Abstract
Objective:
To compare the distress level among Brazilian healthcare professionals during the coronavirus disease 2019 (COVID-19) pandemic and estimate risks by sex, age, and occupation.
Methods:
In a longitudinal cohort design, a nationally distributed online survey was used to collect data from 10,490 active healthcare professionals who worked during the pandemic. Participants were mostly female, aged 18 to 82 years; 13 different health professions and all states of Brazil were represented.
Results:
The most frequent professions were psychology, dentistry, and nursing. The Brief Symptom Inventory (BSI) score suggested an increased distress perception among health professionals. Females showed poorer mental health than males, but the absolute rise in Global Severity Index (GSI) score was larger in males than in females. Younger adults reported more symptoms of psychological distress than older adults. The most impacted age group was between 30-39 years. Nurse technicians presented the highest risk of distress.
Conclusion:
Health professionals are essential to overcoming the pandemic; thus, their mental health status should be monitored, and features associated with increased distress should be identified. Our findings suggest distress risk should be stratified by occupation, age, and sex. Health professionals showed an increased distress perception. Women, individuals between the ages of 30 and 39, nursing personnel, and physicians were more likely to report distress compared with other health professionals.
Keywords: COVID-19, mental health, health workers, pandemics, mental distress
Introduction
Eighteen months since its declaration, the coronavirus disease (COVID-19) pandemic remains an ongoing challenge for countries worldwide, from its social and economic impacts to the availability of enough healthcare facilities to provide adequate care. Healthcare professionals have been essential to overcoming the effects of the pandemic, but have also been exposed to a higher risk of its deleterious impacts, including on their health, financial stability, and family relationships.1 They commonly work long hours, under risk of becoming infected and spreading the virus to their loved ones.2,3 They often face difficult choices while overburdened by the demands of the health care system. The high-stress conditions health personnel have faced since the emergence of the COVID-19 pandemic is undeniable.
Psychological distress is perceived as a persistent feeling of emotional suffering, overwhelm, and vulnerability, as occurs in socially disruptive conditions that promote overload.4 Previous longitudinal studies, such as one conducted in the general population in England, found that psychological distress increased 5% from 2018-2019 to April 2020, a greater increase than expected for that timeframe.5 The authors observed persistent elevated distress reported at the 3-month follow-up, co-occurring with an increase in mental health problems.6 In undergraduate medical students, there was an increase in perceived stress and anxiety levels, apparently related to the pandemic.7 Some studies reported higher stress, fear, anxiety, and depression among healthcare professionals, mostly in cross-sectional designs.8-10 In a study conducted in China, being a nurse, female, working in a hotspot or on the frontline were considered risk factors for mental health symptoms in health professionals.8-10 In addition, the burden on the mental health of professionals could be compounded by the global consequences of the pandemic, which include economic, environmental, and social problems that challenge healthcare systems around the world.11,12 Another factor is the mass media coverage, which could support efforts to control the pandemic or generate more pressure on the mental health of individuals if not based on accurate, reliable information that helps prevent COVID-19 spread.13
In the present study, we measured distress and its demographic features at two timepoints, 6 months apart, during the COVID-19 pandemic. Our aim was to observe and compare distress among Brazilian healthcare occupations and to estimate the associated risk effects of sex, age, and occupation.
Methods
Participants
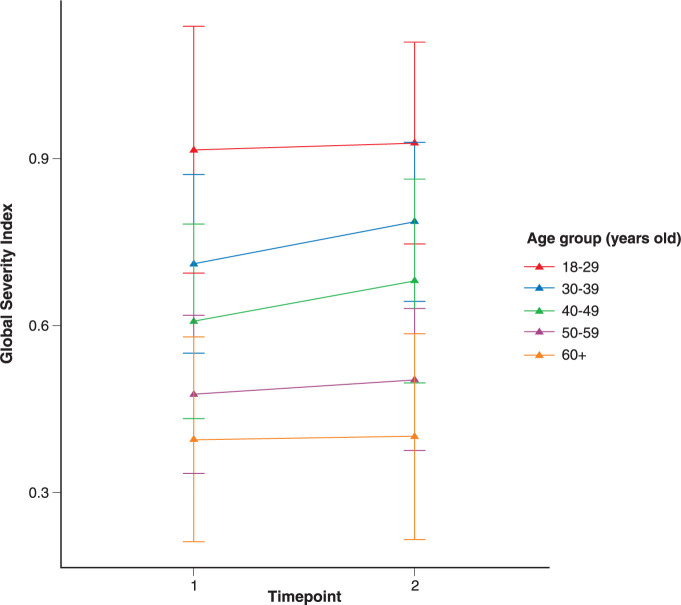
The sample consisted of 10,490 people who answered the survey questionnaire in the first and second timepoints of the longitudinal study and agreed to being followed. The inclusion criteria included working in a healthcare occupation (self-reported). Participants were mostly female (81.1%) and with ages ranging from 18 to 82 years (mean [M] = 37.8; standard deviation [SD] = 10.3); all states of the federation were represented, but the Southeast region of Brazil predominated (52%). The most common health professions were psychology (11.1%), dentistry (9.8%), and nursing (9.5%), among those who responded to the two waves of the survey. Around one-third of the professionals reported fearing the disease at work (30.5% at timepoint 1 and 33.8% at timepoint 2). About 14.2% reported that their families or friends were infected by COVID-19 at the first timepoint, a rate which rose to 35.7% at the second timepoint. About half of the respondents feared spreading the disease to their families or friends (42.5% at timepoint 1 and 50.8% at timepoint 2). Demographics are shown in Figure 1 and Table 1.
Figure 1. Geographical distribution of participants.
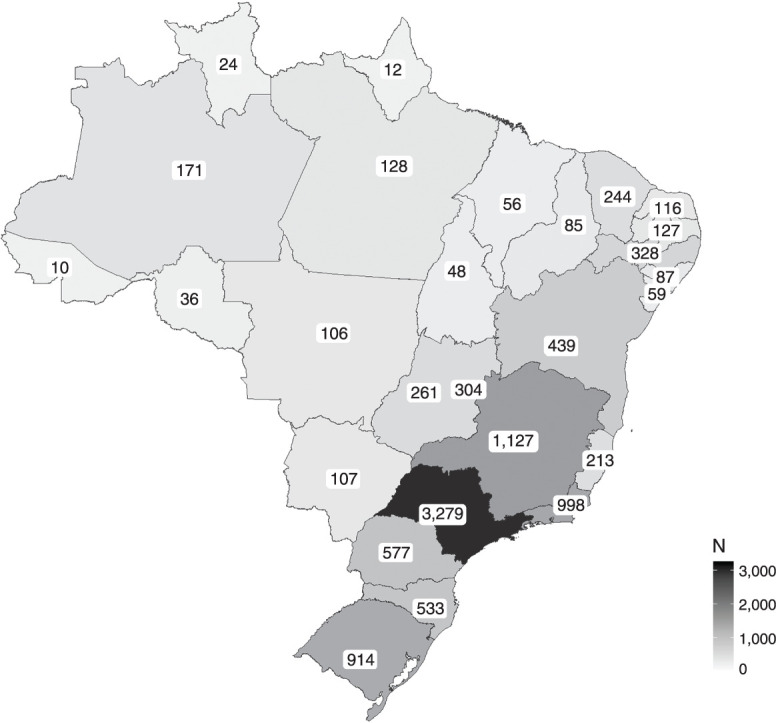
Table 1. Demographics characteristics of the sample (n = 10,490).
| Characteristics | |
|---|---|
| Sex | |
| Female | 8,464 (81.0) |
| Male | 1,975 (19.0) |
| Missing | 51 |
| Age (mean [SD]) | 37.82 (10.33) |
| Missing | 227 |
| Age groups (years old) | |
| 18-29 | 2,536 (25.0) |
| 30-39 | 3,779 (37.0) |
| 40-49 | 2,369 (23.0) |
| 50-59 | 1,271 (12.0) |
| ≥ 60 | 308 (3.0) |
| Missing | 227 |
| Brazilian state | |
| Acre | 10 (< 0.1) |
| Alagoas | 87 (0.8) |
| Amapá | 12 (0.1) |
| Amazonas | 171 (1.6) |
| Bahia | 439 (4.2) |
| Ceará | 244 (2.3) |
| Distrito Federal | 304 (2.9) |
| Espírito Santo | 213 (2.1) |
| Goiás | 261 (2.5) |
| Maranhão | 56 (0.5) |
| Mato Grosso | 106 (1.0) |
| Mato Grosso do Sul | 107 (1.0) |
| Minas Gerais | 1,127 (11.0) |
| Paraná | 577 (5.6) |
| Paraíba | 127 (1.2) |
| Pará | 128 (1.2) |
| Pernambuco | 328 (3.2) |
| Piauí | 85 (0.8) |
| Rio Grande do Norte | 116 (1.1) |
| Rio Grande do Sul | 914 (8.8) |
| Rio de Janeiro | 998 (9.6) |
| Rondônia | 36 (0.3) |
| Roraima | 24 (0.2) |
| Santa Catarina | 533 (5.1) |
| Sergipe | 59 (0.6) |
| São Paulo | 3,279 (32) |
| Tocantins | 48 (0.5) |
| Missing | 101 |
| Occupation | |
| Psychologist | 1,163 (11.1) |
| Dentist | 1,030 (9.8) |
| Nurse | 998 (9.5) |
| Pharmacist/biochemist | 908 (8.7) |
| Physiotherapist | 877 (8.4) |
| Biologist/biomedical scientist | 645 (6.1) |
| Nurse technician | 629 (6.0) |
| Veterinarian | 595 (5.7) |
| Physical educator | 574 (5.5) |
| Dietitian | 537 (5.1) |
| Physician | 440 (4.2) |
| Speech therapist | 354 (3.4) |
| Social worker | 343 (3.3) |
| Health student | 18 (0.2) |
| Others | 1,379 (13.1) |
Data presented as n (%), unless otherwise specified.
Study design
Potential participants were contacted via the Brazilian Ministry of Health by e-mail, and were invited to a voluntary open survey that would take about 25 minutes to be completed. The form was composed of 13 pages, with each page containing one scale; the content and order of these were the same for all participants. Each wave of the survey delivered a cookie to the respondent’s device to facilitate identification of previous responses. The study was publicized online via social media and on the websites of supporting institutions. All participants were directed to the consent form and, after its acceptance, were invited to fill out an anonymous, comprehensive online questionnaire that covers several aspects of individual physical and mental health, behaviors, and consequences of the COVID-19 pandemic. Data collection took place respectively between May-June 2020 (timepoint 1) and December 2020-February 2021 (timepoint 2). At timepoint 1, 223,867 individuals accessed the form, but only 205,591 filled the items about distress. At timepoint 2, 60,448 individuals accessed the form, but only 58,218 filled the items about distress. This corresponds to a 73% attrition rate from the first to the second wave. The data presented herein refer only to those individuals who completed the online questionnaire at both timepoints, which corresponds to 10,490 individuals.
Instruments
The Brief Symptom Inventory (BSI)14 is a 53-item self-report inventory designed to assess psychological distress and psychopathological symptoms across nine dimensions (somatization, obsessive-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) and a Global Severity Index (GSI), which represents the sum of all items. It can be used to assess clinical populations and the general population, with a minimum age of 13 years. The items are rated on a five-point Likert scale (0-4), ranging from “not at all” to “extremely”. The internal structure has been verified for the Brazilian population.15 A bifactor structure was replicated in Brazil and was supported by data. The study suggests that only the GSI was sufficient to explain individual variability. The reliability of the general factor GSI was ωh = 0.98. Normative parameters of the instrument for the Brazilian population were established amid the COVID-19 pandemic.16
Statistical analysis
The population was divided into five age groups (18-29, 30-39, 40-49, 50-59, and 60 years or older) and 22 health occupations were compared. The Wilcoxon signed rank test for paired samples and repeated-measures analysis of variance were used to compare GSI/BSI score means for the overall health professionals and for groups considering sex, age group, and occupation. Post-hoc analysis using Scheffé-corrected p-values was used because it is more appropriate for exploratory hypotheses, for unbalanced data, and is more sensitive to type I error than other methods.17 The analyses were conducted in Jamovi v1.6 software (The Jamovi Project, 2021 version 1.6 – http://www.jamovi.org). A longitudinal Poisson regression was performed to check the rate of the slopes through two timepoints, controlling by age group, sex, occupation, and baseline score. The variables were coded for entry into the model as follows: occupation was transformed to dummy variables, sex used “male” as the reference category, and age groups used 18-to-29 as the reference category. Analyses were performed with the lme418 and jtools19 packages of R v. 4.1.0 software (R Core Team, 2021. https://www.R-project.org/).
Effect sizes were calculated through rank biserial correlations (rc) and partial eta-squared (η2p); interpretation of the magnitudes followed the guidelines proposed by Cohen et al.20,21 For the correlation effect sizes, thresholds are trivial (rc < 0.1), small (rc = 0.1 to 0.3), medium (rc = 0.3 to 0.5), and large (rc > 0.5), and for the partial eta-squared, they are trivial (η2p < 0.01), small (η2p = 0.01 to 0.06), medium (η2p = 0.06 to 0.14), and large (η2p > 0.14).
Ethics statement
The single-cohort longitudinal design of this study was evaluated and approved by the Brazilian National Commission on Research Ethics (Comissão Nacional de Ética em Pesquisa, CONEP) on May 2, 2020 (CAAE 30823620.6.0000.5149). The study complied with the Declaration of Helsinki (1989).
Results
The overall evolution of mental health of the healthcare professionals was verified by comparing both timepoints. The median GSI showed a significant increase for the population of health professionals (Wilcoxon signed rank test, p < 0.001), with a large effect size. The mean differences for GSI in each state are shown in Figure 2. Positive values denote an increase in mean score, and negative values, a decrease.
Figure 2. Difference in Global Severity Index (GSI) means by Brazilian state.
Similarly, the evolution of the score was evaluated for the health professionals, controlling by sex group. No interaction effects were significant (F[1] = 2.18, p = 0.140), while the effects within subjects were significant (F[1] = 72.62, p < 0.001, η2p = 0.007), but with a trivial effect size. The difference between sex groups are also significant (F[1] = 246, p < 0.001, η2p = 0.023), and a small effect size was found. A Wilcoxon paired test comparing both groups confirmed the difference (W = 2.31e+7, p < 0.001, rc = -0.097). At both timepoints, females had worse mean GSI scores than males. However, the absolute rise in scores was higher for males than for females (Δmales = 0.067; Δfemales = 0.047).
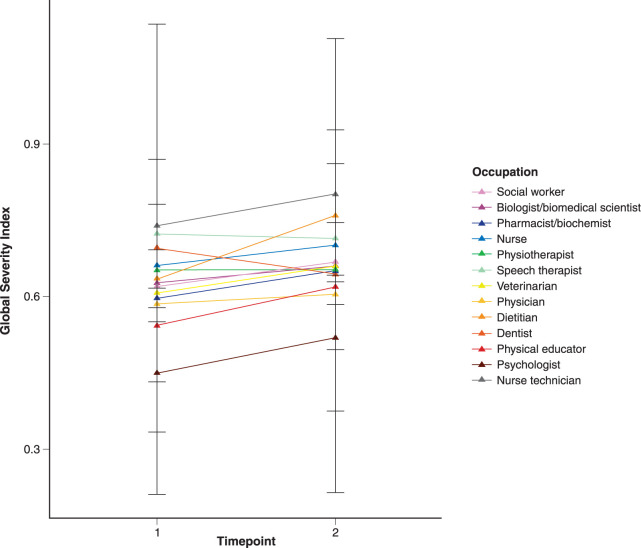
Next, we compared the five age groups at both timepoints. Within- and between-subjects effects were statistically significant, including the interaction between the two timepoints and age groups (F[4] = 2.81, p < 0.024, η2p = 0.001), with a trivial effect size. The difference in means within the two timepoints was also statistically significant (F[1] = 28.32, p < 0.001, η2p = 0.003), with a trivial effect size. The difference between age groups also showed significance, with a medium effect size (F[4] = 200, p < 0.001, η2p = 0.001). Thus, the age groups are relevant to explain differences in GSI score between individuals.
As illustrated by Figure 3, younger individuals reported more symptoms of psychological distress than older respondents during the COVID-19 pandemic. Individuals in the 30-to-49 age group reported more symptoms between timepoints 1 and 2. A post-hoc comparison of the interaction term showed that most paired comparisons are significant for all interaction groups. The exceptions are the mean difference between 18-to-29-year-olds for both first and second timepoints (t[10254] = -3.557; p = 0.179), the difference between 50-to-59-year-olds at timepoint 1 and 50-to-59-year-olds at timepoint 2 (t[10254] = -1.159; p = 0.998) and against the 60-or-older group at timepoint 2 (t[10254] = 3.253; p = 0.306), and for the 60-or-older group at timepoint 1 no differences were found in comparison with 60 or more years old at the timepoint 2 group (t[10254] = -0.823; p = 1.000). In addition, at timepoint 2 there were no differences between the 50-to-59 and 60-or-older groups (t[10254]) = 3.622; p = 0.157).
Figure 3. Means and standard deviation of each age group at timepoints 1 and 2.
In summary, individuals aged 18 to 29 had the highest mean GSI scores in both timepoints and a wide increase in the mean of GSI between timepoints. The same trend was noted for individuals between 30 and 49 years old. On the other side, people 60 years old or older had the lowest means in timepoint 1 and timepoint 2, but they reported an increase in symptoms at timepoint 2. Individuals aged 50 to 59 showed a stable level of distress between timepoint 1 and timepoint 2 (Figure 3).
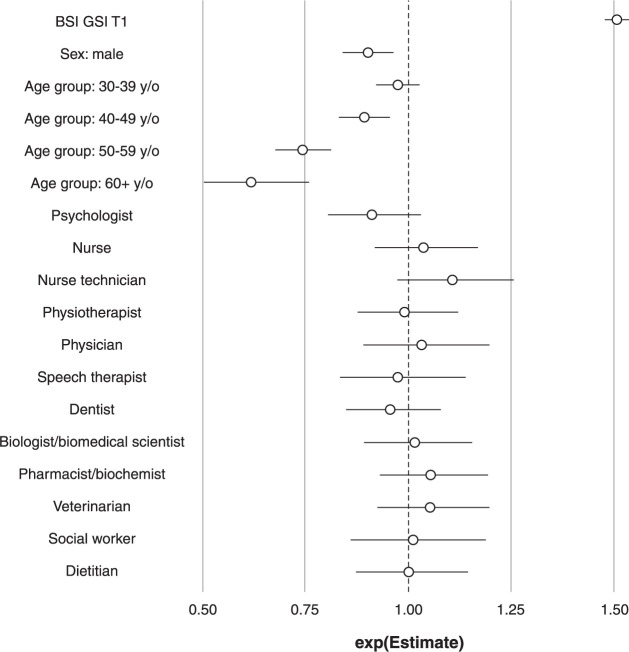
GSI scores were compared among 22 health occupations. The interaction effects were significant (F21 = 3.66, p ≤ 0.001, η2p = 0.007), as were the within-subject effects (F21 = 59.21, p < 0.001, η2p = 0.006), but both showed a trivial effect size. The differences between occupations were also significant (F21 = 9.23, p < 0.001, η2p = 0.019) with a small effect size.
Respondents from 10 of 13 occupations reported an increase in the absolute mean test score in relation to psychological distress (Figure 4). The exceptions were physiotherapy, which remained stable, and dentistry and speech therapy, which reported a decrease in symptoms. Post-hoc comparisons indicated that most of the mean differences were not statistically significant.
Figure 4. Means and standard deviations of Global Severity Index (GSI) scores for each occupation at timepoints 1 and 2.
The last model investigated was the slope variation of all variables of interest between the two timepoints using a Poisson regression model. In the model, the score at timepoint 2 was controlled by the score at timepoint 1, age group, sex, and occupation. The physical education category was excluded from the final model due to matrix singularities, which made its coefficients undefined. After this exclusion, the model adequately converged (χ2[18] = 1971.42, p < 0.001). The baseline score for GSI (odds ratio [OR] = 1.51, p < 0.001), sex (ORmale = 0.90, p < 0.001), and the age groups (OR40-49 years old = 0.89, p < 0.001; OR50-59 years old = 0.74, p < 0.001; OR60+ years old = 0.62, p < 0.001) were statistically significant. None of the occupations had a slope different from 0 (Figure 5). As expected, the baseline GSI score was a good indicator of the GSI score at the second timepoint. Being male or older than 40 years contributed to a lower score on this assessment. Despite variations on the absolute mean score for each occupation, the model did not find any association between having a given occupation and reporting lower or higher symptoms on the GSI scale.
Figure 5. Scaled odds ratio for each predictor of the Global Severity Index (GSI) score at timepoint 2. BSI = Brief Symptom Inventory.
Discussion
Feeling more distressed was common for most health professions through the pandemic. In this study, the first data collection matches the beginning of the pandemic, a time marked by uncertainty, while at the second time point, 6 months later, some health professionals were probably living highly demanding work and domestic routines. In a review of mental health impact on health care professionals who acted in response to previous epidemics, there was a common finding of adverse psychological experiences.22 Wide variability was observed in 94 studies, with 18 to 89% of health workers reporting psychological distress during outbreaks.22 The most common findings were distress and anxiety up to 3 years persisting after the disease outbreak.18 In this pandemic, the risk of feeling distressed could be stratified among health professionals. We found that nurses and doctors reported more distress over time, while for other professions, distress remained stable or even decreased, as was the case for dentistry.
We found higher distress for nurses since the beginning of the pandemic, which might reflect early stressful conditions or an already existing occupational burden. Six months later, nurses still reported high scores of distress. A previous study showed high rates of suicide among nurses compared to physicians and to the general population.23 A Chinese study identified a high number of suicides among nurses, and discussed the need to improve work environment, income, and the psychological condition of this population.24 A 6-month follow up of changes in the stress levels of health professionals in Finland suggests that the measure of distress was an important feature to define worsening outcome.25 Our data also suggest that nurses may require special attention from other professions and society, especially in periods of an even higher work burden. The features related to this finding were not evaluated; however, nurses are a clear target for additional support and mental health care.23
Interesting findings related to sex were observed. Women usually had higher scores early in the pandemic, and scores remained higher over time. In contrast, men’s scores started lower, but seemed to reflect a greater impact of distress after 6 months, showing a more pronounced slope. A Spanish study about distress and loneliness perception during lockdown found lower distress in older respondents, which was attributed to a better use of adaptive coping strategies.26 Here, we found a higher impact among adults aged 30-39 followed by 40-49-year-olds, suggesting a higher impact when compared to older adults. In a Mexican sample, being an adult woman and living with children were risk factors associated with distress.27 We did not evaluate associated factors, but we can assume a potential burden linked to overload for adults, particularly women, who have more to handle at work and at home. Homeschooling children, working from home, fear of economic struggle, and risk of contaminating loved ones were identified as distressing factors in a previous study by our groups.3 All these variables might be important to determine risk of long-lasting psychiatric consequences.
Brazil is a large and heterogeneous country. Data were collected from different municipalities, affected differently by the pandemic. However, all were exposed to a deadly first wave, and for some, the second wave was emerging or ongoing during data collection. As vaccination in Brazil started in January 2021, it had not yet changed the scenario during data collection, but it did provide a perspective of better days ahead. We expect that next waves will start to show a decrease in the number of symptomatic individuals and severity of symptoms tending to decline as vaccines are widely distributed. This will allow people to start having more of a normal life and fewer economic constraints. Despite the representative national health care sampling, this study has some limitations of which we are aware: we likely reached a population with more internet access, and we lost a considerable number of respondents to follow-up, which might have introduced bias.
During the pandemic, there were a multitude of factors associated with healthcare professionals and a constant need to identify ways to minimize impact. Identifying vulnerabilities is essential to optimize efforts and provide the best conditions to mitigate the impacts of COVID-19 and its burden on health workers, especially because this does not cease with the outbreak. Strengths and weakness of the healthcare system, its organizational policies, and social factors that could potentially affect the mental health perceptions of individuals all need to be evaluated. Caring for health professionals seems essential to avoid burnout and to reduce the likelihood of providers leaving their occupation. Our findings suggest that nurses, adults, and women should be targets of any call for action. Since feeling supported was an important feature for physicians’ recovery in China,28 there is a potential benefit to establishing regular screening for stress and anxiety and making mental health services available. In terms of policies, it is paramount to help health professionals fulfill their fundamental work during the most critical times of the pandemic and beyond.
Disclosure
The authors report no conflicts of interest.
Footnotes
How to cite this article: Serpa ALO, Pinto ALB, Diaz AP, Romano-Silva MA, Costa DS, Joaquim RM, et al. The mental health of Brazilian healthcare professionals during the COVID-19 pandemic: a longitudinal study. Braz J Psychiatry. 2022;44:401-408. http://doi.org/10.47626/1516-4446-2021-2347
References
- 1.Sethi BA, Sethi A, Ali S, Aamir HS. Impact of coronavirus disease (COVID-19) pandemic on health professionals. Pak J Med Sci. 2020;36(COVID19-S4):S6–11. doi: 10.12669/pjms.36.COVID19-S4.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Paula JJ, Costa DS, Serpa ALO, da Silva AG, Pinheiro MIC, Malloy-Diniz LF, et al. Quality of life of health care professionals in pandemic times. Clin Neuropsychiatry. 2021;18:113–8. doi: 10.36131/cnfioritieditore20210301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costa DS, de Paula JJ, Serpa ALO, Dias AP, Marques da Rocha MC, Pinto ALB, et al. Predictors of psychological distress and prevalence of self-reported mental disorders across healthcare professionals and the general population during the COVID-19 outbreak in Brazil. doi: 10.31234/osf.io/szhnx. Epub ahead of print. [DOI] [Google Scholar]
- 4.Mirowsky J, Ross CE. Measurement for a human science. J Health Soc Behav. 2002;43:152–70. [PubMed] [Google Scholar]
- 5.Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–92. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Daly M, Sutin AR, Robinson E. Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study. Psychol Med. 2020 Nov 13;:1–10. doi: 10.1017/S0033291720004432. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huckins JF, daSilva AW, Wang W, Hedlund E, Rogers C, Nepal SK, et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: longitudinal smartphone and ecological momentary assessment study. J Med Internet Res. 2020;22:e20185. doi: 10.2196/20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cai H, Tu B, Ma J, Chen L, Fu L, Jian Y, et al. Psychological impact and coping strategies of frontline medical staff in human between January and March 2020 during the outbreak of Coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:e924171. doi: 10.12659/MSM.924171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu CY, Yang YZ, Zhang XM, Xu X, Dou QL, Zhang WW, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect. 2020;148:e98. doi: 10.1017/S0950268820001107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang C, Wang D, Abbas J, Duan K, Mubeen R. Global financial crisis, smart lockdown strategies, and the COVID-19 spillover impacts: a global perspective implications from Southeast Asia. Front Psychiatry. 2021;12:643783. doi: 10.3389/fpsyt.2021.643783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abbas J. Crisis management, transnational healthcare challenges and opportunities: the intersection of COVID-19 pandemic and global mental health. Res Glob. 2021;3:100037. [Google Scholar]
- 13.Su Z, McDonnell D, Wen J, Kozak M, Abbas J, Šegalo S, et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Global Health. 2021;17:4. doi: 10.1186/s12992-020-00654-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Derogatis LR, Spencer P. Upper Saddle River, NJ: Pearson; 1993. Brief symptom inventory: BSI. [Google Scholar]
- 15.Serpa ALO, Costa DS, Ferreira CMC, Pinheiro MIC, Diaz AP, de Paula JJ, et al. Brief symptoms inventory psychometric properties supports the hypothesis of a general psychopathological factor. Trends Psychiatry Psychother. 2021 Mar 23; doi: 10.47626/2237-6089-2021-0207. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Serpa ALO, de Miranda DM, Costa DS, de Paula JJ, Pinheiro MIC, Diaz AP, et al. Brief Symptom Inventory: reporting Brazilian populational parameters during COVID-19 pandemics. Rev Psiquiatr Clin. 2021;48:12–5. [Google Scholar]
- 17.Lee S, Lee DK. What is the proper way to apply the multiple comparison test? Korean J Anesthesiol. 2020;73:572. doi: 10.4097/kja.d.18.00242.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models Usinglme4. J Stat Soft. 2015:67. [Google Scholar]
- 19.Long JA. jtools: Analysis and Presentation of Social Scientific Data [Internet] Apr 25, 2022. cran.r-project.org/package=jtools
- 20.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. Abingdon: Routledge; 2013. [Google Scholar]
- 21.Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 22.Magill E, Siegel Z, Pike KM. The mental health of frontline health care providers during pandemics: a rapid review of the literature. Psychiatr Serv. 2020;71:1260–9. doi: 10.1176/appi.ps.202000274. [DOI] [PubMed] [Google Scholar]
- 23.Davis MA, Cher BAY, Friese CR, Bynum JPW. Association of US nurse and physician occupation with risk of suicide. JAMA Psychiatry. 2021;78:1–8. doi: 10.1001/jamapsychiatry.2021.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeng HJ, Zhou GY, Yan HH, Yang XH, Jin HM. Chinese nurses are at high risk for suicide: a review of nurses suicide in China 2007-2016. Arch Psychiatr Nurs. 2018;32:896–900. doi: 10.1016/j.apnu.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 25.Laukkala T, Suvisaari J, Rosenström T, Pukkala E, Junttila K, Haravuori H, et al. COVID-19 pandemic and Helsinki University Hospital personnel psychological well-being: six-month follow-up results. Int J Environ Res Public Health. 2021;18:2524. doi: 10.3390/ijerph18052524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Losada-Baltar A, Martínez-Huertas JÁ, Jiménez-Gonzalo L, Pedroso-Chaparro MS, Gallego-Alberto L, Fernandes-Pires J, et al. Longitudinal correlates of loneliness and psychological distress during the lockdown situation due to COVID-19. Effects of age and self-perceptions of aging. J Gerontol B Psychol Sci Soc Sci. 2022;77:652–60. doi: 10.1093/geronb/gbab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Toledo-Fernández A, Betancourt-Ocampo D, González-González A. Distress, Depression, anxiety, and concerns and behaviors related to COVID-19 during the first two months of the pandemic: a longitudinal study in adult Mexicans. Behav Sci (Basel) 2021;11:76. doi: 10.3390/bs11050076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peng M, Wang L, Xue Q, Yin L, Zhu BH, Wang K, et al. Post-COVID-19 epidemic: allostatic load among medical and nonmedical workers in China. Psychother Psychosom. 2021;90:127–36. doi: 10.1159/000511823. [DOI] [PMC free article] [PubMed] [Google Scholar]