Abstract
Objective:
To perform a scoping review of the applicability of the Gail model in different countries for different ethnicities.
Methods:
The review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist and search strategies based on the PICOS approach. The reviewed articles were included if they were published between 2013 and 2018 in English, Portuguese, or Spanish; were original articles available in full online; and described the use of the Gail model. The PubMed, Embase, and Web of Science data bases were searched.
Results:
A total of 38 articles eligible for analysis were identified, of which 16 used the Gail model to assess breast cancer risk in women, eight analyzed the applicability of this tool in their population, seven compared the tool and/or modified it according to the specific risk factors of their population, and seven cited the model in determining eligibility for chemoprevention.
Conclusion:
The Gail model has different applicabilities Greater effectiveness and breast cancer risk are found in developed countries.
Key Words: Applicabilities, breast cancer, Gail model, scoping review
Introduction
The incidence of breast cancer is increasing in both developed and developing countries thanks to a rising life expectancy, urbanization, and changes in lifestyle (WHO, 2020). Breast cancer is the most common neoplasm in women worldwide, with an estimated incidence of 2,179,457 new cases and estimated 655,690 deaths in 2020 (GLOBOCAN, 2020). The most recent global estimate, for 2018, indicates that breast cancer is the second-most frequent type of cancer in the general population (2.1 million), second only to lung cancer (2.1 million) (Bray et al., 2014). The five countries with the highest rates of breast cancer for the same year were Belgium with 113.2 cases per 100,000 women, followed by Luxembourg with 109.3, the Netherlands with 105.9, France with 99.1, and New Caledonia (France) with 98.0 cases per 100,000 women (WCRF, 2018).
In Brazil, the number of deaths from breast cancer in 2017 was 16,724 (INCA, 2020). In the same year, 65,357 hospitalizations due to the disease were recorded, and in 2018, 41,192 hospitalizations occurred between January and August (Ministério da Saúde, 2018). The estimated number of new cases for 2020-2022 will be 66,000 cases per year; in Paraná, this estimate is 3,470 new cases (INCA, 2020).
The early diagnosis of breast cancer is important to reduce the mortality rate of this disease. However, in some low- and middle-income countries, due to the limited resources of the health systems, breast cancer diagnosis is most often made at more advanced stages, worsening the prognosis and decreasing patient survival (WCRF, 2018). Screening programs for early diagnosis based on women’s knowledge of breast cancer risk can be implemented in the primary-care setting using validated tools for calculating individual risk, which is a low-cost strategy that can be used in all countries, facilitating decision-making on prevention and screening for this disease.
The Gail model, created in 1989 by Cruzoé et al., (2015) is used worldwide to predict the risk of developing breast cancer in women within the next five years and over the lifetime. It is a valuable tool for assessing specific risks and selecting individual prevention strategies (Wang et al., 2018). It has been used in the selection of women for chemoprevention (Oseni et al., 2016; Wang et al., 2016). Although this model has worldwide validation, its applicability is questionable in some populations because it has significant limitations related to the absence of some risk factors in its formula.
Given this background, a scoping review was conducted to systematically map this research area and to answer the following research question: Does the Gail model have applicability in all countries and indifferent ethnicities?
Materials and Methods
This is a scoping review, a kind of review whose objective is to map the main concepts that support a particular area of knowledge; examine the extent, range, and nature of research; summarize and disseminate research data; and identify the existing research gaps (Arksey et al., 2005). This kind of review differs from Systematic Reviews because the authors do not usually assess the quality of included studies. They also differ from narrative or literature reviews, insofar as the scoping process requires analytical reinterpretation of the literature (Levac et al., 2010).
The methods of this review were based on the guidelines provided by The Joanna Briggs Institute (Peters et al., 2017), and the protocol was elaborated using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) found at www.equator-network.org/Library/reporting-guidelines-underdevelopment/#55 and www.prisma-statement.org/Extensions/InDevelopment.aspx.
To be included in the review, articles had to answer the guiding question: Does the Gail model have applicability in all countries and in different ethnicities? Peer-reviewed articles were included if they were published between 2013 and 2018; written in English, Portuguese, or Spanish; were original articles available in full online; and described the use of the Gail model. Quantitative, qualitative, and mixed-method studies were included to consider different aspects of model use.
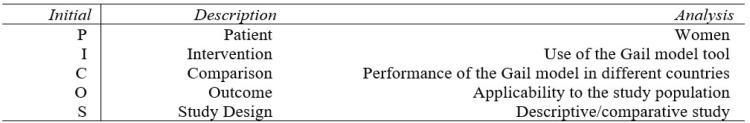
PubMed, Embase, and Web of Science (WOS) were searched with the MeSHterms/descriptors “Breast Neoplasm” and “Breast Cancer” as the main research axis and “Risk Assessment” and “Gail Model” as secondary descriptors. The search strategy was based on the PICOS tool (Figure 1), used in scientific evidence-based practice (Santos et al., 2007).
Figure 1.
Legend?
To reduce the risk of bias in the study, two pairs of researchers examined the 81 identified studies, which were homogeneously and randomly divided between the pairs. By reading the titles and abstracts, each pair discussed the results and selected potentially relevant studies. After this step, the pairs gathered the potential studies and distributed them in equal numbers between the pairs for full reading of the articles and extraction of data and relevant information for the review. The references of the articles selected for data extraction were also read to find any other articles that fit the study inclusion criteria.
The quality of the methodologies of the eligible articles were assessed using the Study Quality Assessment Tools (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools), the results are described in the complementary Table 1, complementary Table 2 and complementary Table 3 (Supplementary Material).
Table 1.
Comparisons of Risk Values for Breast Cancer between Cross-Sectional Studies
| Authors | Country | City | Risk ≥ 1.67% | Mean five-year risk | Minimum risk | Maximum risk | Sample size | Year of publication |
|---|---|---|---|---|---|---|---|---|
| Açikgöz and Ergör | Turkey | Izmir | 15.80% | n/a | n/a | n/a | 227 | 2013 |
| Fikree and Hamadeh | Bahrain | n/a | 4.00% | 0.7±0.37 | 0.2 | 2.4 | 172 | 2013 |
| Garza-Gangemi et al. | Mexico | Mexico city | n/a | 1.18 | n/a | n/a | 1000 | 2014 |
| Erbil et al. | Turkey | Ordu | 7.40% | 0.88±0.91 | 0.2 | 8 | 231 | 2015 |
| Mohammadbeigi et al. | Iran | Qom | n/a | 0.37±0.18 | 0.1 | 1.3 | 296 | 2015 |
| Baytchev et al. | Bulgaria | Sofia | 25.20% | 1.51 | 0.7 | 5.5 | 107 | 2015 |
| Khaliq, Jelovac and Wright | USA | Baltimore | 32.00% | 1.67±0.88 | n/a | n/a | 250 | 2016 |
| Khazaee-Pool et al. | Iran | Tehran | 9.36% | 1.61±0.73 | 0.2 | 13.8 | 3847 | 2016 |
| Mirghafourvand et al. | Iran | Tabriz | n/a | 0.6±0.2 | n/a | n/a | 560 | 2016 |
| Gonzáles, Molina and Reygadas | Mexico | Mexico city | 16.60% | n/a | n/a | n/a | 154 | 2016 |
| Ansari et al. | Iran | Zahedan | n/a | 0.36±0.21 | n/a | n/a | 260 | 2016 |
| Al Otaibi | Saudi Arabia | n/a | 6.70% | 0.87±0.93 | n/a | n/a | 180 | 2017 |
| Ewaid and Al-Azzawi | Iraq | Baghdad | 7.60% | 0.952±1.4 | 0.3 | 7.10% | 250 | 2017 |
| Farahmand et al. | Iran | n/a | n/a | 0.85 | n/a | n/a | 416 | 2017 |
| Bener et al. | Qatar | n/a | n/a | 1.12±0.52 | n/a | n/a | 1338 | 2017 |
| Gama et al. | Brazil | Paranavaí | 13.10% | 1.18±2.63 | 0.2 | 50 | 374 | 2017 |
n/a, data not reported in the study
Table 2.
Comparison of the Applicability of the Gail Model in Different Countries and Populations
| Authors | City/Country | Gail Model Applicability | Sample Size | Publication Year |
|---|---|---|---|---|
| Challa et al. | India | No | 104 | 2013 |
| Lopes et al. | Alfenas, Brazil | No | 105 | 2014 |
| Garza-Gangemi et al. | Mexico City, Mexico | Yes | 1000 | 2014 |
| Thomas et al. | New Delhi, India | No | 222 | 2014 |
| Omranipour et al. | Tehran, Iran | No | 280 | 2015 |
| Clavelle et al. | United States | Yes | 423 | 2015 |
| Crusoé et al. | Salvador, Brazil | No | 64/64 | 2015 |
| Farahmand et al. | Tehran, Iran | No | 416 | 2017 |
The data extraction table was filled out jointly by two reviewers with the main variables to be extracted. These data were mapped independently, their results were discussed, and they were updated continuously in the data collection form in an interactive process. Studies were grouped by the way they used the Gail model tool, to facilitate the analysis and discussion of the results found.
Results
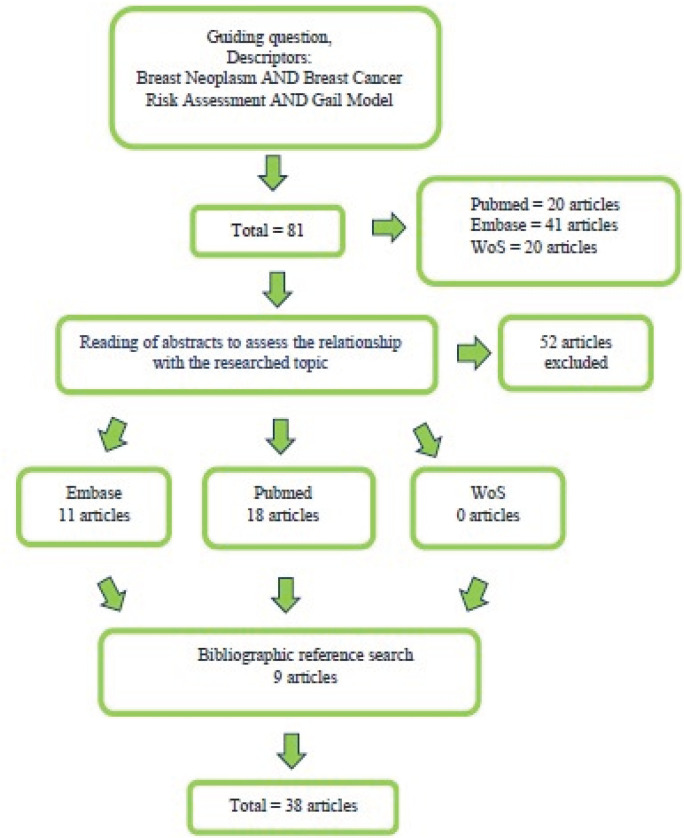
A total of 81 articles were identified, 20 in PubMed, 41 in Embase, and 20 in WOS. Of the total, 52 articles were excluded because they did not meet the inclusion criteria (PICOS), and29 articles remained. Nine other studies that had a direct relationship with this scoping review were included after being identified in their references. Thus, 38 articles were analyzed and included in this review (Figure 2).
Figure 2.
Legend?
When carrying out the quality assessment of eligible articles, according to the Quality Assessment Tool according to the criteria for observational cohort studies and cross-sectional studies, 25 were classified as good and 2 as fair. From the evaluation of the case-control studies, all 3 were classified as good. And, the evaluation of the Controlled Intervention Study, the only eligible article was rated as good (Supplementary Material).
In the different populations evaluated, it was observed that the cities of Baltimore, USA (Khaliq et al., 2016); Sofia, Bulgaria (Baytchev et al., 2015); Mexico City, Mexico (González et al., 2018); Izmir, Turkey (Açikogoz et al., 2013) and Paranavaí, Brazil (Gama et al., 2018), showed the highest proportion of women at high risk (≥ 1.67%) of developing breast cancer. In these populations, the risk of developing breast cancer within the next five years ranged from 1.18% (Paranavaí, Brazil) to 1.67% (Baltimore, USA). The lowest risks of developing breast cancer within the next five years were observed in Zahedan (Ansari et al., 2018) and in Qom (Mohammadbeigi et al., 2015), Iran (Table 1).
Some studies have evaluated the applicability of the Gail model in specific populations (Table 3). In Brazil, the study by Lopes et al. (2014) underestimated the risk of breast cancer, as only 51 (48.57%) of the women who already had breast cancer were identified as high-risk. The same result was found in another Brazilian study conducted by Crusoé et al., (2015), in which a case–control design was used and the mean five-year Gail risk score was higher in the control group than the case group.
In India, the studies conducted by Challa et al., (2013), and Thomas et al., (2016), both case–control, underestimated the risk within five years of developing breast cancer. The same occurred in Iran in the studies by Omranipour et al., (2015) and Farahmand et al., (2017), which underestimated the risk in women with the disease and found no significant between-group difference in the risk factors evaluated by the model (Table 2).
In contrast, in Mexico, a cohort study conducted by Garza-Gangemi et al., (2014) validated the tool, demonstrating that the percentage of women assessed as high risk within up to five years was in agreement with the total number of women diagnosed with breast cancer in the period. A similar result was found in a study conducted by Clavelle et al., (2015) in the United States on a population of homosexual and heterosexual women, as a high risk was found for this population, making the model viable to be routinely used in the clinical setting (Table 2).
In some countries, the Gail model was not considered a good predictor for the calculation of breast cancer risk. Thus, some studies have suggested modifying the model for the specific population to improve its effectiveness, as shown in Box 1.
The study conducted by Ansari et al., (2018) in 260 Iranian women evaluated socioeconomic and reproductive factors, correlating them with the estimated risk of breast cancer using the Gail model. Based on the statistical analysis, the authors concluded that to improve breast cancer screening using the Gail model, the model should be modified for women in southeastern Iran by including known risk factors such as ethnicity, body mass index (BMI), breastfeeding duration, and history of divorce.
However, the study by Rosner et al., (2013), in California, used the Gail model as a parameter in the formulation and validation of another tool, named the Rosner-Colditz model. To fit this model, they used a set of independent prospective data on the incidence of breast cancer, considering future use of hormones based on the type and previous duration of use and other covariates and evaluated the model’s performance using the area under the curve (AUC) and calibration methods. The Rosner-Colditz model showed a stronger performance in predicting the incidence of breast cancer over a five-year time interval, and the AUC values exceeded those of the Gail model by 3-5%, making it more applicable in the local population. Nevertheless, the authors suggested improving the Gail model by adding breast density and other risk markers to those contained in the current model.
The same was observed in Korea in the study conducted by Park et al., (2013) in a set of 3,789 cases and controls, where they evaluated the performance of the Gail model in the population and developed a breast cancer risk assessment tool (KoBCRAT) based on equations developed for the Gail model for predicting the risk of breast cancer from the identification of risk factors among Korean women. The study validated the KoBCRAT based on the expected/observed incidence of breast cancer and the AUC. The Gail model calculated a higher five-year risk for the control group (p = 0.017), while KoBCRAT calculated a higher five-year risk in the case group (p <0.001). Thus, the study concluded that KoBCRAT is a better tool to predict the risk of breast cancer in Korean women compared to the Gail model.
A similar study was conducted in Spanish women by Pastor-Barriso et al., (2013), which recalibrated the Gail model for the lower incidences of breast cancer and risk factors in the studied cohort. The result obtained with the recalibration was generally positive, sore calibration seemed to provide unbiased estimates of absolute risk in that population, although the authors highlighted the need to develop extended models with additional strong risk factors.
The Gail model was also evaluated in China in a study by Zhao et al., (2017), who compared it with the health risk assessment (HRA) model. A total of 3,030 Chinese women were followed up, and the Gail model had a lower specificity than the HRA model, and the sensitivity of the Gail model was greater than that of the HRA model. The AUC and Youden index of the HRA model were more reliable than those of the Gail model. Based on this information, the study concluded that the HRA model is more appropriate for Chinese women than the classic risk assessment tool, the Gail model.
Another comparative study of the Gail model was performed by Shieh et al., (2018), who compared the risk estimates generated by the Breast Cancer Risk Assessment Tool (BCRAT) based on the Gail model, the Breast Cancer Surveillance Consortium model, and the Breast Cancer Surveillance Consortium model modified by the Polygenic Risk Score (BCSC-PRS) in a sample of 2,060 participants. The BCSC-PRS model categorized women below the low-risk threshold and above the moderately high-risk threshold compared to the other two models. Thus, the study suggests that the incorporation of genetic variants in clinical model validation is feasible and could improve risk prediction. Although it was comparative, the study did not report the use of the Gail model as a validated tool in this, population but suggested that changes in variable inclusion could improve its applicability.
In a study conducted in Brazil, Clementino et al., (2013) compared the Gail model with the Claus, BRCAPRO, and BOADICEA models in estimating the risk of breast cancer and the probability of risk conferred by the BRCA 1/2 mutation, correlating the values found in the different models. From on the analyzed data, the study showed that, although based mainly on hormonal and reproductive factors, the risk values estimated by the Gail model over five years were very similar (p <0.05) to the Claus, BRCAPRO, and BOADICEA model values, which estimate the risk based only on family history and age at diagnosis of the affected family members. The study concluded that the risk assessment models for breast cancer and for mutations showed good agreement in their predicted values, but it was recommended to include other risk factors in order to increase the accuracy of these models, given that in Brazil, the adaptation and validation of risk models for breast cancer are necessary.
The Gail model has been used to determine the clinical indication of chemoprevention based on the eligibility of women according to their breast cancer risk (Pruthy et al., 2015; Reimers et al., 2015; Vanegas et al., 2018; Green et al., 2014; Oseni et al., 2016). In turn, Pederson et al. (2018) compared the use of the Gail model and the Tyrer-Cuzick model to determine the risk of breast cancer and the implications for chemoprevention. The analysis showed that the Gail model is limited and should be applied cautiouslyto risk assessment or to counseling on the benefit of chemoprevention because it underestimated the risk in minority populations. The study concluded that dual modeling may be clinically useful in the formulation of chemopreventive recommendations.
Discussion
The Gail model is a validated tool worldwide. However, its applicability in different ethnicities is questionable because it shows significant differences in the risks calculated in different countries. As a consequence, this tool is increasingly being studied to determine its real applicability in breast cancer screening, and it has been modified in some countries through the inclusion of risk factors specific to the resident population.
In this scoping review, we identified 16 studies that addressed the application of the Gail model in specific populations to evaluate the five-year risk of developing breast cancer. As we have seen, high risk was found in developed countries and/or cities with a high development index, as in the studies by (Khaliq et al., 2016) conducted in Baltimore, USA, and by Bener et al. (2017) in Qatar, both countries with high economic development, a factor that influences the population’s lifestyle.
Among the risk factors for breast cancer, lifestyle (alcohol consumption, smoking, sedentarism, poor diet, obesity, and stress) is an important factor in the development of the disease and encompasses situations that are related to the economic condition of the population, as shown in the study by Yang (2017). That study concluded that economic and social development moderate the important influences of income and sex, where women drink more often in communities with greater economic development. Obesity was also associated with economic development in the study by Satman et al., (2013), where the lifestyle of industrialized countries –increased consumption of processed foods with high sugar and fat content and a more sedentary lifestyle with less activity and physical exercise – promote weight gain. The same was observed by Iseri et al., (2009), who found a higher percentage of obesity in women, also associated with lifestyle. A systematic review showed that a low prevalence of obesity was recorded in low-income countries, while a high prevalence was recorded in middle- and high-income countries (Dinsa et al., 2012).
We identified eight studies that evaluated the applicability of the Gail model in different populations. We observed that the model was not applicable to the entire population worldwide, given that different countries have ethnicities with specific characteristics. The studies that showed a positive applicability of the tool were those by Garza-Gangemi et al., (2014) and Clavelle et al., (2015), in Mexico and the United States, respectively. The countries where the model was found to be applicable were the same ones that had a high five-year average risk.
Given the above, seven studies included in our review discussed modifying the Gail model and/or created a new tool to calculate the risk of developing breast cancer based on risk factors specific to their populations (Ansari et al., 2018; Rosner et al., 2013; Park et al., 2013; Pastor-Barriuso et al., 2013; Zhao et al., 2017; Shieh et al., 2018; Clementino et al., 2013). These studies clearly support the importance of knowing the risk factors of each ethnicity and of having an effective and applicable risk calculation tool to improve the effectiveness of breast cancer screening and early detection, which are needed for a better prognosis.
Although the Gail model is discussed regarding its real-world applicability, our findings indicate a lack of studies on this topic. Some of the reviewed studies showed that certain countries still use the tool in clinical settings to determine the eligibility of women for chemoprevention, namely, Pruthi et al., (2015), Reimers et al., (2015), Vanegas et al., (2018), Green et al., (2014), and Oseni et al., (2016). Despite the limitations of the Gail model in some populations due to local risk factors, this tool is indicated by the United States Preventive Services Task Force to determine the eligibility of women for chemoprevention.
In conclusion, the Gail model has different applicabilities for developed and developing countries, being more effective in developed countries. This difference may be related to an unhealthy lifestyle with a consequent increase in risk factors such as obesity, sedentarism, stress, smoking, and alcohol consumption. For developing countries, the Gail model should be improved by including more risk factors specific to each studied population, so that the risk information obtained will be more consistent, thus allowing interventions for women classified as high-risk in order to reduce the morbidity and mortality rates of this disease.
Acknowledgements
This work was carried out with the support of the Coordination for the Improvement of Higher Education Personnel Brazil (CAPES).
References
- Açikogoz A, Ergor G. Compliance with screening recommendations according to breast cancer risk levels in Izmir, Turkey. Asian Pacific J Cancer Prev. 2013;14:1737–42. doi: 10.7314/apjcp.2013.14.3.1737. [DOI] [PubMed] [Google Scholar]
- Al-Otaibi Breast cancer risk assessment using the Gail model and it’s predictors in Saudi women. Asian Pac J Cancer Prev. 2017;18:2971–5. doi: 10.22034/APJCP.2017.18.11.2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ansari H, Mohammadi M, Mohammadi Y, et al. Assessment of socio-economic and menstrual-reproductive factors related to estimated risk of affecting to breast cancer in the Iranian women. Koomesh J Semnan Univ Med Sci. 2018;20:439–46. [Google Scholar]
- Arksey H, O´Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Meth. 2005;8:19–32. [Google Scholar]
- Baytchev G, Inkov I, Kyunchukov N, Zlateva E. Breast cancer risk evaluation – A correlation between mammographic density and the Gail Model. Int J Surg Med. 2015;1:18–21. [Google Scholar]
- Bener A, Çatan F, El Ayoubi HR, Acar A, Ibrahim WH. Assessing breast cancer risk estimates based on the Gail model and its predictors in Qatari women. J Primary Care Commun Health. 2017;8:180–7. doi: 10.1177/2150131917696941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray F, Cueva P, Korir A, et al. Planning and developing populations-base cancer registration in low-and middle-income settings. Lyon, France: International Agency for Research on Cancer; 2014. [PubMed] [Google Scholar]
- Challa VR, Swamyvelu K, Shetty N. Assessment of the clinical utility of the Gail model in estimating the risk of breast cancer in women from the Indian population. Ecancermedicalscience. 2013;7:363. doi: 10.3332/ecancer.2013.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clavelle K, King D, Bazzi AR, Fein-Zachary V, Potter J. Breast cancer risk in sexual minority Women during Routine Screening at an Urban LGBT Health Center. Womens Health Issues. 2015;25:341–8. doi: 10.1016/j.whi.2015.03.014. [DOI] [PubMed] [Google Scholar]
- Clementino LS, Suzuki EH, Oliveira KB. Risk assessment for breast cancer and BRCA mutations in women with personal and familial history. Acta Scientiarum Health Sciences Maringá. 2013;35:263–71. [Google Scholar]
- Cruzoé NSDR, Pinheiro AB, Oliveira JF, et al. Avaliação da aplicabilidade do Modelo de Gail como preditor de risco de cancer de mama em mulheres. Baianas Rev Bras Mastologia. 2015:25. [Google Scholar]
- Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev. 2012;13:1067–79. doi: 10.1111/j.1467-789X.2012.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbil N, Dundar N, Inan C, Bolukbas N. Breast cancer risk assessment using the Gail model: a Turkish study. Asian Pac J Cancer Prev. 2015:16. doi: 10.7314/apjcp.2015.16.1.303. [DOI] [PubMed] [Google Scholar]
- Ewaid SH, Al-Azzawi LHA. Breast cancer risk assessment by Gail model in women of Baghdad. Alexandria J Med. 2017;53:183–6. [Google Scholar]
- Farahmand L, Shojamoradi MH, Najafi M, Majidzadeh-AK The applicability of the Gail model in Iranian population. Multidisciplinary Cancer Invest. 2017:1. [Google Scholar]
- Fikree M, Hamadeh RR. Breast cancer risk assessment among Bahraini women. Baharain Med Bull. 2013;2013:35. [Google Scholar]
- González EZG, Molina JAA, Reygadas AM. Using the Gail model to identify women at hight risk for developing breast cancer – México. Aten Fam. 2018;25:114–7. [Google Scholar]
- Green LE, Dinh TA, Hinds DA. Economic evaluation of using a genetic test to direct breast cancer chemoprevention in white women with a previous breast biopsy. Appl Health Econo Health Policy. 2014;12:203–17. doi: 10.1007/s40258-014-0089-6. [DOI] [PubMed] [Google Scholar]
- Iseri A, Arslan N. Obesity in adults in Turkey: age and regional effects. Eur J Public Health. 2009;19:91–4. doi: 10.1093/eurpub/ckn107. [DOI] [PubMed] [Google Scholar]
- Khazaee-Pool M, Majlessi F, Nedjat S, et al. Assessing breast cancer risk among Iranian women using the Gail model. Asian Pac J Cancer Prev. 2016;17:3759–62. [PubMed] [Google Scholar]
- Khaliq W, Jelovac D, Wright SC. Prevalence of chemopreventive agente use among hospitalized women at high risk for breast cancer: a cross-sectional study. BMJ Open. 2016;6:e012550. doi: 10.1136/bmjopen-2016-012550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levac D, Colquhoun H, O’Brien KK. Scoping studies: Advancing the methodology. Implement Sci. 2020;5:1–9. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes FC, Franco TLB, Gradim CVC. Mensuração dos fatores de risco de mulheres com câncer mamário através do índice de Gail. J Nurs. 2014;2014:8. [Google Scholar]
- Mirghafourvand M, Charandabi SMA, Ahmadpour P, Rahi P. Breast cancer risk based on the Gail model and its predictors in Iranian women. Asian Pac J Cancer Prev. 2016;17:3741–5. [PubMed] [Google Scholar]
- Mohammadbeigi A, Mohammadsalehi N, Valizadeh R, et al. Lifetime and 5 years risk of breast cancer and attributable risk factor according to Gail model in Iranian women. J Pharm Bioallied Sci. 2015;7:2007–11. doi: 10.4103/0975-7406.160020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omranipour R, Karbakhsh M, Behforouz A, et al. Performance of the Gail model for breast cancer risk assessment in Iranian women. Arch Breast Cancer. 2015;2:27–31. [Google Scholar]
- Oseni T, Perkins S, Deutsch E, Soballe P. The use of chemoprevention increases significantly with oncology trained providers and with application of a risk assessment model. Cancer Res. 2016 Doi: 10.1158/1538-7445.SABCS15-P3-08-05. [Google Scholar]
- Park B, Ma SH, Shin A, et al. Korean risk assessment model for breast cancer risk prediction. PLoS One. 2013;8:e76736. doi: 10.1371/journal.pone.0076736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastor-Barriuso R, Ascunce N, Ederra M, Erdoza´inN , Murilo A, Martínez JEA, et al. Recalibration of the Gail model for predicting invasive breast cancer risk in Spanish women: a population-based cohort study. Breast Cancer Res Treat. 138:249–59. doi: 10.1007/s10549-013-2428-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruthi S, Heisey RE, Beyers TB. Chemoprevention for breast cancer. Ann Surg Oncol. 2015;22:3230–5. doi: 10.1245/s10434-015-4715-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimers LL, Sivasubramanian PS, Hershman D, et al. Breast cancer chemoprevention among high-risk women and those whit ductal carcinoma in situ. Breast J. 2015;21:377–86. doi: 10.1111/tbj.12418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosner BA, Colditz GA, Hankinson SE, et al. Validation of Rosner-Colditz breast cancer incidence model using an independent data set, the California Teachers Study. Breast Cancer Res Treat. 2013;142:187–202. doi: 10.1007/s10549-013-2719-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos CMC, Pimenta CADM, Nobre MEC. The PICO strategy for the research question construction and evidence search. Rev Latino-am de Enfermagem. 2007;15:508–11. doi: 10.1590/s0104-11692007000300023. [DOI] [PubMed] [Google Scholar]
- Satman I, Omer B, Tutuncu Y, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28:169–80. doi: 10.1007/s10654-013-9771-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shieh Y, Ziv E, Eklund M. Combining genetic variants and clinical risk factors for breast cancer risk stratification in a population-based trial. J General Int Med. 2018;33:143–4. [Google Scholar]
- Thomas S, Desai G, Pathania OP, et al. Clinico-epidemiological profile of breast cancer patients and the retrospective application of Gail model 2: Na Indian perspective. Breast Dis. 2016;36:15–22. doi: 10.3233/BD-150203. [DOI] [PubMed] [Google Scholar]
- Vanegas A, Vargas JM, Kukafka R, Crew KD. Randomized controlled trial of web-based decision support tools for high-risk women and primary care providers to increase breast cancer chemoprevention. Cancer Res Ongoing Clinical Trials. 2018 doi: 10.1016/j.conctc.2019.100433. DOI: 10.1158/1538-7445.SABCS17-OT3-01-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H, Snyder CF, Larson S, et al. Breast cancer chemoprevention in primary care-assessing readiness for change. Qual Primare Care. 2016;24:283–8. [Google Scholar]
- Wang X, Huang Y, Li L, et al. Assessment of performance of the Gail model for predicting breast cancer risk: a systematic review and meta-analysis with trial sequential analysis. Breast Cancer Res. 2018;20:18. doi: 10.1186/s13058-018-0947-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang XY. How Community-level social and economic developments have changed the patterns of substance use in a transition economy? Health Place. 2017;46:91–100. doi: 10.1016/j.healthplace.2017.05.009. [DOI] [PubMed] [Google Scholar]
- Zhao J, Song X, Leng L. Evaluation of risk assessment tools for breast cancer screening in Chinese population. Int J Clin Exp Med. 2017;10:3582–7. [Google Scholar]