Abstract
Introduction: The development of medical artificial intelligence (AI) is related to programs intended to help clinicians formulate diagnoses, make therapeutic decisions and predict outcomes. It is bringing a paradigm shift to healthcare, powered by the increasing availability of healthcare data and rapid progress in analytical techniques (1). Artificial intelligence techniques include machine learning methods for structured data, such as classical support vector machines and neural networks, modern deep learning (DL), and natural language processing for unstructured data.
Methodology:More than 50 articles were reviewed and 41 of them were shortlisted. The review was based on a literature search in PubMed, Embase, Google Scholar, and Scopus databases.
Review:Laboratory medicine incorporates new technologies to aid in clinical decision-making, disease monitoring, and patient safety. Clinical microbiology informatics is progressively using AI. Genomic information from isolated bacteria, metagenomic microbial results from original specimens, mass spectra recorded from grown bacterial isolates and large digital photographs are examples of enormous datasets in clinical microbiology that may be used to build AI diagnoses.
Conclusion:Technological innovation in healthcare is accelerating and has become increasingly interwoven with our daily lives and medical practices such as smart health trackers and diagnostic algorithms.
Keywords:artificial intelligence, AI, laboratory medicine, infectious diseases, clinical diagnosis.
BACKGROUND
Integrating artificial intelligence (AI) in clinical diagnosis and treatment recommendations is now being widely implemented. Artificial intelligence is a branch of science that deals with helping machines find a solution to complex problems in a more humanlike fashion. This generally involves borrowing characteristics from human intelligence and applying them as algorithms in a computer- friendly way.
INTRODUCTION
The development of medical artificial intelligence is related to the development of AI programs that are intended to help the clinician in the formulation of a diagnosis, making of therapeutic decisions, and prediction of the outcome. Such systems include artificial neural networks (ANN), fuzzy expert systems, hybrid intelligent systems, and evolutionary computation. The advancement of intelligent medical technologies has paved the way for the emergence of a new medical field: augmented medicine. Other digital tools, such as surgical navigation systems for computer-assisted surgery, and virtuality-reality continuum tools for surgery, pain management, and psychotic diseases, are also enabling augmented medicine.
AccuVein is one example. The handheld device uses laser-based technology to “see” through your skin and into your veins. It is intended to make it easier for doctors, nurses or others to find a vein to draw blood or place an IV device.
The augmented reality technology included a headset with a display the doctors could see through to the person. It allowed them to project images from X-rays or computed tomography (CT) scans, for example, onto the body, to see both at the same time. As long as those images are lined up just right, it is as if surgeons have an X-ray vision.
Artificial intelligence aims to mimic human cognitive functions. It is bringing a paradigm shift to healthcare, powered by the increasing availability of healthcare data and rapid progress of analytical techniques (1). Artificial intelligence techniques include machine learning methods for structured data, such as the classical support vector machine and neural network, and modern deep learning, as well as natural language processing for unstructured data. Major areas that use AI tools include cancer, neurology, medicine and cardiology (1).
Machine learning is the type of AI which is being predominantly used in the field of medicine. Neural networks and deep learning are the most complex kinds of machine learning, with many levels of features or variables that predict outcomes.
The detection of possibly malignant tumours in radiography pictures is a common use of deep learning in healthcare.
Deep learning is increasingly being used in radiomics or the discovery of clinically significant patterns in imaging data that are beyond the detection ability of the human eye (2).
Yet, another type, known as natural language processing (NLP), includes applications such as speech recognition, text analysis, translation and other goals related to language. There are two basic approaches to it: statistical and semantic NLP.
In healthcare, the dominant applications of NLP involve the creation, understanding and classification of clinical documentation and published research. Natural language processing systems can analyse unstructured clinical notes on patients, prepare reports (eg, on radiology examinations), transcribe patient interactions and conduct conversational AI.
Robotic process automation employed in healthcare for repetitive operations such as prior authorization, updating patient information, and billing.
Since the 1970s, when MYCIN was created at Stanford to diagnose blood-borne bacterial infections, AI has been focused on disease diagnosis and therapy. Artificial intelligence is a process of acquiring data followed by its interpretation and learning to achieve the desired outcome (3).
METHODOLOGY
More than 50 articles were reviewed, of which 41 were shortlisted. The review was based on a literature search in PubMed, Embase, Google Scholar, and Scopus databases.
REVIEW
Laboratory medicine is always incorporating new technology to aid clinical decision-making, disease monitoring and patient safety. Innovation has the ability to alter healthcare systems and laboratory medicine by providing healthcare workers with the knowledge and tools they need to give better care to more patients while using less resources. Artificial intelligence has the ability to transform present diagnostic, disease preventive and control techniques, dramatically improving patient safety and treatment quality. To enhance workflow and personnel utilisation, labs now employ software to automate sample, operation, and outcome management. Rule-based autoverification, for example, compares patient outcomes to many factors in order to validate and expedite reporting or reactive actions. Simultaneously, sophisticated systems monitor activities to identify bottlenecks and warn of possible problems, such as STAT sample delays or reagent expiry. Healthcare systems rely on digitalization to manage hundreds or thousands of point-of-care (POC) testing devices and their data outside of the central lab. These rule-based programmes conduct activities and calculations directly as they are programmed, following predetermined logic. Artificial intelligence is the next phase in the evolution of laboratory software. Awareness of AI and its applications is still an ongoing debate amongst the treating physicians, but it has shown accuracies in the radiological and laboratory diagnosis of infectious diseases.
Infectious diseases are characterised by rapid transmission and harmful effects, so researchers must explore and foresee the location and future intensity of an epidemic. Mathematicians have been able to use machine learning algorithms not only to estimate the size and location of the epidemic, but also to investigate the infection relationship. The COVID-19 pandemic has recently served as a catalyst for AI and innovation. Kaur et al discussed the results of AI models and shown that human-driven control methods had a major influence on screening, analysis, prediction, and tracking of infected persons. They also compared AI and non-AI based ways to identify COVID-19 symptoms and had clearly highlighted AI as a crucial instrument in infectious disease management as well as its current deployment in the COVID-19 pandemic, with the goal of reducing time, cost and human effort, together with providing efficient and dependable solutions in the pandemic (4).
Lin et al conducted a retrospective study in which they used a deep learning model – COVNet is a COVID-19 detection neural network that was created to extract visual information from volumetric chest CT scans for COVID-19 detection; CT scans of communi- ty-acquired pneumonia (CAP) and other nonpneumonia abnormalities were included to test the robustness of the model. The authors discovered that in the independent test set, the per-scan sensitivity and specificity for identifying CAP were 87% (152 of 175 scans) and 92% (239 of 259 scans), respectively, with an area under the receiver operating characteristic curve of 0.95 (95% CI: 0.93-0.97). They demonstrated that a deep learning algorithm could detect coronavirus 2019 and distinguish it from commu- nity-acquired pneumonia and other lung diseases (5).
Another implementation of AI in the COVID-19 pandemic is treatment surveillance, which allows for automatic prediction of virus spread, diseased individuals and keeping the public informed about the pandemic situation as well as contact tracing of individuals by identifying "hot spots" to trace the infection and predict the future course and chances of remission. Airport testing is one of the numerous precautions used to prevent the spread of a contagious disease. Various machine learning parameters, including Matlab, nested one versus one (OVO) support vector machine (SVM), leave one out cross-validation (LOOCV) and SVM learning method, have been used in combination in diagnostics by separating genetic sequences from bacteria (6).
Also, AI assists in the creation of vaccines and medications by speeding up drug development methodologies, diagnosing processes and clinical trial management (7). Chatbots have been also developed by a number of healthcare organisations to improve mental health services, telehealth as well as patient engagement and wellbeing. Moreover, numerous researchers have highlighted the influence and role of emerging healthcare platforms and electronic mediums such as mobile health, 5G, telemedicine, internet of things, AI and others in the fight against pandemics by acting as advanced weapons to prevent further spread of infection (8-10).
Clinical microbiology informatics is progressively using AI. Genomic information from isolated bacteria, metagenomic microbial results from original specimens, mass spectra recorded from grown bacterial isolates, and huge digital photographs are all examples of enormous data sets in clinical microbiology that may be used to build AI diagnoses (11). Microscopy for traditional Gram stains, ova and parasite production, and histopathology slides might be revolutionised by machine-learning-based image analysis. For instance, a neural network could classify Gram stains from positive blood cultures into Gram positives/negatives and cocci/rods with amazing accuracy (12). Mathison et al offer a computer vision validation for a novel application: protozoa identification in trichrome-stained faecal smears. It is a complete validation of the computer vision programme, including studies of accuracy, precision and detection limit (13). A systematic review documented that machine learning was used for species identification and antibiotic susceptibility testing. Support vector machines, genetic algorithms, artificial neural networks and fast classifiers were among the most extensively utilised machine learning approaches (14). Deep learning is particularly significant for omic analysis because it allows the combination and interpretation of image-based data with – omic information, allowing this data to be used to generate new and more trustworthy knowledge (15). Recently, infectious disorders such as malaria, which have time-consuming diagnosis criteria and need many health services, are diagnosed using machine learning techniques. The use of digital in-line holographic microscopy (DIHM) data processing to detect infected RBCs in the blood of malaria patients is a suitable and cost-effective technology. Furthermore, for training and testing groups, various machine learning techniques are effective and accurate in distinguishing healthy cells from infected ones. Artificial intelligence approaches based on DIHM do not need extensive blood sample processing (16). Infectious outbreaks such as Ebola have necessitated the use of technologically- based approaches such as logistic regression (LR), SVM classifiers (with good accuracy profiles), single layer artificial neural network (ANN) and decision tree (DT), which have proven as a successful set of indicators to be used for various Ebola-related data configurations (17). To allow a better response, technology techniques should also integrate socioeconomic aspects in order to support a consistent approach to infection diagnosis and treatment (18).
Artificial intelligence, which employs convolutional networks, is predicted to play a significant role in cancer outcome prediction. A study conducted by Lee Su-In et al demonstrated a promising approach to identify robust molecular markers for targeted treatment of acute myeloid leukemia (AML) by introducing data from 30 AML patients including genome-wide gene expression profiles and in vitro sensitivity to 160 chemotherapy drugs, a computational method to identify reliable gene expression markers for drug sensitivity by incorporating multi-omic prior information relevant to each gene’s potential to drive cancer. They also showed that their method outperformed several state-of-the-art approaches in identifying molecular markers replicated invalidation data and predicting drug sensitivity accurately (4). Hirasawa et al built a system that could process a large number of stored endoscopic pictures in a short amount of time with clinically meaningful diagnostic capabilities, which may be used in everyday clinical practise to relieve endoscopists' workload (19). Gulshan et al designed an algorithm for identifying referable diabetic retinopathy and macular edoema with excellent sensitivity and specificity (20). Lee et al developed a deep learning-based computer-aided diagnosis approach for detecting cervical lymph node metastases by CT scan in thyroid cancer patients (21). Early lung cancer chest CT scans with AI-assisted automated learning showed good specificity and sensitivity for early lung cancer detection and could be beneficial in the future in assisting doctors in the early diagnosis of microscopic lung cancer nodules (22). Mobedarsany et al showed that AI was proven to be more accurate than surgical pathologists in predicting patient outcomes. This study gives light on the application of deep learning in medicine as well as the integration of histology and genetic data, and ways for dealing with challenges such intratumoral heterogeneity (23). Muneer et al, on the other hand, employed AI approaches to identify glioma grade and their findings were good, with better than 90% accuracy (24). Yala et al created a big database by using a machine learning algorithm to identify important tumour features from breast pathology reports (25). The algorithm-based smartphone software "Skinvision" may assist a user through performing frequent self-checks for skin cancer using a phone and a snapshot of a skin spot. The algorithm, like a doctor, can determine the texture, colour, and form of the lesions. Users get an instant risk assessment for skin lesions in 30 seconds, and the algorithm has been shown to detect 95% of skin cancer at an early stage (26).
IBM's Watson has recently received a lot of attention for its focus on precision medicine, particularly cancer detection and treatment. Watson employs a mix of machine learning and natural language processing techniques. Users discovered how difficult it was to train Watson how to handle certain forms of cancer and integrate it into care procedures and systems, thus initial excitement for this implementation of the technology diminished (27, 28). Recently, Google is working with health-care delivery networks to develop big-data prediction algorithms that will alert physicians to high-risk illnesses like sepsis and heart failure (29). Nvidia, a renowned international technology firm located in the United States, has revealed its ambition to create an AI supercomputer for medical research and medicine delivery in November 2020 (30, 31).
In recent years, the demand for automated laboratory recommendation systems has risen in order to provide more accurate and faster diagnosis. By incorporating image analysis and machine learning into ordinary surgical pathology, the digital revolution is revolutionising the practise of diagnostic surgical pathology. An automated recommendation might help save healthcare resources by improving the accuracy and efficiency of test requests. In a study, it was shown that with limited variables from EHR, the DL model had the greatest discriminating ability for all diagnostic laboratory tests, with a mean AUROC micro of 0.98 and AUROC macro of 0.94, respectively (32). WSI scanners can now capture and store slides in the form of digital pictures, allowing for automated study of histology slides. This scanning, along with deep learning algorithms, enables for the automated detection of lesions based on previously confirmed regions of interest (33). In a simulated setting, machine learning algorithms produced potentially quicker and more accurate diagnoses than 11 pathologists, according to a new research (15). The future laboratory will be more automated and dominated by robotics, as well as more networked to take use of benefits provided by AI and the internet of things (34).
Artificial intelligence has also several administrative applications in healthcare. These are required in healthcare since a typical US nurse, for instance, spends 25% of her time on administrative and regulatory tasks. RPA is the technology that would be most likely to be applicable to this goal. It has a wide range of healthcare applications, including billing process, claims processing and clinical documentation management Based on the DL NHS 111 algorithm, the AI-based clinical assessment service "National health service"- NHS 24 is in the clinical testing phase in Scotland to assist people with minor health concerns at home through telephonic contact (36). Likewise, another virtual care company, "Babylon Health," uses semantic web technology to deliver complementary digital services to improve clinical results. The semantic web aims to make internet data machine-readable. Develop a clinical LDG (Linked Data Graph) to integrate various bioinformatics- based biomedical data banks in a way that is understandable to the average individual who uses AI-based medical services (37).
Before AI may become widespread in medicine, the issue of legal accountability must be settled, particularly in imaging disciplines such as radiology and pathology. The lack of clarity and misunderstanding around important concerns such as the processing of sensitive personal information and data gathering, consent, transparency, storage and other difficulties further complicates and obscures the question of legal accountability for AI-based judgments in medicine. According to a recent study, depending too much on decision support systems in radiology led to a higher rate of false negative diagnoses than when the computer-aided diagnostic system was unavailable to the same group of radiologists (38). In a simulated setting, machine learning algorithms produced potentially quicker and more accurate diagnoses than 11 pathologists according to a new study (15).
Similarly, bringing AI to clinical decision-making also comes with a slew of difficulties. One such challenge is equitable decision-making that does not discriminate based on biases contained in datasets and methodologies used to construct the system. Some AI models lack of transparency, which can have no cognitive similarity to the problem they are tackling, might exacerbate these problems. Understanding the reasons behind a model's choice or suggestion is frequently a difficult task. For instance, if a decision-support tool suggests that a patient's total knee arthroplasty surgery be postponed, the patient and his/her care team might appreciate knowing the variables that led to that conclusion (39, 40).
The laboratory of the future is expected to be increasingly automated and dominated by robotics as well as more networked with the use of AI and the benefits of internet of things (34). Artificial intelligence can be applied across any stream of medical field, including and not limited to clinical and laboratory diagnosis only. One such another example is MetaPath that can be used to prioritize novel drug targets. Such methods can identify combinations of genetic variants or abnormalities that cause disease, including cases where causal genes are either known or unknown. The progress in data integration combined with novel AI/ML algorithms and disease causality modeling will probably shift the paradigm and establish unbiased ways for target selection and prioritization (41).
CONCLUSION
Technological innovation in healthcare is accelerating and has become increasingly interwoven into both our daily lives and medical practice, such as smart health trackers and diagnostic algorithms. Deep learning is now being used to address an increasing number of specialised jobs in medicine. Algorithm help has the ability to increase not only the sensitivity and accuracy of diagnoses, but also the turnaround time, according to the above-presented studies.
Financial support: none declared.
Conflicts of interests: none declared.
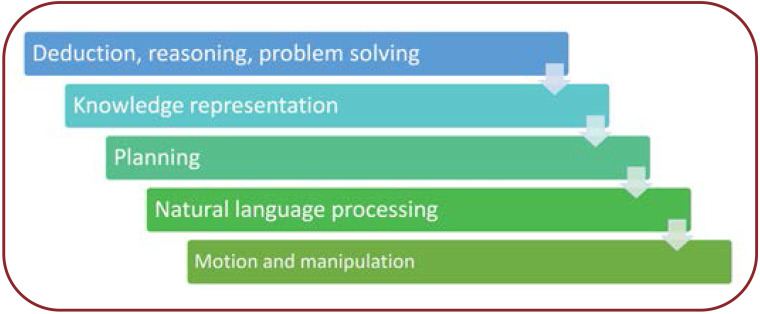
FIGURE 1.
Goals of AI
Contributor Information
Taran Rishit UNDRU, Systems Engineer at TCS, Backend developer at TCS-Apple, Hyd, India.
Utkarsha UDAY, West Bengal University of Health Sciences, Kolkata, India.
Jyothi Tadi LAKSHMI, Department of Microbiology, All India Institute of Medical Sciences, Bibinagar, India.
Ariyanachi KALIAPPAN, Department of Anatomy, AIIMS Bibinagar, Bibinagar, Yadadri-Bhuvanagiri dist., India.
Saranya MALLAMGUNTA, Department of Microbiology, ESIC Medical College and Hospital Sanath Nagar, Hyderabad, India.
Shalam Sheerin NIKHAT, Department of Microbiology, AIIMS Bibinagar, Bibinagar, Yadadri-Bhuvanagiri dist., India.
V SAKTHIVADIVEL, Department of General Medicine, AIIMS Bibinagar, Bibinagar, Yadadri-Bhuvanagiri dist., India.
Archana GAUR, Department of Physiology, AIIMS Bibinagar, Bibinagar, Yadadri-Bhuvanagiri dist., India.
References
- 1.Smith KP, Kirby JE. Image analysis and artificial intelligence in infectious disease diagnostics. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 2020. [DOI] [PMC free article] [PubMed]
- 2.Jiang F, Jiang Y, Zhi H, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2:230–243. doi: 10.1136/svn-2017-000101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6:94. doi: 10.7861/futurehosp.6-2-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaur I, Behl T, Aleya L, et al. Artificial intelligence as a fundamental tool in management of infectious diseases and its current implementation in COVID-19 pandemic. E. nviron Sci Pollut Res Int. 2021;28:40515–40532. doi: 10.1007/s11356-021-13823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li L, Qin L, Xu Z, et al. Using Artificial Intelligence to Detect COVID-19 and Community-acquired Pneumonia Based on Pulmonary CT: Evaluation of the Diagnostic Accuracy. Radiology. 2020;296:E65–E71. doi: 10.1148/radiol.2020200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agrebi S, Larbi A. Use of artificial intelligence in infectious diseases. Artif Intell Precis Health 2020.
- 7.Vaishya R, Javaid M, Khan IH, Haleem A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab Syndr. 2020;14:337–339. doi: 10.1016/j.dsx.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davenport TH, Glaser J. Just-in-time delivery comes to knowledge management. Harv Bus Rev. 2002;80:107–111. [PubMed] [Google Scholar]
- 10.Ye J. The Role of Health Technology and Informatics in a Global Public Health Emergency: Practices and Implications From the COVID-19 Pandemic. JMIR Med Inform. 2020;8:e19866. doi: 10.2196/19866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peiffer-Smadja N, Dellière S, Rodriguez C, et al. Machine learning in the clinical microbiology laboratory: has the time come for routine practice? Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 2020. [DOI] [PubMed]
- 12.Smith KP, Kang AD, Kirby JE. Automated Interpretation of Blood Culture Gram Stains by Use of a Deep Convolutional Neural Network. J Clin Microbiol. 2018;56:e01521–17. doi: 10.1128/JCM.01521-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mathison BA, Kohan JL, Walker JF, et al. Detection of Intestinal Protozoa in Trichrome-Stained Stool Specimens by Use of a Deep Convolutional Neural Network. J Clin Microbiol. 2020;58:e02053–19. doi: 10.1128/JCM.02053-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weis CV, Jutzeler CR, Borgwardt K. Machine learning for microbial identification and antimicrobial susceptibility testing on MALDI-TOF mass spectra: a systematic review. Clin Microbiol Infect Off Publ Eur Soc Clin Microbiol Infect Dis 2020. [DOI] [PubMed]
- 15.Ahmad Z, Rahim S, Zubair M, Abdul-Ghafar J. Artificial intelligence (AI) in medicine, current applications and future role with special emphasis on its potential and promise in pathology: present and future impact, obstacles including costs and acceptance among pathologists, practical and philosophical considerations. A comprehensive review. Diagn Pathol 2021. [DOI] [PMC free article] [PubMed]
- 16.Go T, Kim JH, Byeon H, Lee SJ. Machine learning-based in-line holographic sensing of unstained malaria-infected red blood cells. J Biophotonics. 2018;11:e201800101. doi: 10.1002/jbio.201800101. [DOI] [PubMed] [Google Scholar]
- 17.Colubri A, Silver T, Fradet T, et al. Transforming Clinical Data into Actionable Prognosis Models: Machine-Learning Framework and Field-Deployable App to Predict Outcome of Ebola Patients. PLoS Negl Trop Dis. 2016;10:e0004549. doi: 10.1371/journal.pntd.0004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaur I, Behl T, Aleya L, et al. Artificial intelligence as a fundamental tool in management of infectious diseases and its current implementation in COVID-19 pandemic. Environ Sci Pollut Res. 2021;28:40515–40532. doi: 10.1007/s11356-021-13823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hirasawa T, Aoyama K, Tanimoto T, et al. Application of artificial intelligence using a convolutional neural network for detecting gastric cancer in endoscopic images. Gastric Cancer Off J Int Gastric Cancer Assoc Jpn Gastric Cancer Assoc 2018. [DOI] [PubMed]
- 20.Gulshan V, Peng L, Coram M, et al. Development and Validation of a Deep Learning Algorithm for Detection of Diabetic Retinopathy in Retinal Fundus Photographs. JAMA. 2016;316:2402–2410. doi: 10.1001/jama.2016.17216. [DOI] [PubMed] [Google Scholar]
- 21.Lee JH, Ha EJ, Kim JH. Application of deep learning to the diagnosis of cervical lymph node metastasis from thyroid cancer with CT. Eur Radiol. 2019;29:5452–5457. doi: 10.1007/s00330-019-06098-8. [DOI] [PubMed] [Google Scholar]
- 23.Mobadersany P, Yousefi S, Amgad M, et al. Predicting cancer outcomes from histology and genomics using convolutional networks. Proc Natl Acad Sci USA. 2018;115:E2970–E2979. doi: 10.1073/pnas.1717139115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahammed Muneer K Vnull, Rajendran VR, K PJ. Glioma Tumor Grade Identification Using Artificial Intelligent Techniques. J Med Syst. 2019;43:113. doi: 10.1007/s10916-019-1228-2. [DOI] [PubMed] [Google Scholar]
- 25.Yala A, Barzilay R, Salama L, et al. Using machine learning to parse breast pathology reports. Breast Cancer Res Treat. 2017;161:203–211. doi: 10.1007/s10549-016-4035-1. [DOI] [PubMed] [Google Scholar]
- 26.Malhi IS, Yiu ZZN. Algorithm-based smartphone apps to assess risk of skin cancer in adults: critical appraisal of a systematic review. Br J Dermatol. 2021;184:638–639. doi: 10.1111/bjd.19502. [DOI] [PubMed] [Google Scholar]
- 29.Rysavy M. Evidence-based medicine: a science of uncertainty and an art of probability. Virtual Mentor VM. 2013;15:4–8. doi: 10.1001/virtualmentor.2013.15.1.fred1-1301. [DOI] [PubMed] [Google Scholar]
- 30.Buitrago PA, Nystrom NA, Gupta R, Saltz J. Delivering Scalable Deep Learning to Research with Bridges-AI. In: CARLA 2019.
- 31.Kochanny SE, Pearson AT. Academics as leaders in the cancer artificial intelligence revolution. Cancer. 2021;127:664–671. doi: 10.1002/cncr.33284. [DOI] [PubMed] [Google Scholar]
- 33.Zemouri R, Devalland C, Valmary-Degano S, Zerhouni N. [Neural network: A future in pathology?]. Ann Pathol. 2019;39:119–129. doi: 10.1016/j.annpat.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 34.Kricka LJ. History of disruptions in laboratory medicine: what have we learned from predictions? Clin Chem Lab Med. 2019;57:308–311. doi: 10.1515/cclm-2018-0518. [DOI] [PubMed] [Google Scholar]
- 36.McCartney M. Margaret McCartney: AI in medicine must be rigorously tested. BMJ. 2018;361:k1752. doi: 10.1136/bmj.k1752. [DOI] [PubMed] [Google Scholar]
- 38.Alberdi E, Povykalo A, Strigini L, Ayton P. Effects of incorrect computer-aided detection (CAD) output on decision-making in mammography. Acad Radiol. 2004;11:909–918. doi: 10.1016/j.acra.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 40.Surmacz K, Kamath AF, Andel DV. Fairness in AI: How Can We Avoid Bias and Disparities in Orthopedic Applications of Artificial Intelligence? J Orthop Exp Innov. 2021;4:25901. [Google Scholar]
- 41.Wan G, Du B, Pan S, Haffari G. Reinforcement Learning Based Meta-Path Discovery in Large-Scale Heterogeneous Information Networks. Proc AAAI Conf Artif Intell. 2020;34:6094–6101. [Google Scholar]