Abstract
PURPOSE:
This study was conducted to see whether eyeliner, mascara, or combined eyeliner and mascara (EM) use affects tear production, tear film stability, and meibomian gland (MG) loss.
METHODS:
Two hundred and twenty healthy women underwent noninvasive tear break-up time (NTBUT) measurement, meibography, and Schirmer testing. Study groups were no makeup (NM) group, eyeliner-only group, mascara-only group, and those who used both EM. The one-way analysis of variance test was used for group comparisons. Chi-square test was used for meiboscale comparison.
RESULTS:
NTBUT (seconds) results were 11.5 ± 4.8 (no makeup), 21.3 ± 69 (eyeliner only), 21.8 ± 6.5 (mascara only), and 22.5 ± 7.0 (eyeliner–mascara). The differences between groups were significant (P < 0.0001). All makeup groups (eyeliner only, mascara only, eyeliner–mascara) had significantly diminished values compared with NM group (P < 0.001, P < 0.001 and P = 0.003, respectively). Schirmer test (millimeters) results were 22.7 ± 6.4 (NM group), 21.3 ± 6.9 (eyeliner only), 21.8 ± 6.5 (mascara only), and 22.5 ± 7.0 (eyeliner–mascara) with no significant differences between groups (P = 0.66). Meiboscale grading revealed that NM group had significantly lower values of MG loss compared with eyeliner-only (EO) (P = 0.01), mascara-only (MO) (P = 0.002), and eyeliner-mascara groups (P = 0.007). There were no significant differences between EO and MO (P = 0.31), EO and eyeliner–mascara (P = 0.39), or MO and eyeliner-mascara groups (P = 0.91).
CONCLUSION:
None of the makeup groups had changes in Schirmer wetting. All eye cosmetic groups have significant changes of NTBUT and meibography compared with NM subjects, and yet combined use of EM does not affect ocular surface more adversely than their separate use.
Keywords: Cosmesis, eyelids, ocular surface, tears
INTRODUCTION
Eye cosmetics are in use since ancient Egyptian times for religious, medicinal, and cosmetic purposes.[1,2] These products have the potential to migrate onto the ocular surface and into the tear film, as seen many times during ophthalmological examinations.[3] Both eyeliner and/or mascara use have been suggested to be a major cause of lipid layer destabilization.[4]
Eyeliners are applied adjacently or directly onto the eyelid margin at the mucocutaneous junction. These can come in three forms: cake, liquid, and pencil, the latter two being the predominant forms. For stability, viscosity-controlling agents are used in liquid eyeliners, whereas pencil eyeliners consist of waxes combined with pigments, minerals, or vegetable oils.[5] Liquid eyeliners have a predisposition to infective contaminations due to their high-water content, thus preservatives are included in their formulas. Pencil eyeliners have similar risks; however, their tip can be disposed by eyeliner sharpeners, removing the exposed product and reducing the probability of contamination.[6]
Liquid mascaras come in tubes and get applied by applicator brushes to darken and elongate the eyelashes. Mascaras can be water-based, solvent-based, or a hybrid form, though commonly used ones are in the latter two categories.[7] For water resistance, pigments and waxes are added in their formula.[8]
Meibum from the meibomian glands (MG) forms the coating on the aqueous layer of the tear film and provides stability.[9] MG dysfunction can lead to altered tear film composition and ocular surface diseases, most commonly seen due to MG obstruction.[9] Eyeliner and mascara (EM) use have been suggested to be a major cause of lipid layer destabilization, yet previous studies about tear lipid film and eye cosmetics show mixed results.[10,11]
This study was conducted to see whether eyeliner, mascara, or combined use of these products affects tear production, tear film stability, and MG loss in eye cosmetics users.
METHODS
This is a cross-sectional study (from July 2020 to March 2021) aimed to analyze the effect of pencil-type eyeliner, waterproof mascara, and their combined use on tear film stability and MG loss. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of blinded University. All subjects in the study provided their written informed consent before participation. The trial was registered with ClinicalTrials.gov (blinded).
Study population
The subjects recruited in this study were healthy women without any prior ocular complaints or treatments, aged between 18 and 33 years working as the nursing staff in Hitit University Hospital. None of the subjects were contact lens wearers. The enrolled subjects were classified into four groups: no-makeup group (NM), eyeliner-only (EO) group, mascara-only group (MO), and those who used both EM. Since every subject has used some form of eye makeup previously, NM group consisted of subjects who did not use eye makeup for at least 6 months prior to the study. All subjects in the makeup groups had regular use of eyeliners, mascara, or both for at least 3 days a week within the last 6 months. Eyeliner use was defined as using pencil eyeliners inside the lash line of the lower eyelid. This was done to distinguish the differences that may come from the liquid waterproof mascara usage, which formed the MO group. Subjects were instructed to attend the clinical assessments without their makeup, so the cosmetic remnants would not interfere with dry eye tests.
Study procedures
Eye examination including visual acuity, anterior segment, and fundus examination was performed followed by the first noninvasive tear break-up time (NTBUT) measurement, meibography, and then Schirmer testing. These were measured by two experienced ophthalmology technicians (CD and BS) who did not know the object of the study. None of the subjects had any ocular or systemic diseases or drug use that may affect the ocular surface and MG.
Noninvasive tear break-up time
NTBUT for both eyes was measured using the Sirius anterior segment analysis system (Sirius; CSO, Florence, Italy). Following manual focusing, the participants were instructed to blink twice and then to keep their eyes open as long as possible. The average time of all the break-up intervals forming on the cornea was given by the software as the average NTBUT.
Meibography
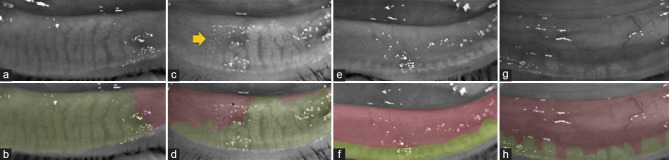
Meibography makes it possible to assess the structure of the MG in vivo by using infrared light. Imaging of the lower MG was obtained in the meibography mode of the Sirius anterior segment analysis system (CSO, Florence, Italy). The lower eyelid was everted, and imaging of the MG was obtained from the tarsal conjunctival surface. The clearest image of the MG structures was selected for grading. Eyelid borders and the borders of the MG were marked with the device software. Sirius anterior segment analysis system gives the MG loss in percentages and grades it into a digital five-grade meiboscale. Grading of this meiboscale was classified by Pult and Nichols as Grade 0 (area of loss 0%), Grade 1 (area of loss 25%), Grade 2 (area of loss 25%–50%), Grade 3 (area of loss 51%–75%), and Grade 4 (area of loss over 75%).[12] Figure 1 shows the images and meiboscales of the study participants.
Figure 1.
Meibography pictures of grades 1–4. (a) Grade 1 meibomian loss, (b) digital calculated meiboscale of the eye above. (c and d) Grade 2 loss. Arrow indicates makeup accumulation. (e) Grade 3 loss of an eyeliner-only subject. Observe the eyeliner remains on the eyelid. (f) Digital calculated meiboscale of the eye above. (g and h) Grade 4 loss
Schirmer test
The Schirmer test was conducted without topical anesthesia using the standardized strip of filter paper in order to observe reflex tearing. It was placed in a hook conformation to the lower eyelid of the outside one-third of the conjunctival sac. Subjects closed their eyelids during the test. After 5 min, the strip was removed and the amount of wetting was recorded in millimeters.
Statistical analysis
Power analysis showed that 54 subjects in each group were needed for statistical significance.[13] The primary outcome variables for this study were Schirmer, NTBUT, and meiboscale grading. Skewness for NTBUT, Schirmer, and meiboscale results were 0.305,-0.43, and 0.25, respectively, all showing symmetric distribution. The meiboscale results showed an intraclass correlation coefficient of 0.97. Continuous data with a normal distribution were represented as mean values and standard deviations. The oneway analysis of variance test with Statistical Package for the Social Science (IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY/USA) was performed. Post hoc Tukey test was used for between-group comparison. Chi-square test was used for meiboscale comparison. A value of P < 0.05 was considered statistically significant. Since both eyes give eligible data for this study, random eye of each subject was taken into the study.[14] Randomization was performed using SPSS. Right and left eye data were given to SPSS for each subject and then “select random cases, one case in each two cases” function was used in order to pick the data set for each subject.
RESULTS
Two hundred and twenty healthy women were enrolled in this study. There were 55 subjects in all four groups. The mean ages of the groups were 25.5 ± 3.8 (NM), 26.3 ± 4.2 (EO), 24.4 ± 3.6 (MO), and 24.6 ± 4.6 (EM) years. The differences between groups regarding to age were insignificant (P = 0.051).
NTBUT (seconds) results were 11.5 ± 4.8 (NM), 21.3 ± 69 (EO), 21.8 ± 6.5 (MO), and 22.5 ± 7.0 (EM). The differences between groups were significant (P < 0.0001). Post hoc Tukey test revealed that all makeup groups (EO, MO, EM) had significantly diminished NTBUT values compared with NM group (P < 0.001, P < 0.001 and P = 0.003 respectively).
Schirmer test (millimeters) results were 22.7 ± 6.4 (NM), 21.3 ± 6.9 (EO), 21.8 ± 6.5 (MO), and 22.5 ± 7.0 (EM). There were no significant differences between groups (P = 0.66).
In meiboscale grading, Chi-square test showed the P value of 0.029. Pair-wise comparisons revealed that NM group had significantly lower values of MG loss compared with EO (P = 0.01), MO (P = 0.002), and EM (P = 0.007). There were no significant differences between EO and MO (P = 0.31), EO and EM (P = 0.39), or MO and EM (P = 0.91). Meiboscale grade to group cross-tabulation is shown in Table 1.
Table 1.
Meiboscore group cross-tabulation (number of subjects in each group)
| Meiboscale grades | Total | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| 0 | 1 | 2 | 3 | 4 | ||
| No eye makeup | 18 | 27 | 8 | 2 | 0 | 55 |
| Eyeliner only | 10 | 25 | 17 | 3 | 0 | 55 |
| Mascara only | 6 | 21 | 24 | 2 | 2 | 55 |
| Eyeliner and mascara | 9 | 18 | 23 | 3 | 2 | 55 |
| Total | 43 | 91 | 72 | 10 | 4 | 220 |
DISCUSSION
To the best of our knowledge, this study is the first to compare MG changes from EO, MO and combined use of both. There are previous studies investigating the effects of eye cosmetics on the ocular surface. In vitro studies of pencil and liquid eyeliners show that they disturb the molecular structure of meibum by elevating its phase transition temperature.[13]
In vivo observational study of 180 subjects showed a significant correlation between eye cosmetic wear and reduced tear film lipid layer thickness.[10] Prabhasawat et al. study the adverse effects of eyeliner on tear film instability and MG, concluding that materials in eyeliners may be affecting MG function by inducing inflammation around the glands, regardless of the exact location of eyeliner application.[14] However, in their study, EM users were combined into a single group and the writers were not able to compare the results of sole eyeliner users with sole mascara users. In contrast, there are also some studies that found mucocutaneous junction pencil eyeliner application without any changes in tear film stability.[11]
MG loss seen in makeup groups might be a result of long duration of eyeliner pigments, mascara remnants, and their migration onto the eyelids – hence obstructing the MG, which in result might affect the delivery of meibum to the ocular surface. Prabhasawat et al. also found MG structural and functional alterations – adding that these changes were not intense enough to produce ocular symptoms.[14]
This study found no significant difference in Schirmer wetting between groups. Previous studies argued that there might be epiphora due to migration and accumulation of kohl in the conjunctiva and lacrimal sac or no change in at all in Schirmer testing.[15,16]
Hypothesis for this study was more cosmetics use should cause more ocular surface damage. However, the results showed no difference between single or combined cosmetics use. This might be because since both EM use may coat the openings of MGs by themselves, their combined use does not actually make any significant difference. However, this is a cross-sectional study and in order to completely come to this conclusion, prospective studies are necessary.
There are some limitations to this study. Foremost is the necessity of higher subject and group numbers that may include comparisons for pencil and liquid eyeliners, different types of eye makeup cleaners and removal styles (water, cotton pads, hand application of cleaner). This study was conducted using a single examination, so further long-term and prospective studies that include baseline objective and subjective dry eye tests before and after cosmetics use can have additional value. Lipid layer interferometry and expressed meibum grading can also be added to future studies. Furthermore, the duration of the use of cosmetics was varied in this study. Subjects did not have specific timelines for when they first started to use eye makeup (for example “since my teen years,” “at least for 2 years” and such) so the criterion was specifically “at least three days a week within the last six months.” With higher number of subjects, cosmetic use in longer duration periods can be studied.
CONCLUSION
This study demonstrated that eye makeup does not affect tear production; all of the studied eye cosmetics cause significant changes of NBUT and meibography compared with NM subjects; however, combined use of EM does not affect ocular surface more adversely than their separate use.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Draelos ZK. Eye cosmetics. Dermatol Clin. 1991;9:1–7. [PubMed] [Google Scholar]
- 2.Wang MT, Craig JP. Investigating the effect of eye cosmetics on the tear film: Current insights. Clin Optom (Auckl) 2018;10:33–40. doi: 10.2147/OPTO.S150926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng A, Evans K, North RV, Purslow C. Migration of cosmetic products into the tear film. Eye Contact Lens. 2015;41:304–9. doi: 10.1097/ICL.0000000000000124. [DOI] [PubMed] [Google Scholar]
- 4.Franck C, Skov P. Foam at inner eye canthus in office workers, compared with an average Danish population as control group. Acta Ophthalmol (Copenh) 1989;67:61–8. doi: 10.1111/j.1755-3768.1989.tb00724.x. [DOI] [PubMed] [Google Scholar]
- 5.Orecchinoi A. Baran R, Maibach H. Cosmetic Dermatology. London UK: Martin Dunitz; 1994. Eye make-up; pp. 143–9. [Google Scholar]
- 6.Draelos ZD. Special considerations in eye cosmetics. Clin Dermatol. 2001;19:424–30. doi: 10.1016/s0738-081x(01)00204-8. [DOI] [PubMed] [Google Scholar]
- 7.Ng A, Evans K, North RV, Jones L, Purslow C. Impact of eye cosmetics on the eye, adnexa, and ocular surface. Eye Contact Lens. 2016;42:211–20. doi: 10.1097/ICL.0000000000000181. [DOI] [PubMed] [Google Scholar]
- 8.Hollenberg J. Color Cosmetics. In: Rieger MM, editor. Harry’s Cosmeticology. Vol. 523. New York, NY: Chemical Publishing Co., Inc; 2000. p. 572. [Google Scholar]
- 9.Chhadva P, Goldhardt R, Galor A. Meibomian gland disease: The role of gland dysfunction in dry eye disease. Ophthalmology. 2017;124:S20–6. doi: 10.1016/j.ophtha.2017.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franck C. Fatty layer of the precorneal film in the 'office eye syndrome'. Acta Ophthalmol (Copenh) 1991;69:737–43. doi: 10.1111/j.1755-3768.1991.tb02052.x. [DOI] [PubMed] [Google Scholar]
- 11.Ng A, Evans K, North R, Purslow C. The effects of cosmetic eye pencil application on the tear film and ocular surface. Invest Ophthalmol Vis Sci. 2013;54:952. [Google Scholar]
- 12.Pult H, Nichols JJ. A review of meibography. Optom Vis Sci. 2012;89:E760–9. doi: 10.1097/OPX.0b013e3182512ac1. [DOI] [PubMed] [Google Scholar]
- 13.Hunter M, Bhola R, Yappert MC, Borchman D, Gerlach D. Pilot study of the influence of eyeliner cosmetics on the molecular structure of human meibum. Ophthalmic Res. 2015;53:131–5. doi: 10.1159/000371852. [DOI] [PubMed] [Google Scholar]
- 14.Prabhasawat P, Chirapapaisan C, Chitkornkijsin C, Pinitpuwadol W, Saiman M, Veeraburinon A. Eyeliner induces tear film instability and meibomian gland dysfunction. Cornea. 2020;39:473–8. doi: 10.1097/ICO.0000000000002198. [DOI] [PubMed] [Google Scholar]
- 15.Hidayat AA, Weatherhead RG, al-Rajhi A, Johnson FB. Conjunctival and lacrimal sac pigmentation by kohl (eyeliner) Br J Ophthalmol. 1997;81:418. doi: 10.1136/bjo.81.5.415d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alkawally M, Paugh J, Van de Pol C, Lin R, Sasai A, Nguyen A. The effect of chronic marginal eyeliner use on tears and meibomian gland function. Poster presented at: Academy 2019 Orlando and 3rd World Congress of Optometry; Orlando, FL. 2019 October;:23–7. [Google Scholar]