Abstract
The COVID-19 worldwide pandemic has forced individuals into an unnatural way of life. Families with children experience unique stressors, such as school closures, disrupted childcare arrangements, requirement of parents to uptake additional responsibilities such as homeschooling, possible financial strain, and lack of breathing space between family members. The adjustments required of parents and children during a pandemic presumably impacts the psychosocial wellbeing of parents and children in different ways. To better under the psychosocial consequences of pandemics on parents, children, and youth, this scoping review used Arksey and O'Malley (2005) five-stage framework to examine the existing research literature on Severe Acute Respiratory Syndrome (SARS), Influenza Type A virus (H1N1), and COVID-19 to answer the following two research questions: (1) What are the psychosocial consequences of pandemics on parents of children and youth? (2) What are the psychosocial consequences of pandemics on children and youth? With the application of inclusion criteria, 29 articles were selected for analysis. Four major themes, including sub-themes emerged: 1) Each family members’ emotions influence one another; 2) Parents experience greater levels of psychosocial problems than adults without children; 3) During a pandemic, parents require informal (social) and formal (specialized professional) support and; 4) Psychosocial consequences of pandemics on children/youth are understudied, indicating the need for more research on children/youth under the age of 20 years. Clinical prevention and intervention suggestions to support the psychosocial wellbeing of parents, children and youth during a pandemic are discussed.
Keywords: Pandemics, COVID-19, Parents, Children and youth, Psychosocial consequences, Resilience
1. Introduction
The spread of COVID-19 was declared a global pandemic by the World Health Organization (WHO) on March 11, 2020. COVID-19 has impinged on individuals worldwide, forcing them into an unnatural way of life. People in countries affected by COVID-19 were immediately advised to practice social distancing measures to control the spread of the disease (Government of Canada, 2021). These measures initially included refraining from meeting with anyone outside of those one lives with, no longer being able to engage in stress-relieving activities such going to the gym, limited options for activities outside of one’s home, and closing of in-person attendance at schools and nonessential workplaces. In many parts of the world, wearing face coverings (masks, shields, other face covering) has been strongly encouraged and even legislated in public areas, enclosed areas, and public transit, with limits to the number of people who can gather together (WHO, 2021).
The outbreak of COVID-19 was preceded by two earlier pandemics – Severe Acute Respiratory Syndrome (SARS), and Influenza Type A virus (H1N1). This is the third pandemic in this millennium. Each of these three pandemics share similarities and differences. Both COVID-19 and SARS are coronaviruses. SARS is referred to as SARS-CoV, and the virus that causes COVID-19 is known as SARS-CoV-2; H1N1(Swine Flu) is an influenza virus and all three originate from and are passed by animals to humans (Tesini, 2020). As such, SARS, H1N1 and COVID-19 outbreaks share similar features that may impact the wellbeing of children and parents: they are all respiratory illnesses, highly communicable viruses that have high mortality rates; in all three cases, the pandemics have led to the implementation of public health policies and measures to reduce the spread of viruses; children and youth are all potential vectors of contamination, and are thus equally targeted by restriction and containment measures. In terms of differences, although all three emphasize social isolation and physical distancing, only COVID-19 conditions have so broadly required wearing face coverings in public spaces and anywhere where physical distancing is not possible, and in some areas such as in China, Canada, the United Kingdom, curfews have been implemented (WHO, 2021). SARS and H1N1 required masks in certain settings, for persons at higher risk living in crowded and congregate settings where the virus was reported (Centers for Disease Control and Prevention, 2005, Centers for Disease Control and Prevention., 2009. With COVID-19, world-wide travel restriction, bans and closing of borders has been necessitated to slow down the spread and stop transmission.
The number of cases and deaths vary between pandemics. According to WHO, a total of 8098 people worldwide became sick with SARS during the 2003 pandemic, of which 774 died. According to the CDC, they estimated that there were 151,700– 575,400 H1N1-related deaths worldwide. As of February 1, 2021, 291 countries have been affected by COVID-19 with 103,503,821 reported infections and 2,239,469 deaths from COVID-19 (Worldometer, 2021).
In relation to this current COVID-19 outbreak, the UN Educational, Scientific and Cultural Organization has estimated that 1.38 billion children were out of school and daycares, without access to group activities, sports or playgrounds (Cluver et al., 2020). Working parents whose children are normally in daycare and/or school for a major portion of the day were now required to provide homeschooling, while simultaneously working from home. In cases where parents are essential service workers and required to work on-site, this has created major upheavals in childcare arrangements. Some parents have had to stop working to take care of their children – adding to financial strains. Further, those parents working in essential services face different stressors with fears about placing themselves, and their family, at heightened risk of disease due to their continued and prolonged exposure to the public. Additionally, families living in overcrowded housing have faced higher rates of transmission and the stresses associated with ensuing health concerns (Ahmad et al., 2020).
The adjustments required for families with children during COVID-19 will presumably impact parents and children in different ways. It is possible that families who are not negatively financially affected by COVID-19, and typically have busy work schedules, may appreciate the extra time at home as a positive event that they would not have otherwise had. However, this does not represent all families. Factors that have been associated with parental stress and burnout, such as parental unemployment, financial insecurity, a lack of leisure time away from children, and lack of social support (Sorkkila & Aunola, 2019), are far more likely during a pandemic when children are home, and everyone is expected to socially distance from their usual social supports. Parents who have children with special needs may experience heightened stress (Sorkkila & Aunola, 2019). Moreover, responsibilities that parents are required to take on as schools are closed add to parents’ stress. For example, research has found that homeschooling mothers experience anxiety and emotional burnout in their roles as both mother, homemaker, and teacher (Baker, 2019). For parents that are involuntarily put into homeschooling roles, these stressors are amplified as these parents are not accustomed, or trained, to provide this type of educational support to their children.
Moreover, “emotion contagion” – when one person’s emotions trigger similar emotions of another person (Neumann & Strack, 2000) – that has been documented amongst parents and children (Barry and Kochanska, 2010, Chi et al., 2019) as well as between siblings (Serra Poirier et al., 2017) outside of pandemic conditions, suggest that the wellbeing of both parents and children warrants special consideration during pandemics. Persistent confinement of family members may create greater potential for both positive and negative emotion contagion. Further, parents who suffer from heightened stress may be less emotionally available toward their children (Roskam et al., 2017).
Heightened familial tensions due to social distancing and isolation orders are evidenced by the rising rates of child abuse and other forms of family violence, including a rise in domestic violence since the COVID-19 pandemic began (Usher et al., 2020). For example, in Canada an increase of 20–30% in rates of gender-based violence and domestic violence have been noted by the Ministry for Women and Gender Equality (Patel, 2020). For children and youth who are exposed to unhealthy or abusive environments in their family home, isolation from peers may exacerbate their psychological distress. In the past, examination of factors that moderate the impact between exposure to domestic violence and adverse adolescent outcomes revealed that peer support moderated the relationship between domestic violence exposure and depression, running away from home, and high school dropout (Tajima et al., 2011).
For children who more heavily rely on peer and social group supports, such as LGBTQ youth, pandemic restrictions that limit social interactions and in-person school attendance may compromise the psychological wellbeing of such youth (Hatchel et al., 2019, Ybarra et al., 2015). Social isolation measures of COVID-19 have required many supports to become virtual, and so a better understanding of the mental health consequences of COVID-19 based restrictions on youth is needed. Considering that isolation from peers and close confinement with family members is more likely for youth during the social distancing measures of COVID-19, particular attention to the welfare of families is undoubtedly necessary during a pandemic, especially in light of the negative impacts that parental neglect and peer isolation can have on youth (Christ et al., 2017) and increased incidence of maltreatment during COVID-19 (Usher et al., 2020).
Given that COVID-19 is the third global pandemic of the 21st century, it seems appropriate to echo what was suggested by critics following the last two pandemics: that future pandemics are likely and that there is a continued need to plan for future pandemics ahead of time rather than as they occur (Miller et al., 2009, Morse et al., 2012). COVID-19 is preceded by SARS in 2002 to 2004 and H1N1/Swine flu in 2009–2010. Scientists warned that “the likelihood of another influenza pandemic during the next 50 years is virtually 100%” (Smil, 2008, p.46), and that it would kill millions of people (Webster, 2018). As predicted, such a pandemic (COVID-19) has occurred – and much earlier than 50 years since Smil’s book was published in 2008. Researchers cautioned following SARS and H1N1 that there were gaps in pandemic planning, including that the need for psychosocial supports for children and families is inadequately addressed (Nicholas et al., 2010). In one study it was suggested that “further explication of the biopsychosocial response of those exposed to pandemic disasters is the first step toward developing best practice approaches to planning, response, and recovery for children and families” (Sprang & Silman, 2013, p. 106). In spite of these recommendations, psychosocial studies on SARS and H1N1 trailed off as soon as the crises passed so that there are no longitudinal studies on parents and children, which is of concern. We could have learned from each of these pandemics to discern long-term effects. These have been missed opportunities that should now be investigated and paid attention to in order to gauge the psychosocial consequences of COVID-19 on parents and children. If acted on now, this affords us the opportunity to identify the psychosocial consequences of COVID-19 on parents and children, to make recommendations for timely responses.
In light of the above, the purpose of this paper was to conduct a scoping review on research studies that examined the psychosocial consequences of the current COVID-19 pandemic and two previous worldwide pandemics, H1N1/Swine flu and SARS, for parents and children. Although definitions slightly vary, psychosocial characteristics refer to “the influences of social factors on an individual’s mental health and behavior” (Vizzotto et al., 2013). Psychosocial consequences can refer to how a person is affected by a situation psychologically or socially (Suzuki & Takei, 2013). These factors and consequences encompass several domains such as psychological symptoms (i.e., anxiety, depression, distress, etc.), cognitive behavioral responses (i.e., satisfaction, self-efficacy, locus of control, etc.), and social factors (i.e., family, relationships with others, changes in personal roles, employment, etc.; Suzuki & Takei, 2013).
As such, Bronfenbrenner, 1977, Bronfenbrenner, 1979 socio-ecological model was used as the undergirding theory for this review in which individual experiences are understood within several interacting and nested experiences. Bronfenbrenner, 1977, Bronfenbrenner, 1979 posited that individual development is influenced by the relationships between the multiple domains of the microsystem (intra-personal factors of the individual); the mesosystem (interpersonal and relational connections); the exosystem (which includes indirect influences that shape individuals’ experiences); and the macrosystem (which includes societal and political influences and oppression). This person-in-environment perspective takes into account all the influences of a pandemic on the individual, their relationships and supports, and the existing environmental impacts as felt through pandemic threats and restrictions resulting in psychosocial consequences.
In summary, in using these definitions, this review focuses on the psychological and social functioning of parents and children as well as factors that deteriorate, maintain, or enhance psychological and social functioning for these individuals. A scoping review was selected as these are not intervention studies that would normally be covered through a systematic review. The objectives of this review were to identify studies on the psychosocial consequences of pandemics on parents and children, and from this to identify what parents can do to maintain their own good mental health, appropriate parenting practices and ways to promote well-being, and therefore resilience, in children in the face of a pandemic.
2. Methodology
A comprehensive scoping review was conducted using Arksey and O'Malley (2005) five-stage framework to better understand the psychosocial consequences of pandemics. The five stages of the review included: (1) identifying the research question; (2) identifying relevant studies; (3) selection of studies; (4) charting the data; and (5) collating, summarizing, and reporting results. The process for each step of this framework will be presented in the methodology of this review. Ethics approval was not required for this scoping review as it is based on the review of published and publicly available literature.
2.1. Identifying the research question
This scoping review examined peer-reviewed research literature surrounding the psychosocial consequences of pandemics on the mental health of parents, children and youth. Global pandemics occurring in the recent millennium – year 2000 and on – were covered. The following research questions were examined:
-
1.
What are the psychosocial consequences of pandemics on parents of children and youth?
-
2.
What are the psychosocial consequences of pandemics on children and youth?
The overall aim of the review outcomes will be to conclude by identifying and relaying recommendations for adult mental health promotion and for parenting to encourage child well-being and resilience in a pandemic.
2.2. Identifying relevant studies
A search of the literature was conducted using specific search terms to retrieve literature on the specified global pandemics in this century (2000–2020). Two electronic databases were selected: Scopus and PsycINFO. These two comprehensive searches produced many duplications of the same studies so that we were assured these were the most relevant databases from which to extract the studies. Peer-reviewed articles that contained one of the following terms in their abstract were included in the search: “SARS,” “H1N1,” “Swine flu,” “coronavirus,” or “COVID-19.” The literature search of Scopus occurred from June 9th to 16th, 2020. The literature search of PsycINFO occurred between July 13th to 15th, 2020, and on August 20, 2020 to capture any additional articles considering the wealth of academic knowledge quickly acquired in the context of the rapidly evolving COVID-19 situation. Consultation with a university librarian specialist provided guidance in databases searched and the credibility of the journals searched in retrieving studies for this scoping review.
2.3. Study selection
Arksey and O'Malley (2005) recommend developing inclusion and exclusion criteria that will produce studies that address the central research questions. The inclusion criteria used in this scoping review was related to the type of study (quantitative, qualitative and mixed methods), the focus of studies, and date of publication (see Table 1 ). Articles published after 2002 and onwards were selected as the first of disease associated with the included pandemics, SARS, first appeared in China in 2002.
Table 1.
Inclusion and exclusion criteria.
| Inclusion Criteria |
|
| Exclusion Criteria |
|
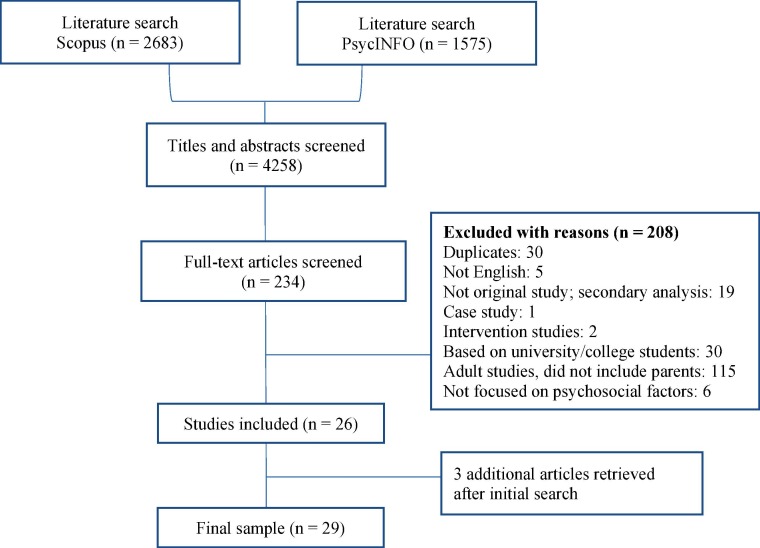
Two authors reviewed and applied the inclusion and exclusion criteria to the articles retrieved in a two-step process. The first author screened the initial 4258 articles that resulted from the initial searches of Scopus and PsycINFO based on their titles and abstracts to assess eligibility for inclusion in this scoping review. This resulted in a list of 234 articles included for further review based on their titles and abstracts. Articles that appeared to be based on adults according to the title and abstract were also selected for further review to assess whether the articles reported on findings for parents. This list of 234 articles was vetted by the second author who then reviewed the titles and abstracts of these articles to determine suitability for inclusion, or further exclusion. The 234 articles underwent a second screening process based on their full-text by both reviewers and a consensus was reached to include 29 articles in the scoping review analysis (Fig. 1 ).
Fig. 1.
Article selection process.
2.4. Charting the data
The fourth stage of the framework was to chart the key information obtained from the studies included in the review. This stage requires authors to decide what information from the studies should be recorded based on what will be most helpful to readers. It was decided for this scoping review to formulate three separate tables, one for each pandemic. Each table comprised of authors, year of publication, study location, study population, aims of the study, brief overview of methodology, and important results (see Tables 2, 3, and 4 in Supplementary Material). From these tables, the authors were able to identify themes and gaps in the literature.
2.5. Collating, summarizing, and reporting the results
The fifth stage of the Arksey and O'Malley (2005) framework involved summarizing and reporting the findings. Charting data allowed the authors of this scoping review to provide a narrative account of findings based on key areas and patterns as well as significant gaps that stand out. The three authors of this scoping review each reviewed the charted data and met together to discuss key findings, patterns, and identified gaps within the data.
Based on this discussion, the first author then initiated a thematic analysis (Braun & Clarke, 2006) of the study findings. Braun and Clarke’s (2006) thematic analysis provided a systematic framework for identifying themes which involved multiple readings of the selected studies by each author, who extracted themes that were then compared and further refined through discussions. A summary of findings was then discussed in virtual meetings with all authors until a consensus was reached.
Preliminary themes that emerged were along individual characteristics and psychosocial impacts, such as age and gender, while other themes reflected relevant processes as these relate to pandemics and psycho-social consequences. A higher-level abstraction identified features related to the different pandemic studies, which revealed gaps and recommendations for future research. Clinical recommendations were also derived from the study results.
3. Results
A summary of the studies included in this scoping review is followed by descriptions of four themes, and sub-themes, that emerged from review of the studies. The focus of studies varied across the three pandemics, although similarities were apparent and allowed for identification of the resultant themes. COVID-19 studies have so far focused on a wider range of psychosocial outcomes compared to the other two pandemics. H1N1 studies largely centered on fears of the disease and the negative consequences of such fears on parents and children, while SARS studies were primarily concerned with parents and children in hospital settings.
3.1. Profile of studies
The final sample consisted of 29 empirical studies (Tables 2–4) that focused on the COVID-19 (n = 19), H1N1 (n = 4), and SARS (n = 6) pandemics. The majority of studies were quantitative studies (n = 19), followed by qualitative (n = 8) and mixed methods studies (n = 2). The studies included the following participants: Studies of parents (n = 13), studies of children (n = 6), pregnant women (n = 5), with one of these studies looking at both pregnant women and their husbands (Ahorsu et al., 2020), studies including both parent and child participants (n = 4) and one study (n = 1) examining both mothers and expectant (pregnant) mothers (Cameron et al., 2020). Studies of pregnant women were included because parenting starts in-utero given the proliferation of prenatal education, input from experts and universal issues of safety for the developing fetus. The locations of where the research was conducted were worldwide (Table 5 in Supplementary Material).
3.2. Themes
Four themes, with corresponding sub-themes, reflect the psychosocial consequences of pandemics on parents and children, according to what is available through empirical literature. These are described and discussed below.
3.2.1. Theme 1: Each family members’ emotions influence one another – Emotion contagion can have negative effects
Across the three pandemics, emotional contagion was identified, so that the emotions of family members affect other family members. In a study of the effects of COVID-19 fear among pregnant women and their husbands, both participants’ fear of COVID-19 was positively associated with their own and their partners’ depression, suicidal intention, preventive COVID-19 behaviors, and negatively associated with their mental quality of life (Ahorsu et al., 2020). Interestingly, husbands’ fear of COVID-19 had a substantially stronger impact on their wives’ psychological wellbeing compared to the effect of wives’ fear on their husbands (Ahorsu et al., 2020). One COVID-19 study presented marital quality as a protective factor from depression for both pregnant women and mothers (Cameron et al., 2020), while another study identified relationship strain as a risk factor for depression symptoms among pregnant women during COVID-19 (Lebel et al., 2020). Although these two latter studies do not describe emotional contagion per se, they nevertheless similarly illustrate how the emotional environment in the home can either positively or negatively impact the mood of pregnant women and mothers. Collectively, these studies illustrate the importance of intimate partners’ emotional support toward one another during the stressful time of a pandemic in order to regulate one another’s emotions.
Studies conducted on the H1N1 pandemic highlight the influence of family members on one another beyond parents. Remmerswaal & Muris (2011) found that children’s fears of H1N1 and parents’ fears of H1N1 were significantly related to one another, with the way parents relay information about the disease to their children as having a significant influence on their children’s fears. This association remained significant while controlling for other sources of information, such as friends or school, which highlights the important influence that parents have on their children’s emotions about a pandemic virus. Sprang and Silman (2013) found a significant relationship between PTSD symptoms in parents and children of the same family during the H1N1 pandemic period. More specifically, 85.7% of children whose parents met PTSD cutoff levels also met clinical cutoff scores, compared to 14.3% of children whose parents did not meet PTSD criteria. Parents in this study reported that one distinct challenge they experienced was managing their own and their children’s anxiety surrounding the pandemic. Both these studies highlight the influence of parents’ emotions and fears on their children’s emotions and fears.
The SARS studies in this review that included children were those children who were hospitalized during the SARS pandemic (Koller et al., 2006a, Koller et al., 2006b, Koller et al., 2010). Within these studies, it was explained that during the hospitalization of these children, physical contact with parents was none to minimal, and so healthcare workers acted as primary caregivers to hospitalized children during this time. Accordingly, children described the importance of communication between themselves and healthcare providers, reporting that most communication they received from providers made them feel anxiety, fear and confusion (Koller et al., 2010). On the other hand, healthcare workers caring for these children discussed their challenges with dealing with the separation anxiety that children were feeling (Koller et al., 2006a, Koller et al., 2006b). Even within temporary caregiver-child situations made necessary by the isolation measures of a pandemic, the importance of emotion regulation and support between children and their temporary caregivers (i.e., healthcare providers) remained a vital consideration.
3.2.2. Theme 2: Parents experience greater levels of psychosocial problems than adults without children
A second observation evident among studies in all three pandemics was that fears and worries related to the pandemics were more prevalent among parents compared to adults without children. With one exception (Tull et al., 2020), parents, and mothers particularly, had higher levels of COVID-19 concerns than adults without children (Fitzpatrick et al., 2020, Korajlija and Jokic-Begic, 2020), with specific fears of young children contracting COVID-19 (Wang et al., 2020a). Fears related to COVID-19 were positively associated with depression and anxiety (Ahorsu et al., 2020, Fitzpatrick et al., 2020, Wang et al., 2020), suicidal intention (Ahorsu et al., 2020), and maintaining COVID-19 safety behaviours (Ahorsu et al., 2020, Korajlija and Jokic-Begic, 2020). Experiences of mothers across countries indicated that mothers in general showed more concerns and stressors due to additional burdens on their gendered roles as well as more fears of COVID-19 transmission (Fitzpatrick et al., 2020, Korajlija and Jokic-Begic, 2020, Safdar and Yasmin, 2020). For example, in a study of mothers in Pakistan who were professionals, and forced to lock down, qualitative data described their struggles to meet the traditional wife and mother roles (Safdar & Yasmin, 2020).
The reviewed SARS studies assessed pandemic-related fears and worries for parents in unique situations. Koh et al. (2005) examined the experiences of 10, 511 healthcare workers during the SARS pandemic. They found that the majority (82%) were worried about spreading the disease to family, friends, or colleagues. Healthcare workers with children experienced increased stress at work and reported the highest rates of feeling like their family members were socially ostracized because of their job, more than healthcare workers who were single or those who were married without children. Further, in studies that examined how parents felt during the hospitalization of their child, hospitalized due to SARS, these parents reported feelings of worry, a lack of control, and frustration and distress for not being permitted to be with their child (Koller et al., 2006a, Koller et al., 2006b). Findings of the SARS studies contribute to this theme in that parents directly involved with the pandemic (i.e., healthcare workers, parents whose child is hospitalized), as well as those less directly impacted, all experience pandemic-related worries. In relation to H1N1, Mesch et al. (2013) found that between the first wave of H1N1 and the second wave, during which time the media coverage on the pandemic increased, parents of children across age groups (children 0–6; 6–11; 11–17 years) experienced a moderately significant increase in worrisome feelings.
3.2.2.1. Sub-theme: Pregnancy and pandemics
Fear of COVID-19 was reported among pregnant women and their partners (Ahorsu et al., 2020), as well as fear of H1N1 among pregnant women (Lohm et al., 2014). Specifically, with H1N1, news media exposure increased worries for both pregnant women and parents in general (Lohm et al., 2014, Mesch et al., 2013). Additionally, an H1N1 study cited expectant parents’ needs for support through qualitative feedback from pregnant women contemplating vaccination during the pandemic – in particular the support of physicians’ advice in making health decisions (Lohm et al., 2014). One study on women who were pregnant during the COVID-19 pandemic (Berthelot et al., 2020), along with research during the SARS pandemic (Lee et al., 2006), demonstrated that they had higher levels of psychological distress, such as anxiety, and these were compared to women pregnant prior to these pandemics. During the SARS pandemic, there was a significant negative correlation between social support and depression scores with pregnant women, implying a lower likelihood of depression among pregnant women who had more social support (Lee et al., 2006). Important to note, across all three pandemics, social distancing appeared to be a coping strategy to manage pandemic-related fears and worries among pregnant women and parents (Korajlija and Jokic-Begic, 2020, Lohm et al., 2014, Lee et al., 2006).
3.2.3. Theme 3: During a pandemic, parents require informal and formal (specialized professional) support
Studies of parents that examined support needs show that both strong social and professional supports during a pandemic are required. Several COVID-19 studies reported on parents’ need for social and professional support to alleviate their psychosocial stress, as described below. This need is greater for parents with children with special needs.
3.2.3.1. Sub-theme: Parents of children with special needs
Three COVID-19 studies of parents with children diagnosed with autism spectrum disorders (ASD) were located (Cahapay, 2020, Colizzi et al., 2020, Esentürk, 2020), whereby parents reported more challenges than experienced prior to COVID-19. These included disruption to structured activities, routines, and schooling for their children. Parents also cited that, as a result of these disruptions, coupled with spending more time indoors, their children experienced anxiety and distress, and an increase in behavioural problems (Cahapay, 2020, Colizzi et al., 2020, Esentürk, 2020). Furthermore, children with ASD who were not receiving indirect school support were more likely to exhibit more serious behavior problems (Colizzi et al., 2020). To cope, some families found that support from other family members with homeschooling and mutual support between other families that have children with ASD was helpful (Cahapay, 2020). The most commonly cited needs for parents during COVID-19 was in-home healthcare support (Colizzi et al., 2020), experts’ support and family education (Esentürk, 2020). Clearly, familial, social, and professional support is necessary for parents of children with special needs during COVID-19.
3.2.3.2. Sub-theme: Parents of children without special needs
For parents of children without special needs, similar supports are also identified to help with the crisis of the pandemic. Lades et al. (2020) found that although spending more time with children was associated with positive affect among parents in their study, homeschooling was associated with notably higher negative affect among parents. Additionally, parents with lower perceived social support were more likely to experience anxiety and depressive symptoms (Lebel et al., 2020). With the additional responsibilities and time constraints presented by isolation measures, parents may not be able to receive the professional support that they need. Among mothers who presented with clinically relevant depression or anxiety, only 21.48% had accessed individual counselling in the past month (Cameron et al., 2020). Noted barriers to accessing mental health services were lack of time or energy, and the cost of services (Cameron et al., 2020). Considering that financial strain and employment loss were also associated with psychological distress among mothers (Berthelot et al., 2020, Cameron et al., 2020, Lebel et al., 2020), accessibility of mental health services is an important consideration during pandemics when financial hardship is more prevalent in families. The “stacking” of stressors, or cumulative effects of stress, should be further recognized as increasing vulnerabilities for mental health problems.
With the H1N1 studies, parents noted the importance of acquiring mental health services for their children. In one study comparing isolating/quarantined families with families that were not isolating/quarantined, the researchers found higher utilization of mental health services amongst families with containment experiences, with 33.4% of parents reporting that their child/children began using mental health services related to their pandemic experience (Sprang & Silman, 2013).
The SARS studies explored the needs and coping strategies of parents whose children were hospitalized due to SARS. Parents regarded having regular communication with their child and healthcare providers as vitally important during this time (Koller et al., 2006b). Parents in one study did not want to speak with other family members about their child’s hospitalization so as to not induce worry, and they instead found it helpful when doctors kept them informed about their child’s condition (Chan et al., 2007). These parents expressed satisfaction with the quality of care their child received from health professionals during the hospitalization (Chan et al., 2007).
3.2.4. Theme 4: Psychosocial consequences of pandemics on children/youth is understudied, indicating the need for more research on children/youth under the age of 20 years
The focus of studies on children across the three pandemics varied. While some COVID-19 studies examined the psychosocial impacts of the pandemic on the wellbeing of children, H1N1 studies were primarily concerned with children's H1N1 fears and psychological symptoms of isolated children, and SARS studies that included children focused on child participants who were hospitalized during the SARS pandemic because they had contracted SARS.
COVID-19 studies on children have provided several insights. First, older youth may be more impacted on a psychosocial level compared to younger children. Liu et al. (2020) found that older students were more concerned about COVID-19 compared to primary school students in the 5th and 6th grades. Similarly, among adolescents between the ages of 12 to 18 years old, increasing school grade was associated with a higher prevalence of depressive and anxiety symptoms (Zhou et al., 2020). This study also found that female students had higher depressive and anxiety symptoms than male students (Zhou et al., 2020). Level of awareness of COVID-19 (Zhou et al., 2020) and concern about COVID-19 (Liu et al., 2020) impacted psychological health problems among these youth. Furthermore, fear of COVID-19 was associated with greater obsessive-compulsive disorder symptoms and depression-anxiety symptoms among adolescents (Secer & Ulas, 2020). At the same time, one study on individuals aged between 14 and 35 years old found no significant difference between the adolescents and adults on any mental health factors (Liang et al., 2020).
One area of concern that has been voiced throughout the COVID-19 pandemic is the importance of peers for children and youth, and how isolation may negatively impact their wellbeing. The findings on this matter are mixed based on two studies that examined the impact of isolation on adolescents. One study in the United States found no association between the degree of social distancing practiced by adolescents and their mental health (Oosterhoff et al., 2020), whereas one study conducted in China found that prolonged lockdown (identified as one month of lockdown in this study) had an adverse impact on the mental health of adolescents (Wang et al., 2020b). Interestingly, the study that found no association noted that the reasons for social distancing were related to mental health symptoms among adolescents (Oosterhoff et al., 2020). For example, adolescents that stayed home and practiced social distancing because they would have preferred to stay home anyway reported less anxiety and depression symptoms. On the other hand, youth practicing social distancing to avoid judgement reported greater anxiety symptoms, and youth social distancing because a friend told them reported greater depressive symptoms (Oosterhoff et al., 2020).
During H1N1, children were fearful of the disease (Remmerswaal and Muris, 2011, Sprang and Silman, 2013). These fears were influenced by their parents’ fears and how their parents transmitted information about the pandemic to them (Remmerswaal & Muris, 2011), and whether their parents were affected by the disease (Sprang & Silman, 2013) – an example of the impact of emotional contagion. In a study that compared children who experienced social distancing measures and those who did not, there was a significant difference for meeting the clinical cut-off score for PTSD among children who had been in isolation (30%) versus children who had not been in isolation and quarantine (1.1%; Sprang & Silman, 2013).
Among the three studies in this review that concentrated on children hospitalized during SARS (Koller et al., 2006a, Koller et al., 2006b, Koller et al., 2010), all reported that children experienced various distressing emotions, such as fear, confusion, anxiety, sadness, worry, and loneliness. Some children who were hospitalized due to SARS continued to show signs of distress after they were discharged from the hospital, such as becoming upset when a parent left home for work (Koller et al., 2006a). The Koller et al. (2010) study also included children and adolescents hospitalized during the SARS pandemic, but not due to SARS.
Overall, it is clear that throughout all three pandemics, children and youth are aware of and experience fears related to the pandemic; however, research on the psychosocial consequences of the pandemics on children not directly impacted by the viruses is minimal. Some patterns appear to be emerging in COVID-19 studies, however inconsistent at times, and so further research is needed to solidify the impacts of pandemic circumstances on the psychosocial wellbeing of children and youth.
4. Discussion
This scoping review, using Arksey and O'Malley (2005) five step framework, examined 29 peer-refereed studies on the psychosocial impacts of COVID-19, H1N1/Swine flu, and SARS pandemics on parents, including pregnant mothers, and children. Four clear themes emerged from the review: 1) Each family members’ emotions influence one another - emotion contagion can have negative effects; 2) Parents experience greater levels of psychosocial problems than adults without children; 3) During a pandemic, parents require informal (social) and formal (specialized professional) support and; 4) Psychosocial consequences of pandemics on children/youth is understudied, indicating the need for more research on children/youth under the age of 20 years. These will be discussed in detail, but first observational comments are offered about the literature as a whole.
In terms of the available literature, there were significantly more COVID-19 studies than other pandemic related studies, and these continue to proliferate. Speculating on this, the authors surmised that COVID-19 has spread more rapidly to the Western world and has thus received more attention. As well, the rapid transmission rates of COVID-19 and significantly higher death rates are of greater concern than past pandemics since the year 2000. For example, a comparison of prevalence of the pandemic diseases in the United States illustrates this: SARS was detected in only 8 people (WHO); there were 60.8 million cases of H1N1 and 12, 469 deaths (CDC); and as of September 24, 2020 (at the conclusion of study data collection), there were a reported 32,298,738 COVID-19 cases and 984,974 deaths (Worldometer, 2021).
Research on both the short-term and long-term impacts of both the SARS and H1N1 pandemics on children and parents would have provided greater insight on the types of mental health and social supports that would be most beneficial to parents during the current COVID-19 pandemic. However, due to discontinued focus on the psychosocial impact of pandemics once the crises passed, there are no longitudinal studies on the psychosocial consequences of the SARS or H1N1 pandemic on parents and children. Longitudinal studies from each of these pandemics would have been helpful in preparing for the effects of COVID-19 on the wellbeing of children and adults. Research on the psychosocial consequences of COVID-19 should consider longitudinal designs in order to better inform prevention and intervention programs in the event of a future pandemic. Longitudinal studies could also identify protective factors that help alleviate both short-term and long-term negative consequences of pandemic conditions (e.g., what types of supports help people navigate in-the-moment struggles during a pandemic and which supports help buffer potential long-term effects of pandemics such as social anxiety).
There are some trends that are not strong enough to be labeled as themes but should be noted, nonetheless. In terms of age, some studies showed that older youth (adolescents) showed increased levels of anxiety and depression (Liu et al., 2020, Zhou et al., 2020). In terms of gender, some studies revealed that adult women and female adolescents show greater rates of pandemic-related worry, anxiety, depression (Korajlija and Jokic-Begic, 2020, Mesch et al., 2013, Zhou et al., 2020). Beyond the studies included in this review, other studies that looked at the psychosocial impacts of pandemics on adults in general found that female gender was associated with greater COVID-19 fear (Broche-Pérez et al., 2020, Yildirim et al., 2020), high death anxiety related to H1N1 (Elizarrarás-Rivas et al., 2010), and higher likelihood of PTSD among SARS survivors (Mak et al., 2010). In a study that looked at self-reported anxiety and depression in the weeks following the COVID-19 pandemic among young adults, nonbinary participants reported the highest levels of depression and anxiety, followed by female participants, and then male participants (Alonzi et al., 2020). These authors pointed to the importance of identifying young adult subgroups who are already at an increased risk for mental health difficulties in order to provide supportive services to them as soon as possible to prevent mental health decline during a pandemic (Alonzi et al., 2020).
One of the most significant findings in this review shows that family members’ emotions influence one another during a pandemic. Parents’ fears of pandemics and PTSD symptoms were associated with their children’s fears and PTSD symptoms, and children reported that communication from caregivers during a pandemic could elicit anxiety, fear, and confusion (Koller et al., 2010, Remmerswaal and Muris, 2011, Sprang and Silman, 2013). During COVID-19, social distancing measures have required that individuals isolate with those whom they usually live with. Therefore, parents and their young children are isolating in their homes together. With an increase in social closeness among family members during a pandemic, the importance of emotional regulation among family members is imperative as each family member’s emotional state can influence that of another family member. Two studies with adults that did not meet the inclusion criteria for this review also found that family members' level of worry about a pandemic predicted adults' own levels of worry about a pandemic (Goodwin et al., 2011, Prati et al., 2011). Parents should practice affect regulation and process their fears surrounding pandemics in order to lessen the risk of transmitting negative affect and fears to their children. A related factor found through this review as important for parents’ mental health is relationship/marital quality (Cameron et al., 2020, Lebel et al., 2020). Therefore, in two-parent households, parents should support one another and discuss and process their feelings with their partners in order to support their own mental health, and in turn their children’s mental health.
Secondly, compared to adults without children, parents experience heightened levels of pandemic fear, which is associated with various psychosocial problems. Increased stress among parents could be expected as COVID-19 places additional responsibilities on people. Moreover, for parents who lost their jobs due to the closure of non-essential services, they are presumably at a heightened risk for becoming overwhelmed, given the findings in this review that highlighted that financial strain was associated with psychological distress among parents (Berthelot et al., 2020, Cameron et al., 2020, Lebel et al., 2020). Financial stress is a reality for many families during COVID-19 such as in Canada where 3 million jobs were lost by May 2020, with single parents’ unemployment rising by 53.9% (Statistics Canada, 2020). Parents with compromised income face difficulties in meeting the educational needs of their children through home-schooling, as this usually requires updated technologies. Working parents who have to manage work and home life to a greater extent with the added responsibilities of homeschooling and constant childcare also experience considerable stress for different reasons but with the same implications for mental health.
Parents who are essential service workers and thus required to work with the public during a pandemic experience their own unique stress. Koh et al. (2005) reported increased stress among parents who were healthcare workers during the SARS pandemic, and other research has found that emotional exhaustion of employees can contribute to strained family issues (Liang, 2015). As such, psychosocial supports for parents working in essential service workplaces is important to consider so that their own mental health is protected, therefore reducing the chance of bringing home job-related stress.
A non-scientific poll conducted in the United States by the American Psychological Association (APA) during the COVID-19 pandemic supports the finding from this review that parents experience increased stress during pandemics. The poll found that parents of children under 18, on average, feel significantly more stressed than adults without children (APA, 2020). In this report, parents described several sources of stress: family members getting coronavirus; government response to coronavirus; disrupted routines; getting coronavirus themselves; meeting basic needs; self-isolation; access to healthcare services; and missing out on major milestones such as the graduation of a child (APA, 2020). There is a clear need for additional supports for parents in order to alleviate their own stress, which in turn may limit negative emotion contagion in families.
In line with this, our review found that research from all three pandemics suggests that parents require social, familial, and professional support during a pandemic to reduce parental stress, anxiety, and depression. Needs are greater for families experiencing financial strain and those with children with special needs. The current review included three studies on parents of children with ASD during COVID-19 (Cahapay, 2020, Colizzi et al., 2020, Esentürk, 2020). Research conducted prior to COVID-19 indicated that parents of children with ASD, compared to parents with typically developing children, report significantly greater psychological distress, parenting stress, and attachment-related anxiety (Keenan et al., 2016). With regular supports and routines being disrupted during a pandemic, it is not surprising that this situation would be an even more difficult time than usual for parents (Cahapay, 2020, Colizzi et al., 2020, Esentürk, 2020). Even more worrisome is an examination of support needs that mothers and fathers of children with ASD reported as important yet unmet needs prior to the pandemic (Hartley & Schultz, 2015), all of which are conceivably less likely to be met during lockdown measures. For example, some of the top unmet important support needs were to have time to spend alone with my partner; for my child to have social activities other than with his/her own parents and siblings; my child to have friends of his/her own; take family vacations each year (Hartley & Schultz, 2015). Parents of children with special needs require particular attention during a pandemic when their social and professional supports may be compromised, and their support needs may thus be further unmet. Future research on the experience of parents with children with other health or mental health conditions that require regular support is also warranted.
Finally, there is very little research on psychosocial consequences of pandemics on children and youth, indicating a strong need for studies with participants under the age of 20 years. It is evident that children and youth are aware of pandemics as they are occurring and experience fears related to pandemics; however, research on the psychosocial impacts of the pandemics on children are mixed and difficult to draw confident conclusions from. The voices of children themselves could prove especially useful in terms of providing them with appropriate supports. For instance, children hospitalized during the SARS pandemic provided the following suggestions for ways to decrease the stress of children who are hospitalized during a pandemic: prioritizing the presence of family and friends; age-appropriate communication so as to not increase anxiety or confusion; the use of many toys and activities as distractions; and limiting exposure to pandemic-related news (Koller et al., 2006a, Koller et al., 2006b, 2010). More research that captures the experiences of children and youth during a pandemic will provide useful insight when considering what supports would be most helpful to children and youth during pandemics.
As children return to school during the COVID-19 pandemic, it is important to consider the possible psychosocial impacts on children and youth of these unusual school routines and regulations. Routines for children are likely to be impacted well beyond the duration of the pandemic, which in itself is uncertain at the moment. With children returning to school, their experience is expected to be different than prior to the pandemic. A study that explored the influence of SARS on children’s routines and behaviour when preschools in China re-opened after a 6-week closure found several changes to preschool routines and social interactions among children (Rao, 2006). Among 20 preschools included in this study, changes in routines included heightened hygiene requirements, shorter school days, temperature measurement of children when they arrived, and cancellation of previously regular activities such as snack time, physical education, and music lessons. Social interactions among children were altered and reduced as children were not allowed to share toys, they were required to wear a mask when speaking with peers, children had to face the wall to eat if snack time was not cancelled, and there were fewer opportunities to interact in large groups as group size decreased in all schools.
Finally, minority youth, such as sexual minority youth, racialized youth, and youth living in poverty, are an under-studied area in regard to pandemic impacts. In a secondary analysis of 31 text-based chat transcripts from a chat-based support group for LGBTQ youth occurring during COVID-19, youth expressed LGBTQ-specific challenges such as being isolated at home with unsupportive parents, losing “safe spaces” that they had outside of the home, less access to peers to whom they had disclosed their LGBTQ identity, lost access to in-person LGBTQ youth organizations, and hesitation to engage in virtual therapy within the home where their parents were in close proximity (Fish et al., 2020). With reduced access to in-person support for sexual minority youth, and likewise other minority youth, the psychological wellbeing of these young people may be compromised. Research with youth with diverse identities would help inform programs for these youth during the current COVID-19 pandemic and for future pandemics, so that all youth receive supports that best meet their unique needs.
5. Clinical implications
The first point of prevention and intervention for negative psychosocial consequences during a pandemic, especially now with COVID-19, is with the parents. If the parents are not doing well in terms of psychosocial well-being, their children may not do well. Child and youth specific considerations should also be followed to mitigate pandemic-related negative psychosocial consequences. Several recommendations and key messages based on the findings of this review are as follows:
-
•
Parents and professionals should be made aware of the issue of emotional contagion and what this means in parenting children and youth
-
•
Parents need to be supported through their own stress management and self-care so as to reduce negative emotional contagion
-
•
Connecting with social supports should be encouraged for families (parents and children) even with physical distancing to reduce social isolation, through approaches that can be done in safe and creative ways
-
•
Towards prevention, health care providers and mental health professionals need to provide support and expert advice to parents by actively reaching out to parents and not waiting until problems are identified – using a universal approach
-
•
Public awareness campaigns on mental health for adults and children should be implemented with corresponding access to mental health services
-
•
Parents need to be given specific strategies to help their children in managing their emotions and behavior through concrete suggestions, such as referring them to easy to access resources (i.e., CDC COVID-19 Parental Resource Kit; UNICEF guide for parents)
-
•
Physicians working with pregnant women need to be aware of their unique stressors and offer resources for support and information on COVID-19 related to pregnancy, and pre- and post-natal care
-
•
Other significant adults in caregiving roles (i.e., childcare providers; foster care parents; extended family members) need to be given mental health information and access to supports and resources
-
•
Schools are an important source of identification of mental health issues and need to connect students of all ages to mental health supports as school personnel and social workers will observe issues early on in educational settings
-
•
Schools need to be financially supported by governments to provide increased support to students during and post pandemic as psychosocial needs will be increased
6. Limitations
Although the search process for this review was thorough, some limitations exist. As the search process was largely concluded in August 2020, and COVID-19 studies appear to be published at a continuous rate, some eligible studies may have been missed and thus not included in the review. Methodological limitations of the overall available literature also exist. Longitudinal studies for previous pandemics are lacking. The studies are cross-sectional, so the results only reflect a snapshot of one point in time. Studies that compared concerns or other psychosocial factors using two different samples at two different times are limited in their ability to analyze behaviours over time. It is also not clear in many of these studies whether study participants may have had pre-existing anxiety, depression or PTSD for other reasons prior to the onset of the pandemics. Likewise, for studies that reported on PTSD, it is unknown whether participants had previous PTSD that might have gotten re-activated by COVID-19 or another pandemic.
Not all studies on children and youth were comparable in terms of the age of the samples. Some studies included ages 12–21.4 years (Wang et al., 2020, Wang et al., 2020) while others had cut-offs of 18 or 20. Moreover, based on the description provided on the 12–21.4 years age group in the noted studies (Wang et al., 2020, Wang et al., 2020), it is unclear whether these samples were mainly college/university students. University students are generally considered a specific and perhaps more resilient group, so that findings extracted primarily from university students would not be considered transferable to youth in general.
Moreover, as mentioned, considerably more research has been produced related to the psychosocial consequences of pandemics during COVID-19 as it has more seriously impacted Western countries. Future research should aim to consider the experiences of individuals worldwide, including countries in the Global South where individuals may face unique stressors during a pandemic.
7. Conclusion
The opportunity to plan for today and the future, through identifying and mitigating the negative psychosocial consequences of pandemics for parents and children, exists right now. This scoping review has highlighted important findings of the consequences of global pandemics on parents, children and youth. Research on the long-term psychosocial consequences of pandemics is lacking as studies from past pandemics, such as H1N1 and SARS, did not employ longitudinal designs. Attention to pandemics seem to discontinue shortly after they end, without consideration for the importance of building knowledge for future pandemics – and experts strenuously predict that more pandemics are on their way. These missed opportunities should not be repeated with the current pandemic and its aftermath.
Under pandemic public health safety measures and ensuing restrictions, family members live together in closer proximity, experiencing unique stressors, while being seriously constrained in their social connections outside of the family by being restricted from school, social activities for both parents and youth, sports, arts, and a host of other social contacts. This makes emotion contagion a pertinent issue for transmission of anxiety and worries, spurring the need for public health campaigns on how to promote and maintain good mental health, and the implications for parenting. Launching public awareness campaigns that not only stress the physical aspects of a coronavirus, its transmission and consequences, but also highlight the psychosocial consequences are called for. Increasing service availability and access to mental health services goes hand in hand with raising public awareness – this needs to include the elimination of waiting lists and increased funding for schools and social services to respond to pandemic-related issues.
Finally, research on the psychosocial impacts of COVID-19 on families, parents and children, with a significant focus for bringing the voices of children and youth into the research, especially minority youth, should continue even when COVID-19 has been brought under control. Longitudinal studies are key in determining both short-term and long-term impacts of pandemics on the mental health and wellbeing of families in order to inform public health policies and provide rationale for sufficient funding and service supports.
Funding
This work was supported by the Social Sciences and Humanities Research Council [Ref.: 767-2020-2810]; and the Margaret and Wallace McCain Family Chair in Child and Family.
CRediT authorship contribution statement
Rusan Lateef: Conceptualization, Formal analysis, Writing - original draft, Investigation, Writing - review & editing, Funding acquisition. Ramona Alaggia: Conceptualization, Formal analysis, Funding acquisition. Delphine Collin- Vézina: Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.childyouth.2021.106002.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Ahmad K., Erqou S., Shah N., Nazir U., Morrison A.R., Choudhary G., Wu W.C. Association of poor housing conditions with covid-19 incidence and mortality across US counties. Plos One. 2020;15(11):0241327. doi: 10.1371/journal.pone.0241327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorsu, D. K., Imani, V., Lin, C., Timpka, T., Brostrom, A., Updegraff, J.A., Arestedt, K., Griffiths, M.D., & Pakpour, A. H. (2020). Associations between fear of covid-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-partner interdependence modelling. International Journal of Mental Health and Addiction, (2020). 10.1007/s11469-020-00340-x. [DOI] [PMC free article] [PubMed]
- Alonzi S., La Torre A., Silverstein M.W. The psychological impact of preexisting mental and physical health conditions during the covid-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):238. doi: 10.1037/tra0000840. [DOI] [PubMed] [Google Scholar]
- American Psychological Association. (2020). Stress in the time of COVID-19. https://www.apa.org/news/press/releases/stress/2020/stress-in-america-covid.pdf.
- Arksey H., O'Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Baker E.E. Motherhood, homeschooling, and mental health. Sociology Compass. 2019;13(9) doi: 10.1111/soc4.12725. [DOI] [Google Scholar]
- Barry R.A., Kochanska G. A longitudinal investigation of the affective environment in families with young children: From infancy to early school age. Emotion. 2010;10(2):237–249. doi: 10.1037/a0018485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berthelot N., Lemieux R., Garon-Bissonnette J., Drouin-Maziade C., Martel É., Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstetricia Et Gynecologica Scandinavica. 2020;99(7):848–855. doi: 10.1111/aogs.13925. [DOI] [PubMed] [Google Scholar]
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 93. doi:10.1191/1478088706qp063oa.
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychologist. 1977;32:513–531. [Google Scholar]
- Bronfenbrenner U. Harvard University Press; Cambridge, Mass: 1979. The ecology of human development: Experiments by nature and design. [Google Scholar]
- Broche-Pérez Y., Fernández-Fleites Z., Jiménez-Puig E., Fernández-Castillo E., Rodríguez-Martin B.C. Gender and fear of covid-19 in a Cuban population sample. International Journal of Mental Health and Addiction. 2020;1–9:1–9. doi: 10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahapay M.B. How Filipino parents home educate their children with autism during covid-19 period. International Journal of Developmental Disabilities. 2020;1–4:1–4. doi: 10.1080/20473869.2020.1780554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron E.E., Joyce K.M., Delaquis C.P., Reynolds K., Protudjer J.L.P., Roos L.E. Maternal psychological distress & mental health service use during the covid-19 pandemic. Journal of Affective Disorders. 2020;276:765–774. doi: 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2005, May 3). Supplement D: Community Containment Measures, Including Non-Hospital Isolation and Quarantine. https://www.cdc.gov/sars/guidance/d-quarantine/index.html.
- Centers for Disease Control and Prevention (2009, September 24). Interim Recommendations for Facemask and Respirator Use to Reduce 2009 Influenza A (H1N1) Virus Transmission. https://www.cdc.gov/h1n1flu/masks.htm.
- Chan S.S.C., Leung D., Chui H., Tiwari A.F.Y., Wong E.M.Y., Wong D.C.N.…Lau Y. Parental response to child's isolation during the SARS outbreak. Ambulatory Pediatrics. 2007;7(5):401–404. doi: 10.1016/j.ambp.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi P., Du H., King R.B., Zhou N., Cao H., Lin X. Well-being contagion in the family: Transmission of happiness and distress between parents and children. Child Indicators Research : The Official Journal of the International Society for Child Indicators. 2019;12(6):2189–2202. doi: 10.1007/s12187-019-09636-4. [DOI] [Google Scholar]
- Christ S.L., Kwak Y.Y., Lu T. The joint impact of parental psychological neglect and peer isolation on adolescents’ depression. Child Abuse & Neglect. 2017;69:151–162. doi: 10.1016/j.chiabu.2017.04.015. [DOI] [PubMed] [Google Scholar]
- Cluver L., Lachman J.M., Sherr L., Wessels I., Krug E., Rakotomalala S.…McDonald K. Parenting in a time of COVID-19. The Lancet. 2020;395(10231):e64. doi: 10.1016/S0140-6736(20)30736-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of covid-19 in autism spectrum disorder: An online parent survey. Brain Sciences. 2020;10(6) doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elizarrarás-Rivas J., Vargas-Mendoza J.E., Mayoral-García M., Matadamas-Zarate C., Elizarrarás-Cruz A., Taylor M., Agho K. Psychological response of family members of patients hospitalised for influenza a/h1n1 in Oaxaca, Mexico. Bmc Psychiatry. 2010;10:104. doi: 10.1186/1471-244X-10-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esentürk O.K. Parents’ perceptions on physical activity for their children with autism spectrum disorders during the novel coronavirus outbreak. International Journal of Developmental Disabilities. 2020;1–12:1–12. doi: 10.1080/20473869.2020.1769333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish J.N., McInroy L.B., Paceley M.S., Williams N.D., Henderson S., Levine D.S., Edsall R.N. “I’m kinda stuck at home with unsupportive parents right now”: LGBTQ youths' experiences with covid-19 and the importance of online support. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine. 2020;67(3):450–452. doi: 10.1016/j.jadohealth.2020.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of covid-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice and Policy. 2020;12(S1):21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Goodwin R., Gaines S.O., Myers L., Neto F. Initial psychological responses to swine flu. International Journal of Behavioral Medicine: Official Journal of the International Society of Behavioral Medicine. 2011;18(2):88–92. doi: 10.1007/s12529-010-9083-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada (2021, January 18). Coronavirus disease (COVID-19): Prevention and risks. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks.html.
- Hartley S.L., Schultz H.M. Support needs of fathers and mothers of children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2015;45(6):1636–1648. doi: 10.1007/s10803-014-2318-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatchel T., Subrahmanyam K., Negriff S. Adolescent peer victimization and internalizing symptoms during emerging adulthood: The role of online and offline social support. Journal of Child and Family Studies. 2019;28(9):2456–2466. doi: 10.1007/s10826-018-1286-y. [DOI] [Google Scholar]
- Keenan B.M., Newman L.K., Gray K.M., Rinehart N.J. Parents of children with ASD experience more psychological distress, parenting stress, and attachment-related anxiety. Journal of Autism and Developmental Disorders. 2016;46(9):2979–2991. doi: 10.1007/s10803-016-2836-z. [DOI] [PubMed] [Google Scholar]
- Koh D., Lim M.K., Chia S.E., Ko S.M., Qian F., Ng V.…Fones C. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore what can we learn? Medical Care. 2005;43(7):676–682. doi: 10.1097/01.mlr.0000167181.36730.cc. [DOI] [PubMed] [Google Scholar]
- Koller D., Nicholas D., Gearing R., Kalfa O. Paediatric pandemic planning: Children's perspectives and recommendations. Health & Social Care in the Community. 2010;18(4):369–377. doi: 10.1111/j.1365-2524.2009.00907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koller D.F., Nicholas D.B., Goldie R.S., Gearing R., Selkirk E.K. Bowlby and Robertson revisited: The impact of isolation on hospitalized children during SARS. Journal of Developmental and Behavioral Pediatrics. 2006;27(2):134–140. doi: 10.1097/00004703-200604000-00010. [DOI] [PubMed] [Google Scholar]
- Koller D.F., Nicholas D.B., Goldie R.S., Gearing R., Selkirk E.K. When family-centered care is challenged by infectious disease: Pediatric health care delivery during the SARS outbreaks. Qualitative Health Research. 2006;16(1):47–60. doi: 10.1177/1049732305284010. [DOI] [PubMed] [Google Scholar]
- Korajlija, L.A., & Jokic‐Begic, N. (2020). Covid‐19: concerns and behaviours in Croatia. British Journal of Health Psychology, (20200516). 10.1111/bjhp.12425. [DOI] [PMC free article] [PubMed]
- Lades L.K., Laffan K., Daly M., Delaney L. Daily emotional well-being during the covid-19 pandemic. British Journal of Health Psychology. 2020;2020 doi: 10.1111/bjhp.12450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the covid-19 pandemic. Journal of Affective Disorders. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee D.T.S., Sahota D., Leung T.N., Yip A.S.K., Lee F.F.Y., Chung T.K.H. Psychological responses of pregnant women to an infectious outbreak: A case-control study of the 2003 SARS outbreak in Hong Kong. Journal of Psychosomatic Research. 2006;61(5):707–713. doi: 10.1016/j.jpsychores.2006.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang H. Are you tired? spillover and crossover effects of emotional exhaustion on the family domain. Asian Journal of Social Psychology. 2015;18(1):22–32. doi: 10.1111/ajsp.12075. [DOI] [Google Scholar]
- Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. The effect of covid-19 on youth mental health. The Psychiatric Quarterly. 2020;91(3):841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding covid-19 among Chinese college and primary school students: A cross-sectional survey. Psychiatry Research. 2020;289 doi: 10.1016/j.psychres.2020.113070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohm, D., Flowers, P., Stephenson, N., Waller, E., & Davis, M. D. (2014). Biography, pandemic time and risk: pregnant women reflecting on their experiences of the 2009 influenza pandemic. Health (London, England : 1997), 18(5), 493–508. 10.1177/1363459313516135. [DOI] [PubMed]
- Mak I.W., Chu C.M., Pan P.C., Yiu M.G., Ho S.C., Chan V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. General Hospital Psychiatry. 2010;32(6):590–598. doi: 10.1016/j.genhosppsych.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesch G.S., Schwirian K.P., Kolobov T. Attention to the media and worry over becoming infected: The case of the swine flu (h1n1) epidemic of 2009. Sociology of Health & Illness. 2013;35(2):325–331. doi: 10.1111/j.1467-9566.2012.01500.x. [DOI] [PubMed] [Google Scholar]
- Miller M.A., Viboud C., Balinska M., Simonsen L. The signature features of influenza pandemics–implications for policy. The New England Journal of Medicine. 2009;360(25):2595–2598. doi: 10.1056/NEJMp0903906. [DOI] [PubMed] [Google Scholar]
- Morse S.S., Mazet J.A., Woolhouse M., Parrish C.R., Carroll D., Karesh W.B.…Daszak P. Prediction and prevention of the next pandemic zoonosis. Lancet. 2012;380(9857):1956–1965. doi: 10.1016/S0140-6736(12)61684-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann R., Strack F. “Mood contagion”: The automatic transfer of mood between persons. Journal of Personality and Social Psychology. 2000;79(2):211–223. doi: 10.1037//0022-3514.79.2.211. [DOI] [PubMed] [Google Scholar]
- Nicholas D., Patershuk C., Koller D., Bruce-Barrett C., Lach L., Shaul R.Z., Matlow A. Pandemic planning in pediatric care: A website policy review and national survey data. Health Policy. 2010;96(2):134–142. doi: 10.1016/j.healthpol.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosterhoff B., Palmer C.A., Wilson J., Shook N. Adolescents' motivations to engage in social distancing during the covid-19 pandemic: Associations with mental and social health. Journal of Adolescent Health. 2020;67(2):179–185. doi: 10.1016/j.jadohealth.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel, R. (2020). Minister says COVID-19 is empowering domestic violence abusers as rates rise in parts of Canada. CBC News, April 27, 2020.
- Prati G., Pietrantoni L., Zani B. A social-cognitive model of pandemic influenza h1n1 risk perception and recommended behaviors in Italy. Risk Analysis. 2011;31(4):645–656. doi: 10.1111/j.1539-6924.2010.01529.x. [DOI] [PubMed] [Google Scholar]
- Rao N. SARS, preschool routines and children’s behaviour: Observations from preschools in Hong Kong. International Journal of Early Childhood : Journal of Omep: L’Organisation Mondiale Pour L’Education Prescolaire. 2006;38(2):11–22. doi: 10.1007/BF03168205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remmerswaal D., Muris P. Children's fear reactions to the 2009 swine flu pandemic: The role of threat information as provided by parents. Journal of Anxiety Disorders. 2011;25(3):444–449. doi: 10.1016/j.janxdis.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Roskam I., Raes M.E., Mikolajczak M. Exhausted parents: Development and preliminary validation of the parental burnout inventory. Frontiers in Psychology. 2017;8 doi: 10.3389/fpsyg.2017.00163. 163 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safdar, M., & Yasmin, A. M. (2020). Covid-19: a threat to educated Muslim women's negotiated identity in Pakistan. Gender, Work and Organization, (2020). 10.1111/gwao.12457. [DOI] [PMC free article] [PubMed]
- Secer, I., & Ulas, S. (2020). An investigation of the effect of covid-19 on OCD in youth in the context of emotional reactivity, experiential avoidance, depression and anxiety. International Journal of Mental Health and Addiction, (2020). 10.1007/s11469-020-00322-z. [DOI] [PMC free article] [PubMed]
- Serra Poirier C., Brendgen M., Vitaro F., Dionne G., Boivin M. Contagion of anxiety symptoms among adolescent siblings: A twin study. Journal of Research on Adolescence. 2017;27(1):65–77. doi: 10.1111/jora.12254. [DOI] [PubMed] [Google Scholar]
- Smil V. MIT Press; 2008. Global catastrophes and trends: The next 50 years. [Google Scholar]
- Sorkkila M., Aunola K. Risk factors for parental burnout among Finnish parents: The role of socially prescribed perfectionism. Journal of Child and Family Studies. 2019;29(3):648–659. doi: 10.1007/s10826-019-01607-1. [DOI] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Statistics Canada, 2020. Labour Force Survey, May 2020. Retrieved from www150.statcan.gc.ca/n1/daily-quotidien/200605/dq200605a-eng.htm.
- Suzuki S., Takei Y. In: Encyclopedia of Behavioral Medicine. Gellman M.D., Turner J.R., editors. Springer; New York, NY: 2013. Psychosocial factors and traumatic events. [DOI] [Google Scholar]
- Tajima E.A., Herrenkohl T.I., Moylan C.A., Derr A.S. Moderating the effects of childhood exposure to intimate partner violence: The roles of parenting characteristics and adolescent peer support. Journal of Research on Adolescence. 2011;21(2):376–394. doi: 10.1111/j.1532-7795.2010.00676.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tesini, B.L. (2020) Coronoaviruses and acute respiratory syndromes (COVID-19, MERS, and SARS). Merck Manual, December 2020.
- Tull M.T., Edmonds K.A., Scamaldo K.M., Richmond J.R., Rose J.P., Gratz K.L. Psychological outcomes associated with stay-at-home orders and the perceived impact of covid-19 on daily life. Psychiatry Research. 2020;289 doi: 10.1016/j.psychres.2020.113098. 113098 113098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher K., Bhullar N., Durkin J., Gyamfi N., Jackson D. Family violence and covid-19: Increased vulnerability and reduced options for support. International Journal of Mental Health Nursing. 2020;29(4):549–552. doi: 10.1111/inm.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vizzotto A.D.B., de Oliveira A.M., Elkis H., Cordeiro Q., Buchain P.C. In: Encyclopedia of Behavioral Medicine. Gellman M.D., Turner J.R., editors. Springer; New York, NY: 2013. Psychosocial Characteristics. [DOI] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (covid-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S.…Ho C. A longitudinal study on the mental health of general population during the covid-19 epidemic in China. Brain Behavior and Immunity. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster R.G. Otago University Press; 2018. Flu hunter: Unlocking the secrets of a virus. [Google Scholar]
- World Health Organization (2021, January 22). Coronavirus disease (COVID-19) advice for the public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- Worldometer (2021, February 1). Coronavirus. https://www.worldometers.info/coronavirus/.
- Ybarra M.L., Mitchell K.J., Palmer N.A., Reisner S.L. Online social support as a buffer against online and offline peer and sexual victimization among U.S. LGBT and non-LGBT youth. Child Abuse & Neglect. 2015;39:123–136. doi: 10.1016/j.chiabu.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildirim M., Geçer E., Akgül Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against covid-19. Psychology, Health & Medicine. 2020;1–9:1–9. doi: 10.1080/13548506.2020.1776891. [DOI] [PubMed] [Google Scholar]
- Zhou S., Zhang L., Wang L., Guo Z., Wang J., Chen J.…Chen J. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. European Child and Adolescent Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.