sample size was satisfactory. Moreover, because of the difficulty of selecting patients with similar caries lesions in two separate teeth, it was necessary to consider each eligible tooth as an independent analysis unit. This was also reported in a previous study7. However, it is reasonable to assume that caries development, progression and arrest may differ among teeth, even within the same individual because if they did not, patients would present with concomitant caries in all homologous teeth. Therefore, this did not seem to influence the results of the present investigation.
Conflicts of interest
None declared.
REFERENCES
- 1.Bader JD, Shugars DA. The evidence supporting alternative management strategies for early occlusal caries and suspected occlusal dentinal caries. J Evid Base Dent Pract. 2006;6:91–100. doi: 10.1016/j.jebdp.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Weerheijm KL, van Amerongen WE, Eggink CO. The clinical diagnosis of occlusal caries: a problem. ASDC J Dent Child. 1989;56:196–200. [PubMed] [Google Scholar]
- 3.Murdoch-Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc. 2003;134:87–95. doi: 10.14219/jada.archive.2003.0021. [DOI] [PubMed] [Google Scholar]
- 4.Brostek A. Early diagnosis and minimally invasive treatment of occlusal caries – a clinical approach. Oral Health Prev Dent. 2004;2(Suppl 1):313–319. [PubMed] [Google Scholar]
- 5.Mertz-Fairhurst EJ, Curtis JW, Jr, Ergle JW, et al. Ultraconservative and cariostatic sealed restorations: results at year 10. J Am Dent Assoc. 1998;129:55–66. doi: 10.14219/jada.archive.1998.0022. [DOI] [PubMed] [Google Scholar]
- 6.Alves LS, Fontanella V, Damo AC, et al. Qualitative and quantitative radiographic assessment of sealed carious dentin: a 10-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:135–141. doi: 10.1016/j.tripleo.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 7.Borges BC, Campos GB, da Silveira AD, et al. Efficacy of a pit and fissure sealant in arresting dentin non-cavitated caries: a 1-year follow-up, randomised, single-blind, controlled clinical trial. Am J Dent. 2010;23:311–316. [PubMed] [Google Scholar]
- 8.Needleman I, Worthington H, Moher D, et al. Improving the completeness and transparency of reports of randomised trials in oral health: the CONSORT Statement. Am J Dent. 2008;21:7–12. [PubMed] [Google Scholar]
- 9.Martínez-González MA, Sánchez-Villegas A, Fajardo JF. 3rd ed. Ediciones Díaz de Santos; Madrid: 2009. Bioestadística Amigable; p. 919. [Google Scholar]
- 10.de Andrade AK, Duarte RM, Medeiros e Silva FD, et al. 30-month randomised clinical trial to evaluate the clinical performance of a nanofill and a nanohybrid composite. J Dent. 2011;39:8–15. doi: 10.1016/j.jdent.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Fones CA. 2nd ed. Lea & Febiger; Philadelphia, PA; New York, NY: 1921. Mouth Hygiene. A Text Book for Dental Hygienists; p. 334. [Google Scholar]
- 12.Borges BC, de SouzaBorges J, de Araujo LS, et al. Update on non-surgical, ultraconservative approaches to treat effectively non-cavitated caries lesions in permanent teeth. Eur J Dent. 2011;5:229–236. [PMC free article] [PubMed] [Google Scholar]
- 13.Pitts NB. Modern concepts of caries measurement. J Dent Res. 2004;83(Spec Issue C):43–47. doi: 10.1177/154405910408301s09. [DOI] [PubMed] [Google Scholar]
- 14.McComb D. Systematic review of conservative operative caries management strategies. J Dent Educ. 2001;65:1154–1161. [PubMed] [Google Scholar]
- 15.Dennison JB, Hamilton JC. Treatment decisions and conservation of tooth structure. Dent Clin N Am. 2005;49:825–845. doi: 10.1016/j.cden.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 16.Aguilar FG, Drubi-Filho B, Casemiro LA, et al. Retention and penetration of a conventional resin-based sealant and a photochromatic flowable composite resin placed on occlusal pits and fissures. J Indian Soc Pedod Prev Dent. 2007;25:169–173. doi: 10.4103/0970-4388.37012. [DOI] [PubMed] [Google Scholar]
- 17.Borges BC, Araújo RF, Dantas RF, et al. Efficacy of a non-drilling approach to manage non-cavitated dentin occlusal caries in primary molars: a 12-month randomised controlled clinical trial. Int J Paediatr Dent. 2012;22:44–51. doi: 10.1111/j.1365-263X.2011.01156.x. [DOI] [PubMed] [Google Scholar]
- 18.Donly KJ. Sealants: where we have been; where we are going. Gen Dent. 2002;50:438–440. [PubMed] [Google Scholar]
- 19.Yamamoto H, Iwami Y, Unezaki T, et al. Fluoride uptake around cavity walls: two-dimensional mapping by electron probe microanalysis. Oper Dent. 2000;25:104–112. [PubMed] [Google Scholar]
- 20.Borges BC, Bezerra GV, Mesquita JdeA, et al. Effect of irradiation times on the polymerisation depth of contemporary fissure sealants with different opacities. Braz Oral Res. 2011;25:135–142. doi: 10.1590/s1806-83242011000200007. [DOI] [PubMed] [Google Scholar]
- 21.Borges BC, Souza-Júnior EJ, Catelan A, et al. Influence of extended light exposure time on the degree of conversion and plasticisation of materials used as pit and fissure sealants. J Investig Clin Dent. 2010;1:151–155. doi: 10.1111/j.2041-1626.2010.00015.x. [DOI] [PubMed] [Google Scholar]