Abstract
The aim of this study was to test the hypothesis that the conventional restorative treatment (CRT) and the atraumatic restorative treatment (ART) protocols, in comparison with the ultra-conservative treatment (UCT) protocol, would increase the quality of life of children over a period of 1 year. Cavitated primary molars of 302 children 6–7 years of age were treated according to the CRT, ART and UCT protocols at the school compound. Children’s parents completed the Brazilian version of the Early Childhood Oral Health Impact Scale (B-ECOHIS) at baseline and one year later. Paired t-test, Chi-square test and anova were applied in analysing the data. Questionnaires from 277 and 160 children were collected at baseline and after 1 year, respectively. A statistically significant difference in B-ECOHIS scores over the 1-year period was found for domains ‘child symptoms’ (P = 0.03) and ‘child psychology’ (P = 0.02). Treatment protocols did not statistically significantly influence the changes in B-ECOHIS scores over the 1-year period (P = 0.78). It can be concluded that the UCT protocol was as good as the two restorative protocols. All treatment protocols were effective in reducing children’s experience of pain, their sleeping problems and their irritability and/or frustration levels over the 1-year period.
Key words: Quality of life, dental caries, children, atraumatic restorative treatment, early childhood oral health impact scale
INTRODUCTION
It is well accepted that assessing the oral health of people exclusively through quantitative measurement is insufficient for answering all questions relevant to public oral health practice and knowledge1. A simple way of reporting such measurements is through the use of the decayed, missing, filled teeth (DMFT) index. The final outcome, usually represented by a mean score, shows the magnitude of dental caries, but not the impact of that magnitude on the daily life and general health of the individual2. Therefore, socio-dental assessment of oral needs, including quality of life, is considered important for health planners in developing policies that can greatly enhance oral health3.
Understanding how people perceive the impact of oral health on their lives has become a topic of interest in the dental community during the past decade. In this time a number of different oral health problems, such as toothache, cavitated dentine lesions4., 5. temporomandibular disorder, tooth loss and dry mouth6, have been associated with a poorer quality of life. In addition, non-dental conditions, such as socio-economic aspects, have also been linked to lower oral-health-related quality of life (OHRQoL) scores7. Difficulty in eating and sleeping exemplify daily activities that can be negatively influenced by oral health problems5., 8. and can negatively influence the overall quality of life of children, adolescents, adults and the elderly9., 10., 11..
In relation to dental caries, most of the published research has focused on the impact of the disease and its consequences for the individual’s daily performance, showing an association between dental caries and poorer OHRQoL4., 5.. But what would the effect of providing curative care be on the OHRQoL? Tanzanian adolescents with pain-associated dental caries lesions reported an improvement in OHRQoL 6 months after being treated10. The best result was obtained when restorative treatment was accompanied by tooth extraction. This might indicate that tooth cavities, per se, are not entirely relevant to improved OHRQoL in the absence of pain. This outcome is in line with the results of an investigation that aimed to assess the impact of cavitated dentine lesions, toothache, history of extraction and the presence of fistulae and abscesses on young children’s OHRQoL. The study showed that of the caries-related variables studied, cavitated dentine lesions had less impact than the others on the children’s OHRQoL, according to the parents’ perceptions5. Therefore, the decision was made to investigate how the treatment of those cavities would affect childrens’ quality of life.
In 2008, a trial started in which cavities in primary molars were treated according to three treatment protocols: conventional restorative treatment (CRT), atraumatic restorative treatment (ART) and ultra-conservative treatment (UCT). The last protocol consisted of restoring small cavities with ART and brushing medium- and large-sized cavities plaque-free with toothbrushes and fluoridated toothpaste under supervision12. It was thought that the two restoration groups would experience a higher quality of life over a period of 1 year. The hypothesis was, therefore, that over a period of 1 year the quality of life of children treated according to the CRT and the ART protocols would increase more than that of those treated according to the UCT protocol.
MATERIALS AND METHODS
Sampling procedure
The study was implemented in Paranoá, a low-socio-economic suburban area of Brasilia, Brazil. An oral health epidemiological survey assessed the prevalence of dental caries and its severity, using ICDAS II, among Grade 1 school children. A sample was then drawn from children with good general health and at least two cavitated dentine carious lesions in primary molars13., 14.. The sample was used for comparing three different treatment protocols in a controlled clinical trial using a parallel group design. The research protocol was approved by the Human Ethics Committee of the University of Brasília Medical School (reference no. 081/2008), registered at the Dutch Trial Registration Centre (reference no. 1699) and was conducted in full accordance with the World Medical Association Declaration of Helsinki. An informed consent document explaining the nature of the investigations was signed by one of each child’s parents or their carer.
The three treatment protocol groups for managing cavitated dentine lesions in primary teeth were: CRT and ART as the control groups and UCT as the test group. All six public schools in Paranoá were enrolled in the study. Children were from the same socio-economic background. As a dental unit equipped with rotary equipment was present in two of the six schools; these schools were allocated to the CRT group. The remaining four schools were randomly allocated to the ART and UCT groups, using the toss of a coin. At baseline, no statistically significant differences were observed in gender, mean dmft- and mean DMFT-scores, and type of surface among the children in the three treatment protocol groups12.
Provision of treatment
Treatment was performed by three trained and calibrated paedodontists, aided by trained dental assistants, on school premises during May and July 2009. Before provision of curative treatment, children were given an oral hygiene kit and instructed how to apply the toothbrush and fluoridated dentifrice properly, as well as the specially provided plaque-disclosing dentifrice. They were also educated about healthy and bad dietary habits. This health information was also contained in brochures that were provided to the parents; see de Amorim et al.12, for further information about the trial.
In the CRT protocol dentine carious cavities in primary molars were treated with rotary instruments and restored with amalgam (Permite Regular set®; SDI, Melbourne, Victoria, Australia). Cavity outlines were prepared according to Black’s principles, but without extension for prevention. A slow, round bur was used for removing demineralised dentine. Suction was used during preparation and filling of the cavity.
In the ART protocol dentine carious cavities in primary molars were accessed and cleaned with hand instruments only (ART Kit®; Henry Schein, Chicago, IL, USA), conditioned for 10 seconds with a wet cotton wool pellet saturated with the glass-ionomer liquid, washed for 5 seconds and dried for 5 seconds with cotton wool pellets and restored using a high-viscosity glass-ionomer (Ketac Molar Easymix®; 3M ESPE, Seefeld, Germany). The chair-side assistant mixed the glass-ionomer with a metal spatula on a glass plate in accordance with the manufacturer’s instructions. The glass-ionomer was inserted into the cavity in a few increments, using an applier/carver instrument (ART Kit; Henry Schein), overfilled and pressed down by a finger covered in a thin layer of petroleum jelly. The bite was checked and the applier/carver ART instrument was used in removing excess material.
In the UCT protocol small dentine carious cavities in primary molars were treated according to the ART approach, in the same manner as used for the ART treatment protocol. Medium-sized single and multiple-surface dentine carious cavities of symptomless primary molars were enlarged, by extending their edges with a hatchet (ART Kit; Henry Schein). In this way, cavities were made easily accessible, facilitating plaque removal in aproximal surfaces, through a bucco-lingual technique of brushing with a fluoridated dentifrice. Large dentine carious cavities in symptomless primary molars were left open and cleaned in the same way as medium-sized cavities. A trained dental assistant supervised the tooth brushing on school days during the trial period. The classification of cavity size in primary molars was based on a previous study15.
In each treatment protocol group local anaesthesia was administered when the child indicated pain or whenever the operator judged it necessary. In deep cavities, a Ca(OH)2 liner was applied. In proximal cavities, a wooden wedge and steel matrix band (Injecta®; Diadema, São Paulo, Brazil) in a Tofflemire matrix retainer (Golgran®, São Paulo, Brazil) were used. Cotton wool rolls were used for isolating the teeth during restorations.
Oral health-related quality of life assessment
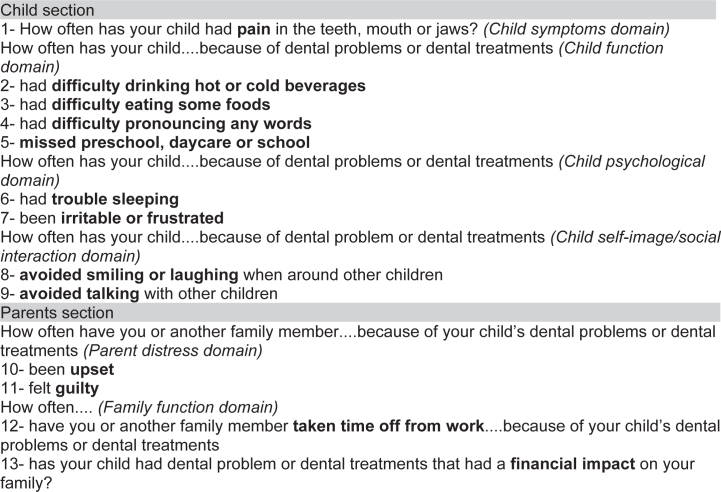
Oral health-related quality of life was assessed, using the Brazilian Early Childhood Oral Health Impact Scale (B-ECOHIS); a questionnaire comprising 13 questions, divided into two sections. The first nine questions are related to the oral health impact on the child’s quality of life (child section), while the last four questions concern the oral health impact on the quality of life of the child’s parents (parents section) (Figure 1). The B-ECOHIS has been validated for use in Brazil from the original ECOHIS16. The latter was created with the aim of providing a short instrument for assessing the impact of oral problems and related treatment experiences on the quality of life, which could be used in epidemiological surveys to discriminate between children with and without dental disease experience17.
Figure 1.
The Early Childhood Oral Health Impact Scale (ECOHIS) questionnaire by child and parent sections and domain group. Response options: 0 = never to 4 = very often, 5 = don’t know17.
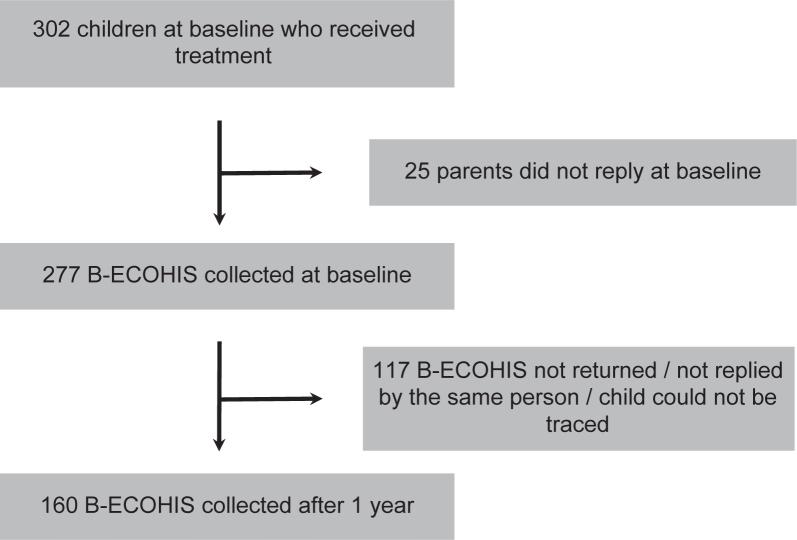
The B-ECOHIS was presented to the parents on two different occasions: (1) at baseline (when the epidemiological survey took place) and (2) at follow-up (1 year after the treatment was provided). Parents were informed that they should complete the questionnaire about the situation after the treatment was performed. On both occasions parents were contacted by telephone, to reinforce the need to fill in the questionnaire. Questionnaires that were returned fully completed by the same person at baseline and follow-up were included in the analysis. The flow diagram of the study is presented in Figure 2.
Figure 2.
Study flow diagram.
Data analysis
A power calculation, using an α of 0.05 and a 1 – β of 0.8, considering an increase in the survival rate of non-restored teeth, from 82%18 to 92% clinically significant, correcting for dependency of restorations of 10% and for an estimated loss-to-follow-up of 8% after 2 years, preceded the sampling procedure. A statistician from the Dental College of the University of Nijmegen, the Netherlands, used SPSS (Chicago, IL, USA) to analyse the data. Differences between the mean scores of the responses from the B-ECOHIS questionnaire obtained at year 1 and at baseline were calculated and tested, using a paired t-test. A chi-square test was used for testing differences between respondents and non-respondents with regard to gender. All other differences between respondents and non-respondents were tested using t-tests. One-way anova was applied in testing for effects of the treatment protocols on the difference in mean B-ECOHIS scores over the 1-year period. A statistically significant difference was set at α = 0.05.
RESULTS
Description of subjects
Of the 302 6- to 7-year-old children who received treatment, 277 (151 boys and 126 girls; 176 6-year-olds and 101 7-year-olds) responded to the B-ECOHIS at baseline. One year later 160 of these children (84 boys and 76 girls) again responded, resulting in a response rate of 57.7%. With regard to age (P = 0.50), gender (P = 0.43), mean d2mfs (P = 0.37), mean d3mfs (P = 0.32), mean D2MFT (P = 0.22), mean D3MFT (P = 0.84), and overall B-ECOHIS domain (P = 0.41), there was no statistically significant effect between respondents and non-respondents. The mean values of caries-related and B-ECOHIS variables at baseline are presented in Table 1. Caries experience in the primary dentition was high. The mean scores for the child and parent domains of the B-ECOHIS were low.
Table 1.
Mean values and standard deviation (SD) of caries-related and the Brazilian version of the Early Childhood Oral Health Impact Scale (B-ECOHIS) variables at baseline
| Baseline | n | Mean | SD |
|---|---|---|---|
| Caries | |||
| d2mfs | 277 | 22.1 | 10.9 |
| d3mfs | 277 | 14.9 | 9.8 |
| D2MFS | 277 | 3.2 | 3.0 |
| D3MFS | 277 | 0.3 | 1.1 |
| B-ECOHIS | |||
| Child symptom | 266 | 1.48 | 1.11 |
| Child function | 271 | 0.69 | 0.72 |
| Child psychology | 270 | 0.86 | 0.98 |
| Child social interaction | 265 | 0.43 | 0.83 |
| Parent distress | 268 | 1.01 | 1.07 |
| Family function | 270 | 0.50 | 0.76 |
Effects of B-ECOHIS over the 1-year period
The mean value of the difference in mean B-ECOHIS scores over the 1-year period, their standard error (SE) and P-value by B-ECOHIS domains are presented in Table 2. A statistically significant difference in mean B-ECOHIS scores over the 1-year period was found for the domains ‘child symptoms’ (P = 0.03) and ‘child psychology’ (P = 0.02). The magnitude of the mean difference in mean B-ECOHIS scores was −0.24 (child symptoms) and −0.21 (child psychology). No statistically significant difference in mean B-ECOHIS scores over the 1-year period for all domains combined was observed (P = 0.40).
Table 2.
Mean value of the difference in mean Brazilian version of the Early Childhood Oral Health Impact Scale (B-ECOHIS) scores between baseline and 1 year later, their standard error (SE) and P-value by B-ECOHIS domains
| Domains | n | Mean | SE | P |
|---|---|---|---|---|
| Difference in child symptom | 153 | −0.24 | 0.11 | 0.03 |
| Difference in child function | 157 | −0.02 | 0.07 | 0.82 |
| Difference in child psychology | 154 | −0.21 | 0.09 | 0.02 |
| Difference in child social interaction | 156 | −0.07 | 0.09 | 0.41 |
| Difference in parent distress | 156 | −0.07 | 0.10 | 0.46 |
| Difference in family function | 155 | 0.06 | 0.08 | 0.45 |
| Difference overall | 160 | 0.05 | 0.08 | 0.40 |
Effect of treatment protocols on the B-ECOHIS
The distribution of children across the treatment protocols was 118 (CRT), 76 (ART) and 83 (UCT) at baseline and 55 (CRT), 47 (ART) and 58 (UCT) 1 year later. The mean value of the difference in mean B-ECOHIS scores over the 1-year period, their standard error (SE) and P-value by B-ECOHIS domain and by treatment protocol are presented in Table 3. Results show no statistically significant effect in the mean difference, in mean B-ECOHIS scores for all the domains over the 1-year period among the treatment protocols (P = 0.78). This implies that there was no difference between the three treatment protocols regarding the B-ECOHIS scores at baseline and 1 year later. The UCT protocol was as good as the two restorative protocols.
Table 3.
The mean value of the difference in mean B-ECOHIS scores between baseline and 1 year later, their standard error (SE) and P-value by B-ECOHIS domains and by treatment protocols
| Domains and protocols | n | Mean | SE | P |
|---|---|---|---|---|
| Difference in child symptom | ||||
| CRT | 52 | −0.27 | 0.18 | 0.77 |
| ART | 44 | −0.32 | 0.16 | |
| UCT | 58 | −0.14 | 0.19 | |
| Difference in child function | ||||
| CRT | 55 | −0.01 | 0.12 | 0.84 |
| ART | 46 | −0.08 | 0.13 | |
| UCT | 57 | −0.01 | 0.11 | |
| Difference in child psychology | ||||
| CRT | 54 | −0.21 | 0.15 | 1.00 |
| ART | 45 | −0.21 | 0.15 | |
| UCT | 56 | −0.21 | 0.16 | |
| Difference in child social interaction | ||||
| CRT | 55 | −0.02 | 0.14 | 0.08 |
| ART | 46 | −0.38 | 0.14 | |
| UCT | 56 | −0.09 | 0.16 | |
| Difference in parent distress | ||||
| CRT | 54 | 0.06 | 0.17 | 0.63 |
| ART | 46 | −0.11 | 0.18 | |
| UCT | 57 | −0.17 | 0.17 | |
| Difference in family function | ||||
| CRT | 54 | −0.13 | 0.13 | 0.06 |
| ART | 45 | 0.34 | 0.17 | |
| UCT | 57 | −0.02 | 0.12 | |
| Difference overall | ||||
| CRT | 55 | −0.04 | 0.11 | 0.78 |
| ART | 47 | 0.01 | 0.11 | |
| UCT | 58 | −0.10 | 0.11 | |
ART, atraumatic restorative treatment; CRT, conventional restorative treatment; UCT, ultra-conservative treatment.
DISCUSSION
Methodology
Although all possible efforts were made to reach all parents of the study children after 1 year, the response rate was only 58%. A higher percentage of questionnaires were collected but some had not been completed by the parent/carer who had responded at baseline. As OHRQoL is based on individual perceptions, in order to avoid bias these questionnaires were excluded. This lowered the number of questionnaires eligible for analyses. The reduced number of questionnaires did not lead to a selective drop-out of children, as the non-response analysis showed. Furthermore, not all questionnaires had been fully completed, which accounts for the different numbers of questionnaires analysed per domain. The analyses have been carried out correctly and the findings of the present study reflect the true situation but, as this was the first time that the ECOHIS was used to detect changes in the OHRQoL after dental treatment, its evaluative properties should be further investigated.
Findings
The hypothesis was not accepted. After 1 year, the quality of life of children treated by the UCT protocol was not worse than that of their peers treated by the two restorative protocols. This was unexpected, as the UCT protocol leaves medium- and large-sized cavities unrestored, which was thought to cause pain during eating and consequently, unpleasant feelings. It appears, therefore, that leaving cavities open but brushing them plaque-free daily does not seem to result in deterioration of the quality of life of school-going children. This finding requires confirmation.
The results of the present study did not show overall improvements in the quality of life of children and their families 1 year after primary molars had been treated according to one of the three treatment protocols. That finding may result from the low mean scores of the child and parent domains, which averaged between ‘never’ and ‘hardly ever’ having problems of different types in their oral cavities.
Studies on the impact of treating cavitated carious lesions on the OHRQoL of children have focused mainly on treatment under general anaesthesia19., 20., 21. and have shown an improvement in the OHRQoL. The fact that children had been treated under general anaesthesia might indicate that parents were very disturbed by the seriousness of their children’s dental problems. It is, therefore, impossible to compare the impacts on the OHRQoL of dental treatments performed under general anaesthesia and those administered in dental clinics and field situations.
The findings of the present study differ from those of the few studies that have dealt with the topic in a dental clinic situation9., 10., 22.. In comparing the outcomes of the present study with those referred to above, some aspects such as the age of the participants, the assessment instrument used, the environment in which the treatment was provided and the severity of dental caries across the population should be considered.
The children in the present study were too young to report the impact of their oral health on their lives. Parents filled in the B-ECOHIS questionnaire, which is reported to be the best proxy-report method to use23. It is known, however, that data covering children, when provided by parents, may be incomplete24. It is possible that in the present study parents were unable to perceive subtle changes in their children’s feelings related to conditions in the mouth over the 1-year period, as parents were not present when the treatment was provided. This may have influenced their interest and perceptions regarding their children’s oral health problems. The subjects in the studies by Mashoto et al.10 and Alves et al.22 were 12–19 years and 12 years, respectively. These studies used different OHRQoL assessment instruments from those used in the present study, namely the child-OIPD10 and CPQ11-1422. Because they were older, the adolescents filled in the questionnaire themselves. This certainly improved the quality of the data collected in the two studies above compared to the present study. Because of the age difference and different use of OHRQoL assessment instruments, comparison of the findings of this study with those of the two other studies mentioned above is not possible.
Cunnion et al.9 investigated children from 2 years to 8 years of age and thus covered the ages of the children in the present study. The children received restorative care at paediatric dental clinics in two medical centres in the USA. Some children were affected by severe early-childhood caries (S-ECC). Parents filled in the newly developed self-report OHRQoL assessment instrument, termed POQL, which is different from the B-ECOHIS used in the present study. The severity of dental caries was much higher in children in the USA than in those in the present study. Unfortunately, the publication does not state whether the treatment was provided under general anaesthesia and does not mention what kind of curative care was offered, which hampers true comparison with the present study. It appears that many different OHRQoL assessment instruments have been used for different age groups, with different levels of caries severity, and, therefore, the findings of the present study cannot be compared meaningfully with those available in the literature. This calls for unity among researchers regarding the OHRQoL assessment instruments to be used in certain age groups.
When the two sections of the B-ECOHIS were analysed separately, it was noted that the parents’ contribution to the final score was greater than the childrens’ contribution. In the former, parents had the opportunity to express their own feelings about their children’s oral health problems and they may have felt guilty25. This is understandable, as the study was performed in a deprived area in which access to dental treatment is almost non-existent for these children. Their inability to pay for their children’s dental treatment elsewhere might have influenced their perceptions even after the treatment was provided free-of-charge. However, this assumption requires further investigation.
There were two domains, ‘child symptoms’ and ‘child psychology’, in which the quality of life improved after treatment. These domains reflected children’s experience of pain, difficulty in sleeping and frustration/irritation because of oral problems. Parents can easily notice such conditions even if they see the children only in the evening hours, as was mentioned in informal talks with children, parents and school staff.
In conclusion, there was no difference between the three treatment protocols regarding changes in the ORHQoL of these children after 1 year. The UCT protocol was as good as the two restorative protocols. All treatment protocols were effective in reducing children’s pain experiences, their sleeping problems and their irritability and/or frustration levels after 1 year. The use of ECOHIS in longitudinal studies should be further investigated.
Acknowledgements
The authors thank the children, parents, directors and teachers of the public schools in Paranoá for participating in the study. They are grateful to FAP-DF (Fundação de Apoio à Pesquisa do Distrito Federal), Brasília, Brazil and the Radboud University Nijmegen, the Netherlands, for financially supporting the study. A special thanks is extended to all dentists and assistants who participated in this study.
CONFLICT OF INTEREST
None declared.
REFERENCES
- 1.Bower E, Scambler S. The contributions of qualitative research towards dental public health practice. Community Dent Oral Epidemiol. 2007;35:161–169. doi: 10.1111/j.1600-0528.2006.00368.x. [DOI] [PubMed] [Google Scholar]
- 2.Al Shamrany M. Oral health-related quality of life: a broader perspective. East Mediterr Health J. 2006;12:894–901. [PubMed] [Google Scholar]
- 3.Sheiham A. Oral health, general health and quality of life. Bull WHO. 2005;83:644–645. [PMC free article] [PubMed] [Google Scholar]
- 4.Gradella CM, Barnabé E, Bönecker M, et al. Caries prevalence and severity, and quality of life in Brazilian 2- to 4-year-old children. Community Dent Oral Epidemiol. 2011;39:498–504. doi: 10.1111/j.1600-0528.2011.00625.x. [DOI] [PubMed] [Google Scholar]
- 5.Leal SC, Bronkhorst EM, Fan M, et al. Untreated cavitated dentine lesions: impact on children’s quality of life. Caries Res. 2012;46:102–106. doi: 10.1159/000336387. [DOI] [PubMed] [Google Scholar]
- 6.Naito M, Yuasa H, Nomura Y, et al. Oral health status and health-related quality of life: a systematic review. J Oral Sci. 2006;48:1–7. doi: 10.2334/josnusd.48.1. [DOI] [PubMed] [Google Scholar]
- 7.Fuentes-García A, Lera L, Sánchez H, et al. Oral health-related quality of life of older people from three South American cities. Gerodontology. 2013;30:67–75. doi: 10.1111/j.1741-2358.2012.00649.x. [DOI] [PubMed] [Google Scholar]
- 8.Abanto J, Carvalho TS, Mendes FM, et al. Impact of oral diseases and disorders on oral health-related quality of life of preschool children. Community Dent Oral Epidemiol. 2011;39:105–114. doi: 10.1111/j.1600-0528.2010.00580.x. [DOI] [PubMed] [Google Scholar]
- 9.Cunnion DT, Spiro A, 3rd, Jones JA, et al. Pediatric oral health-related quality of life improvement after treatment of early childhood caries: a prospective multisite study. J Dent Child. 2010;77:4–11. [PMC free article] [PubMed] [Google Scholar]
- 10.Mashoto K, Astrom AN, Skeie MS, et al. Changes in the quality of life of Tanzanian school children after treatment interventions using the Child-OIPD. Eur J Oral Sci. 2010;118:626–634. doi: 10.1111/j.1600-0722.2010.00776.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee IC, Yang YH, Ho PS, et al. Exploring the quality of life after denture-wearing within elders in Kaohsiung. Gerodontology. 2012;29:e1067–e1077. doi: 10.1111/j.1741-2358.2012.00614.x. [DOI] [PubMed] [Google Scholar]
- 12.de Amorim RG, Leal SC, Mulder J et al. Amalgam and ART restorations in children: a controlled clinical trial. Clin Oral Invest 2013. doi: 10.1007/s00784-013-0955-x. [DOI] [PubMed]
- 13.de Amorim RG, Figueiredo MJ, Leal SC, et al. Caries experience in a child population in a deprived area of Brazil, using ICDAS II. Clin Oral Invest. 2012;16:513–520. doi: 10.1007/s00784-011-0528-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Figueiredo MJ, de Amorim RG, Leal SC, et al. Prevalence and severity of clinical consequences of untreated dentine carious lesions in children from a deprived area of Brazil. Caries Res. 2011;45:435–442. doi: 10.1159/000330531. [DOI] [PubMed] [Google Scholar]
- 15.Topaloglu-Ak A, Eden E, Frencken JE, et al. Two year survival rate of class II composite resin restorations prepared by ART with and without a chemomechanical caries removal gel in primary molars. Clin Oral Investig. 2009;13:325–332. doi: 10.1007/s00784-008-0241-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tesch FC, Oliveira BH, Leão A. Semantic equivalence of the Brazilian version of the Early Childhood Oral Health Impact Scale. Cad Saude Publica. 2008;24:1897–1909. doi: 10.1590/s0102-311x2008000800018. [DOI] [PubMed] [Google Scholar]
- 17.Pahel BT, Rozier RG, Slade GD. Parental perceptions of children’s oral health: the Early Childhood Oral Health Impact Scale (ECOHIS) Health Qual Life Outcomes. 2007;5:6. doi: 10.1186/1477-7525-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Levine RS, Pitts NB, Nugent Z. The fate of 1587 unrestored carious deciduous teeth: a retrospective general dental practice based study from northern England. Br Dent J. 2001;193:99–103. doi: 10.1038/sj.bdj.4801495. [DOI] [PubMed] [Google Scholar]
- 19.Klaassen MA, Veerkamp JS, Hoogstraten J. Young children’s Oral Health-Related Quality of Life and dental fear after treatment under general anaesthesia: a randomized controlled trial. Eur J Oral Sci. 2009;117:273–278. doi: 10.1111/j.1600-0722.2009.00627.x. [DOI] [PubMed] [Google Scholar]
- 20.Gaynor WN, Thomson WN. Changes in young children’s OHRQoL after dental treatment under general anaesthesia. Int J Paediatr Dent. 2012;22:258–264. doi: 10.1111/j.1365-263X.2011.01190.x. [DOI] [PubMed] [Google Scholar]
- 21.Thomson WN, Malden PE. Assessing change in the family impact of caries in young children after treatment under general anaesthesia. Acta Odontol Scand. 2011;69:257–262. doi: 10.3109/00016357.2011.554862. [DOI] [PubMed] [Google Scholar]
- 22.Alves LS, Damé-Teixeira N, Susin C et al. Association among quality of life, dental caries treatment and intraoral distribution in 12-year-old South Brazilian schoolchildren. Community Dent Oral Epidemiol 2012. doi: 10.1111/j.1600-0528.2012.00707.x. [DOI] [PubMed]
- 23.Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children’s health-related quality of life: an analysis of 13,878 parent’s reliability and validity across age subgroups using the PedsQLTM 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5:2. doi: 10.1186/1477-7525-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barbosa TS, Gavião MB. Oral health-related quality of life in children: part III. Is there agreement between parents rating their children’s oral health-related quality of life? A systematic review. Int J Dent Hyg. 2008;6:108–113. doi: 10.1111/j.1601-5037.2007.00271.x. [DOI] [PubMed] [Google Scholar]
- 25.Carvalho TS, Abanto J, Mendes FM, et al. Association between parental guilt and oral health problems in preschool children. Braz Oral Res. 2012;26:557–563. doi: 10.1590/s1806-83242012000600012. [DOI] [PubMed] [Google Scholar]