Abstract
Objectives: The aim of the present study was to review the pertinent literature with reference to the clinical efficacy of antibiotics in the treatment of peri-implantitis. Methods: To address the focused question ‘Are locally and systemically delivered antibiotics useful in the treatment of peri-implantitis?’ PubMed/Medline and Google-scholar databases were explored from 1992 until February 2013 using a combination of the following keywords: ‘antibiotic,’ ‘dental implant,’ ‘inflammation,’, ‘peri-implantitis’ and ‘treatment’. Letters to the editor, case-reports and unpublished data were excluded. Results: Ten studies were included. In six studies, peri-implantitis was treated using a non-surgical approach (scaling and root planing), whereas in four studies, a surgical approach was adopted for treating peri-implantitis. In three studies systemic antibiotics were administered and in six studies locally delivered antibiotics were used for treatment. One study used the oral route for antibiotic delivery. In three studies, minocycline hydrochloride was locally delivered as an adjunctive therapy to non-surgical mechanical debridement of infected sites. Nine studies reported that traditional peri-implantitis treatment with adjunct antibiotic therapy reduces gingival bleeding, suppuration and peri-implant pocket depth. In one study, despite surgical debridement of infected sites and systemic antibiotic cover, nearly 40% of the implants failed to regain stability. There was no placebo or control group in eight out of the nine studies included. Conclusion: The significance of adjunctive antibiotic therapy in the treatment of peri-implantitis remains debatable.
Key words: Antibiotic, dental implant, inflammation, peri-implantitis, treatment
INTRODUCTION
It is well-known that dental implants can osseointegrate and remain functionally stable in healthy as well as medically compromised individuals1., 2., 3., 4., 5., 6., 7., 8., 9., 10., 11., 12., 13., 14.; however, the risk of complications occurring following implant placement cannot be disregarded13., 14.. Risk factors associated with peri-implant complications include inadequate primary stability at the time of implant placement, occlusal trauma, fractured components, pain, local and systemic infections, neuropathy and tobacco smoking15., 16., 17.. Peri-implantitis (PI) is an inflammatory condition characterised by loss of supporting bone in the tissues surrounding the implant18. In general, the frequency of PI has been reported to be 5–8% for various implant systems19. Clinical signs of PI include gingival bleeding, suppuration, increased pocket depth (PD) and implant mobility; whereas alveolar bone loss can be observed on radiographs18., 20., 21.. In addition, studies have also shown a similarity in bacterial flora associated with PI and periodontitis8., 22., 23., 24..
Various treatment regimes for PI have been proposed in the literature. These include plaque control regimens, mechanical debridement of the affected areas, irrigation with antiseptic agents [such as chlorhexidine (CHX), saline and 10% hydrogen per oxide], surgical flap access into infected peri-implant tissues and laser therapy8., 9., 25., 26..
As it is known that bacteria can transfer from periodontally involved teeth to an implant, and that the microbes associated with PI resemble those of periodontal disease22., 25., it is hypothesised that local or systemic delivery of antibiotics with traditional PI treatment regimes eliminates periodontopathogenic bacteria to a greater extent compared with when these treatment regimes are performed alone. This may in turn facilitate healing of PI sites. As locally and/or systemically delivered antibiotics apparently play essential roles in the treatment of PI, it is pertinent to investigate the type of antibiotic, dosage and duration of use that would be most effective for treating PI.
The aim of the present review was to assess the clinical efficacy of antibiotics in the treatment of PI.
METHODS
Focused question
The focused question addressed was: ‘What is the clinical efficacy of locally and systemically delivered antibiotics in the treatment of PI?’
Inclusion criteria
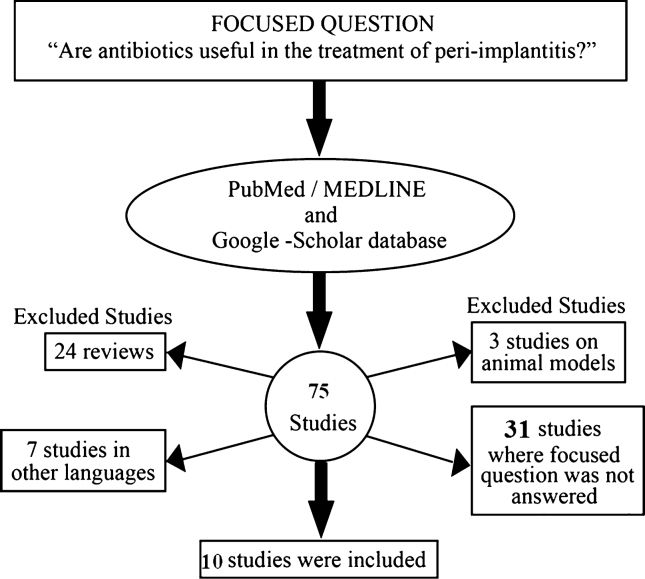
The selection protocol encompassed the following: (1) original studies; (2) clinical studies; (3) hand searching of the reference lists of potentially relevant original and review studies; (4) intervention (use of locally and systemically delivered antibiotics in the treatment of PI); and (5) studies published only in the English language (Figure 1).
Figure 1.
Study selection protocol.
Exclusion criteria
The exclusion criteria encompassed the following: (1) experimental studies; (2) letters to the editor; (3) historic reviews; and (4) unpublished data (Figure 1). Any disagreement among the authors was resolved via discussion.
Search methods
As a first step, the authors searched the National Library of Medicine, Washington, DC (MEDLINE–PubMed) and Google Scholar databases for appropriate articles addressing the focus question (as stated above). These databases were explored from 1992 up to and including February 2013 using the following key indexing terms in different combinations: ‘antibiotic’, ‘dental implant’, ‘inflammation’, ‘peri-implantitis’ and ‘treatment’.
In the second step, reference lists of original and review studies that were found to be relevant in the first step were hand-searched. Titles of research articles containing words suggesting the use of antibiotics as adjuncts to PI therapy were also sought. After final selection, studies that fulfilled the selection criteria were processed for data extraction.
Data extraction and management
The initial search yielded 75 articles. Scrutiny of the titles and abstracts abridged the number of studies to 101., 2., 3., 4., 5., 6., 7., 8., 9., 10.. Sixty-five studies that did not abide by the inclusion criteria were excluded (see Appendix A). As a limited number of original clinical studies addressed our focused question, the pattern of the present systematic review was customised to primarily summarise the pertinent data.
RESULTS
Characteristics of studies included
All studies1., 2., 3., 4., 5., 6., 7., 8., 9., 10. were performed at universities or health-care centres. The numbers of patients included in these studies ranged from 9 to 281 individuals. These individuals were aged between 25 years and 79 years. The total numbers of dental implants inserted in the study participants ranged between 9 and 193 titanium implants. Three studies4., 6., 7. were randomised clinical trials, two studies2., 5. had a prospective cohort design, two studies8., 10. were prospective follow-ups, two1., 9. studies were case series and one study2 had a retrospective design (Table 1).
Table 1.
Clinical studies on the effect of antibiotic therapy on the treatment of peri-implantitis (PI)
| Author/s et al. (Year) | Study design | Subjects/number of implants | Treatment protocol | Antibiotic/s used | Route of antibiotic delivery | Control/placebo group? (Yes/No) | Follow-up | Main results |
|---|---|---|---|---|---|---|---|---|
| AlGhamdi AS1 | Case series | 80/193 | Open flap debridement and implant surface cleaning with hand instruments | Tetracycline solution + doxycycline powder | Local | No | ~30 months | Open flap debridement with adjunct antibiotic therapy caused significant reduction in probing depth and suppuration at PI sites |
| Heitz-Mayfield et al.2 | Prospective cohort study | 24/36 | Open flap debridement, implant surface cleaning with hand instruments and saline irrigation | Amoxicillin + metronidazole | Systemic | No | 12 months | Open flap debridement with adjunct antibiotic therapy caused significant reduction in probing depth and suppuration at PI sites |
| Charalampakis et al.3 | Retrospective | 281/NA | 228 patients (83.2%) were treated surgically (open flap debridement, implant surface cleaning) 46 patients (16.8%) were treated non-surgically (mechanical debridement via curettes). |
Amoxicillin + metronidazole (~50% cases) Metronidazole (~20% cases) Ciprofloxacin (~11% cases) Others (~19% cases) |
Oral | No | 1–6 years | Bone plasty with adjunct antibiotic therapy antibiotics during surgery was significantly associated with arrested PI lesions. |
| Renvert et al.4 | Single-masked, randomised, two-arm clinical trial | 25/31 | Non-surgical (scaling and root planing) | Minocycline hydrochloride | Local | No | 12 months | Mechanical treatment of PI with minocycline hydrochloride as an adjunct demonstrated reduction in probing depth |
| Salvi et al.5 | Open-label case cohort study | 25/31 | Mechanical debridement with curettes | Minocycline hydrochloride | Local | No | 12 months | Mechanical treatment of PI with minocycline hydrochloride as an adjunct demonstrated reduction in probing depth |
| Renvert et al.6 | Randomised clinical trial | 32/NA | Non-surgical mechanical debridement with curettes and CHX wash | Minocycline hydrochloride | Local | No | 12 months | Mechanical treatment of PI with minocycline hydrochloride as an adjunct demonstrated reduction in probing depth |
| Büchter et al.7 | Randomised clinical trial | 28/48 | Non-surgical mechanical debridement with curettes | Doxycycline | Local | Yes | 4.5 months | Probing attached levels were significantly higher in PI cases treated with non-surgical debridement + doxycycline than those treated with non-surgical debridement alone |
| Leonhardt et al.8 | Prospective follow-up | 9/44 | Open flap debridement and disinfection with 10% hydrogen per oxide | Part 1: clindamycin Part 2: amoxicillin + metronidazole Part 3: tetracycline Part 4: tetracycline Part 5: amoxicillin + metronidazole Part 6: ciprofloxacin Part 7: sulfonamide + trimethoprim Part 8: metronidazole Part 9: ciprofloxacin |
Systemic | No | 5 years | Despite surgical debridement and antibiotic therapy, seven implants were lost. In 58% cases, surgical treatment with adjunct antibiotic therapy was successful for treating PI |
| Mombelli et al.9 | Case series | 25/30 | Local debridement and irrigation with 0.2% CHX | Tetracycline HCl-containing fibres | Local | No | 12 months | Local treatment of PI with tetracycline HCL-containing fibres as an adjunct demonstrated reduction in probing depth and bleeding |
| Mombelli & Lang10 | Prospective follow-up | 9/9 | Local debridement and irrigation with 0.5% CHX | Ornidazole (1 g daily for 10 days) | Systemic | No | 12 months | Local treatment of PI with ornidazole as an adjunct demonstrated reduction in probing depth and bleeding |
CHX, chlorhexidine.
In six studies4., 5., 6., 7., 9., 10., PI was treated using a non-surgical approach (scaling and root planing), whereas in four studies1., 2., 3., 8. a surgical approach (open flap debridement) was adopted. In three studies2., 8., 10. systemic antibiotics were administered to the study subjects, whereas six studies1., 4., 5., 6., 7., 9. used locally delivered antibiotics for the treatment of PI. One study2 used the oral route for antibiotic delivery. In three studies, minocycline hydrochloride was locally delivered as an adjunctive therapy to non-surgical mechanical debridement of infected sites4., 5., 6.. Nine studies1., 2., 3., 4., 5., 6., 7., 9., 10. reported that traditional PI treatment with adjunct antibiotic therapy reduced gingival bleeding, suppuration and peri-implant pocket depth. In one study8, despite surgical debridement of infected sites and systemic antibiotic cover, nearly 40% of the implants failed to regain stability. There was no placebo or control group in nine studies1., 2., 3., 4., 5., 6., 8., 9., 10.. These results are shown in Table 1.
DISCUSSION
From the studies1., 2., 3., 4., 5., 6., 7., 8., 9., 10. included in the present systemic review, it is postulated that antibiotics, when used as adjuncts to conventional PI treatment regimes, promote healing of inflamed peri-implant tissues. Although mechanical debridement and disinfection of implant surfaces (using curettes and CHX, respectively) removes the oral biofilm and periopathogenic microbes to some extent, it is tempting to speculate that an absolute extermination of the oral biofilm is difficult to accomplish because of variations in surface characteristics and the morphology of various implant systems. This may be a logical foundation for using locally delivered and systemic antibiotics as adjuncts to conventional PI treatment regimes. Nevertheless, there is no scientific justification in this regard because none of the clinical studies1., 2., 3., 4., 5., 6., 7., 8., 9., 10. included in the present review used a control group (that is, treatment of PI without local or systemic antibiotics). The study by Leonhardt et al.8 reported 5-year results following the treatment of PI. In this study8, the PI lesions were surgically exposed, affected implants were cleaned with an antiseptic agent and systemic antibiotics were administered. The results showed that, despite the surgical and antimicrobial treatment regimen applied, additional loss of supporting bone was found in nearly 40% of the advanced PI lesions. Thus the clinical efficacy of antibiotics as adjuncts to conventional PI therapy is rather dubious. There is an urgent need for double-blinded placebo-controlled randomised clinical trials to demonstrate the efficacy of locally delivered and systemically delivered antibiotics in the treatment of PI.
It is notable that the type of antibiotic, route of administration, dosage and duration of use varied among studies. For example, in the studies by Renvert and colleagues4., 6. and Salvi et al.5 local delivery of 1 mg of minocycline hydrochloride, when used as an adjunct to mechanical debridement of implant sites, was reported to reduce inflammation, whereas Büchter et al.7 showed that local delivery of doxycycline as an adjunct is effective in the treatment of PI. Heitz-Mayfield et al.2 reported that systemic administration of a combination of amoxicillin and metronidazole promotes the healing of inflamed peri-implant tissues following surgical curettage whereas Mombelli & Lang10, reported that mechanical debridement of PI lesions, pocket irrigation with chlorhexidine and adjunctive systemic administration of 1000 mg ornidazole resulted in improved clinical conditions. In this context, the criteria for selecting the type and dosage of an antibiotic for the treatment of PI are yet to be established.
In conclusion, our focused question ‘What is the clinical efficacy of locally and systemically delivered antibiotics in the treatment of PI?’ remains unanswered.
Acknowledgements
The authors would like to thank the College of Dentistry Research Center and Deanship of Scientific Research at King Saud University, Saudi Arabia for funding this research project (Research project # FR 0050). [Correction added on 24 May 2013, after first online publication: new Acknowledgement text has been added.]
Conflict of interest
None declared.
A APPENDIX
List of studies excluded. Reason for exclusion is shown in parenthesis after the reference.
Alissa R, Oliver RJ. Influence of prognostic risk indicators on osseointegrated dental implant failure: a matched case-control analysis. J Oral Implantol 2012 38: 51–61 (focused question not answered).
Ayangco L, Sheridan PJ. Development and treatment of retrograde peri-implantitis involving a site with a history of failed endodontic and apicoectomy procedures: a series of reports. Int J Oral Maxillofac Implants 2001 16: 412–417 (focused question not answered).
Behneke A, Behneke N, d’Hoedt B. Treatment of peri-implantitis defects with autogenous bone grafts: 6-month to 3-year results of a prospective study in 17 patients. Int J Oral Maxillofac Implants 2000 15: 125–138 (focused question not answered).
Bories C, Struillou X, Badran Z et al. Peri-implantitis: tools and techniques for disinfecting the implant surface. Schweiz Monatsschr Zahnmed 2011 121: 341–355 (article in German).
Bortolaia C, Sbordone L. Biofilms of the oral cavity. Formation, development and involvement in the onset of diseases related to bacterial plaque increase. Minerva Stomatol 2002 51: 187–192 (focused question not answered).
Bumgardner JD, Adatrow P, Haggard WO et al. Emerging antibacterial biomaterial strategies for the prevention of peri-implant inflammatory diseases. Int J Oral Maxillofac Implants 2011; 26: 553–60 (Review).
Bunetel L, Guérin J, Agnani G et al. In vitro study of the effect of titanium on porphyromonas gingivalis in the presence of metronidazole and spiramycin. Biomaterials 2001 22: 3067–3072 (focused question not answered).
El Chaar ES, Jalbout ZN. Regeneration of an osseous peri-implantitis lesion. Periodontal Clin Investig 2002 24: 5–10 (focused question not answered).
Ericsson I, Persson LG, Berglundh T et al. The effect of antimicrobial therapy on periimplantitis lesions. An experimental study in the dog. Clin Oral Implants Res 1996 7: 320–328 (animal study).
Esposito M, Grusovin MG, Coulthard P et al. The efficacy of interventions to treat peri-implantitis: a Cochrane systematic review of randomised controlled clinical trials. Eur J Oral Implantol 2008 1: 111–125 (Review).
Esposito M, Grusovin MG, Worthington HV. Interventions for replacing missing teeth: treatment of peri-implantitis. Cochrane Database Syst Rev 2012 1: CD004970 (Review).
Esposito M, Grusovin MG, Worthington HV. Treatment of peri-implantitis: what interventions are effective? A Cochrane systematic review. Eur J Oral Implantol 2012 5: S21–S41(Review).
Esposito M, Hirsch JM, Lekholm U et al. Biological factors contributing to failures of osseointegrated oral implants. (II). Etiopathogenesis. Eur J Oral Sci 1998 106: 721–764 (Review).
Ewald A, Ihde S. Salt impregnation of implant materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 107: 790–795 (focused question not answered).
Faggion CM Jr, Schmitter M. Using the best available evidence to support clinical decisions in implant dentistry. Int J Oral Maxillofac Implants 2010 25: 960–969 (Review).
Hämmerle CH, Fourmousis I, Winkler JR et al. Successful bone fill in late peri-implant defects using guided tissue regeneration. A short communication. J Periodontol 1995 66: 303–308 (focused question not answered).
Irshad M, van der Reijden WA, Crielaard W et al. In vitro invasion and survival of porphyromonas gingivalis in gingival fibroblasts; role of the capsule. Arch Immunol Ther Exp (Warsz) 2012 60: 469–476 (focused question not answered).
Kaplan I, Anavi K, Anavi Y et al. The clinical spectrum of Actinomyces-associated lesions of the oral mucosa and jawbones: correlations with histomorphometric analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 108: 738–746 (focused question not answered).
Kivelä-Rajamäki M, Maisi P, Srinivas R et al. Levels and molecular forms of MMP-7 (matrilysin-1) and MMP-8 (collagenase-2) in diseased human peri-implant sulcular fluid. J Periodontal Res 2003 38: 583–590 (focused question not answered).
Klinge B, Gustafsson A, Berglundh T. A systematic review of the effect of anti-infective therapy in the treatment of peri-implantitis. J Clin Periodontol 2002 29: 213–225; discussion 232-3 (Review).
Klinge B, Hultin M, Berglundh T. Peri-implantitis. Dent Clin North Am 2005 49: 661–676, vii-–viii (Review).
Kotsovilis S, Karoussis IK, Trianti M et al. Therapy of peri-implantitis: a systematic review. J Clin Periodontol 2008 35: 621–629 (Review).
Kozlovsky A, Mozes O, Nemcovsky CE et al. Differential diagnosis and treatment strategies for peri-implant diseases. Refuat Hapeh Vehashinayim 2003 20: 30–41, 100 (article in Hebrew).
Liao J, Anchun M, Zhu Z et al. Antibacterial titanium plate deposited by silver nanoparticles exhibits cell compatibility. Int J Nanomedicine 2010 5: 337–342 (focused question not answered).
López-Cerero L. Dental implant-related infections. Enferm Infecc Microbiol Clin 2008 26: 589–592 (article in Spanish).
Mattheos N, Collier S, Walmsley AD. Specialists’ management decisions and attitudes towards mucositis and peri-implantitis. Br Dent J 2012 Jan 13; 212: E1. doi: 10.1038/sj.bdj.2012.1 (focused question not answered).
Meffert RM. Periodontitis vs. peri-implantitis: the same disease? The same treatment? Crit Rev Oral Biol Med 1996 7: 278–291 (Review).
Meisel P, Kocher T. Photodynamic therapy for periodontal diseases: state of the art. J Photochem Photobiol B 2005 79: 159–170 (focused question not answered).
Mombelli A, Moëne R, Décaillet F. Surgical treatments of peri-implantitis. Eur J Oral Implantol 2012 5: S61–S70 (Review).
Mombelli A. Microbiology and antimicrobial therapy of peri-implantitis. Periodontol 2000 2002 28: 177–189 (Review).
Mouratidou A, Karbach J, d’Hoedt B et al. Antibiotic susceptibility of cocultures in polymicrobial infections such as peri-implantitis or periodontitis: an in vitro model. J Periodontol 2011 82: 1360–1366 (focused question not answered).
Norowski PA Jr, Bumgardner JD. Biomaterial and antibiotic strategies for peri-implantitis: a review. J Biomed Mater Res B Appl Biomater 2009 88: 530–543 (Review).
Okayasu K, Wang HL. Decision tree for the management of periimplant diseases. Implant Dent 2011 20: 256–261 (Review).
Otto M, Gluckman H. The treatment of peri-mucositis and peri-implantitis 1. SADJ 2008 63: 250, 252 (Review).
Paquette DW, Ryan ME, Wilder RS. Locally delivered antimicrobials: clinical evidence and relevance. J Dent Hyg 2008 82: 10–15 (Review).
Persson GR, Salvi GE, Heitz-Mayfield LJ et al. Antimicrobial therapy using a local drug delivery system (Arestin) in the treatment of peri-implantitis. I: Microbiological outcomes. Clin Oral Implants Res 2006 17: 386–393 (focused question not answered).
Persson LG, Araújo MG, Berglundh T et al. Resolution of peri-implantitis following treatment. An experimental study in the dog. Clin Oral Implants Res 1999 10: 195–203 (animal study).
Persson LG, Berglundh T, Lindhe J et al. Re-osseointegration after treatment of peri-implantitis at different implant surfaces. An experimental study in the dog. Clin Oral Implants Res 2001 12: 595–603 (focused question not answered).
Persson LG, Ericsson I, Berglundh T et al. Guided bone regeneration in the treatment of periimplantitis. Clin Oral Implants Res 1996 7: 366–372 (focused question not answered).
Persson LG, Ericsson I, Berglundh T et al. Osseintegration following treatment of peri-implantitis and replacement of implant components. An experimental study in the dog. J Clin Periodontol 2001 28: 258–263 (animal study).
Persson LG, Mouhyi J, Berglundh T et al. Carbon dioxide laser and hydrogen peroxide conditioning in the treatment of periimplantitis: an experimental study in the dog. Clin Implant Dent Relat Res 2004 6: 230–238 (focused question not answered).
Pye AD, Lockhart DE, Dawson MP et al. A review of dental implants and infection. J Hosp Infect 2009 72: 104–110 (Review).
Rams TE, Balkin BE, Roberts TW et al. Microbiological aspects of human mandibular subperiosteal dental implants. J Oral Implantol 2011 Jul 18. [Epub ahead of print] (focused question not answered).
Renvert S, Roos-Jansåker AM, Claffey N. Non-surgical treatment of peri-implant mucositis and peri-implantitis: a literature review. J Clin Periodontol 2008 35: 305–315 (Review).
Romeo E, Lops D, Storelli S et al. Clinical peri-implant sounding accuracy in the presence of chronic inflammation of peri-implant tissues. Clinical observation study. Minerva Stomatol 2009 58: 81–91 (focused question not answered).
Roos-Jansåker AM, Renvert S, Egelberg J. Treatment of peri-implant infections: a literature review. J Clin Periodontol 2003 30: 467–485 (Review).
Saini R. Ozone therapy in dentistry: A a strategic review. J Nat Sci Biol Med 2011 2: 151–153 (Review).
Sánchez-Gárces MA, Gay-Escoda C. Periimplantitis. Med Oral Patol Oral Cir Bucal 2004 9: 63–74 (article in Spanish).
Schuckert KH, Jopp S, Teoh SH. Mandibular defect reconstruction using three-dimensional polycaprolactone scaffold in combination with platelet-rich plasma and recombinant human bone morphogenetic protein-2: de novo synthesis of bone in a single case. Tissue Eng Part A 2009 15: 493–499 (focused question not answered).
Sennerby L, Persson LG, Berglundh T et al. Implant stability during initiation and resolution of experimental periimplantitis: an experimental study in the dog. Clin Implant Dent Relat Res 2005 7: 136–140 (focused question not answered).
Shumaker ND, Metcalf BT, Toscano NT et al. Periodontal and periimplant maintenance: a critical factor in long-term treatment success. Compend Contin Educ Dent 2009 30: 388–390, 392, 394 passim; quiz 407, 418 (focused question not answered).
Singh P. Understanding peri-implantitis: a strategic review. J Oral Implantol 2011 37: 622–626 (Review).
Sorsa T, Tervahartiala T, Leppilahti J et al. Collagenase-2 (MMP-8) as a point-of-care biomarker in periodontitis and cardiovascular diseases. Therapeutic response to non-antimicrobial properties of tetracyclines. Pharmacol Res 2011 63: 108–113 (focused question not answered).
Stellini E, Migliorato A, Mazzoleni S et al. Topical treatment of peri-implantitis with metronidazole dental gel 25%. Clinical analysis and microbiological control. Minerva Stomatol 2000 49: 59–67 (article in Italian).
Suh JJ, Simon Z, Jeon YS et al. The use of implantoplasty and guided bone regeneration in the treatment of peri-implantitis: two case reports. Implant Dent 2003 12: 277–282 (focused question not answered).
Tanner A, Stillman N. Oral and dental infections with anaerobic bacteria: clinical features, predominant pathogens, and treatment. Clin Infect Dis 1993 16(Suppl 4): S304–S309 (Review).
Tanner A. Microbial etiology of periodontal diseases. Where are we? Where are we going? Curr Opin Dent 1992 2: 12–24. (Review).
Tinti C, Parma-Benfenati S. Treatment of peri-implant defects with the vertical ridge augmentation procedure: a patient report. Int J Oral Maxillofac Implants 2001 16: 572–577 (focused question not answered).
van Winkelhoff AJ, van der Avoort PG, Wismeijer D. Infectious complications with dental implants. Ned Tijdschr Tandheelkd 2009 116: 193–197 (Article article in Dutch).
van Winkelhoff AJ, Wolf JW. Actinobacillus actinomycetemcomitans-associated peri-implantitis in an edentulous patient. A case report. J Clin Periodontol 2000 27: 531–535 (focused question not answered).
van Winkelhoff AJ. Antibiotics in the treatment of peri-implantitis. Eur J Oral Implantol 2012 5(Suppl): S43–S50 (Review).
Waasdrop J, Reynolds M. Nonsurgical treatment of retrograde peri-implantitis: a case report. Int J Oral Maxillofac Implants 2010 25: 831–833 (focused question not answered).
Yuan K, Chen KC, Chan YJ et al. Dental implant failure associated with bacterial infection and long-term bisphosphonate usage: a case report. Implant Dent 2012 21: 3–7 (focused question not answered).
Zhou L, Lin Y, Qiu LX et al. Clinical study of periocline on peri-implantitis treatment. Zhonghua Kou Qiang Yi Xue Za Zhi 2006 41: 299–303 (article in Spanish).
REFERENCES
- 1.AlGhamdi AS. Successful treatment of early implant failure: a case series. Clin Implant Dent Relat Res. 2012;14:380–387. doi: 10.1111/j.1708-8208.2009.00267.x. [DOI] [PubMed] [Google Scholar]
- 2.Heitz-Mayfield LJ, Salvi GE, Mombelli A, et al. Anti-infective surgical therapy of peri-implantitis. A 12-month prospective clinical study. Clin Oral Implants Res. 2012;23:205–210. doi: 10.1111/j.1600-0501.2011.02276.x. [DOI] [PubMed] [Google Scholar]
- 3.Charalampakis G, Rabe P, Leonhardt A, et al. A follow-up study of peri-implantitis cases after treatment. J Clin Periodontol. 2011;38:864–871. doi: 10.1111/j.1600-051X.2011.01759.x. [DOI] [PubMed] [Google Scholar]
- 4.Renvert S, Lessem J, Dahlen G, et al. Mechanical and repeated antimicrobial therapy using a local drug delivery system in the treatment of peri-implantitis: a randomized clinical trial. J Periodontol. 2008;79:836–844. doi: 10.1902/jop.2008.070347. [DOI] [PubMed] [Google Scholar]
- 5.Salvi GE, Persson GR, Heitz-Mayfield LJ, et al. Adjunctive local antibiotic therapy in the treatment of peri-implantitis II: clinical and radiographic outcomes. Clin Oral Implants Res. 2007;18:281–285. doi: 10.1111/j.1600-0501.2007.01377.x. [DOI] [PubMed] [Google Scholar]
- 6.Renvert S, Lessem J, Dahlen G, et al. Topical minocycline microspheres versus topical chlorhexidine gel as an adjunct to mechanical debridement of incipient peri-implant infections: a randomized clinical trial. J Clin Periodontol. 2006;33:362–369. doi: 10.1111/j.1600-051X.2006.00919.x. [DOI] [PubMed] [Google Scholar]
- 7.Buchter A, Meyer U, Kruse-Losler B, et al. Sustained release of doxycycline for the treatment of peri-implantitis: randomised controlled trial. Br J Oral Maxillofac Surg. 2004;42:439–444. doi: 10.1016/j.bjoms.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Leonhardt A, Dahlen G, Renvert S. Five-year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol. 2003;74:1415–1422. doi: 10.1902/jop.2003.74.10.1415. [DOI] [PubMed] [Google Scholar]
- 9.Mombelli A, Feloutzis A, Bragger U, et al. Treatment of peri-implantitis by local delivery of tetracycline. Clinical, microbiological and radiological results. Clin Oral Implants Res. 2001;12:287–294. doi: 10.1034/j.1600-0501.2001.012004287.x. [DOI] [PubMed] [Google Scholar]
- 10.Mombelli A, Lang NP. Antimicrobial treatment of peri-implant infections. Clin Oral Implants Res. 1992;3:162–168. doi: 10.1034/j.1600-0501.1992.030402.x. [DOI] [PubMed] [Google Scholar]
- 11.Javed F, Romanos GE. Impact of diabetes mellitus and glycemic control on the osseointegration of dental implants: a systematic literature review. J Periodontol. 2009;80:1719–1730. doi: 10.1902/jop.2009.090283. [DOI] [PubMed] [Google Scholar]
- 12.Javed F, Almas K. Osseointegration of dental implants in patients undergoing bisphosphonate treatment: a literature review. J Periodontol. 2010;81:479–484. doi: 10.1902/jop.2009.090587. [DOI] [PubMed] [Google Scholar]
- 13.Javed F, Al-Hezaimi K, Almas K, et al. Is Titanium Sensitivity Associated with Allergic Reactions in Patients with Dental Implants? A Systematic Review. Clin Implant Dent Relat Res. 2013;15:47–52. doi: 10.1111/j.1708-8208.2010.00330.x. [DOI] [PubMed] [Google Scholar]
- 14.Javed F, Al-Askar M, Qayyum F, et al. Oral squamous cell carcinoma arising around osseointegrated dental implants. Implant Dent. 2012;21:280–286. doi: 10.1097/ID.0b013e31824cde85. [DOI] [PubMed] [Google Scholar]
- 15.Javed F, Al-Hezaimi K, Al-Rasheed A, et al. Implant survival rate after oral cancer therapy: a review. Oral Oncol. 2010;46:854–859. doi: 10.1016/j.oraloncology.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010;38:612–620. doi: 10.1016/j.jdent.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 17.Parameter on placement and management of the dental implant. American Academy of Periodontology. J Periodontol. 2000;71:870–872. doi: 10.1902/jop.2000.71.5-S.870. [DOI] [PubMed] [Google Scholar]
- 18.Lindhe J, Berglundh T, Ericsson I, et al. Experimental breakdown of peri-implant and periodontal tissues. A study in the beagle dog. Clin Oral Implants Res. 1992;3:9–16. doi: 10.1034/j.1600-0501.1992.030102.x. [DOI] [PubMed] [Google Scholar]
- 19.Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29(Suppl 3):197–212. doi: 10.1034/j.1600-051x.29.s3.12.x. discussion 232-193. [DOI] [PubMed] [Google Scholar]
- 20.Buser D, Janner SF, Wittneben JG, et al. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res. 2012;14:839–851. doi: 10.1111/j.1708-8208.2012.00456.x. [DOI] [PubMed] [Google Scholar]
- 21.Aljateeli M, Fu JH, Wang HL. Managing peri-implant bone loss: current understanding. Clin Implant Dent Relat Res. 2012;14(Suppl 1):e109–e118. doi: 10.1111/j.1708-8208.2011.00387.x. [DOI] [PubMed] [Google Scholar]
- 22.Aoki M, Takanashi K, Matsukubo T, et al. Transmission of periodontopathic bacteria from natural teeth to implants. Clin Implant Dent Relat Res. 2012;14:406–411. doi: 10.1111/j.1708-8208.2009.00260.x. [DOI] [PubMed] [Google Scholar]
- 23.Mombelli A, Marxer M, Gaberthuel T, et al. The microbiota of osseointegrated implants in patients with a history of periodontal disease. J Clin Periodontol. 1995;22:124–130. doi: 10.1111/j.1600-051x.1995.tb00123.x. [DOI] [PubMed] [Google Scholar]
- 24.Salvi GE, Furst MM, Lang NP, et al. One-year bacterial colonization patterns of Staphylococcus aureus and other bacteria at implants and adjacent teeth. Clin Oral Implants Res. 2008;19:242–248. doi: 10.1111/j.1600-0501.2007.01470.x. [DOI] [PubMed] [Google Scholar]
- 25.Marotti J, Tortamano P, Cai S, et al. Decontamination of dental implant surfaces by means of photodynamic therapy. Lasers Med Sci. 2013;28:303–309. doi: 10.1007/s10103-012-1148-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Renvert S, Samuelsson E, Lindahl C, et al. Mechanical non-surgical treatment of peri-implantitis: a double-blind randomized longitudinal clinical study I: clinical results. J Clin Periodontol. 2009;36:604–609. doi: 10.1111/j.1600-051X.2009.01421.x. [DOI] [PubMed] [Google Scholar]