Abstract
Prenatal sonographic assessment of the posterior fossa in the mid-sagittal plane at 11-14 weeks’ gestation has been highlighted as an essential diagnostic step by the current literature. This approach is used for the early detection of open spina bifida during the first trimester by analyzing the three spaces of the posterior fossa: brain stem, the fourth ventricle and cisterna magna. Abnormal size of fetal posterior fossa spaces is an important sign in the diagnosis of fetuses with central nervous system malformation and needs to be submitted for differential diagnosis when any alterations are observed. Among them, Dandy-Walker malformation is one of the major causes of congenital hydrocephalus, being a rare condition, with poor-prognosis, manifested by enlarged posterior fossa. On the basis of available evidence, the assessment of the fetal posterior cranial fossa is feasible from 11 to 14 weeks gestational age and it is believed that abnormal appearance of the posterior fossa at this stage of pregnancy could improve early detection of Dandy-Walker malformation by prompting an early second trimester ultrasound evaluation.
Keywords:Dandy-Walker malformation, posterior fossa, brainstem, fourth ventricle, cisterna magna.
INTRODUCTION
Cerebral malformations are among the most common types of major congenital abnormalities. Ultrasound examination has proved its role as an effective modality for prenatal diagnosis of these abnormalities. Therefore, assessment of the fetal posterior fossa in the mid-sagittal plane at 11-14 weeks’ gestation is an essential diagnostic step used in the early detection of open spina bifida by analyzing the three spaces of this fossa: brain stem, the fourth ventricle and cisterna magna. Abnormal size of fetal posterior fossa spaces is an important sign in the diagnosis of fetuses with central nervous system (CNS) malformation and needs to be submitted for differential diagnosis when any alterations are observed. Among them, Dandy-Walker malfor- mation is a rare condition referring to a complex developmental anomaly of the cerebellar vermis, with persistent of Blake’s pouch, being also a major causes of congenital hydrocephalus, with poor prognosis (1).
CASE REPORT
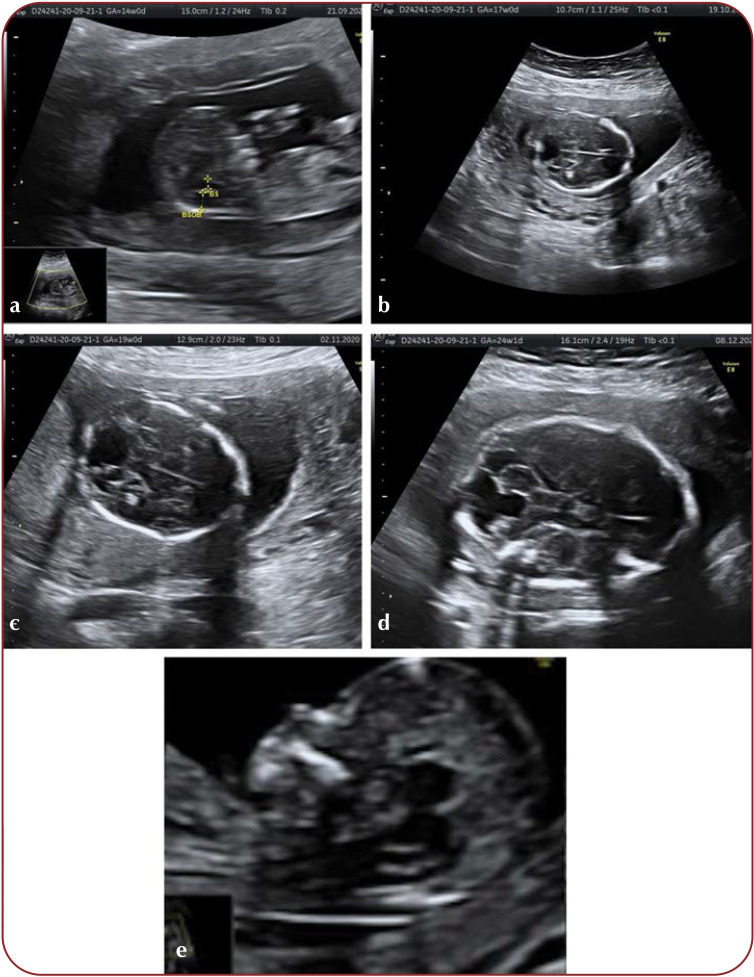
A 40-year old multigravida was referred for routine antenatal ultrasound at 14 weeks of gestation. The fetal posterior fossa was examined by transabdominal scan in the mid-sagittal plane: only two of the three posterior brain spaces were identified, because the border between the forth ventricle (intracranial translucency-IT) and cisterna magna was not visible (Figure 1a).
We measured the brainstem (BS) diameter and brainstem to occipital bone (BSOB) distance and calculated the BS/BSOB ratio. Brainstem to occipital bone consists of the fouth ventricle–cisterna magna complex, the two structures being separated by a visible border (Figure 1e). In the normal fetuses, the BS/BSOB ratio is less than 1 and it is not correlated with the gestational age (2). In the fetuses with open spina bifida, the BS/BSOB ratio is greater than 1: there is an increased brain stem diameter and decreased fourth ventricle and cisterna magna diameters (2). In Dandy-Walker malformation there is an increased BSOB diameter and especially a decreased BS/BSOB ratio (3-5). In our case, the BS/BSOB ratio was less then 1, with no visible border between the fouth ventricle and cistena magna (Figure 1a). The abnormal aspect of the posterior fossa raised the suspicion of a CNS anomaly such as Dandy-Walker complex (1).
A more frequent and detailed follow-up continued and a transabdominal ultrasound evaluation at 17 weeks was performed; extracranial defects, including coarctation of the aorta, bilateral hydronephrosis and talipes, were also revealed. We performed amniocentesis, which revealed normal karyotype. The advanced genetic testing (microarray-CGH testing) was offered but declined, as the patient was committed to the pregnancy (6). Other transabdominal ultrasound evaluations of the brain structures at 19 and 24 weeks of gestation were performed in a transverse axis and showed agenesis of the cerebellar vermis (Figure 1c and Figure 1d), with no evidence of additional intracranial structural defects. A magnetic resonance imaging (MRI) scan was offered but declined.
The fetus developed fetal growth restriction and was monitored by serial ultrasound scans until 32 weeks, when delivery was performed. The newborn presented with growth restriction and severe neurodevelopmental delay and survived only a few weeks. The structural defects were confirmed postnatally by morpho-pathological examination.
DISCUSSION AND CONCLUSION
Some of the CNS anomalies such as acrania, alobar holoprosencephaly or encephalocele are always visible and must be detected during the 11-14 weeks’ scan (5). Other anomalies are potentially detectable by analyzing the indirect signs. Opens spina bifida and Dandy-Walker malformation could be detected in the first trimester by examining the posterior fossa stuctures: brain stem, the fourth ventricle and cisterna magna in the same mid-sagital view that we use in the measurment of nuchal translucency. However, a detailed examnination is required in the early second trimester to confirm the diagnosis.
Patients with a higher risk for a CNS abnormality or those with suspicious findings are required to undergo fetal neurosonography in a maternofetal medicine department, by clinicians with expertise in the field.
When a posterior fossa cyst is detected, absence or hypoplasia of the cerebellar vermis is a key finding for distinguishing between a Dandy-Walker malformation and an arachnoid cyst (6). Moreover, for the differential diagnosis, we should bear in mind that Dandy-Walker malformation it is usually accompanied by other intracranial anomalies like agenesis of the corpus callosum, holoprosencephaly, occipital encephaloceles and ocular defects, but also extracranial anomalies like polycystic kidneys, cardiovascular defects and limb anomalies, abnormalities that our case study developed during the gestation (7, 8). Etiology reunites genetic causes under the form of chromosomal abnormalities, but also environmental factors such as viral infections, alcohol and diabetes.
Before establishing the final diagnosis of Dandy-Walker malformation, a good knowledge regarding the anatomy and natural development of cerebellar vermis is required. It completes its formation form cranial to caudal and sometimes the communication between the forth ventricle and cisterna magna persists open from the 16th to late 20th week of gestation. Therefore, an ultrasound reevaluation between 20 and 22 weeks of gestation is necessary (9).
To exclude other malformations in the area of the CNS, especially morphologic abnormalities, MRI can be performed and, if any chromosomal abnormalities are suspected, genetic testing by CGH array can be of great support.
To conclude, on the basis of available evidence, the assessment of the fetal posterior cranial fossa is feasible from 11 to 14 weeks of gestational age and it is believed that abnormal appearance of the posterior fossa at this stage of pregnancy could improve early detection of Dandy-Walker malformation by prompting an early second trimester ultrasound evaluation, together with other imaging investigations and use of genetics.
Conflict of interests: none declared.
Financial support: none declared.
FIGURE 1.
Ultrasound appearance of fetal posterior fossa and prenatal diagnosis of Dandy-Walker malformation: (a) the brainstem (BS) diameter and brainstem to occipital bone (BSOB) distance and a BS/BSOB ratio calculated by us which was lower than 1; (b) Transabdominal ultrasound evaluation – transverse section of the posterior fossa at 17 weeks; (c) and (d) Transabdominal ultrasound evaluation of the brain structures at 19 and 24 weeks of gestation, which were performed in a transverse axis, showed agenesis of the cerebellar vermis, with no evidence of additional intracranial structural defects; (e) normal appearance of fetal posterior fossa: brain stem, the fourth ventricle, cisterna magna.
Contributor Information
Nicolae GICA, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital Bucharest, Romania.
Anca Maria PANAITESCU, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital Bucharest, Romania.
Corina GICA, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital Bucharest, Romania.
Andreea DUMITRU, Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital Bucharest, Romania.
Radu BOTEZATU, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital Bucharest, Romania.
Gheorghe PELTECU, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital Bucharest, Romania.
Ana Maria VAYNA, Department of Obstetrics and Gynaecology, Filantropia Clinical Hospital Bucharest, Romania.
References
- 1.Volpe P, Muto B, Passamonti U, et al. Abnormal sonographic appearance of posterior brain at 11-14 weeks and fetal outcome. Prenatal diagnosis. 2015;35:717–723. doi: 10.1002/pd.4598. [DOI] [PubMed] [Google Scholar]
- 2.Lachmann R, Chaoui R, Moratalla Jose, et al. Posterior brain in fetuses with open spina bifida, at 11 to 13 weeks. Prenat Diagn. 2011;31:103–106. doi: 10.1002/pd.2632. [DOI] [PubMed] [Google Scholar]
- 3.Lachmann R, Sinkovskaya E, Abuhamad A. Posterior brain in fetuses with Dandy-Walker malformation with complete agenesis of the cerebellar vermis at 11-13 weeks: a pilot study. Prenat Diagn. 2012;32:1–4. doi: 10.1002/pd.3899. [DOI] [PubMed] [Google Scholar]
- 4.Chaoui R, Benoit B, Mitkowska-Wozniak H, Helinhg KS. Assessment of intracranial translucency in the detection of spina bifida at 11- 13 -week scan. Ultrasound Obstet Gynecol. 2009;34:249–252. doi: 10.1002/uog.7329. [DOI] [PubMed] [Google Scholar]
- 5.Vayna AM, Veduta A, Duta S, et al. Diagnosis of fetal structural anomalies at 11 to 14 weeks. J Ultrasound Med. 2018;37:2063–2073. doi: 10.1002/jum.14561. [DOI] [PubMed] [Google Scholar]
- 6.Liu F, Zhang Z, Lin X, et al. Development of the human fetal cerebellum in the second trimester: a post mortem magnetic resonance imaging evaluation. J Anat. 2011;219:582–588. doi: 10.1111/j.1469-7580.2011.01418.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guibaud L, Larroque A, Ville D, et al. Prenatal diagnosis of 'isolated' Dandy-Walker malformation: imaging findings and prenatal counselling. Prenat Diagn. 2012;32:185–193. doi: 10.1002/pd.3828. [DOI] [PubMed] [Google Scholar]
- 8.Murray JC, Johnson JA, Bird TD. Dandy-Walker malformation: etiologic heterogeneity and empiric recurrence risk. Clin Genet. 1985;28:272–276. doi: 10.1111/j.1399-0004.1985.tb00401.x. [DOI] [PubMed] [Google Scholar]
- 9.Paladini D, Quarantelli M, Pastore G, et al. Abnormal or delayed development of the posterior membranous area of the brain: anatomy, ultrasound diagnosis, natural history and outcome of Blake's pouch cyst in the fetus. Ultrasound Obstet Gynecol. 2012;39:279–287. doi: 10.1002/uog.10138. [DOI] [PubMed] [Google Scholar]
- 10.Edwards TJ, Sherr EH, Barkovich AJ, Richards LJ. Clinical, genetic and imaging findings identify new causes for corpus callosum development syndromes. Brain. 2014;137:1579–1613. doi: 10.1093/brain/awt358. [DOI] [PMC free article] [PubMed] [Google Scholar]