Abstract
Objective: The aim of the study is to determine whether in Belgium dentists feel confident to diagnose a medical emergency situation in their dental practice. Methods: A questionnaire was completed by 7.0% of the active Belgian general dental practitioners (n = 548) including questions on the frequency and knowledge of medical emergency situations in the dental office, history of dental training to treat emergency situations and confidence level in treating emergency situations. Results: A medical history of each patient was taken by 55.3% of the dentists. A link was found between years since graduation and the systematic decline of a medical history in a new patient (P = 0.001): the older the dentist, the less consistent was the updating of medical history. Almost 50% of the dentists (49.4%) never participated in any basic life support (BLS) training during their undergraduate education. Moreover, 78.3% never had any paediatric BLS training during undergraduate education and BLS training after graduation was lacking by 37.2% of the dentists. Conclusion: Knowledge of BLS should be fundamental to medical professionals. The more BLS training a practitioner has experienced, the more self-secure they feel coping with an emergency situation.
Key words: Basic life support (BLS) training, dentist and medical emergency situations, dentists and medical history
INTRODUCTION
Data concerning the prevalence of medical emergencies in dental practice are scarce. However, if medical emergencies do happen, dentists may need to cope with life-threatening situations1. In Western society life expectancy increases and so health-care workers are faced with an older population with more chronic illness, greater intake of medication and an increased risk of drug interaction and adverse effects. As a result, the older patient is at greater risk of a medical emergency during and after dental treatment2.
It is obvious that dental treatment can increase the possibility of a medical emergency situation3 because of ‘emotional stress’ on the patient’s ability to cope with dental treatment procedures, the use of local anaesthetics and surgical treatments. Greenwood described that medical emergencies during dental treatment are more common in a hospital environment than in a private dental setting but indicated that the same problems are found in both4. Every dentist can expect to be involved at some time in an emergency situation directly or indirectly related to dental treatment5.
A 10-year survey in the UK on the occurrence of emergency situations revealed that, in dental practice, vasovagal syncope is the most common complication. Dental practitioners indicated that 70.2% of them faced at least one medical emergency situation during 10 years of practice6. A German study by Muller et al.7 revealed that 57% of the dentists faced at least three emergency situations during 1 year. About 36% of the dentists had faced more then 10 emergency situations in the last year. Vasovagal syncope, hypertension, epilepsy, hypoglycaemia and asthmatic attack are indicated as the most common reported problems. In previous reports it is described that, excluding syncope, the incidence of a medical emergency situation in a general dental practice appears to be once every 21to 4 years8 .
The best option to prevent medical complications in the medically compromised population during dental treatment is a multidisciplinary approach. However, in their practice only the dentist is responsible for the medically compromised patient. This responsibility is implemented by the European Union, and described in ‘The Report of the European Advisory Committee on the Training of Dental Practitioners’; ‘Clinical Proficiencies required for the Practice of Dentistry in the European Union’9.
Prevention of medical emergencies during dental treatment is crucial10. This can be done following some fundamental principles. Regular updating of patients’ medical history is mandatory. A thorough medical history should be able to identify most patients at risk and allow necessary adjustments to dental treatment8. The medical history can immediately draw the attention of the dentist to any potential medical emergencies that may arise. It is particularly important to obtain information on known allergies or adverse reactions of medications11. A full knowledge of the medical history of the patient is indispensable in order to reduce, or eliminate potential risks11. Therefore, it is mandatory that the dentist must have a medical history of each patient at his or her disposal10.
Dentists must also be able to diagnose and treat the most common medical emergencies (e.g. syncope), as well as effectively respond to certain less frequent, or even rare, but potentially life-threatening emergencies, particularly with a focus on those that may arise as a result of dental treatment (e.g. anaphylactic reaction to an anaesthetic administered)4. Multiple skills are needed in order to make the correct diagnosis and subsequently start the correct therapy. The dentist should have knowledge of pharmacology, anatomy, physiology, pathology and clinical diagnosis11. However Girdler & Smith1 showed that only 12.9% of the dentists consider themselves competent to make the correct diagnosis of a medical emergency. According to these results, more than 50% of UK dentists provide no appropriate treatment.
The aim of the study is to determine whether the dentists in Belgium feel confident to deal with the threat of a medical emergency situation in their dental practice.
METHODS
A validated questionnaire was distributed before the start of several dental meetings in Belgium. During a 15-minute period dentists filled in the questionnaire, verbal consent was obtained from the participants and the questionnaires were immediately collected. Anonymity of the respondents was respected; the questionnaires were not encrypted. The research was conducted in full accordance with the World Medical Association Declaration of Helsinki.
The survey contained closed questions in different categories: How frequently is each new patient submitted to a medical history and a check on every consultation? What is the prevalence of medical emergencies in private dental practice? Has the dentist ever faced a medical emergency during his/her career as dentist? If so what kind of emergency: ‘vasovagal syncope’, ‘diabetes problem’, ‘seizure attack’, ‘anaphylactic shock’, ‘cardiac arrest’, and ‘non-diagnosed strange reaction of the patient’? The questionnaire also included general and demographic information on dentists and their dental practice.
Questions about self-perception regarding diagnosis and adequate treatment of medical emergency situations in practice were asked. Participants assessed their competencies in diagnostics and treatment skills regarding heart attack, anaphylactic shock, hypertension, airway obstruction, cardiac arrest, epileptic attack, asthma attack and a diabetes problem. The last questions were answered with a value on a Likert scale of 1 (‘completely disagree’) to 6 (‘completely agree’) in response to the statement: ‘I can diagnose my patient in a medical emergency of ….’. This is analogous to the question: ‘I can help my patient in the following emergency of …..’.
The questionnaire was pilot tested before the study. The relevance of questions, response format and phrasing was evaluated. The process resulted in some questions being deleted and rephrased. A test–retest with 10 dentists from different ages/gender and region was performed, with a 6-month interval, to assess the reliability of the questionnaire.
Statistical analysis
The data obtained were systematically collected and missing data noted. For descriptive statistics of the variables, as well as calculating significant differences, SPSS (Statistical Package of Sciences, SPSS Inc., Chicago, IL, USA) for Windows (version 16.0) was used. Non-parametric tests were applied to determine differences between the various categories in order to discover and analyse relationships. Pearson chi-square and Fisher’s exact tests were performed to examine the proposed research questions. Statistical significant difference was determined at P = 0.05.
RESULTS
Demographic data
Five hundred and fifty-eight questionnaires were collected. Some were excluded from the analysis as the respondents were not general dental practitioners (n = 10). A total of 548 questionnaires were eligible for analysis.
Demographic data are shown in Table 1. The vast majority of the participants had a dental practice for more than 20 years in a rural environment (61.1%). About 55.3% of Belgian dentists did implement effectively a medical history for each patient; 26.6% of the dentists ‘usually’ took a medical history, 9.1% sometimes took a medical history and 8.6% never took a medical history. The systematic updating of the medical history of ‘regular’ patients is reported by 27.7% of respondents; 30.3% checked the medical history in most cases on a regular basis, 21.9% of the dentists did it sometimes and 19.2% did not check medical history at all.
Table 1.
Sample distribution of dentists
| Gender | |
| Male | 57.8% |
| Female | 42.2% |
| Profession | |
| Dentist | 100% |
| Working envirronment | |
| Rather rural | 36.1% |
| Rather urban | 25% |
| Small city (+30,000–70,000 inhabitants) | 17.5% |
| City (+70,000 inhabitants) | 21% |
| No response | 0.4% |
| Graduated since | |
| <5 years | 4.2% |
| 5 < 10 years | 6.8% |
| 10 < 20 years | 12.6% |
| 20 < 30 years | 38.3% |
| >30 years | 38.1% |
Table 2 shows the percentage of dentists who faced a medical emergency situation during their professional practice. The prevalence of specific medical emergencies is noted in the second part of the Table.
Table 2.
Prevalence of medical emergency situation in the dental office
| Number of dentists % (n) | |
|---|---|
| Did you had an emergency situation in your dental office? | |
| Yes | 43.6 (239) |
| No | 56 (307) |
| No response | 0.4 (2) |
| If Yes what kind of emergency situation? | |
| Vasovagal syncope | 34.3 (188) |
| Diabetes problem (Hypo-/Hyperglycemia) | 8.4 (46) |
| Epileptic insult | 16.1 (89) |
| Allergic shock | 3.8 (21) |
| Cardiac arrest | 0.4 (2) |
| Emergency situation but no diagnose | 9.3 (51) |
| Others | 6.2 (34) |
The most frequently reported emergency was vasovagal syncope (34.3%), followed by epilepsy and diabetic problems (8.4%). The number of cases of anaphylactic shock (3.8%) and cardiac arrest (0.4%) reported was limited.
Basic life support (BLS)-training
Table 3a shows that only 38.5% of the dentists participated in least one BLS training course during their undergraduate dental training but 49.4% never participated in any BLS training. Only 6.6% of the dentists had BLS training in two or more years of the undergraduate dentist training. Of our sample, 78.3% have never received any paediatric BLS training. Table 3b shows that only 47.5% of the dentists had one or two BLS training sessions after graduation and 37.2% never had BLS training since they were professionally active. Further, 21.4% (n = 117) of the dentists never had any BLS training either during or after graduation. In addition, 42.8% (n = 377) of the dentists never had any paediatric BLS training.
Table 3.
(a) BLS-training and education during undergraduate studies. (b) BLS-training and education after graduation
| Adults (%) | Children (%) | |
|---|---|---|
| (a) | ||
| Never | 49.4 | 78.3 |
| During 1 year | 31.9 | 11.6 |
| During ≥2 years | 6.6 | 3.4 |
| Do not remember | 12.0 | 6.8 |
| (b) | ||
| Never | 37.2 | 78.3 |
| 1–2 times | 47.5 | 17.6 |
| 3–5 times | 12.2 | 3.3 |
| 6–10 times | 1.7 | 0.2 |
| >10 times | 1.5 | 0.6 |
Competences (self perception)
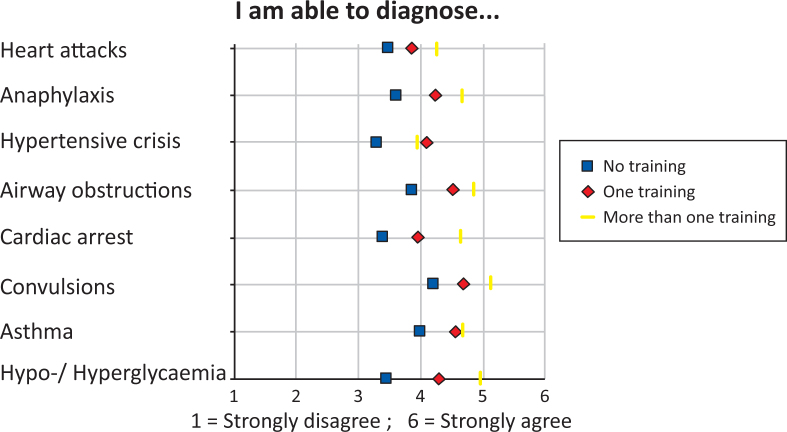
The Likert scale (Figure 1) illustrates how competent the respondents felt to diagnose an emergency situation according to their respective training.
Figure 1.
Level of competence to diagnose the emergency situation.
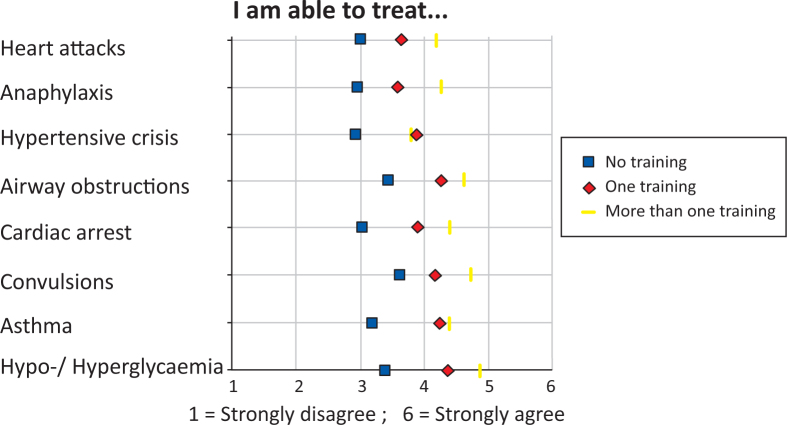
Figure 2 shows the average extent to which the dentists thought, as a result of their training, they were able to offer assistance to a patient who needed medical attention. The same result was found in being able to make a diagnosis. In particular, the more training the practitioner has experienced, the more secure the dentist felt. However, the diagnosis of hypertension was an exception.
Figure 2.
Confidence level of the dentist to treat the emergency according to specific training.
In our study no link could be detected between systematic updating of the medical history of patients and the occurrence of a medical emergency (P = 0.92). A relation was found between the years since graduation and the systematic decline of taking a medical history in new patients (P = 0.001), and the older the dentist, the less consistent the updating of medical history. More than 1 in 10 (11.1%) of the dentists who graduated more than 30 years ago do not take any medical history at all.
DISCUSSION
This paper aimed to determine whether dentists in Belgium feel confident in having the knowledge to make diagnoses and the relevant skills to help a patient in a medical emergency. The nature of the most common emergencies was also reported. Similar studies are found in the literature but most often these point to limited skills in cardiopulmonary resuscitation. Other emergency situations such as anaphylactic shock, diabetes problem, epilepsy, etc., have only been studied in the UK11. Taking into account the differences in education and training in dentistry in different countries and the differences in dental practice management and the legal aspects in each country, it is difficult to compare the results obtained. Results from a Belgian pilot study, conducted in 2008 in order to validate the questionnaire, indicated a possible lack of knowledge of BLS in Belgium. However, the sample size was too small to draw well-founded conclusions and was therefore succeeded. The questionnaire used in the current study reached dentists of all ages and included both recent graduates and dentists who graduated more than 30 years ago. Dentists were spread around the country with a balanced distribution between rural and urban situated practices. In the year 2010, 7,794 general dental practitioners were active in Belgium12. Our sample consists of 548 respondents. Thus our manuscript describes a representative sample (7.03%) in regard to the current Belgian general dentist population.
Using a questionnaire one must be aware of the so-called ‘response bias’. Anonymity of the responders of the questionnaire had to restrict this form of bias13. Often, a tendency to answer in a desirable social way can influenced the results. Therefore, especially when personal competences are involved, embarrassment, responsibility and reluctance play a role.
Unlike similar studies, this survey takes an overview of the entire dental career of the respondents to date. By interpretation of the results, difference between the ‘self-rated’ and the actual control of specific skills should be clear. However, the magnitude and scope of the present study did not include any test of practical ability and/or knowledge. The latter could show differences in results14 and further research in Belgium is needed.
It should be clear that any dentist can expect to be involved in the diagnosis of, if not treating, medical emergencies4. Of the dentists, 43.6% will face at least one medical emergency during their career. Müller et al.7 however, indicated that 57% of the German dentists faced one to three medical emergencies during a study period of only 12 months. In addition, 36% of the German dentists faced 10 emergency situations.
Almost half of the dentists in Belgium had already faced a medical emergency in their practice, but in most cases these were not life-threatening. Only a small percentage of dentists participating this study followed repeated BLS training and were confident to respond adequately to a possible emergency situation. The vast majority considered themselves poorly prepared and this indicates a need for advanced training.
In Belgium, vasovagal syncope is by far the most frequently reported emergency situation in dental practice (34.4%). This corresponds with previous report6. Anaphylactic shock and cardiac arrest were very rarely reported (i.e. by 3.8% and 0.4%, respectively, of the respondents). However, cardiac arrest is the main item in BLS training.
With the exception of hypertension, it is clear that the more a dental practitioner is trained, the more competent they consider themselves to diagnose a problem. These results indicate that practitioners who are trained only once feel more self-confident compared with multiply-trained practitioners. Epileptic attack, diabetes problem and airway obstruction appear to be the easiest problems to diagnose.
It should be noted that in the present study, the number of emergencies per dentist per year was not asked for. This manuscript is a survey of the whole career of the dentist, with a focus whether or not a particular emergency situation had occurred, regardless of the frequency of each type. In the current study it was therefore not possible to determine out the relative incidence of certain emergencies.
Haas8 and Abraham-Inpijn15 indicated that a thorough medical history should be available for each individual patient. A medical history can help to reduce the risk of emergencies4. It is clear that, in Belgium, medical history is taken far less frequently than is acceptable in the literature. Possible explanation could be the relatively very low exposure rate to life-threatening emergencies in a dental office.
Although no correlation between the regular updating of medical history and the occurrence of a medical emergency was found, it is encouraging to note that younger dentists take and update the medical history of their patients more frequently than do their older colleagues.
Since 2010 Belgium has a system that includes continuing education for the general dental practitioners to maintain their professional licence16. However BLS training and education appear to be, until now, not obligatory, although the lack of BLS knowledge should be incompatible with a medical profession.
Limited data were found on an international level regarding the training and knowledge of dental general practitioners and BLS training. It could be interesting to make comparisons with other nations regarding this fundamental medical topic, especially with regard to the worrying nature of the findings in Belgium.
Repetition of BLS training on a regular basis is important. Each dentist has a responsibility to identify medical emergencies and provide first aid. From the results of the questionnaire it can be concluded, however, that emergency situations are rare and seldom life-threatening, and that Belgian dentists are aware of a lack of knowledge, training and skills in an emergency situation. For a medical professional, knowledge of BLS should be fundamental. Additional and repeated training in BLS is necessary to develop the skills needed to cope with medical emergencies and adverse events in dental practice.
Acknowledgement
The authors are grateful to the general dental practitioners that participated in the study.
Competing interest
None declared.
REFERENCES
- 1.Girdler NM, Smith DG. Prevalence of emergency events in British dental practice and emergency management skills of British dentists. Resuscitation. 1999;41:159–167. doi: 10.1016/s0300-9572(99)00054-4. [DOI] [PubMed] [Google Scholar]
- 2.Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in Great Britain. Part 2: drugs and equipment possessed by GDPs and used management of emergencies. Br Dent J. 1999;186:125–130. doi: 10.1038/sj.bdj.4800040. [DOI] [PubMed] [Google Scholar]
- 3.Broadbent JM, Thomson WM. The readiness of New Zealand general dental practitioners for medical emergencies. N Z Dent J. 2001;97:82–86. [PubMed] [Google Scholar]
- 4.Greenwood M. Medical emergencies in dental practice. Dent Update. 2009;36:202–211. doi: 10.12968/denu.2009.36.4.202. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg M. Preparing for medical emergencies: the essential drugs and equipment for the dental office. J Am Dent Assoc. 2010;141(S):14–19. doi: 10.14219/jada.archive.2010.0351. [DOI] [PubMed] [Google Scholar]
- 6.Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in Great Britain. Part 1: their prevalence over a 10-year period. Br Dent J. 1999;186:72–79. doi: 10.1038/sj.bdj.4800023. [DOI] [PubMed] [Google Scholar]
- 7.Muller MP, Hansel M, Stehr SN, et al. A state-wide survey of medical emergency management in dental practices: incidence of emergencies and training experience. Emerg Med J. 2008;25:296–300. doi: 10.1136/emj.2007.052936. [DOI] [PubMed] [Google Scholar]
- 8.Haas DA. Emergency drugs. Dent Clin North Am. 2002;46:815–830. doi: 10.1016/s0011-8532(02)00027-7. [DOI] [PubMed] [Google Scholar]
- 9.http://www.erc.edu (Brussels, 4 June 1996;XV/E/8316/8/93). Accessed 23 December 2012
- 10.Abraham–Inpijn L. Elsevier Gezondheidszorg; Maarssen: 2000. Voorkomen Van Medische Accidenten Voor Het Medisch Risico Registrerend Anamnesesysteem (MRRA) [Google Scholar]
- 11.Kogan S. Medical emergencies for dentists. Oral Surg Oral Med Oral Pathol. 1958;11:359–363. doi: 10.1016/0030-4220(58)90072-0. [DOI] [PubMed] [Google Scholar]
- 12.www.health.belgium.be/filestore/19081317_NL/STATAN2011NLversionTVV.pdf. Accessed 10 April 2013
- 13.Verstraete B. Het sociaal wenselijk antwoorden bij adolescentie-enquêtes. Inter-universitaire scriptie, Leuven, Jeugdgezondheidszorg, Katholieke Universiteit Leuven, 2008
- 14.Atherton GJ, McCaul JA, Williams SA. Medical emergencies in general dental practice in Great Britain. Part 3: perceptions of training and competence of GDPs in their management. Br Dent J. 1999;186:159–167. doi: 10.1038/sj.bdj.4800073. [DOI] [PubMed] [Google Scholar]
- 15.Abraham-Inpijn L, Russell G, Abraham DA, et al. A patient-administered Medical Risk Related History questionnaire (EMRRH) for use in 10 European countries (multicenter trial) Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:597–605. doi: 10.1016/j.tripleo.2007.09.032. [DOI] [PubMed] [Google Scholar]
- 16.http://www.health.fgov.be/eportal/Healthcare/healthcareprofessions/Dentists/Accessandpracticeoftheprofessi/Acquiringandmaintainingthetitle/index.htm?fodnlang=en. Accessed 10 April 2013