Abstract
Purpose
To assess the impact of parental socioeconomic status and keratoconus literacy on pediatric eye rubbing and keratoconus severity.
Methods
In this mixed-methods study, pediatric keratoconus patients (age ≤ 18 years) were retrospectively identified. Sociodemographic and clinical characteristics were extracted from the electronic medical record (EMR). Telephone surveys were subsequently conducted to assess parental keratoconus literacy, receipt of counseling on keratoconus prevention, eye rubbing, and household socioeconomic factors not available in the EMR. Parents reporting poor keratoconus literacy were probed via semi-structured interview to explore barriers to their understanding.
Results
Forty-eight patients met inclusion criteria, 22 (46%) of whom were reached by telephone. Most patients were insured by Medicaid (73%) and current eye rubbers (82%). Few parents reported good or excellent keratoconus literacy now (32%) or at the time of diagnosis (18%). Parents with a high-school education, limited English proficiency, lower income level, and Medicaid insurance tended to have lower keratoconus literacy, though this was not statistically significant. Parental keratoconus literacy was not correlated with disease severity. High-school education, limited English proficiency, lower income level, and Medicaid insurance were correlated with steeper keratometry readings, which was statistically significant for high-school education. In-depth interviews revealed parents felt unconfident with eye health in general and perceived a personal responsibility for learning more.
Conclusion
This is the first study exploring keratoconus literacy from a socioeconomic perspective, demonstrating lower literacy among socioeconomically marginalized parents and a tendency toward more severe disease in their children.
Keywords: keratoconus, social determinants of health, health literacy, disparities
Introduction
Keratoconus is characterized by ectatic protrusion of the cornea and is associated with chronic and rigorous eye rubbing.1 Treatment of eye rubbing triggers, such as allergic conjunctivitis, and patient education are tantamount to halting the development of keratoconus.2 In the United States, socioeconomically marginalized patients bear a high burden of disease3,4 and are more likely to suffer vision loss from chronic eye conditions.5 Keratoconus patients from lower socioeconomic backgrounds are more likely to have severe disease and to require corneal transplantation compared to their more economically privileged counterparts.6 Socioeconomic status encompasses income level, educational attainment, English proficiency, and race/ethnicity. The influence of socioeconomic status on disease outcomes is at least partly mediated by health literacy.7 Health literacy describes the ability to understand and act on health-related information. Children of parents with lower educational attainment and poorer health literacy are at higher risk for non-adherence to patching for amblyopia and topical glaucoma therapy.8–10 Few studies have explored the influence of socioeconomic factors and health literacy on keratoconus severity and management. The purpose of this mixed-methods study is to assess, in a pediatric population, the impact of parental socioeconomic status and keratoconus literacy on pediatric eye rubbing behaviors and keratoconus severity.
Methods
This study was conducted in accordance with the tenets of the Declaration of Helsinki under the approval of the University of California San Francisco (UCSF) Institutional Review Board. Pediatric patients (current age ≤ 18 years) at UCSF with an International Classification of Diseases (ICD) diagnosis of keratoconus (ICD-9 code 371.6, ICD-10 code H18.609) were retrospectively identified and screened for eligibility. UCSF is a public academic medical institution and tertiary referral center with a broad catchment area serving a socioeconomically diverse population. The retrospective period dated from 2015 (the opening year of the pediatric medical center) to 2019. Clinical documentation of keratoconus and complete data in the electronic medical record (EMR) were required for inclusion.
In this mixed-methods study, sociodemographic and clinical characteristics (including age, gender, primary language spoken, insurance payer, and corneal topography) were obtained retrospectively from the EMR. Surveys of patients’ parents were subsequently conducted to assess parental keratoconus literacy (currently and at the time of diagnosis), as this is not routinely elicited or documented in clinical encounters. Parents were also queried regarding their child’s eye rubbing behaviors, receipt of counseling from the doctor on keratoconus prevention, and household sociodemographic factors not available in the EMR (including highest educational attainment, income level, and reliability of transportation to and from clinic appointments). Surveys were conducted by telephone due to precautions imposed by the coronavirus disease 2019 (COVID-19) pandemic. Parents provided verbal consent. Written information about the study was available upon request. The telephone survey is contained in Supplement 1. Parents who reported poor keratoconus literacy were probed via semi-structured in-depth interview to explore barriers to their understanding. Certified institutional telephone interpreters were used for parents for whom English was not the preferred language. Interview prompts are shown in Supplement 2.
The chi-square test of independence and t-test were used to assess the impact of socioeconomic factors on keratoconus literacy, and the impact of both of these variables on patient eye rubbing and disease severity (defined using steep keratometry in diopters, D). Statistical significance was set a priori at P < 0.05. Stata software version 15.1 (StataCorp, College Station, TX) was used for statistical analysis. Interviews were audio recorded and transcribed, then analyzed using thematic analysis.11
Results
Survey
Forty-eight patients met the inclusion criteria. Parents of 22 patients were reached by telephone for a survey response rate of 46%. The mean patient age was 15 years (range: 13–17). Most patients were male (n = 14, 64%) and insured by Medicaid (n = 16, 73%). More than half of parents were English proficient (n = 13, 59%), college-educated (n = 12, 54%), and reported good or excellent transportation to and from clinic appointments (n = 19, 86%), though half endorsed commuting 1 hour or more (n = 11, 50%).
Most children were currently still rubbing their eyes (n = 18, 82%). Few parents reported good or excellent knowledge of keratoconus now (n = 7, 32%) or at the time of diagnosis (n = 4, 18%). Fifty-nine percent (n = 13) of parents reported that they were educated about disease prevention at the time of diagnosis. Eighty-two percent (n = 18) reported that they had since been counseled on prevention. Nineteen patients (86%) had keratometry data in the EMR, and the mean steep keratometry of our study patient cohort was 52.7 D (SD: 9.5).
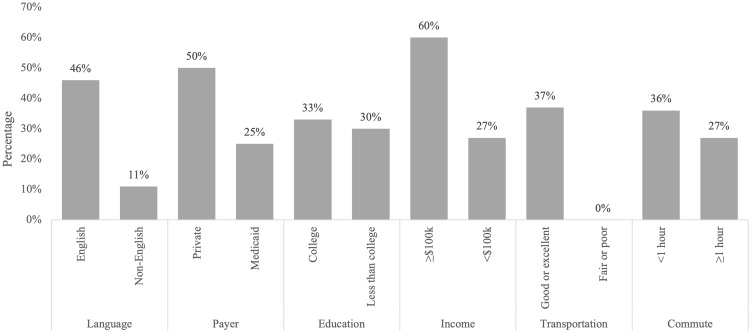
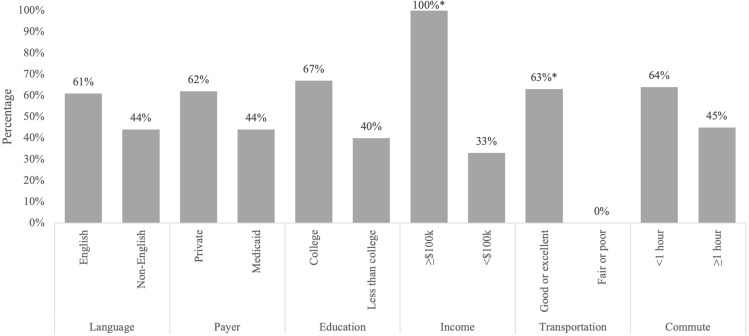
In regard to the influence of socioeconomic factors on keratoconus literacy, language spoken, parental educational level, parental income level, insurance payer, and reliability of transportation were not correlated with parental knowledge of keratoconus at the time of diagnosis. However, parents with children insured by Medicaid, no college education, limited English proficiency, and lower incomes were less likely to report receiving education on keratoconus prevention at the time of diagnosis. They were also less likely to endorse “good” or “excellent” knowledge of keratoconus, though none of these associations were statistically significant, as shown in Table 1 and Figure 1. However, lower income patients and those with unreliable transportation were significantly less likely to report having ever received education on keratoconus prevention: χ2 (1, N = 19) = 6.67, P = 0.010, χ2 (1, N = 22) = 4.17, P = 0.041, respectively. See Figure 2.
Table 1.
Parental Understanding of Keratoconus, Education on Keratoconus Prevention, Eye Rubbing Behaviors, and Keratoconus Severity, Stratified by Socioeconomic Factors
| Household Language | Insurance Payer | Highest Parental Education | Annual Household Income | Transportation to/from Clinic | Commute to/from Clinic | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| English | Non-English | P | Private | Medicaid | P | ≥College | <College | P | ≥100k | <100k | P | Good or Excellent | Fair or Poor | P | <1 Hour | ≥1 Hour | P | |
| Understanding at time of diagnosis | ||||||||||||||||||
| Good or excellent | 2 (15%) | 2 (22%) | 0.68 | 2 (15%) | 2 (22%) | 0.91 | 1 (8%) | 3 (30%) | 0.19 | 0 (0%) | 3 (20%) | 0.28 | 3 (16%) | 1 (33%) | 0.46 | 0 (0%) | 4 (36%) | 0.027 |
| Fair or poor | 11 (85%) | 7 (78%) | 11 (85%) | 7 (78%) | 11 (92%) | 7 (70%) | 5 (100%) | 12 (80%) | 16 (84%) | 2 (67%) | 11 (100%) | 7 (64%) | ||||||
| Educated on prevention at time of diagnosis | ||||||||||||||||||
| Yes | 7 (54%) | 4 (44%) | 0.66 | 4 (67%) | 2 (33%) | 0.34 | 7 (58%) | 4 (40%) | 0.39 | 4 (80%) | 6 (40%) | 0.12 | 10 (53%) | 1 (33%) | 0.53 | 6 (55%) | 5 (45%) | 0.67 |
| No | 6 (46%) | 5 (56%) | 7 (44%) | 9 (56%) | 5 (42%) | 6 (60%) | 1 (20%) | 9 (60%) | 9 (47%) | 2 (67%) | 5 (45%) | 6 (55%) | ||||||
| Current understanding | ||||||||||||||||||
| Good or excellent | 6 (46%) | 1 (11%) | 0.083 | 3 (50%) | 4 (25%) | 0.26 | 4 (33%) | 3 (30%) | 0.87 | 3 (60%) | 4 (27%) | 0.18 | 7 (37%) | 0 (0%) | 0.2 | 4 (36%) | 3 (27%) | 0.65 |
| Fair or poor | 7 (54%) | 8 (89%) | 3 (50%) | 12 (75%) | 8 (67%) | 7 (70%) | 2 (40%) | 11 (73%) | 12 (63%) | 3 (100%) | 7 (64%) | 8 (73%) | ||||||
| Educated on prevention | ||||||||||||||||||
| Yes | 8 (61%) | 4 (44%) | 0.43 | 8 (62%) | 4 (44%) | 0.097 | 8 (67%) | 4 (40%) | 0.21 | 5 (100%) | 5 (33%) | 0.010 | 12 (63%) | 0 (0%) | 0.041 | 7 (64%) | 5 (45%) | 0.39 |
| No | 5 (39%) | 5 (56%) | 5 (38%) | 5 (56%) | 4 (33%) | 6 (60%) | 0 (0%) | 10 (67%) | 7 (37%) | 3 (100%) | 4 (36%) | 6 (55%) | ||||||
| Current eye rubbing | ||||||||||||||||||
| Yes | 11 (85%) | 7 (78%) | 0.68 | 6 (100%) | 12 (75%) | 0.18 | 11 (92%) | 7 (70%) | 0.19 | 0 (0%) | 4 (27%) | 0.2 | 4 (21%) | 0 (0%) | 0.38 | 2 (18%) | 2 (18%) | 1.0 |
| No | 2 (15%) | 2 (22%) | 0 (0%) | 4 (25%) | 1 (8%) | 3 (30%) | 5 (100%) | 11 (73%) | 15 (79%) | 3 (100%) | 9 (82%) | 9 (82%) | ||||||
| Current eye rubbing pressure | ||||||||||||||||||
| Light | 2 (17%) | 4 (57%) | 0.067 | 0 (0%) | 6 (46%) | 0.044 | 3 (25%) | 3 (43%) | 0.42 | 0 (0%) | 5 (42%) | 0.086 | 5 (31%) | 1 (33%) | 0.94 | 2 (18%) | 4 (50%) | 0.14 |
| Medium or hard | 10 (83%) | 3 (43%) | 6 (100%) | 7 (54%) | 9 (75%) | 4 (57%) | 5 (100%) | 7 (58%) | 11 (69%) | 2 (67%) | 9 (82%) | 4 (50%) | ||||||
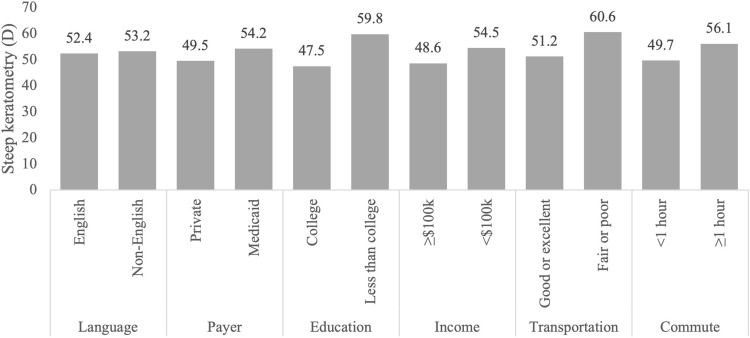
| Steep K (mean, D) | 52.4 | 53.2 | 0.88 | 49.5 | 54.2 | 0.34 | 47.5 | 59.8 | 0.002 | 48.6 | 54.5 | 0.28 | 51.2 | 60.6 | 0.12 | 49.7 | 56.1 | 0.15 |
Notes: P-values were computed using the chi-square test for significance or the t-test. Bold p-values highlight significance at <0.05.
Abbreviations: P, p-value, K, keratometry, D, diopters, 100k, 100,000.
Figure 1.
Percentage of parents, stratified by socioeconomic status, endorsing good or excellent current knowledge of keratoconus. Factor levels are not paired and the maximum percentage for each column is 100%. For example, 60% of patients with a household income ≥$100,000 reported good or excellent knowledge compared to 27% of patients with a household income <$100,000.
Figure 2.
Percentage of parents, stratified by socioeconomic status, who reported receiving education on keratoconus progression. Asterisks (*) indicate statistical significance at P < 0.05. Factor levels are not paired and the maximum percentage for each column is 100%.
The prevalence of eye rubbing did not vary by socioeconomic status or keratoconus literacy. Patients who were privately-insured were more likely than Medicaid-insured patients to be described by their parents as medium or hard (as opposed to light) eye rubbers, χ2 (1, N = 19) = 4.05, p = 0.044. In regard to disease severity, patients from non-English-speaking, Medicaid-insured, less educated, and lower income backgrounds, as well as those with less reliable transportation and longer commute times, tended to have steeper keratometry readings, but only lower education was statistically significant, t(17) = −3.60, P = 0.002, as shown in Figure 3. Parental keratoconus literacy was not correlated with disease severity.
Figure 3.
Mean steep keratometry (in diopters) by socioeconomic status.
When probed for barriers to their understanding, respondents were able to describe the physical features of keratoconus and define eye rubbing as a risk factor. A few noted potential serious complications, namely corneal hydrops. In terms of knowledge deficits, parents expressed wanting to know the exact cause of their child’s keratoconus. When asked to describe their interactions with our doctors, they described receiving clear and thorough explanations. Non-English-speaking parents stated language was not a barrier due to the presence of language interpreters. A few described their ignorance of eye health in general and a need for more information, a better description of certain terms, and greater opportunity to ask questions. One parent described a personal responsibility for learning more, stating, “maybe it’s just us that we need to do more research.” Another parent suggested a more paternalistic approach, “I don’t ask questions, I trust the doctor.” A few described delays in reaching a specialist or difficulty affording antihistamine eye drops to discourage eye rubbing. Supplement 2 contains comments organized by theme.
Discussion
This study examined parental keratoconus literacy, pediatric eye rubbing, and keratoconus severity from a socioeconomic perspective. Low socioeconomic status is associated with a higher risk of vision loss from treatable eye conditions,5 and this association is at least partly mediated by health literacy.7 Few studies have explored health literacy in patients with chronic eye diseases. In the adult population, patients receiving intravitreal treatment for chronic retinal diseases, such as age-related macular degeneration, have been shown to have low rates of health literacy.12 Poor health literacy has been associated with a higher prevalence of preventable conditions such as diabetic retinopathy and severe glaucoma,13,14 and lower treatment compliance.15 A recent Swiss study of patients with keratoconus identified dramatically little knowledge about the typical signs, risk factors, and treatment options for keratoconus, and patients with a university degree showed only a moderately higher knowledge level.16 Similarly, in this study, keratoconus literacy was low, with few parents reporting satisfactory understanding of keratoconus currently or at the time of diagnosis. Parents from socioeconomically marginalized backgrounds (ie, limited English proficiency, lower income, lower educational attainment, and unreliable transportation) endorsed poorer keratoconus literacy than parents from more privileged backgrounds. Their children also tended to have more severe keratoconus by steep keratometry, but this was only statistically significant for parents with lower educational attainment.
Socioeconomic barriers to eye care are well-demonstrated.5,17 Ethnic minority status, low educational attainment, and low income are associated with underutilization of preventative eye care and higher risk of vision loss from preventable conditions.5 Patients insured by Medicaid – a proxy for socioeconomic status – have been shown to have more severe keratoconus and to have a higher risk of corneal transplantation compared to commercially insured patients.6 Barriers to care for socioeconomically marginalized patients include economic and systems-related factors (eg, cost of care, lack of insurance coverage, provider inaccessibility), patient-related factors (eg, limited time for medical care, transportation barriers, overshadowing by comorbidities, low health literacy), and the patient-provider relationship (eg, lack of communication or trust, language discordance).5,18,19 Prior studies of the relation between education level and keratoconus incidence have been inconclusive, showing either no relation,20 an association with lower education,21 or an association with higher education due to a greater likelihood of seeking care.22
In this study, we interviewed parents reporting a poor understanding of keratoconus to contextualize the survey findings. All parents accurately described the signs of keratoconus and risk factors and denied major barriers to their understanding. There are a few explanations for the apparent discord between the survey and interview findings. Patients from marginalized backgrounds have been shown to be reluctant to express their own lack of knowledge or to suggest that their health experience is different because of their social status or spoken language .23 There is also evidence that people with low socioeconomic status tend to have less trust in doctors and confidence in their ability to understand health information.24,25 Thus, parents may have assumed a knowledge gap in their understanding due to lower trust in the health information they were given or lack of confidence in their own understanding.
There are several study limitations. The small sample size renders this study underpowered for statistical significance. While the survey response rate was less than 50%, this is in line with the average response rate for telephone surveys.26 Furthermore, since more marginalized patients tend to have lower response rates on telephone surveys,26 our conclusions likely underrepresent the full impact of socioeconomic barriers in parental understanding of keratoconus. Parents were asked to recall their knowledge of keratoconus at the time of diagnosis, which is subject to recall bias, and we did not use a validated or objective measure of health literacy for keratoconus. Use of objective assessments may distinguish true knowledge gaps from those influenced by sociocultural factors, though the latter was of interest in this particular study. Surveys and interviews were conducted one-on-one by telephone as this study was performed during the COVID-19 pandemic. In-person focus groups are more appropriate for needs assessments, with the interactive format and facilitated discussion allowing participants to offer new and collaborative ideas.27
In conclusion, this is the first study exploring keratoconus literacy from a socioeconomic perspective. We demonstrate poorer understanding among socioeconomically marginalized parents and a tendency toward more severe disease in their children. Socioeconomic status and health literacy are important drivers of pediatric health disparities. Future studies should explore the use of health literacy assessments and educational interventions to improve outcomes for patients from all backgrounds.28
Funding Statement
This project received funding from the University of California San Francisco (UCSF) Inquiry Funding Office and was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number UL1 TR001872. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. This project was also made possible in part by unrestricted grant funding from That Man May See (San Francisco, CA) and Research to Prevent Blindness (New York, NY) to the University of California San Francisco, Department of Ophthalmology.
Abbreviations
ICD, International Classification of Diseases; D, diopter.
Disclosure
Dr Neel D Pasricha reports personal fees from iota Biosciences, outside the submitted work. No conflicting relationship exists for any author.
References
- 1.Najmi H, Mobarki Y, Mania K, et al. The correlation between keratoconus and eye rubbing: a review. Int J Ophthalmol. 2019;12(11):1775–1781. doi: 10.18240/ijo.2019.11.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McMonnies CW. Management of chronic habits of abnormal eye rubbing. Cont Lens Anterior Eye. 2008;31(2):95–102. doi: 10.1016/j.clae.2007.07.008 [DOI] [PubMed] [Google Scholar]
- 3.Bjur KA, Wi CI, Ryu E, et al. Socioeconomic Status, Race/ Ethnicity, and Health Disparities in Children and Adolescents in a Mixed Rural-Urban Community-Olmsted County, Minnesota. Mayo Clin Proc. 2019;94(1):44–53. doi: 10.1016/j.mayocp.2018.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butler AM. Social Determinants of Health and Racial/Ethnic Disparities in Type 2 Diabetes in Youth. Curr Diab Rep. 2017;17(8):60. doi: 10.1007/s11892-017-0885-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elam AR, Lee PP. High-risk populations for vision loss and eye care underutilization: a review of the literature and ideas on moving forward. Surv Ophthalmol. 2013;58(4):348–358. doi: 10.1016/j.survophthal.2012.07.005 [DOI] [PubMed] [Google Scholar]
- 6.Ahmad TR, Kong AW, Turner ML, et al. Socioeconomic Correlates of Keratoconus Severity and Progression. Cornea. 2022. doi: 10.1097/ico.0000000000002993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stormacq C, Van den Broucke S, Wosinski J. Does health literacy mediate the relationship between socioeconomic status and health disparities? Integrative review. Health Promot Int. 2019;34(5):e1–e17. doi: 10.1093/heapro/day062 [DOI] [PubMed] [Google Scholar]
- 8.Hudak DT, Magoon EH. Poverty predicts amblyopia treatment failure. J Aapos. 1997;1(4):214–215. doi: 10.1016/s1091-8531(97) [DOI] [PubMed] [Google Scholar]
- 9.Wang J. Compliance and patching and atropine amblyopia treatments. Vision Res. 2015;114:31–40. doi: 10.1016/j.visres.2015.02.012 [DOI] [PubMed] [Google Scholar]
- 10.Freedman RB, Jones SK, Lin A, Robin AL, Muir KW. Influence of parental health literacy and dosing responsibility on pediatric glaucoma medication adherence. Arch Ophthalmol. 2012;130(3):306–311. doi: 10.1001/archopthalmol.2011.1788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crabtree BF, Miller WL. Doing Qualitative Research. Sage Publications; 1999. [Google Scholar]
- 12.Jandorf S, Krogh Nielsen M, Sørensen K, Sørensen TL. Low health literacy levels in patients with chronic retinal disease. BMC Ophthalmol. 2019;19(1):174. doi: 10.1186/s12886-019-1191-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juzych MS, Randhawa S, Shukairy A, Kaushal P, Gupta A, Shalauta N. Functional health literacy in patients with glaucoma in urban settings. Arch Ophthalmol. 2008;126(5):718–724. doi: 10.1001/archopht.126.5.718 [DOI] [PubMed] [Google Scholar]
- 14.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475 [DOI] [PubMed] [Google Scholar]
- 15.Muir KW, Santiago-Turla C, Stinnett SS, et al. Health literacy and adherence to glaucoma therapy. Am J Ophthalmol. 2006;142(2):223–226. doi: 10.1016/j.ajo.2006.03.018 [DOI] [PubMed] [Google Scholar]
- 16.Baenninger PB, Bachmann LM, Ritzmann M, et al. Do Patients With Keratoconus Have Minimal Disease Knowledge? Cornea. 2021;40(5):624–627. doi: 10.1097/ico.0000000000002501 [DOI] [PubMed] [Google Scholar]
- 17.Sarezky D, Orlin SE, Pan W, VanderBeek BL. Trends in Corneal Transplantation in Keratoconus. Cornea. 2017;36(2):131–137. doi: 10.1097/ico.0000000000001083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Buhr E, Tannen A. Parental health literacy and health knowledge, behaviours and outcomes in children: a cross-sectional survey. BMC Public Health. 2020;20(1):1096. doi: 10.1186/s12889-020-08881-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20(9):800–806. doi: 10.1111/j.1525-1497.2005.0174.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sahebjada S, Chan E, Xie J, Snibson GR, Daniell M, Baird PN. Risk factors and association with severity of keratoconus: the Australian study of Keratoconus. Int Ophthalmol. 2021;41(3):891–899. doi: 10.1007/s10792-020-01644-6 [DOI] [PubMed] [Google Scholar]
- 21.Naderan M, Shoar S, Rezagholizadeh F, Zolfaghari M, Naderan M. Characteristics and associations of keratoconus patients. Cont Lens Anterior Eye. 2015;38(3):199–205. doi: 10.1016/j.clae.2015.01.008 [DOI] [PubMed] [Google Scholar]
- 22.Gordon-Shaag A, Millodot M, Shneor E, Liu Y. The genetic and environmental factors for keratoconus. Biomed Res Int. 2015;2015:795738. doi: 10.1155/2015/795738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arpey NC, Gaglioti AH, Rosenbaum ME. How Socioeconomic Status Affects Patient Perceptions of Health Care: a Qualitative Study. J Prim Care Community Health. 2017;8(3):169–175. doi: 10.1177/2150131917697439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bleacher H, English A, Leblanc W, Dickinson LM. Associations Between Patients’ Unmet Social Needs and Self-Reported Health Confidence at One Primary Care Clinic. J Prim Care Community Health. 2020;11:2150132720921329. doi: 10.1177/2150132720921329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Richardson A, Allen JA, Xiao H, Vallone D. Effects of race/ethnicity and socioeconomic status on health information-seeking, confidence, and trust. J Health Care Poor Underserved. 2012;23(4):1477–1493. doi: 10.1353/hpu.2012.0181 [DOI] [PubMed] [Google Scholar]
- 26.Sinclair M, O’Toole J, Malawaraarachchi M, Leder K. Comparison of response rates and cost-effectiveness for a community-based survey: postal, internet and telephone modes with generic or personalised recruitment approaches. BMC Med Res Methodol. 2012;12:132. doi: 10.1186/1471-2288-12-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leung FH, Savithiri R. Spotlight on focus groups. Can Fam Physician. 2009;55(2):218–219. [PMC free article] [PubMed] [Google Scholar]
- 28.Scott AW, Elam AR, Nwanyanwu K. Addressing Disparities in Eye Care-The Time Is Now. JAMA Ophthalmol. 2021. doi: 10.1001/jamaophthalmol.2021.2053 [DOI] [PubMed] [Google Scholar]