Abstract
Background
Social and environmental factors play an important role in the rising health care burden of cardiovascular disease. The Centers for Disease Control and Prevention developed the Social Vulnerability Index (SVI) from US census data as a tool for public health officials to identify communities in need of support in the setting of a hazardous event. SVI (ranging from a least vulnerable score of 0 to a most vulnerable score of 1) ranks communities on 15 social factors including unemployment, minoritized groups status, and disability, and groups them under 4 broad themes: socioeconomic status, housing and transportation, minoritized groups, and household composition. We sought to assess the association of SVI with self‐reported prevalent cardiovascular comorbidities and atherosclerotic cardiovascular disease (ASCVD).
Methods and Results
We performed a retrospective cohort analysis of adults (≥18 years) in the Behavioral Risk Factor Surveillance System 2016 to 2019. Data regarding self‐reported prevalent cardiovascular comorbidities (including diabetes, hypertension, hyperlipidemia, smoking, substance use), and ASCVD was captured using participants' response to a structured telephonic interview. We divided states on the basis of the tertile of SVI (first—participant lives in the least vulnerable group of states, 0–0.32; to third—participant lives in the most vulnerable group of states, 0.54–1.0). Multivariable logistic regression models adjusting for age, race and ethnicity, sex, employment, income, health care coverage, and association with federal poverty line were constructed to assess the association of SVI with cardiovascular comorbidities. Our study sample consisted of 1 745 999 participants ≥18 years of age. States in the highest (third) tertile of social vulnerability had predominantly Black and Hispanic adults, lower levels of education, lower income, higher rates of unemployment, and higher rates of prevalent comorbidities including hypertension, diabetes, chronic kidney disease, hyperlipidemia, substance use, and ASCVD. In multivariable logistic regression models, individuals living in states in the third tertile of SVI had higher odds of having hypertension (odds ratio (OR), 1.14 [95% CI, 1.11–1.17]), diabetes (OR, 1.12 [95% CI, 1.09–1.15]), hyperlipidemia (OR, 1.09 [95% CI, 1.06–1.12]), chronic kidney disease (OR, 1.17 [95% CI, 1.12–1.23]), smoking (OR, 1.05 [95% CI, 1.03–1.07]), and ASCVD (OR, 1.15 [95% CI, 1.12–1.19]), compared with those living in the first tertile of SVI.
Conclusions
SVI varies across the US states and is associated with prevalent cardiovascular comorbidities and ASCVD, independent of age, race and ethnicity, sex, employment, income, and health care coverage. SVI may be a useful assessment tool for health policy makers and health systems researchers examining multilevel influences on cardiovascular‐related health behaviors and identifying communities for targeted interventions pertaining to social determinants of health.
Keywords: cardiovascular disease, risk factors, social vulnerability, SVI
Subject Categories: Cardiovascular Disease, Health Services, Social Determinants of Health
Nonstandard Abbreviations and Acronyms
- ADI
Area Deprivation Index
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- SDOH
social determinants of health
- SVI
Social Vulnerability Index
- SVI‐Ts
Social Vulnerability Index tertiles
Clinical Perspective.
What Is New?
Adverse social determinants of health, including financial insecurity, poor access to health care, neighborhood deprivation, and race‐ and ethnicity‐based discrimination, predispose marginalized communities to adverse health outcomes. We sought to assess whether the Social Vulnerability Index, a composite measure of a community's social determinants of health, is associated with cardiovascular health.
We analyzed a nationally representative sample to evaluate the association between the Social Vulnerability Index and self‐reported cardiovascular comorbidities (including diabetes, hypertension, hyperlipidemia, smoking, and substance use) and atherosclerotic cardiovascular disease.
What Are the Clinical Implications?
We found that the Social Vulnerability Index varies across the US states and is associated with prevalent cardiovascular comorbidities and atherosclerotic cardiovascular disease, independent of age, sex, income, health care coverage, or race and ethnicity, such that higher social vulnerability was associated with worse cardiovascular health.
The Social Vulnerability Index may be a useful assessment tool for health policy makers and health systems researchers examining multilevel influences on cardiovascular‐related health behaviors and identifying communities for targeted interventions pertaining to social determinants of health.
Cardiovascular diseases are the leading cause of mortality and a significant contributor to disability, with a 2‐fold increase in global prevalence and a 1.5‐fold increase in associated mortality between 1990 and 2019. 1 In the United States, it is the cause of death of nearly 900 000 adults, and carries a health care cost burden of ≈$213 billion annually. 2 This trend is concerning, as there have been significant therapeutic advancements in the primary and secondary prevention of cardiovascular disease. It may be reflective of a change in societal and environmental factors that impact dietary patterns and levels of physical activity. Further, there are significant disparities in access to health care across race and ethnicity and economic groups, which may impact the overall cardiovascular health of the population. 3 Adverse social circumstances, referred to as social determinants of health (SDOH), including financial insecurity, poor access to health care, neighborhood deprivation, and race‐ and ethnicity‐based discrimination, predispose marginalized communities to adverse health outcomes. 3 , 4 Thus, an in‐depth assessment of SDOH that influence cardiovascular health can help identify populations that may benefit the most from targeted public health interventions.
The Centers for Disease Control and Prevention (CDC) developed the Social Vulnerability Index (SVI) from US census data to help public health officials identify communities that may be at high risk for hazardous events such as disease outbreak and natural disasters. It takes into account important SDOH such as education, employment, population density, housing, and race and ethnicity composition. 5
Although originally designed to allocate resources such as food, water, and emergency personnel to communities in the event of a natural disaster, social vulnerability has been shown to be a significant determinant of health outcomes, including cognition, disability, and overall mortality. 6 , 7
Many of the components of the SVI closely associate with a population's ability to access health care resources, be adherent to the recommended therapeutic plan of action, or follow up consistently with the health care system; which may consequently affect risk of cardiovascular disease. For example, communities with lower levels of education and income may not have sufficient health care literacy or financial means for health care and a healthy and balanced diet. Therefore, it is possible that the SVI could inform not only emergency preparedness, but also efforts to impact chronic diseases such as the epidemic of cardiometabolic diseases. The present study sought to evaluate the association of SVI with cardiovascular risk factors and atherosclerotic cardiovascular disease (ASCVD) across the United States using a large, nationally representative sample.
Methods
All data and materials used in this article have been made publicly available and can be accessed at https://www.cdc.gov/brfss/data_documentation/index.htm (Behavioral Risk Factor Surveillance System data) and https://www.atsdr.cdc.gov/placeandhealth/svi/at‐a‐glance_svi.html (Social Vulnerability Index data).
The Behavioral Risk Factor Surveillance System (BRFSS) survey, established by the CDC, is a nationwide telephone‐based questionnaire of a representative sample of US residents regarding health‐related risk behaviors, chronic health conditions, and use of preventive services. BRFSS includes participants in all 50 states as well as the District of Columbia and 3 US territories, making it the largest telephone‐based survey in the world. The BRFSS allows population level investigations on the association of behavioral risk factors with various diseases. It is a deidentified and publicly available (http://www.cdc.gov/brfss) data set, and hence exempted from the institutional review board approval. The estimates provided by the BRFSS have previously been validated against other established surveys such as the National Health and Nutrition Examination Survey and the National Health Interview Survey. 8 , 9
We used self‐reported data from the 2016 to 2019 BRFSS surveys. Baseline and demographic characteristics, including participant age, race and ethnicity, employment, education status, and income level, were self‐reported. ASCVD status was classified on the basis of participants responding to the question, “Have you ever had coronary heart disease or myocardial infarction or stroke?” Cardiovascular comorbidities were identified on the basis of the following questions: “Have you ever been told by a doctor, nurse, or other health professional that you have high blood pressure?”; “Have you ever been told by a doctor, nurse, or other health professional that you have diabetes?”; “Have you ever been told by a doctor, nurse, or other health professional that your blood cholesterol is high?”; and “Have you ever been told by a doctor, nurse, or other health professional that you have kidney disease, excluding kidney stones, bladder infection, or incontinence?” Smoking status was ascertained by asking the participants, “Do you now smoke cigarettes every day, some days, or not at all?” Those who replied “every day” or “some days” were considered current smokers. E‐cigarette status was ascertained by asking the participants, “Do you now use e‐cigarettes or other vaping products every day, some days, or not at all?” Those who replied “every day” or “some days” were considered current e‐cigarette users. Current marijuana use was defined as the use of marijuana or hashish for ≥1 days in the past 30 days.
We used SVI data from the CDC's Agency for Toxic Substances and Disease Registry, 10 which ranks every US census tract on 15 social attributes using the American Community Survey data and groups them into 4 related themes: socioeconomic status (below poverty, unemployed, income, and no high school diploma); household composition and disability (aged ≥65 years, aged ≤17 years, aged >5 years with a disability, and single‐parent households), minoritized groups and language (minoritized groups and individuals speak English “less than well”), and housing type and transportation (multiunit structure, mobile home, crowding, no vehicle, and group quarters) (Table 1).
Table 1.
Summary of Themes and Underlying Social Factors That Constitute the Social Vulnerability Index 5
| Themes | Social factors |
|---|---|
| Socioeconomic status | Below poverty line |
| Unemployed | |
| Income | |
| No high school diploma | |
| Household composition and disability | Aged ≥65 y |
| Aged ≤17 y | |
| Civilian with a disability | |
| Single‐parent households | |
| Minoritized groups and language | Minoritized groups |
| Aged ≥5 y who speaks English “less than well” | |
| Housing type and transportation | Multiunit structures |
| Mobile homes | |
| Crowding | |
| No vehicle | |
| Group quarters |
Based on the methodology that measures census tract rankings, the SVI files also provide county‐level rankings, which can then be used to generate state‐level rankings across the entire United States for the 15 individual variables and 4 themes—the overall state‐level SVI. The percentile rank ranges from 0 to 1, with higher values exhibiting greater vulnerability than the lower values. For the purpose of this study, we used state‐level SVI rankings to link it with the demographic and health‐behavior related data for each state provided in the BRFSS; that is, while health‐related data were analyzed at an individual participant level, the SVI was used as an ecological variable depending on which state the participant resided in.
We analyzed these cross‐sectional data using survey weights for BRFSS provided by the CDC to account for the survey design and ensure the representativeness of the data to the US population. The distribution of health‐related behavioral risk factors in groups on the basis of SVI tertiles (SVI‐Ts; first—participant lives in the least vulnerable group of states, 0–0.32; to third—participant lives in the most vulnerable group of states, 0.54–1.0) was ascertained. A multivariable logistic regression model adjusting for age, race and ethnicity, sex, employment, income, health care coverage, and association with federal poverty line (all variables were collected at the individual level) was used to study the association of social vulnerability with the presence of cardiovascular comorbidities, including diabetes, hypertension, smoking, hyperlipidemia, substance use, and ASCVD. We further mapped the prevalence of diabetes, hypertension, and ASCVD stratified by SVI‐Ts across the US states. As a prespecified exploratory analysis, we evaluated the associations of each individual component of the overall SVI with cardiovascular comorbidities, including diabetes, hypertension, smoking, hyperlipidemia, and ASCVD. To compare the SVI with other measures of SDOH, we performed secondary analyses to evaluate the association of cardiovascular comorbidities across tertiles of the Area Deprivation Index (ADI), 11 with the aim of assessing which score is a better statewide discriminator of the study sample's SDOH. All analyses were conducted using Stata version 16.1 (StataCorp, College Station, TX).
Results
Our study sample included 1 745 999 participants aged >18 years. The baseline characteristics of the participants stratified by SVI‐Ts are listed in Table 2. Compared with states in the second and first SVI‐Ts, states in the third SVI‐T (most vulnerable) had a higher proportion of Black (13.4% versus 11.4% versus 7.4%) and Hispanic (22.5% versus 10.8% versus 7.5%) participants, lower proportion of college‐educated participants (25.7% versus 29.4% versus 30.7%), higher proportion of families with <$10 000 annual income (6.6% versus 4.6% versus 3.5%), and higher rates of unemployment (20.1% versus 17.3% versus 14.2%). They also had a higher prevalence of cardiovascular comorbidities, including hypertension (33.4% versus 32% versus 30.3%), diabetes (12.1% versus 10.9% versus 9.6%), chronic kidney disease (CKD; 3.3% versus 2.9% versus 2.6%), hyperlipidemia (31.9% versus 31.3% versus 30.1%), and ASCVD (8.8% versus 8.5% versus 7.6%) (Table 3).
Table 2.
Self‐Reported Baseline and Demographic Characteristics Across Tertiles of SVI
| First tertile (SVI 0.00–0.32) | Second tertile (SVI 0.33–0.53) | Third tertile (SVI 0.54–1) | P value | |
|---|---|---|---|---|
| Female sex, n (%) | 313 224 (51.1) | 309 462 (51.4) | 330 269 (51.2) | 0.32 |
| Race and ethnicity, n (%) | ||||
| White | 486 925 (78.1) | 424 895 (69.6) | 396 913 (55.0) | <0.001 |
| Black | 23 269 (7.8) | 39 966 (11.4) | 74 122 (13.4) | |
| Hispanic | 23 808 (7.5) | 38 917 (10.8) | 62 875 (22.5) | |
| Other * | 29 325 (6.6) | 46 298 (8.2) | 39 027 (9.1) | |
| Age, n (%) | <0.001 | |||
| 18–34 y | 88 867 (29.6) | 90 434 (29.3) | 97 220 (30.2) | |
| 35–44 y | 66 194 (15.9) | 64 182 (15.9) | 68 819 (16.7) | |
| 45–54 y | 86 593 (16.2) | 88 222 (16.5) | 88 859 (16.5) | |
| 55–64 y | 124 716 (17.3) | 120 209 (17.1) | 119 095 (16.1) | |
| ≥65 y | 206 641 (30.0) | 199 050 (21.1) | 211 083 (20.5) | |
| Education status, n (%) | <0.001 | |||
| <High school | 29 610 (9.5) | 37 453 (11.6) | 58 573 (15.5) | |
| High school–college | 318 958 (59.7) | 302 365 (59.1) | 324 781 (58.9) | |
| >College | 222 370 (30.7) | 219 960 (29.4) | 199 439 (25.7) | |
| Income level, n (%) | ||||
| <$10 k | 15 657 (3.5) | 19 601 (4.6) | 28 736 (6.6) | <0.01 |
| $10–$15 k | 19 756 (3.6) | 21 663 (4.2) | 29 108 (5.6) | |
| $15–$20 k | 29 242 (5.9) | 32 388 (7.0) | 40 256 (8.0) | |
| $20–$25 k | 38 332 (7.2) | 41 771 (8.7) | 48 220 (9.9) | |
| $25–$35 k | 48 715 (9.3) | 48 127 (9.8) | 53 034 (10.7) | |
| $35–$50 k | 69 939 (13.5) | 64 138 (13.1) | 66 281 (13.0) | |
| $50–$75 k | 83 834 (16.8) | 74 653 (15.5) | 71 011 (14.2) | |
| >$75 k | 171 688 (40.2) | 165 761 (37.1) | 138 376 (32.1) | |
| Employment status, n (%) | ||||
| Employed | 304 944 (61.5) | 280 218 (58.1) | 265 693 (55.9) | <0.01 |
| Unemployed | 77 151 (14.2) | 89 787 (17.3) | 115 086 (20.1) | |
| Student | 13 870 (5.7) | 15 392 (5.8) | 15 569 (5.5) | |
| Retired | 171 230 (18.5) | 170 815 (18.8) | 181 926 (18.4) | |
Data are presented as unweighted N (weighted proportions). SVI indicates Social Vulnerability Index.
*Other indicated BRFSS has delieneated remaining ethnicities.
Table 3.
Self‐Reported Cardiovascular Comorbidities and Health Related Behaviors Across Tertiles of SVI
| First tertile (SVI 0.00–0.32) | Second tertile (SVI 0.33–0.53) | Third tertile (SVI 0.54–1) | P value | |
|---|---|---|---|---|
| Hypertension, n (%) | 112 788 (30.3) | 102 793 (32.0) | 124 619 (33.4) | <0.01 |
| Hyperlipidemia, n (%) | 98 736 (30.1) | 91 183 (31.3) | 104 305 (31.9) | <0.01 |
| Diabetes, n (%) | 70 107 (9.6) | 74 066 (10.9) | 89 824 (12.1) | <0.01 |
| Current smoker, n (%) | 74 172 (14.8) | 77 868 (16.4) | 89 078 (15.9) | <0.01 |
| Current E‐cigarette use, n (%) | 11 275 (5.3) | 13 029 (5.7) | 13 386 (5.8) | <0.01 |
| Current marijuana use, n (%) | 9326 (8.5) | 3663 (9.7) | 9933 (11.3) | <0.01 |
| Chronic kidney disease, n (%) | 19 340 (2.6) | 21 314 (2.9) | 25 569 (3.3) | <0.01 |
| ASCVD, n (%) | 60 877 (7.6) | 63 336 (8.5) | 76 052 (8.8) | <0.01 |
Data are presented as unweighted N (weighted proportions). ASCVD indicates atherosclerotic cardiovascular disease; and SVI, social vulnerability index.
Geographical mapping of states by SVI‐Ts showed that the largest concentration of states with more social vulnerabilities were clustered across the southwestern and southeastern parts of the United States (Figure S1). The distribution of the prevalence of diabetes, hypertension, and ASCVD by SVI‐Ts (Figures 1 and 2) showed a similar trend.
Figure 1. State‐level variation in tertiles of social vulnerability index and prevalence of self‐reported hypertension (A) and diabetes (B).
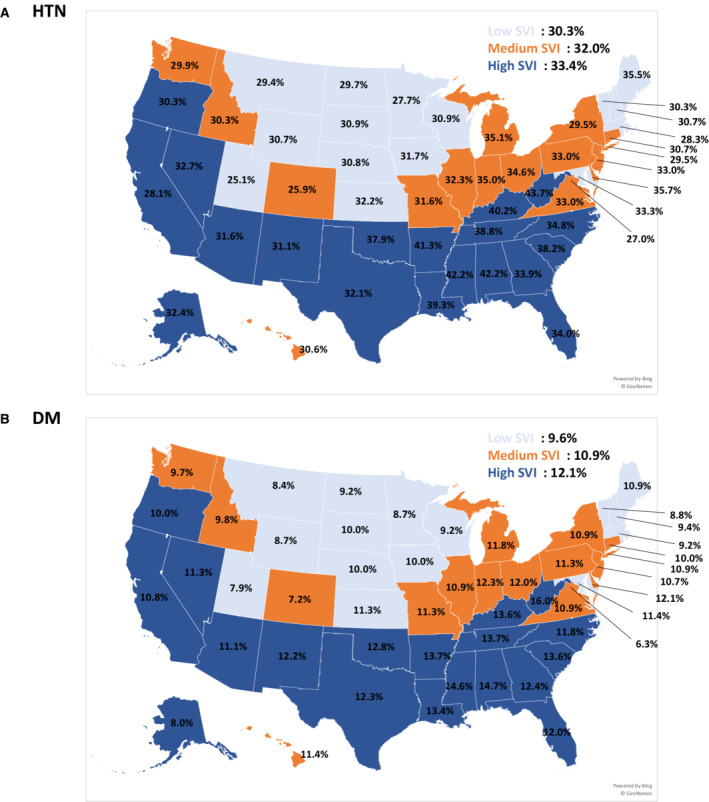
SVI indicates Social Vulnerability Index.
Figure 2. State‐level variation in tertiles of the SVI and prevalence of self‐reported atherosclerotic cardiovascular disease.
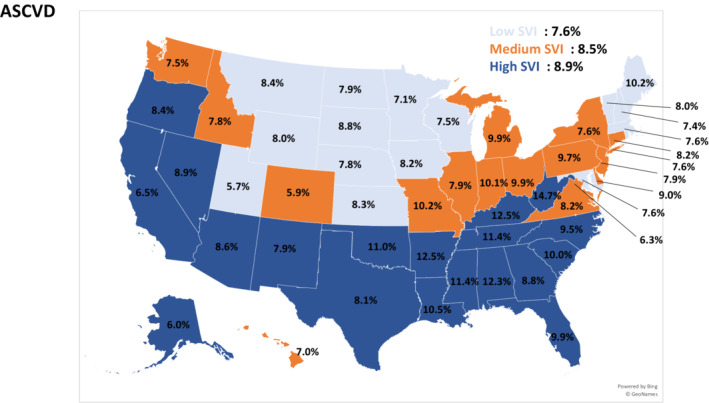
ASCVD indicates atherosclerotic cardiovascular disease; and SVI, Social Vulnerability Index.
In multivariable logistic regression models adjusting for age, race and ethnicity, sex, employment, income, health care coverage, and association with the federal poverty line, the participants residing in states in the third SVI‐T had higher odds of hypertension (odds ratio [OR], 1.14 [95% CI, 1.11–1.17]), diabetes (OR, 1.12 [95% CI, 1.09–1.15]), hyperlipidemia (OR, 1.09 [95% CI, 1.06–1.12]), CKD (OR, 1.17 [95% CI, 1.12–1.23]), smoking (OR, 1.05 [95% CI, 1.03–1.07]), e‐cigarette use (OR, 1.22 [95% CI, 1.16–1.29]), marijuana use (OR, 1.57 [95% CI, 1.49–1.67]), and ASCVD (OR, 1.15 [95% CI, 1.12–1.19]), compared with the participants residing in states in the first SVI‐T (Table 4). Further, the odds of the constituent participants having these comorbidities increased across increasing SVI‐Ts (Table 4). In the prespecified exploratory analysis stratified by individual themes of SVI (Table 5), we found that the socioeconomic status and household composition were more strongly associated with the prevalence of cardiovascular comorbidities and health‐related behaviors, whereas the minoritized groups and housing/transport component were associated with higher odds of use of e‐cigarettes and marijuana, as well as self‐reported CKD, but not with other cardiovascular comorbidities and health‐related behaviors. For the minoritized groups and housing/transport components, higher vulnerability was associated with lower odds of cigarette smoking. In the secondary analyses comparing the SVI to the ADI, we found that the ADI was numerically more strongly associated with certain cardiovascular comorbidities such as hypertension, diabetes, and hyperlipidemia, while the SVI had a stronger association with other conditions such as CKD and marijuana use (Table S1).
Table 4.
Odds Ratios (95% CIs) for the Association of Tertiles of SVI With Self‐Reported Chronic Comorbidities
| Odds ratio (95% CI) | ||
|---|---|---|
| Unadjusted | Adjusted | |
| Hypertension | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.08 (1.06–1.10) | 1.03 (1.01–1.06) |
| SVI ≥0.54 | 1.15 (1.13–1.18) | 1.14 (1.11–1.17) |
| Hyperlipidemia | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.06 (1.04–1.08) | 1.04 (1.01–1.06) |
| SVI ≥0.54 | 1.09 (1.06–1.11) | 1.09 (1.06–1.12) |
| Diabetes | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.15 (1.13–1.18) | 1.06 (1.03–1.08) |
| SVI ≥0.54 | 1.29 (1.26–1.32) | 1.12 (1.09–1.15) |
| Current smoker | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.12 (1.10–1.15) | 1.11 (1.09–1.14) |
| SVI ≥0.54 | 1.08 (1.06–1.10) | 1.05 (1.03–1.07) |
| Current E‐cigarette use | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.10 (1.05–1.15) | 1.15 (1.09–1.21) |
| SVI ≥0.54 | 1.09 (1.04–1.14) | 1.22 (1.16–1.29) |
| Current marijuana use | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.16 (1.09–1.23) | 1.17 (1.09–1.25) |
| SVI ≥0.54 | 1.37 (1.31–1.44) | 1.57 (1.49–1.67) |
| CKD | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.11 (1.07–1.15) | 1.05 (1.01–1.10) |
| SVI ≥0.54 | 1.27 (1.22–1.32) | 1.17 (1.12–1.23) |
| ASCVD | ||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.13 (1.10–1.15) | 1.09 (1.06–1.12) |
| SVI ≥0.54 | 1.18 (1.15–1.21) | 1.15 (1.12–1.19) |
ASCVD indicates atherosclerotic cardiovascular disease; CKD, chronic kidney disease; and SVI, Social Vulnerability Index. Model is adjusted for age, sex, race and ethnicity, employment, income, association with federal poverty line, and health plan coverage.
Table 5.
Odds Ratios (95% CIs) for the Association of Tertiles of Individual Components of the Overall SVI (Modified SVI) With Self‐Reported Cardiovascular Comorbidities
|
Socioeconomic status component Odds ratio (95% CI) |
Household composition component Odds ratio (95% CI) |
Minoritized groups component Odds ratio (95% CI) |
Housing/transportation component Odds ratio (95% CI) |
|
|---|---|---|---|---|
| Adjusted | Adjusted | Adjusted | Adjusted | |
| Hypertension | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.03 (1.01–1.05) | 1.06 (1.03–1.09) | 1.01 (0.98–1.04) | 1.05 (1.02–1.07) |
| SVI ≥0.54 | 1.14 (1.11–1.17) | 1.23 (1.20–1.27) | 0.98 (0.95–1.01) | 0.97 (0.95–0.99) |
| Hyperlipidemia | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.01 (0.99–1.04) | 0.95 (0.93–0.98) | 1.04 (1.01–1.06) | 1.04 (1.01–1.06) |
| SVI ≥0.54 | 1.08 (1.05–1.11) | 1.08 (1.05–1.11) | 1.03 (0.99–1.06) | 1.03 (0.99–1.05) |
| Diabetes | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.06 (1.03–1.09) | 1.06 (1.03–1.09) | 0.97 (0.95–0.99) | 1.02 (1.00–1.05) |
| SVI ≥0.54 | 1.14 (1.11–1.17) | 1.20 (1.17–1.23) | 0.97 (0.94–0.99) | 0.98 (0.95–1.00) |
| Current E‐cigarette use | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.11 (1.05–1.16) | 0.98 (0.93–1.04) | 1.08 (1.03–1.14) | 1.05 (0.99–1.11) |
| SVI ≥0.54 | 1.19 (1.12–1.25) | 1.14 (1.08–1.20) | 1.07 (1.01–1.14) | 1.07 (1.02–1.13) |
| Current marijuana use | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.10 (1.02–1.16) | 1.43 (1.35–1.51) | 0.85 (0.79–0.91) | 0.98 (0.92–1.05) |
| SVI ≥0.54 | 1.49 (1.41–1.57) | 0.74 (0.69–0.79) | 1.53 (1.42–1.65) | 1.65 (1.54–1.76) |
| Current smoker | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.11 (1.09–1.13) | 1.04 (1.02–1.07) | 0.85 (0.83–0.87) | 1.09 (1.06–1.11) |
| SVI ≥0.54 | 1.17 (1.15–1.19) | 1.17 (1.14–1.20) | 0.80 (0.78–0.82) | 0.90 (0.87–0.92) |
| CKD | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.04 (1.01–1.06) | 1.12 (1.06–1.18) | 0.98 (0.94–1.02) | 1.02 (0.98–1.07) |
| SVI ≥0.54 | 1.03 (1.01–1.05) | 1.19 (1.13–1.24) | 1.08 (1.03–1.13) | 1.06 (1.01–1.11) |
| ASCVD | ||||
| SVI <0.33 | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) | 1.00 (ref) |
| SVI 0.33–0.53 | 1.07 (1.04–1.10) | 1.06 (1.02–1.09) | 0.98 (0.96–1.01) | 1.10 (1.07–1.13) |
| SVI ≥0.54 | 1.16 (1.13–1.20) | 1.20 (1.17–1.24) | 0.95 (0.93–0.98) | 0.99 (0.97–1.03) |
Model is adjusted for age, sex, race and ethnicity, employment, income, association with federal poverty line, and health plan coverage. ASCVD indicates atherosclerotic cardiovascular disease; CKD, chronic kidney disease; ref, reference value; and SVI, Social Vulnerability Index.
Discussion
In the present study, we found that social vulnerability was associated with worse overall and cardiovascular health, such that participants residing in US states with a higher SVI had a higher prevalence of chronic conditions and at‐risk health behaviors including diabetes, hypertension, hyperlipidemia, smoking, e‐cigarette use, marijuana use, ASCVD, and CKD. Further, this pattern of disease prevalence had a geographical trend, such that the southwestern and southeastern states consistently had higher social vulnerability and a higher prevalence of cardiovascular disease, compared with the rest of the country.
The causal relationships between traditional risk factors (such as smoking, diabetes, hypertension, and dyslipidemia) and ASCVD have been extensively studied, allowing clinicians and health policy makers to devise and implement counteractive measures. However, the association of disease processes with socioeconomic and environmental factors remains incompletely understood. A large part of this problem is the complex interplay of multiple social, cultural, environmental, and economic factors. The SVI is unique in its holistic approach leveraging 4 important themes, with 15 underlying subcomponents that can help quantify the complex interplay of the social determinants of health and can be used to assess a community's ability to adequately support its population in the face of natural disasters. In our study, we found that the socioeconomic and household components were more strongly associated with the prevalence of cardiovascular comorbidities, compared with housing and transport and minoritized group components. The socioeconomic theme takes into account a community's average income and education status. Studies have shown that higher education levels and health care literacy are inversely associated with the incidence of ASCVD. 12 An individual's economic status affects their ability to follow a nutritious dietary pattern, seek health care, and adhere to guideline‐directed medical therapy. 13 The household composition theme is reflective of the number of dependents in a household and other life stressors, including being a single parent and caring for the elderly, factors that have been associated with higher risk for ASCVD. 14 Based on our findings and previous literature, the authors believe that education attainment, economic status, and the number of dependents have a greater impact on a population's health status than other components of the SVI. Racial and ethnic minoritized groups, including Blacks, Hispanics, and Asians, have a higher prevalence of traditional cardiovascular risk factors and lower use of guideline‐directed treatment, and may face language and cultural barriers in accessing the care they need. 15 Finally, the housing and transportation theme incorporates the impact of the physical and cultural environment. Disadvantaged neighborhoods have been shown to have higher population density; lower access to transportation; fewer sidewalks and recreation spaces for physical activity; fewer grocery stores with affordable, healthy food; and lack of social support and community cohesion—all of which increase the risk for cardiovascular disease directly or indirectly. 16 Thus, even though the SVI was developed as a tool to identify populations at greater risk in the setting of natural disasters, the findings of our study suggest it can be used for identifying populations in greater need of preventive care to lower the morbidity and mortality related to cardiovascular disease and its associated risk factors.
Other measures of SDOH, such as the ADI 11 or Social Deprivation Index, 17 although similar in theme, are not as comprehensive as the SVI. While the ADI predominantly focuses on economic deprivation, 11 the Social Deprivation Index covers limited social characteristics (poverty, <12 years of education, single‐parent household, rented housing unit, the overcrowded housing unit, households without a car, and nonemployed adults aged <65 years), limiting their scope when compared with SVI. 17 The SVI covers some unique variables, such as minoritized groups, English language insufficiency, elderly (aged >65 years), children (aged <18 years), and aged >5 years with a disability, allowing a more global assessment of social vulnerability for a given community. Further, being a composite of 4 individual themes, the SVI allows a more granular exploration of individual components of SDOH that can impact a population's health status and provide actionable information to health policy makers.
A previous cross‐sectional analysis from the Canadian PACEinMM (Patient‐Centered Innovations for Persons With Multimorbidity) study showed that in a cohort of 301 adult participants from Canada, the SVI strongly correlated with the prevalence of chronic conditions, such as obesity, depression/anxiety, and cardiovascular diseases. 18 Their study used a related but modified version of the SVI compared with the one developed by the CDC. 18 Another study by Gay et al 19 used the SVI to explain county‐level variation in youth physical fitness across the public schools of Georgia. In their study of 2126 public schools, they found that SVI themes explained most of the variation (R2 values, 11.5% to 26.6%) in youth physical fitness levels.
Previous studies have also shown that lower economic status is consistently associated with higher ASCVD risk. 20 A multicenter study from the United States and Finland found that lower economic status was associated with a higher prevalence of ASCVD, nonfatal myocardial infarction, and sudden cardiac death. 20 Importantly, the impact of economic status on an individual's health may be modifiable, such that improvement in economic condition may lead to better health status. This was shown in a study of 5579 adults without cardiovascular disease who were enrolled in the Health and Retirement Study. 21 In their study, Machado et al. found that participants who experienced upward wealth mobility (by at least 1 quintile) had independently lower cardiovascular risk compared with participants with stable wealth from 50 to 64 years of age, and participants who experienced downward wealth mobility had higher cardiovascular risk after 65 years of age. 21 This relation with economic status could in part be related to lack of access to quality care, inability to afford medications as well as lower use of guideline‐directed medical therapy. 13 In addition to an individual's economic status, an individual's physical and cultural environment are also associated with health status. 11 , 16 Epidemiologic data from the ARIC (Atherosclerosis Risk in Communities) and the Jackson Heart Study have shown that individuals residing in disadvantaged neighborhoods have worse cardiometabolic health at baseline and have higher risk of incident ASCVD on long‐term follow‐up. 16 , 22 Low‐income neighborhoods often have fewer supermarkets, and consequently limited access to fresh fruits and vegetables, which may in turn contribute to increased ASCVD risk. 23 , 24 People with socioeconomic disadvantage are more prone to smoking, heavier alcohol use, obesity, and physical inactivity and may have limited access to preventive care, which can contribute to the development of cardiovascular diseases. 25 The SVI, by providing a composite metric encompassing important social determinants of health, may serve as a valuable tool for both researchers, health systems, and health policy makers to allocate resources for targeted interventions to combat the epidemic of cardiometabolic and other noncommunicable diseases.
Limitations
Our results must be interpreted in the context of several important limitations. This was a cross‐sectional study, and therefore directionality and causality cannot be inferred. For instance, the probability of reverse association exists, that is, higher social vulnerability attributable to higher prevalence of comorbidities. In any epidemiologic study, there is a possibility of residual confounding. The SVI and health behaviors of populations residing in the respective states may be influenced by migration patterns and other unaccounted factors. The data pertaining to health conditions and health‐related behaviors from BRFSS is self‐reported and is susceptible to respondent bias. Finally, the SVI is calculated on a census tract level, and we have extrapolated these to state‐level data by using the composite US database, in which all tracts are ranked against one another, allowing for state‐level evaluation of SVI. Thus, our results cannot be used to inform county and census‐level inferences. Because of privacy concerns, BRFSS data are not available to us at the county level (ie, we have only state of residence available for each participant). Consequently, we merged BRFSS with state‐level SVI rankings to allow for a homogenous comparison of social vulnerability with prevalent cardiovascular comorbidities.
Conclusions
The SVI varies across the US states and is associated with cardiovascular comorbidities and atherosclerotic cardiovascular disease, independent of age, race and ethnicity, sex, employment, income, and health care coverage. The SVI may be a useful assessment tool for health policy makers, health systems, and researchers examining multilevel influences on health behaviors, and identifying and allocating resources to communities at risk of cardiovascular diseases attributable to social determinants of health.
Sources of Funding
This study received funding from makeadent.org and the Ram and Sanjita Kalra Aavishqaar Fund.
Disclosures
Dr Rodriguez was funded by a career development award from the National Heart, Lung, and Blood Institute (K01 HL 144607) and the American Heart Association/Robert Wood Johnson Harold Amos Medical Faculty Development Program. Dr Virani reported grants from the US Department of Veterans Affairs, World Heart Federation, Tahir, and Jooma Family Research Grant during the conduct of the study and other support from the American College of Cardiology Honorarium in his role as the associate editor for Innovations ACC.org outside the submitted work. No other disclosures were reported. The remaining authors have no conflicts of interests to declare.
Supporting information
Table S1
Figure S1
For Sources of Funding and Disclosures, see page 10.
References
- 1. Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Health and Economic Costs of Chronic Diseases|CDC . June 23, 2021. Available at: https://www.cdc.gov/chronicdisease/about/costs/index.htm. Accessed July 13, 2021.
- 3. Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11(3):238–245. doi: 10.2174/1573403x11666141122220003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Carnethon MR, Pu J, Howard G, Albert MA, Anderson CAM, Bertoni AG, Mujahid MS, Palaniappan L, Taylor HA Jr, Willis M, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136(21):e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 5. Flanagan BE, Hallisey EJ, Adams E, Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the Centers for Disease Control and Prevention's social vulnerability index. J Environ Health. 2018;80(10):34–36. [PMC free article] [PubMed] [Google Scholar]
- 6. Wallace LMK, Theou O, Pena F, Rockwood K, Andrew MK. Social vulnerability as a predictor of mortality and disability: cross‐country differences in the survey of health, aging, and retirement in Europe (SHARE). Aging Clin Exp Res. 2015;27(3):365–372. doi: 10.1007/s40520-014-0271-6 [DOI] [PubMed] [Google Scholar]
- 7. Armstrong JJ, Andrew MK, Mitnitski A, Launer LJ, White LR, Rockwood K. Social vulnerability and survival across levels of frailty in the Honolulu‐Asia aging study. Age Ageing. 2015;44(4):709–712. doi: 10.1093/ageing/afv016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nelson DE, Powell‐Griner E, Town M, Kovar MG. A comparison of National Estimates from the National Health Interview Survey and the behavioral risk factor surveillance system. Am J Public Health. 2003;93(8):1335–1341. doi: 10.2105/ajph.93.8.1335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li C, Balluz LS, Ford ES, Okoro CA, Zhao G, Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the behavioral risk factor surveillance system, the National Health Interview Survey, and the National Health and nutrition examination survey, 2007‐2008. Prev Med. 2012;54(6):381–387. doi: 10.1016/j.ypmed.2012.04.003 [DOI] [PubMed] [Google Scholar]
- 10. CDC/ATSDR's Social Vulnerability Index (SVI) . April 28, 2021. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. Accessed September 17, 2021.
- 11. Knighton AJ, Savitz L, Belnap T, Stephenson B, VanDerslice J. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. EGEMS (Wash DC). 2016;4(3):1238. doi: 10.13063/2327-9214.1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dégano IR, Marrugat J, Grau M, Salvador‐González B, Ramos R, Zamora A, Martí R, Elosua R. The association between education and cardiovascular disease incidence is mediated by hypertension, diabetes, and body mass index. Sci Rep. 2017;7:12370. doi: 10.1038/s41598-017-10775-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hanley GE, Morgan S, Reid RJ. Income‐related inequity in initiation of evidence‐based therapies among patients with acute myocardial infarction. J Gen Intern Med. 2011;26(11):1329–1335. doi: 10.1007/s11606-011-1799-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee S, Colditz G, Berkman L, Kawachi I. Caregiving to children and grandchildren and risk of coronary heart disease in women. Am J Public Health. 2003;93(11):1939–1944. doi: 10.2105/ajph.93.11.1939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leigh JA, Alvarez M, Rodriguez CJ. Ethnic minorities and coronary heart disease: an update and future directions. Curr Atheroscler Rep. 2016;18(2):9. doi: 10.1007/s11883-016-0559-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205 [DOI] [PubMed] [Google Scholar]
- 17. Social Deprivation Index (SDI) . Available at: https://www.graham‐center.org/rgc/maps‐data‐tools/sdi/social‐deprivation‐index.html. Accessed September 18, 2021.
- 18. Nguyen TN, Ngangue P, Bouhali T, Ryan BL, Stewart M, Fortin M. Social vulnerability in patients with multimorbidity: a cross‐sectional analysis. Int J Environ Res Public Health. 2019;16(7):1244. doi: 10.3390/ijerph16071244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gay JL, Robb SW, Benson KM, White A. Can the social vulnerability index be used for more than emergency preparedness? An examination using youth physical fitness data. J Phys Act Health. 2016;13(2):121–130. doi: 10.1123/jpah.2015-0042 [DOI] [PubMed] [Google Scholar]
- 20. Kucharska‐Newton AM, Harald K, Rosamond WD, Rose KM, Rea TD, Salomaa V. Socioeconomic indicators and the risk of acute coronary heart disease events: comparison of population‐based data from the United States and Finland. Ann Epidemiol. 2011;21(8):572–579. doi: 10.1016/j.annepidem.2011.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Machado S, Sumarsono A, Vaduganathan M. Midlife wealth mobility and long‐term cardiovascular health. JAMA Cardiol. 2021;1152–1160. doi: 10.1001/jamacardio.2021.2056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barber S, Hickson DA, Kawachi I, Subramanian SV, Earls F. Neighborhood disadvantage and cumulative biological risk among a socioeconomically diverse sample of African American adults: an examination in the Jackson heart study. J Racial Ethn Health Disparities. 2016;3(3):444–456. doi: 10.1007/s40615-015-0157-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Retail Stores in Poor Urban Neighborhoods ‐ ALWITT ‐ 1997 ‐ Journal of Consumer Affairs ‐ Wiley Online Library . Available at: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1745‐6606.1997.tb00830.x. Accessed July 24, 2021.
- 24. Giang T, Karpyn A, Laurison HB, Hillier A, Perry RD. Closing the grocery gap in underserved communities: the creation of the Pennsylvania fresh food financing initiative. J Public Health Manag Pract. 2008;14(3):272–279. doi: 10.1097/01.PHH.0000316486.57512.bf [DOI] [PubMed] [Google Scholar]
- 25. Yeates K, Lohfeld L, Sleeth J, Morales F, Rajkotia Y, Ogedegbe O. A global perspective on cardiovascular disease in vulnerable populations. Can J Cardiol. 2015;31(9):1081–1093. doi: 10.1016/j.cjca.2015.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Figure S1


