Abstract
Objective: To evaluate the efficacy of periapical infiltration injection of dexamethasone and morphine in reducing postoperative endodontic pain. Method: Ninety patients participated in this double-blind randomised controlled clinical trial. They were referred to the dental school of Shahid Beheshti Medical University, Tehran, Iran for conventional endodontic treatment of molar teeth. The canals of each tooth were completely prepared with cleansing and shaping. The patients were randomly divided into three experimental groups to receive dexamethasone, morphine or normal saline (1 mL). Patients were then instructed to complete a pain diary 4, 8, 24 and 48 h after the appointment. Statistical analysis consisted of chi-squared test, analysis of variance and Kruskal–Wallis test. Results: There was a statistically significant correlation between dexamethasone or morphine treatment and decreased levels and incidence of endodontic pain at 4, 8 and 24 h, but not at 48 h (P < 0.05). It was also observed that dexamethasone was significantly more effective (56.7% no pain) than morphine (43.3% no pain). Conclusion: Periapical infiltration of dexamethasone and morphine led to a considerable decrease in postoperative endodontic pain during the first 24 h after operation. Dexamethasone was more effective than morphine in pain reduction.
Key words: Dexamethasone, morphine, postoperative pain, endodontic, periapical infiltration injection
INTRODUCTION
Flare-up is a frequently reported complaint, referring to pain or swelling after endodontic operations. This pain may originate from bacterial, mechanical or chemical irritation1. A positive correlation between preoperative and postoperative pain has been reported2. Nearly 40% of patients suffer from pain after endodontic treatments3. Patients usually experience the most severe pain within 12 h after the operation4. However, the severity of pain may vary depending on the nature of the insulting agent and the endurance of periradicular tissues5.
Debridement and shaping of the root canal system can harm periapical tissues, and may unintentionally allow bacteria and bacterial products, necrotic pulp tissue or caustic irrigating solution to enter through the apical foramen. This may result in a vascular response to tissue damage, including the release of inflammatory mediators, such as prostaglandins and leucotrienes, which, in turn, will trigger pain fibres6., 7., 8..
During an operation, pain can be managed effectively by anaesthetic techniques; however, postoperative pain is a matter of concern, and the minimisation of a patient’s discomfort postoperatively is necessary9. In an attempt to eliminate, or at least abate, postoperative pain, several methods have been employed. These methods include the use of intracanal medications or systemic medications, such as narcotic analgesics, steroids or nonsteroidal anti-inflammatory agents10. Antibiotics have also been proposed as a solution, mainly because of the role of microorganisms in infected root canal systems11.
In situations in which pain stems from chronic inflammation, a flood of primed immune cells, cytokines and other inflammatory mediators is involved. This postoperative pain can be controlled with steroids, such as dexamethasone, a synthetic glucocorticoid with anti-inflammatory activity, by preventing the release of inflammatory mediators9., 12., 13.. These drugs can be delivered orally, or by intraligamentary, intraosseous and intramuscular injection14.
Opioids have been used to ease pain for many years. According to many studies, the use of morphine in any location close to nerve fibres results in anaesthesia because of the presence of opioid receptors from the trigeminal ganglion to the free pulpal nerve endings. The opioids bind to specific receptors, and thereby subdue the synaptic chemical transmissions and hinder pain perception in higher centres15., 16.. Some studies have reported that endodontic and inflammatory pain can be reduced by intraligamentary injection of morphine17., 18.. The pain-relieving effects of morphine in inflammatory periradicular teeth have been shown to be the result of a reduction in the speed of nerve impulse transmission, which prevents the release of chemical mediators, such as substance P19. Shantiaee and Soluti20 have shown that both morphine and lidocaine have long-lasting effects on C-fibres; however, morphine has only a short-term effect in 33.3% of cases. In inflammatory situations in which lidocaine blocks A-fibre transmission, morphine can increase the stimulation threshold and reduce the velocity of transmission.
Few studies have evaluated the effects of periapical infiltration injection with dexamethasone in the prevention and control of postendodontic pain after root canal instrumentation21., 22.. To date, no study has assessed the effects of the supraperiostal form of injection of morphine on postoperative endodontic pain.
The purpose of this study was to evaluate the efficacy of periapical infiltration injection of dexamethasone and morphine versus placebo in reducing postoperative endodontic pain.
METHODS
The study protocol was approved by the Ethics Committee of Shahid Beheshti Medical University, Tehran, Iran. Ninety patients, aged 18–42 years, participated in this double-blind randomised controlled clinical trial. They were initially referred to the dental school of Shahid Beheshti Medical University for conventional endodontic treatment of maxillary and mandibular molar teeth because of exposure, inflammation or necrosis of the pulp.
Inclusion criteria
Patients who were in a healthy condition [American Society of Anesthesiologists (ASA) I or II], required endodontic treatment in upper or lower molar teeth, had no history of root canal therapy and had signed a human subject committee approved consent form were included in this study.
Exclusion criteria
Patients who had taken analgesic or anti-inflammatory drugs within the last 8 h, had an acute endodontic or periodontal abscess or any periodontal diseases, required prophylactic antibiotics, were pregnant or lactating, had mental disabilities, had systemic diseases that contraindicated endodontic therapy, had an active infectious process or had sensitivity or adverse reactions to dexamethasone were excluded from this study. In order to avoid the high risk of postoperative pain resulting from over-instrumentation, the treatment of teeth having incompletely formed apices was excluded.
Prior to treatment, a careful medical and dental history was taken. Preoperative data for each case were recorded in the patient’s chart, including age, sex, pulp vitality and intensity and duration of pain if present. Sensitivity to percussion and condition of the periapical tissues (with or without radiolucency) were also noted.
The severity of pain was measured by the visual analogue scale modified by Torabinejad et al.23 According to this scale, the level of pain was documented by the operator in the range 0–9. Zero represented no pain, 1–3 denoted mild pain, 4–6 denoted moderate pain and 7–9 indicated severe pain.
In each case, after the administration of local anaesthesia and application of a rubber dam, an access cavity was prepared. All canals were prepared using a step-back flared technique. The root canals were instrumented with a No. 25 K file, or larger instrument, according to the size of the canal, with thorough irrigation with 2.5% sodium hypochlorite. Each root canal was instrumented at 1 mm short of the radiographic apex.
Treatments were performed using a two-visit technique. The canals were completely prepared with cleansing and shaping at the first visit. The pulp chamber was closed with a cotton pellet and Cavit, and no intracanal medicament was used. Obturation was performed at the second appointment.
Patients were randomly assigned to three experimental groups. Each group received a similar supraperiosteal manner of injection in the buccal vestibule and close to the root apex of the target tooth. After this, the drug was deposited slowly. Group 1 received 1 mL of normal saline, Group 2 received 1 mL (4 mg) of dexamethasone (8 mg per 2 mL; Darupakhsh Pharmaceutical Co., Tehran, Iran) and Group 3 received 1 mL (1 mg) morphine (0.1 mL morphine and 0.9 mL sterile water) (10 mg per 1 mL; Tolidaru, Tehran, Iran). The patients were instructed to take rescue medication (500 mg acetaminophen) when needed and to record in a diary each time the medication was used.
The administration was double-blind; the agent was unknown to the patient and to the operator. The three agents were coded by an uninvolved party and the code was not broken until completion of the study.
Patients were instructed to complete a pain diary assessing their level of pain after 4, 8, 24 and 48 h following the appointment. They were asked to rate the degree of inter-appointment pain based on a modified visual analogue scale. The levels of pain included none, mild, moderate and severe.
All data were entered into an SPSS computer analysis system (SPSS Inc., Chicago, IL, USA), and statistical analysis, consisting of chi-squared test, analysis of variance (ANOVA) and Kruskal–Wallis test, was performed. Tests were considered to be statistically significant when P < 0.05.
RESULTS
The sample was evenly distributed in terms of gender, pulp and periapical condition, group of involved teeth and presence of pretreatment pain, with no significant difference between the groups (Table 1). The level of preoperative pain for all patients was almost similar. No statistically significant difference was found among the groups for the number of anaesthetic cartridges used or duration of treatment.
Table 1.
Demographic and clinical features
| Variable | Group 1 (placebo) | Group 2 (dexamethasone) | Group 3 (morphine) |
|---|---|---|---|
| (n = 30) | (n = 30) | (n = 30) | |
| Gender (%) | |||
| Male | 36.7 | 30 | 33.3 |
| Female | 63.3 | 70 | 66.7 |
| Pulp status (%) | |||
| Vital | 80 | 80 | 73.3 |
| Nonvital | 20 | 20 | 26.7 |
| Teeth (%) | |||
| Upper | 60 | 53.3 | 50 |
| Lower | 40 | 46.7 | 50 |
| Presence of pretreatment pain (%) | 100 | 96.7 | 96.7 |
| Presence of periapical radiolucency (%) | 20 | 26.7 | 23.3 |
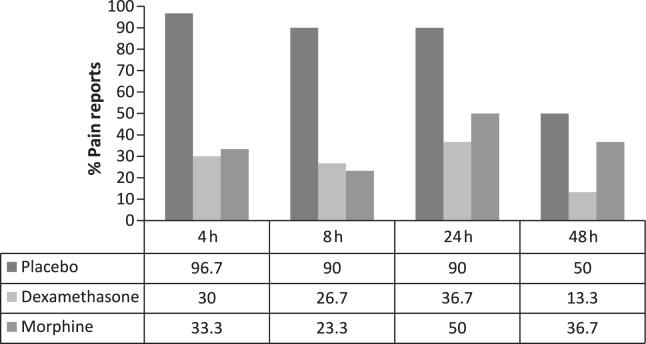
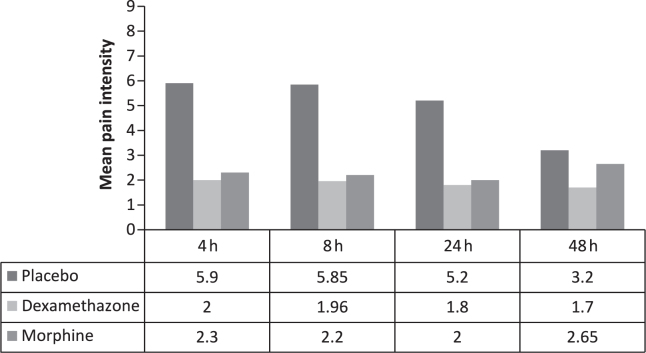
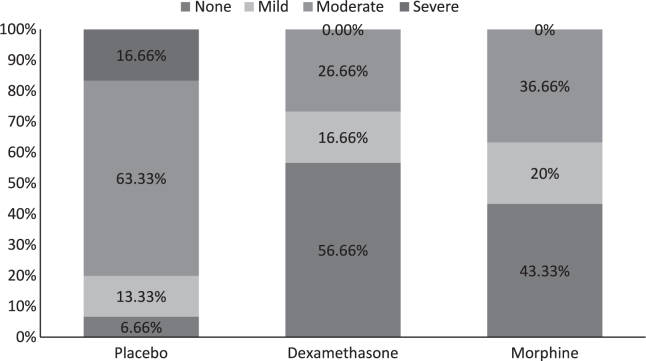
The efficacy of the different medications used to control postoperative endodontic pain is represented in Figures 1 and 2. Dexamethasone and morphine treatment were associated with significantly lower levels of pain, and also a decreased incidence of endodontic pain at 4, 8 and 24 h after operation. No statistically significant difference was observed in the level of pain at 48 h. In terms of the treatment of postoperative endodontic pain, dexamethasone proved to be more effective (56.7% reported no pain) than morphine (43.3% reported no pain) (P < 0.05).
Figure 1.
Percentage of pain reported at each interval in the placebo, dexamethasone and morphine groups.
Figure 2.
Mean pain intensity in each group at each time point.
With the aim of estimating the relative risk, the incidence of each pain category (no pain, mild, moderate and severe pain) was assessed separately without considering the initiation point of pain (Figure 3). The prevalence and severity of pain were significantly lower in the groups treated with dexamethasone and morphine.
Figure 3.
Percentage of none, mild, moderate and severe postoperative pain in the placebo group without consideration of the onset of pain.
The relative risks for moderate to severe pain in patients receiving dexamethasone and morphine injection were 1 : 3 and 1 : 2, respectively. This indicates that the incidence of moderate to severe pain would have been considerably higher if patients had not received these injections.
The number of analgesic tablets (rescue medication) taken by volunteers was significantly different among the groups (P < 0.05), and the largest amount of medication was taken in the placebo group (Table 2).
Table 2.
Frequency of over-the-counter medication use after treatment
| Medication drug | Supplement medication | No supplement medication | Total |
|---|---|---|---|
| Placebo | 24 (80%) | 6 (20%) | 30 (100%) |
| Dexamethasone | 8 (26.6%) | 22 (73.4%) | 30 (100%) |
| Morphine | 11 (36.6%) | 19 (63.4%) | 30 (100%) |
| Total | 32 | 58 | 90 |
Dexamethasone and morphine proved to be more efficacious for the upper than lower teeth. Pulp and periapical conditions did not exhibit any significant correlation with the efficacy of dexamethasone or morphine.
Less than 10% of patients in the morphine group reported nausea. In addition, less than 10% of patients in the dexamethasone group experienced dizziness.
DISCUSSION
The results of this study showed that a periapical infiltration of 4 mg of dexamethasone or 1 mg of morphine decreased considerably postoperative endodontic pain at 4, 8 and 24 h after operation. A visual analogue scale was used in this study. This scale is believed to be valid and sensitive, and has been used in previous studies21., 23..
Our results, indicating a reduction in pain on administration of dexamethasone or morphine, are in agreement with other studies9., 10., 17., 18., 19., 21.. This anti-pain effect gradually receded after the first day, so that no significant effect was perceived after 48 h. Such a duration of effect seems to be sufficient for the relief of postendodontic pain, as it has been shown that the pain reaches its maximum within the first 24 h after operation9., 10., 23..
Dexamethasone is a powerful anti-inflammatory agent that can reduce postendodontic pain, as described in previous studies10., 24., 25., 26.. Marshall et al.9 have reported that the administration of 4 mg of dexamethasone considerably decreases postoperative endodontic pain. Although dexamethasone may hamper the immune process against microorganisms, it has been shown to be harmless in short-term treatments27.
Opioid receptors are present in the peripheral nerve endings of afferent neurones18. Thus, blockade of these receptors by locally administered opioids, such as morphine, may induce analgesia. In this study, 1 mg of morphine was administered, a dosage that has been proven to have no systemic effect28.
The consumption of supplemental medication is an indicator of endodontic pain because, when the drugs had an insufficient analgesic effect, rescue medication was taken to diminish the pain. From our results, patients in the placebo group took more rescue medication, especially at 4 h after the operation. This result confirms that morphine and dexamethasone have an analgesic effect after endodontic operations22., 29..
At all time points, dexamethasone relieved pain more effectively than morphine, a result that is in agreement with the study of Campbell and Kendrick30. The relatively weak local effect of morphine can be attributed to innervation at the site of injection or to the lower activity of the receptors at the injection site. No case of severe pain was reported in either group. With regard to the incidence of pain, dexamethasone more effectively decreased the incidence of pain than morphine after 4, 24 and 48 h. The time point of 8 h after operation was the only point at which morphine proved to be more effective in reducing the incidence of pain. The most considerable differences in the alleviating features of dexamethasone and morphine were recorded at the 24-h and 48-h time points.
The efficacy of both dexamethasone and morphine was higher in the upper teeth. The incidence of side-effects in the upper teeth was also higher after injection of these drugs. This may be related to the trabecular structure of the maxillary bone, enhancing the ability of the drugs to enter the bloodstream. Supraperiostal administration, the technique used in this study, possesses several advantages, such as a simple procedure of injection, less discomfort and anxiety for the patient, and a minimum need for extra armamentarium21.
Although antibiotics were not used in this study, no infectious complication was noted in any of the experimental groups. As suggested by previous studies, infections do not develop after the short-term use of steroids in uninfected patients9. Two side-effects, slight nausea and dizziness, were observed in the morphine and dexamethasone groups, respectively. Nausea after the consumption of morphine has also been reported in the study by Campbell and Kendrick30.
Although many factors, such as systemic condition, age, root anatomy and pulp status, may have influenced the results of this study, we were able to control for some of these factors by using the same method of canal preparation, tooth type and a sample population evenly distributed with regard to a number of factors, including gender, pulp and periapical status, site of affected teeth (upper or lower jaw) and presence of pretreatment pain.
In conclusion, this clinical investigation showed that the periapical infiltration of dexamethasone and morphine can lead to a considerable decrease in postoperative endodontic pain in the first 24 h after operation. According to the results of this study, dexamethasone was more effective than morphine. Further clinical studies examining different techniques are recommended to elucidate the potential of these drugs in the context of endodontic treatment.
Acknowledgement
This study was not financially supported by any institution.
Conflict of interest
There was no potential conflict of interest for any of the authors in this research.
REFERENCES
- 1.Zuckerman O, Metzger Z, Sela G, et al. [“Flare-up” during endodontic treatment – etiology and management] Refuat Hapeh Vehashinayim. 2007;24:19–26. [PubMed] [Google Scholar]
- 2.O’Keefe EM. Pain in endodontic therapy: preliminary study. J Endod. 1976;2:315–319. doi: 10.1016/S0099-2399(76)80047-7. [DOI] [PubMed] [Google Scholar]
- 3.Seltzer S, Bender IB, Ehrenreich J. Incidence and duration of pain following endodontic therapy. Relationship to treatment with sulfonamides and to other factors. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1961;14:74–82. doi: 10.1016/0030-4220(61)90476-5. [DOI] [PubMed] [Google Scholar]
- 4.Seymour RA, Blair GS, Wyatt FAR. Postoperative dental pain and analgesics efficacy. Part I. Br J Oral Surg. 1983;21:290–297. doi: 10.1016/0007-117x(83)90017-3. [DOI] [PubMed] [Google Scholar]
- 5.Martin H, Cunningham WT. An evaluation of postoperative pain incidence following endosonic and conventional root canal therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1982;54:74–76. doi: 10.1016/0030-4220(82)90419-4. [DOI] [PubMed] [Google Scholar]
- 6.Matusow RJ. The flare-up phenomena in endodontics: a clinical perspective and review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1988;65:750–753. doi: 10.1016/0030-4220(88)90023-0. [DOI] [PubMed] [Google Scholar]
- 7.Goodman LS, Gilman A. 8th edn. Pergamon Press; New York, NY, USA: 1990. Pharmacological Basis of Therapeutics; pp. 574–596. 1436–1459. [Google Scholar]
- 8.Cohen S, Hargreaves KM. 9th edn. E Mosby; St Louis, MO, USA: 2006. Pathways of the Pulp. [Google Scholar]
- 9.Marshall JG, Walton RE. The effect of intramuscular injection of steroid on posttreatment endodontic pain. J Endod. 1984;10:584–588. doi: 10.1016/S0099-2399(84)80106-5. [DOI] [PubMed] [Google Scholar]
- 10.Liesinger A, Marshall FJ, Marshall JG. Effect of variable doses of dexamethasone on post treatment endodontic pain. J Endod. 1993;19:35–39. doi: 10.1016/S0099-2399(06)81039-3. [DOI] [PubMed] [Google Scholar]
- 11.Kusner G, Reader A, Beck FM, et al. A study comparing the effectiveness of ibuprofen (Motrin), Empirin with Codeine #3, and Synalgos-DS for relief of postendodontic pain. J Endod. 1984;10:210–214. doi: 10.1016/S0099-2399(84)80085-0. [DOI] [PubMed] [Google Scholar]
- 12.Mohammadi Z. Systemic and local applications of steroids in endodontics: an updated review. Int Dent J. 2009;59:297–304. [PubMed] [Google Scholar]
- 13.Javidannejad S. 4th edn. The University Sciences; Tehran, Iran: 2001. Drugs Information (Iran Generic Drugs) pp. 291–293. [Google Scholar]
- 14.Marshall JG. Consideration of steroid for endodontic pain. Endod Topics. 2002;3:41–51. [Google Scholar]
- 15.Mohammadi Z, Farhad A, Khalesi M. Pharmacological strategies to control post-operative endodontic pain. Dent Res J. 2007;4:61–68. [Google Scholar]
- 16.Wynn RL. Narcotic analgesics for dental pain: available products, strengths, and formulations. Gen Dent. 2001;49:126–128. 130, 132. [PubMed] [Google Scholar]
- 17.Dionne RA, Lepinski AM, Gordon SM, et al. Analgesic effects of peripherally administered opioids in clinical models of acute and chronic inflammation. Clin Pharmacol Ther. 2001;70:66–73. doi: 10.1067/mcp.2001.116443. [DOI] [PubMed] [Google Scholar]
- 18.Hargreaves KM, Joris JL. The peripheral analgesic effects of opioids. APS J. 1993;2:51–59. [Google Scholar]
- 19.Likar R, Sittl R, Gragger K, et al. Peripheral morphine analgesia in dental surgery. Pain. 1998;76:145–150. doi: 10.1016/s0304-3959(98)00036-0. [DOI] [PubMed] [Google Scholar]
- 20.Shantiaee Y, Soluti A. Comparison of infradental nerve response to inflamed pulp after local application of lidocaine and lidocaine plus morphine in cats. J Dent Sch. 2008;26:296–302. [Google Scholar]
- 21.Mehrvarzfar P, Shababi B, Sayyad R, et al. Effect of supraperiosteal injection of dexamethasone on postoperative pain. Aust Endod J. 2008;34:25–29. doi: 10.1111/j.1747-4477.2007.00076.x. [DOI] [PubMed] [Google Scholar]
- 22.Pochapski MT, Santos FA, de Andrade ED, et al. Effect of pretreatment dexamethasone on postendodontic pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108:790–795. doi: 10.1016/j.tripleo.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 23.Torabinejad M, Cymerman JJ, Frankson M, et al. Effectiveness of various medications on postoperative pain following complete instrumentation. J Endod. 1994;20:345–354. doi: 10.1016/S0099-2399(06)80098-1. [DOI] [PubMed] [Google Scholar]
- 24.Glassman G, Krasner P, Morse DR, et al. A prospective randomized double-blind trial on efficacy of dexamethasone for endodontic interappointment pain in teeth with asymptomatic inflamed pulps. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1989;61:96–100. doi: 10.1016/0030-4220(89)90310-1. [DOI] [PubMed] [Google Scholar]
- 25.Moskow A, Morse DR, Kransar P, et al. Intracanal use of a corticosteroid solution as an endodontic anodyne. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1984;58:600–604. doi: 10.1016/0030-4220(84)90086-0. [DOI] [PubMed] [Google Scholar]
- 26.Ouyang Y, Tang Z, Chen S. [Clinical study on preventing endodontic inter appointment pain with dexamethasone] Zonghua Kou Qiang Yi Xue Za Zhi. 2001;36:206–208. [PubMed] [Google Scholar]
- 27.Beirne OR, Hollander B. The effect of methylprednisolone on pain, trismus, and swelling after removal of third molars. Oral Surg Oral Med Oral Pathol. 1986;61:134–138. doi: 10.1016/0030-4220(86)90173-8. [DOI] [PubMed] [Google Scholar]
- 28.Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995;332:1685–1690. doi: 10.1056/NEJM199506223322506. [DOI] [PubMed] [Google Scholar]
- 29.Marshall JG, Liesinger AW. Factors associated with endodontic posttreatment pain. J Endod. 1993;19:573–575. doi: 10.1016/S0099-2399(06)81290-2. [DOI] [PubMed] [Google Scholar]
- 30.Campbell Wl, Kendrick RW. Postoperative dental pain – a comparative study of anti-inflammatory and analgesic agents. UIster Med J. 1991;60:39–43. [PMC free article] [PubMed] [Google Scholar]