Abstract
The recent description and re-classification of the mesentery as an organ prompted renewed interest in its role in physiological and pathological processes. With an improved understanding of its anatomy, accurately and reliably assessing the mesentery with non-invasive radiological investigation becomes more feasible.
Multi-detector computed tomography is the main radiological modality employed to assess the mesentery due to its speed, widespread availability, and diagnostic accuracy.
Pathologies affecting the mesentery can be classified as primary or secondary mesenteropathies. Primary mesenteropathies originate in the mesentery and subsequently progress to involve other organ systems (e.g., mesenteric ischemia or mesenteric volvulus). Secondary mesenteropathies describe disease processes that originate elsewhere and progress to involve the mesentery with varying degrees of severity (e.g., lymphoma).
The implementation of standardized radiological imaging protocols, nomenclature, and reporting format with regard to the mesentery will be essential in improving the assessment of mesenteric anatomy and various mesenteropathies.
In this article, we describe and illustrate the current state of art in respect of the radiological assessment of the mesentery.
Keywords: mesentery, radiology, organ, mesenteropathy, peritoneum
The recent description of the mesentery as a continuous structure extending from the gastroduodenal junction to the anorectal junction 1 2 contrasts with prior descriptions detailing a fragmented, discontinuous structure and has strengthened the assertion that the mesentery is a distinct organ.
Depictions of the mesentery as a continuous structure extend back to Da Vinci's illustrations in the 15th century and Toldt's publications in the 19th century. 3 The idea that the mesentery is absent or discontinuous in the ascending and descending colon was popularized with the publication of Henry Gray's book “Anatomy, Descriptive and Surgical” in 1858. 4 The concept of multiple mesenteries was further supported by the findings of the well-respected surgeon Sir Frederick Treves in 1885. 5 The emergence of Gray's textbook as a cornerstone of surgical anatomy reference texts helped cement the concept of a discontinuous mesentery (and hence multiple mesenteries) in the minds of radiologists, anatomists, medical educators, and surgeons alike. A proposed explanation of this erroneous description is based on the fact that Toldt's fascia (connective tissue occupying the space between the mesentery and posterior abdominal wall) is extremely thin and consequently not readily identifiable on radiological imaging, intraoperatively or following post cadaveric fixation. 3 These properties led to a perpetuation of the belief in the absence of a mesentery in the left and right mesocolon in normality. Utilizing a prospective observational cohort study design and modern technical advancements (including high resolution laparoscopic imaging). Culligan et al demonstrated that the right and left colon always have adjoining mesentery. 6 These findings were confirmed with subsequent assessment of cadaveric models and with cross-referencing of photographs of cross-sectional cadaveric anatomy with corresponding axial computed tomography (CT) images. 7 8 9
The welcome simplification and clarification of the anatomy of the mesentery has allowed the development of universal nomenclature and terminology in colonic surgery and will likely facilitate a more standardized approach to teaching and research in this area. 10 A standardized radiological approach and reporting nomenclature would logically accompany.
The concept of the mesentery as a distinct organ is supported by its substantive size, mesenteric abnormalities causing disease, 11 successful mesenteric-based treatment strategies, 12 13 ability to logically classify pathologies as primary and secondary mesenteropathies and its contribution to systemic diseases. 14 15 Numerous clinical opportunities will emerge with a more consistent understanding of the mesentery. For example, the assessment of involvement of the mesentery in relation to colonic malignancy is essential 16 and is improved with greater knowledge of the function and anatomy of the mesentery. Also, more accurate understanding of the peritoneal spaces will improve the assessment of the distribution and origin of peritoneal collections. 17
Radiological investigations of the mesentery in normality and diseased states now requires review. Classically, the radiological assessment of the mesentery was considered challenging with limited overall utility in view of the difficulty of correlating the prevailing discontinuous model of the mesentery with radiological findings. 18 The assumption the mesentery is a continuous structure means the task of accurate and consistent radiological characterization of the normal and diseased mesentery becomes more feasible. 8 It has been shown that the sensitivity of CT in identifying the non-diseased mesentery is 75%, 86%, and 88% for the ascending, descending, and sigmoid mesocolons, respectively. 8
To accurately assess a structure on radiological images, a clear understanding of its anatomy and association with adjacent structures is essential. The mesentery extends from the dorsal mesogastrium and mesoduodenum proximally to involve the mesenteric root, small intestinal region of mesentery, the right mesocolon, the left mesocolon, the mesosigmoid and the mesorectum distally. 2 The mesentery is involved in maintaining the position of all of the abdominal digestive organs and achieves this with additional contributions from (1) the peritoneal reflection, (2) the connective tissue termed Toldt's fascia, 19 and (3) from vascular pedicles/entry points of the main vascular supply of the mesentery i.e., superior and inferior mesenteric arteries and veins.
In this review article, we describe and illustrate the current state of radiology of the mesentery.
Radiology of the Mesentery
The mesentery is remotely located in the abdomen. Direct visualization of the mesentery requires surgery, either open, laparoscopic, or robotic. 12 Radiological imaging is a non-invasive method of assessment of the mesentery. It is challenging to routinely and consistently identify normal mesenteric and peritoneal structures using current radiological techniques. However, recent advances in cross-sectional imaging technology, in particular multi-detector CT, have made this task easier. Notwithstanding this, typically a section of mesentery normally becomes conspicuous or a focus of attention only when involved in a pathological process.
Ultrasound (US) has a limited role in the assessment of the mesentery. US is frequently utilized to excellent effect in investigating and treating intrabdominal fluid collections. US can also be used to biopsy mesenteric masses and assess mesenteric vasculature with doppler ultrasound. 20 It provides increased versatility and reduced cost in comparison to CT with the additional benefit of no ionizing radiation being delivered to the patient. However, the quality of images produced is user dependent. Given the inability to image the abdomen as a whole, however, it has limited clinical utility in assessment of the mesentery ( Fig. 1 ).
Fig. 1.
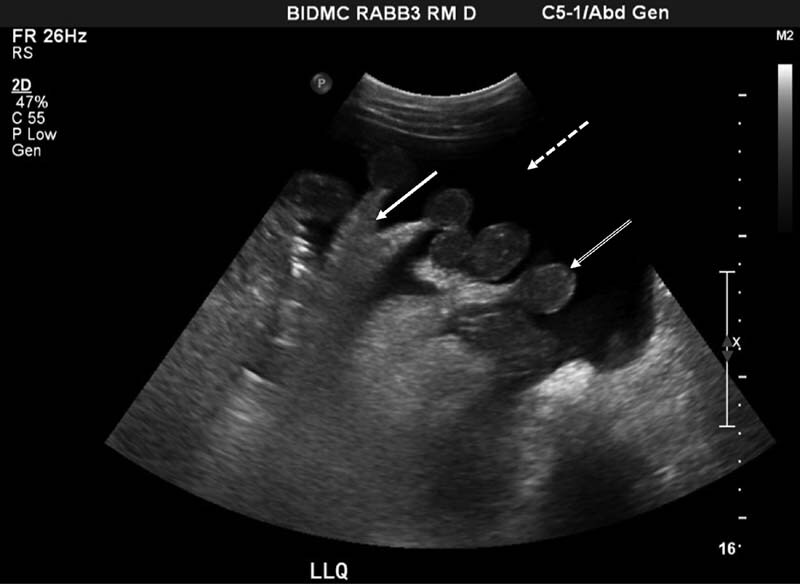
Image depicting ultrasonographic appearance in a patient with intra-abdominal free fluid (dashed arow). The presence of fluid allows the small bowel loops (double line arrow) and associated mesentery (solid arrow) to be clearly identified.
As a result of its availability, speed and diagnostic accuracy multi-detector CT is the most common radiological investigation employed for acute or chronic abdominal pathology. Multi-detector CT provides high-contrast, high-resolution imaging with isotropic voxels allowing multiplanar reconstructions and thus improved ability to interrogate an aspect of anatomy or pathology in detail ( Figs. 2 and 3 ).
Fig. 2.

Photograph depicting the appearance of a coronal section of the abdomen obtained by computerised tomographic (CT) imaging of the abdomen. Intravenous contrast was administered and the CT was viewed in the portal phase. A large volume of intraperitoneal free fluid (double line arrow) is demonstrated. The free fluid delineates fatty and vascular structures of the small bowel region of the mesentery (dashed arrow) and sigmoid region of the mesentery (solid arrow).
Fig. 3.
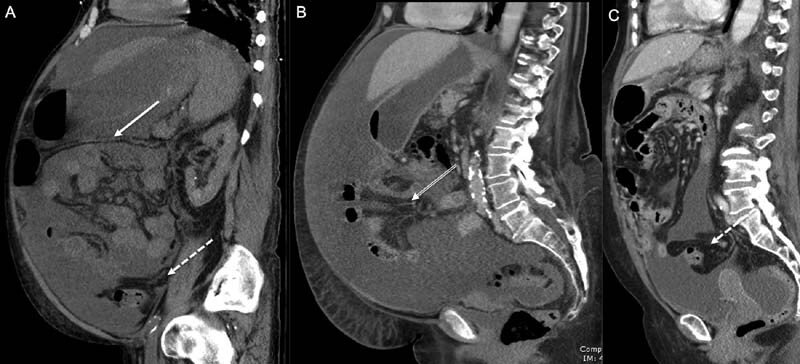
Panel of photographs generated from computerized axial tomographic imaging of the abdomen and pelvis ( A – C ) with intravenous contrast in the portal venous phase. The sagittal aspect of the abdomen is demonstrated showing a large volume of intraperitoneal free fluid. This fluid delineates the transverse mesocolon (solid arrow), small bowel region of the mesentery (double line arrow) and mesosigmoid (dashed arrow).
Magnetic resonance imaging (MRI) is less frequently utilized due to practical limitations. For example, the process of acquiring images in MRI is significantly longer than that of CT and can be difficult for unwell patients to tolerate. Patient motion artifact, bowel gas artifact and ‘chemical shift’ artifact limit the quality of abdominal images. 21 ‘Chemical shift’ artifact refers to fact that the MRI scanner slightly misregisters and subsequently misrepresents the anatomy of closely adherent fat and soft tissue as a result of differences in their chemical constitution. This is particularly unhelpful when one is attempting to assess soft tissue planes ( Fig. 4 ).
Fig. 4.
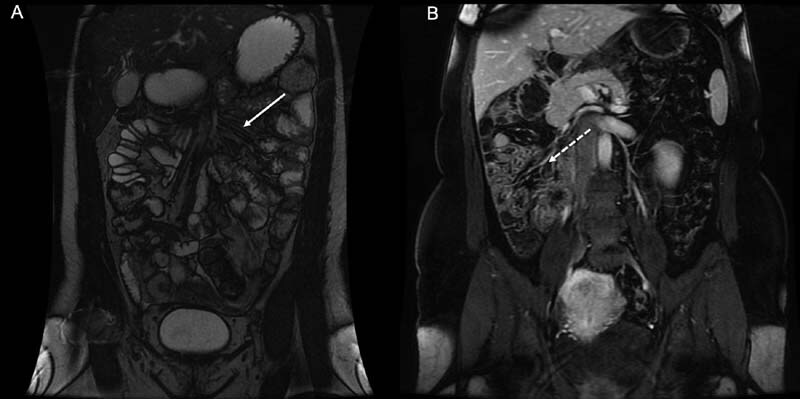
( A ) Photograph of T2 weighted coronal image of the of the abdomen generated from magnetic resonance imaging (MRI). The photograph demonstrates how MRI can be used to depict the anatomy of the small bowel region of the mesentery in normality (solid arrow). ( B ) Photograph of T1 fat-saturated coronal MRI with contrast demonstrating malrotation; the small bowel and adjoining mesentery are located on the right side of the abdomen (dashed arrow).
Angiography of the mesenteric vessels has been effectively employed utilizing digital subtraction techniques, CT and MRI. Positron emission tomography/CT (PET/CT) is frequently utilized in oncological imaging and has demonstrated good sensitivity in the detection of mesenteric involvement of disease. 22
“Mesenteropathies” or diseases relating to the mesentery can be classified as primary (originating in the mesentery and may, in turn, involve other organs) and secondary (extending to involve the mesentery from an initial pathological process in another organ or organ system). Mesenteropathies are receiving renewed interest as a result of the reclassification of the mesentery as a distinct organ.
Primary Mesenteropathies
Mesenteric Ischemia
Mesenteric ischemia refers to both acute and chronic conditions that result in inadequate blood supply to the intestines. Acute mesenteric ischemia is an uncommon but critical condition that requires urgent investigation and treatment as a result of a significant associated morbidity and mortality. 23 The vast majority of acute mesenteric ischemia is a result of vascular occlusion 24 and principally involves the superior mesenteric artery as a result of its anatomical orientation. Other causes of acute ischemia include low flow states secondary to trauma or cardiogenic shock. 25
While having good specificity, ultrasound examination has suboptimal sensitivity for mesenteric ischemia and has a limited role in modern radiological assessment of mesenteric ischemia. The investigation of choice is CT angiography 26 which is more widely available and less invasive than formal catheter directed fluoroscopic angiography. It also allows assessment of the intestine for secondary signs of ischemia while facilitating alternative diagnoses in a patient with an acute abdomen. 27 28 Pertinent radiological findings include filling defects in the lumen of the vessel, focal low density (hypoattenuation) in the bowel wall, a segment of bowel wall thickening, peri-colonic fat stranding, pneumatosis intestinalis and portal venous gas that is typically identified in the periphery of the liver. High signal (hyperattenuation) of the bowel wall can also be seen as a result of localized hyperemia. Identifying a combination of these findings allows the reporting radiologist to have more confidence in the diagnosis of acute mesenteric ischemia. Magnetic resonance angiography (MRA) is being increasingly utilized in the assessment of mesenteric ischemia and has been shown to be quite sensitive and specific in the assessment of proximal occlusions or stenoses in the main mesenteric arteries however this imaging modality is limited in its ability to identify distal pathology. 29 30 As a result of the time penalty incurred by an MRI examination, it has limited utility in the assessment of the acute abdomen. Animal-based studies have investigated the possible role of PET/CT in the assessment of acute mesenteric ischemia by imaging the reduction in blood flow in the liver as a result of acute mesenteric ischemia and have prompted exploration of its potential for clinical use. 31
Malrotation/Non Rotation and Volvulus
Malrotation occurs when the normal embryological development and positioning of the large and small bowel in the abdominal cavity is arrested. This can result in failure of the mesentery of the right colon to correctly adhere to the posterior abdominal wall. This condition does not always present pathologically and is commonly identified incidentally on CT imaging. 32 Radiological findings of malrotation include abnormal positioning of the small bowel and associated mesentery on the right side of the abdominal cavity, failure of the third part of the duodenum to cross the midline and abnormal anatomical orientation of the superior mesenteric artery and superior mesenteric vein. 33 Upper gastrointestinal barium studies and barium enemas have classically been utilized to investigate malrotation and are utilized to particularly good effect in the pediatric population. In current practice, CT is increasingly the examination of choice in adults. 33
Failure of the correct fixation of the mesentery allows the intestine to be more mobile than normal and can predispose the patient to intestinal volvulus. Volvulus has a characteristic appearance on CT imaging and is readily diagnosed with identification of a twisted vascular pedicle (“vascular whirl sign”) ( Fig. 5 ), tapering of the intestinal lumen to the obstruction point (“bird beak sign”) and associated bowel obstruction. Large bowel volvulus is a primary mesenteropathy that is potentially life-threatening and is thus a surgical emergency.
Fig. 5.
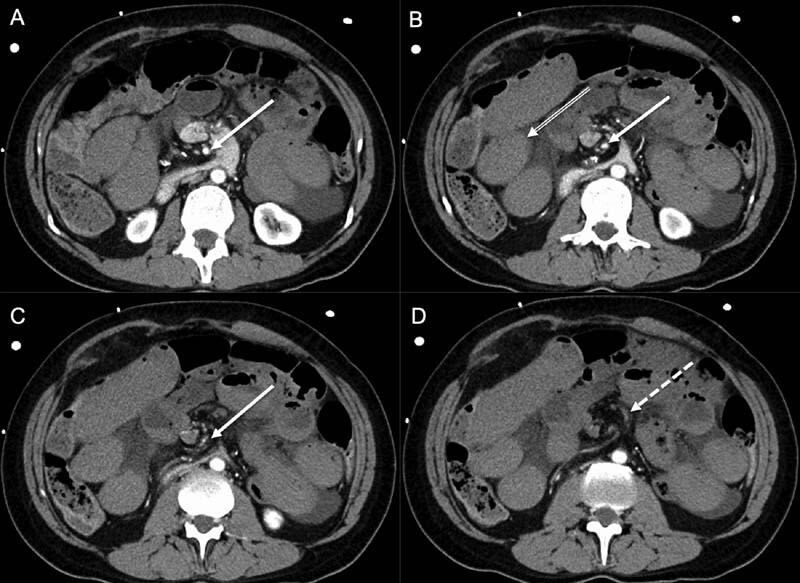
Panel of photographs generated from computerised axial tomographic imaging of the abdomen and pelvis ( A – D ). Intravenous contrast was administered and axial images were taken in the arterial phase. The images progress cranio-caudally to demonstrate the superior mesenteric artery (solid arrow) in the mesentery adjoining the small bowel. The superior mesenteric artery is occluded by a mesenteric volvulus. These properties collectively result in the “vascular whirl” sign (dashed arrow). There is hypoattenuation of the small bowel wall (double line arrow) indicating small bowel ischemia.
Sclerosing Mesenteritis
A rare disease of unknown cause, sclerosing mesenteritis characteristically presents with chronic inflammation of the mesentery. 34 It preferentially involves the region of the mesentery adjoining the small bowel over that adjoining the large bowel. 35 36 Proposed pathogenesis of this condition include autoimmune causes, trauma, infection, and ischemia. 37 38 CT is the imaging modality of choice and imaging findings can vary from subtle hyperattenuation in the mesentery to a focal distinct soft tissue mass. The most common finding is that of a soft tissue mass in the region of the mesentery adjoining the small bowel with the adjacent bowel wall typically not involved. The mass can involve mesenteric vasculature and develop collaterals. Fat around the mesenteric vasculature is preserved and produces the “fat ring sign,” which is specific for sclerosing mesenteritis. This can help distinguish sclerosing mesenteritis from other pathologies such as lymphoma or carcinomatosis. 39 Calcification and cystic change can be present in the mesentery secondary to necrosis and lymphatic obstruction, respectively. 40 41 Mesenteric panniculitis is a term utilized for a primarily chronic inflammatory process but is considered within the spectrum of sclerosing mesenteritis. The combination of hyperattenuation of the mesentery with associated small lymph nodes, and the absence of a discrete soft tissue mass generates an appearance termed “misty mesentery.” The “misty mesentery” is not specific to mesenteric panniculitis; hyperattenuation of the mesentery also occurs in lymphoma, hemorrhage or localized edema. 42 43 Although biopsy is required to confirm sclerosing mesenteritis, radiological characteristics that can be useful in guiding the differential diagnosis; lymphoma does not cause mesenteric vascular compromise and does not demonstrate calcification.
Peritoneal Mesothelioma
The peritoneum is a mesothelium supported by a connective tissue base of variable thickness. 44 The parietal peritoneum lines the free surface of the non-mesenteric domain of the abdomen. 44 Visceral peritoneum lines the free surface of organs of the mesenteric domain of the abdomen (including the mesentery). 44 The peritoneal reflection is the mesothelial junction between the parietal and visceral components of the peritoneum and its various anatomical modifications are termed ligaments, folds, reflections and membranes. 44 Peritoneal mesothelioma can arise anywhere along the continuum of the parietal, visceral peritoneum and the reflection. It can thus arise in association with the mesentery.
Mesothelioma is a rare malignancy that develops on serosal membranes and is most commonly associated with the pleural space but can also involve the peritoneal space, including the mesentery. Peritoneal mesothelioma can be divided into subgroups including malignant and cystic mesothelioma and can have a varied radiological appearance. 45
With regard to malignant mesothelioma, occupational asbestos exposure is a large contributing factor and this disease is typically identified in males in their fifth to sixth decade of life. 46 As a result of the vague abdominal symptoms associated with peritoneal mesothelioma, presentation is typically late with advanced disease and poor prognosis.
Overall, CT characteristics range from ‘dry’ peritoneal masses to ‘wet’ ascites associated with peritoneal nodularity and omental masses. In contrast to the more common pleural based disease, calcification is rarely a feature of peritoneal mesothelioma. 47 Peritoneal mesothelioma is a diagnosis of exclusion and can be difficult to distinguish from other peritoneal diseases that involve mesenteric soft tissue masses such as peritoneal carcinomatosis, lymphomatosis and tuberculosis. Prior history of asbestos exposure, absence of liver metastases and low volume of ascites in comparison to the level of peritoneal disease can all help guide the diagnosis to peritoneal mesothelioma of the mesentery. 48 In contrast, cystic mesothelioma presents in middle-aged females with a history of prior abdominal surgery or pelvic inflammatory disease and is not associated with asbestos exposure. 49 Imaging features consist of a unilocular or multilocular cystic mass and typically primarily involves the pelvis. Cystic mesothelioma is considered a benign condition, although malignant transformation has been described. 50
Mesenteric Hematoma
A spontaneous mesenteric hematoma is a rare condition that has been described infrequently in the literature. 51 This occurs when active mesenteric hemorrhage or a cause for hemorrhage cannot be identified on CT or formal catheter directed angiography. The patient can be managed conservatively if clinically stable. 52
Crohn's Disease
A role of the mesentery in Crohn's disease has been proposed and is subject to some debate. It has been postulated that, contrary to conventional theories, Crohn's disease may be a primary mesenteropathy and that intestinal involvement is the end-result of disease progression from the mesentery. Desreumaux et al demonstrated that mesenteric changes can be identified radiologically prior to any appreciable intestinal pathology in early Crohn's disease. 15 Recent studies have shown that partial or complete resection of the mesentery in addition to the intestinal resection has significantly reduced rates of recurrence requiring operation and allowed a shorter length of bowel to be resected. 12 In classical surgery for Crohn's disease, the intestine was normally amputated at its junction with the mesentery and the mesentery was retained. In April 2020, Guglielmo et al published a consensus statement on preferred radiological reporting descriptions and terminology with MRI and CT enterography for Crohn's disease of the small bowel. 53 They highlighted mesenteric findings associated with Crohn's disease as being an essential part of any radiological report. Peri-enteric inflammation, engorged vasa recta or “comb sign,” 54 fibrofatty infiltration, 55 mesenteric venous thrombosis and lymphadenopathy are the key mesenteric findings in the radiological assessment of small bowel Crohn's disease. Adopting standardised reporting nomenclature will promote consistent and reliable assessment of the mesentery in Crohn's disease and many other mesenteropathies. 56
Secondary Mesenteropathies
Lymphomatosis/Carcinomatosis
Peritoneal lymphomatosis refers to the intraperitoneal spread of lymphoma. Approximately 40% of lymphoma patients will develop extra-nodal involvement with an associated overall poorer prognosis. 57 Characteristic CT findings include caking of the omental region of the mesentery with homogenous bulky lesions and smooth homogenous infiltration ( Fig. 6 ) of the peritoneum can also be seen. There can also be small nodules with subtle localized infiltration with a characteristic “smudged” appearance. Diffusely distributed enlarged mesenteric lymph nodes and intestinal involvement are typical of lymphomatosis. 58
Fig. 6.
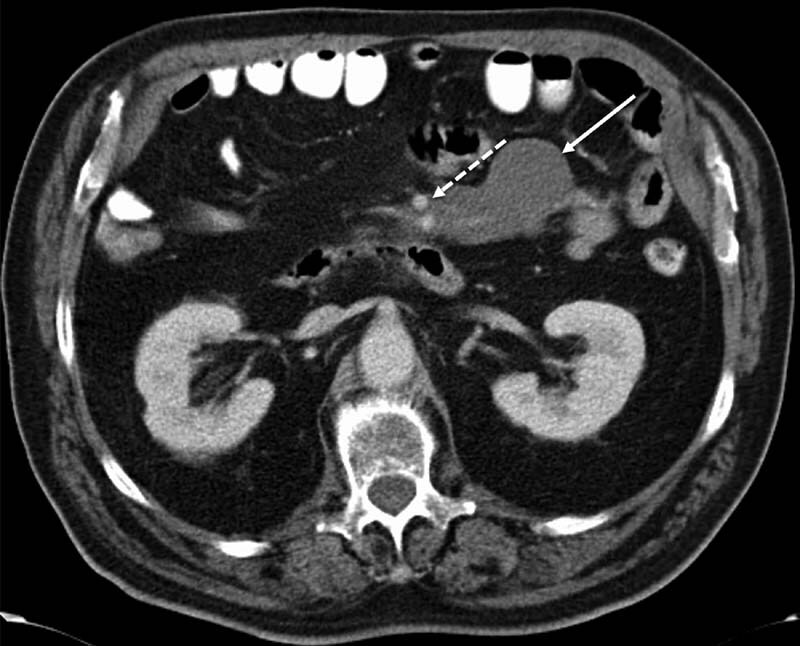
Photograph depicting the axial appearance of the abdomen obtained by computerised tomographic (CT) imaging. Intravenous contrast was administered and the CT was viewed in the portal phase. The image includes a well-defined smooth homogenous soft tissue mass (solid arrow) in the mesentery adjoining the small bowel mesentery that encases but does not occlude the mesenteric vasculature (dashed arrow). These appearances are consistent with mesenteric lymphoma.
Peritoneal deposition of carcinoma metastasis is a well-documented pathogenesis and typically arises from a gastric, colonic or ovarian source. 59 Differentiating carcinomatosis from lymphomatosis can be challenging. Carcinomatosis, in contrast to lymphomatosis, is normally associated with localized (rather than diffuse) lymphadenopathy as well as moderate to large volume ascites. 60
Pseudomyxoma Peritonei
Pseudomyxoma peritonei is a very rare presentation of a secondary mesenteropathy that develops from a low grade mucinous carcinoma of the appendix and that that progresses to involve the peritoneal cavity. 61 It is characterized by the presence of a thick mucinous fluid in the peritoneal cavity and mucinous deposits on the peritoneum. The mucinous fluid has a low attenuation on CT with occasional soft tissue tumor deposits or compressed mesentery presenting as regions of increased attenuation in the fluid. 62 Scalloping of visceral surfaces of the intra-abdominal organs (including the mesentery) is a key radiological finding that is helpful in differentiating pseudomyxoma peritonei from simple ascites. Scalloping is normally most noticeable at the surface of the liver and spleen. 57
Tuberculosis
The abdomen is the most common site of extrapulmonary tuberculosis (TB) with the mesentery being the most common intra-abdominal site of disease. 63 Spread of TB occurs either through involvement and subsequent rupture of mesenteric lymph nodes, or hematogenously, or by direct invasion. 64 CT findings include ascites, contrast enhancing smooth peritoneal thickening, mesenteric fat stranding and necrotic or calcified lymph nodes. 64 Radiological abnormalities in carcinomatosis often have a nodular, irregular pattern while those associated with tuberculosis are more smoothly contoured. Intra-abdominal lymph node involvement is not commonly associated with the peritoneal form of tuberculosis. 65
Conclusion
Historically the mesentery has been largely side-lined and received little overall attention. With the recognition of the mesentery as a distinct organ, a more central role in physiology and pathology can be proposed. From a radiological perspective this will require the establishment of dedicated imaging protocols for various imaging modalities, adoption of standard nomenclature and report formatting and re-education regarding the correct anatomy of the mesentery (and associated structures such as the peritoneum). CT is by far the most common and currently most useful imaging modality in use but there is significant potential for MRI and PET/CT in imaging and characterizing mesenteric abnormalities. The direction of future radiological research will be greatly assisted by a multidisciplinary approach and in turn will likely prove significantly beneficial to advance patient care.
Conflict of Interest None declared.
Abbreviations
CTcomputed tomography
USultrasound
MRImagnetic resonance imaging
PETpositron emission tomography
MRAmagnetic resonance angiography
References
- 1.Coffey J C, O'Leary D P. The mesentery: structure, function, and role in disease. Lancet Gastroenterol Hepatol. 2016;1(03):238–247. doi: 10.1016/S2468-1253(16)30026-7. [DOI] [PubMed] [Google Scholar]
- 2.Byrnes K G, Walsh D, Dockery P, McDermott K, Coffey J C. Anatomy of the mesentery: Current understanding and mechanisms of attachment. Semin Cell Dev Biol. 2019;92:12–17. doi: 10.1016/j.semcdb.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 3.Byrnes K G, Walsh D, Lewton-Brain P, McDermott K, Coffey J C. Anatomy of the mesentery: Historical development and recent advances. Semin Cell Dev Biol. 2019;92:4–11. doi: 10.1016/j.semcdb.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Gray H. John W. Parker and Son; 1858. Anatomy, Descriptive and Surgical. [Google Scholar]
- 5.Treves F.Lectures on the anatomy of the intestinal canal and peritoneum in man BMJ 18851(1264):580–583. 10.1136/bmj.1.1264.580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Culligan K, Coffey J C, Kiran R P, Kalady M, Lavery I C, Remzi F H.The mesocolon: a prospective observational study Colorectal Dis 20121404421–428., discussion 428–430. Doi: 10.1111/j.1463-1318.2012.02935.x [DOI] [PubMed] [Google Scholar]
- 7.Culligan K, Walsh S, Dunne C. The mesocolon: a histological and electron microscopic characterization of the mesenteric attachment of the colon prior to and after surgical mobilization. Ann Surg. 2014;260(06):1048–1056. doi: 10.1097/SLA.0000000000000323. [DOI] [PubMed] [Google Scholar]
- 8.Coffey J C, Culligan K, Walsh L G. An appraisal of the computed axial tomographic appearance of the human mesentery based on mesenteric contiguity from the duodenojejunal flexure to the mesorectal level. Eur Radiol. 2016;26(03):714–721. doi: 10.1007/s00330-015-3883-0. [DOI] [PubMed] [Google Scholar]
- 9.Spitzer V, Ackerman M J, Scherzinger A L, Whitlock D. The visible human male: a technical report. J Am Med Inform Assoc. 1996;3(02):118–130. doi: 10.1136/jamia.1996.96236280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coffey J C, Sehgal R, Culligan K. Terminology and nomenclature in colonic surgery: universal application of a rule-based approach derived from updates on mesenteric anatomy. Tech Coloproctol. 2014;18(09):789–794. doi: 10.1007/s10151-014-1184-2. [DOI] [PubMed] [Google Scholar]
- 11.Osiro S B, Cunningham D, Shoja M M, Tubbs R S, Gielecki J, Loukas M. The twisted colon: a review of sigmoid volvulus. Am Surg. 2012;78(03):271–279. [PubMed] [Google Scholar]
- 12.Coffey J C, O'Leary D P, Kiernan M G, Faul P. The mesentery in Crohn's disease: friend or foe? Curr Opin Gastroenterol. 2016;32(04):267–273. doi: 10.1097/MOG.0000000000000280. [DOI] [PubMed] [Google Scholar]
- 13.Coffey J C, Dillon M, Sehgal R. Mesenteric-based surgery exploits gastrointestinal, peritoneal, mesenteric and fascial continuity from duodenojejunal flexure to the anorectal junction–a review. Dig Surg. 2015;32(04):291–300. doi: 10.1159/000431365. [DOI] [PubMed] [Google Scholar]
- 14.Tracy R P. Is visceral adiposity the “enemy within”? Arterioscler Thromb Vasc Biol. 2001;21(06):881–883. doi: 10.1161/01.atv.21.6.881. [DOI] [PubMed] [Google Scholar]
- 15.Desreumaux P, Ernst O, Geboes K. Inflammatory alterations in mesenteric adipose tissue in Crohn's disease. Gastroenterology. 1999;117(01):73–81. doi: 10.1016/s0016-5085(99)70552-4. [DOI] [PubMed] [Google Scholar]
- 16.Dighe S, Purkayastha S, Swift I. Diagnostic precision of CT in local staging of colon cancers: a meta-analysis. Clin Radiol. 2010;65(09):708–719. doi: 10.1016/j.crad.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 17.Koo B C, Chinogureyi A, Shaw A S. Imaging acute pancreatitis. Br J Radiol. 2010;83(986):104–112. doi: 10.1259/bjr/13359269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dodds W J, Darweesh R M, Lawson T L. The retroperitoneal spaces revisited. AJR Am J Roentgenol. 1986;147(06):1155–1161. doi: 10.2214/ajr.147.6.1155. [DOI] [PubMed] [Google Scholar]
- 19.Stecco C, Sfriso M M, Porzionato A. Microscopic anatomy of the visceral fasciae. J Anat. 2017;231(01):121–128. doi: 10.1111/joa.12617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Esteban J M, Maldonado L, Sanchiz V, Minguez M, Benages A. Activity of Crohn's disease assessed by colour Doppler ultrasound analysis of the affected loops. Eur Radiol. 2001;11(08):1423–1428. doi: 10.1007/s003300000770. [DOI] [PubMed] [Google Scholar]
- 21.Akisik F M, Sandrasegaran K, Aisen A M, Lin C, Lall C.Abdominal MR imaging at 3.0 T Radiographics 200727051433–1444., discussion 1462–1464. Doi: 10.1148/rg.275075023 [DOI] [PubMed] [Google Scholar]
- 22.Satoh Y, Ichikawa T, Motosugi U. Diagnosis of peritoneal dissemination: comparison of 18F-FDG PET/CT, diffusion-weighted MRI, and contrast-enhanced MDCT. AJR Am J Roentgenol. 2011;196(02):447–453. doi: 10.2214/AJR.10.4687. [DOI] [PubMed] [Google Scholar]
- 23.Herbert G S, Steele S R. Acute and chronic mesenteric ischemia. Surg Clin North Am. 2007;87(05):1115–1134, ix. doi: 10.1016/j.suc.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 24.Bradbury A W, Brittenden J, McBride K, Ruckley C V. Mesenteric ischaemia: a multidisciplinary approach. Br J Surg. 1995;82(11):1446–1459. doi: 10.1002/bjs.1800821105. [DOI] [PubMed] [Google Scholar]
- 25.Patel T, Kuladhipati I, Shah S. Successful percutaneous endovascular management of acute post-traumatic superior mesenteric artery dissection using a transradial approach. J Invasive Cardiol. 2010;22(04):E61–E64. [PubMed] [Google Scholar]
- 26.Oliva I B, Davarpanah A H, Rybicki F J. ACR Appropriateness Criteria ® imaging of mesenteric ischemia. Abdom Imaging. 2013;38(04):714–719. doi: 10.1007/s00261-012-9975-2. [DOI] [PubMed] [Google Scholar]
- 27.Shih M C, Angle J F, Leung D A. CTA and MRA in mesenteric ischemia: part 2, Normal findings and complications after surgical and endovascular treatment. AJR Am J Roentgenol. 2007;188(02):462–471. doi: 10.2214/AJR.05.1168. [DOI] [PubMed] [Google Scholar]
- 28.Shih M C, Hagspiel K D. CTA and MRA in mesenteric ischemia: part 1, Role in diagnosis and differential diagnosis. AJR Am J Roentgenol. 2007;188(02):452–461. doi: 10.2214/AJR.05.1167. [DOI] [PubMed] [Google Scholar]
- 29.Meaney J F. Non-invasive evaluation of the visceral arteries with magnetic resonance angiography. Eur Radiol. 1999;9(07):1267–1276. doi: 10.1007/s003300050833. [DOI] [PubMed] [Google Scholar]
- 30.Meaney J F, Prince M R, Nostrant T T, Stanley J C. Gadolinium-enhanced MR angiography of visceral arteries in patients with suspected chronic mesenteric ischemia. J Magn Reson Imaging. 1997;7(01):171–176. doi: 10.1002/jmri.1880070126. [DOI] [PubMed] [Google Scholar]
- 31.Kiss J, Naum A, Kudomi N. Non-invasive diagnosis of acute mesenteric ischaemia using PET. Eur J Nucl Med Mol Imaging. 2009;36(08):1338–1345. doi: 10.1007/s00259-009-1094-0. [DOI] [PubMed] [Google Scholar]
- 32.Zissin R, Rathaus V, Oscadchy A, Kots E, Gayer G, Shapiro-Feinberg M. Intestinal malrotation as an incidental finding on CT in adults. Abdom Imaging. 1999;24(06):550–555. doi: 10.1007/s002619900560. [DOI] [PubMed] [Google Scholar]
- 33.Pickhardt P J, Bhalla S. Intestinal malrotation in adolescents and adults: spectrum of clinical and imaging features. Am J Roentgenol. 2002;179(06):1429–1435. doi: 10.2214/ajr.179.6.1791429. [DOI] [PubMed] [Google Scholar]
- 34.Lawler L P, McCarthy D M, Fishman E K, Hruban R. Sclerosing mesenteritis: depiction by multidetector CT and three-dimensional volume rendering. Am J Roentgenol. 2002;178(01):97–99. doi: 10.2214/ajr.178.1.1780097. [DOI] [PubMed] [Google Scholar]
- 35.Sabaté J M, Torrubia S, Maideu J, Franquet T, Monill J M, Pérez C. Sclerosing mesenteritis: imaging findings in 17 patients. Am J Roentgenol. 1999;172(03):625–629. doi: 10.2214/ajr.172.3.10063848. [DOI] [PubMed] [Google Scholar]
- 36.Pérez-Fontán F J, Soler R, Sanchez J, Iglesias P, Sanjurjo P, Ruiz J. Retractile mesenteritis involving the colon: barium enema, sonographic, and CT findings. Am J Roentgenol. 1986;147(05):937–940. doi: 10.2214/ajr.147.5.937. [DOI] [PubMed] [Google Scholar]
- 37.Katz M E, Heiken J P, Glazer H S, Lee J K. Intraabdominal panniculitis: clinical, radiographic, and CT features. Am J Roentgenol. 1985;145(02):293–296. doi: 10.2214/ajr.145.2.293. [DOI] [PubMed] [Google Scholar]
- 38.Durst A L, Yarom R, Luttwak E M. Malignant fibromatous peritoneal mesothelioma associated with liposclerotic mesenteritis. Am J Gastroenterol. 1971;55(05):477–481. [PubMed] [Google Scholar]
- 39.Zhang P, Dyer R B. The “fat ring” sign of sclerosing mesenteritis. Abdom Radiol (NY) 2018;43(07):1839–1840. doi: 10.1007/s00261-017-1353-7. [DOI] [PubMed] [Google Scholar]
- 40.Johnson L A, Longacre T A, Wharton K A, Jr, Jeffrey R B. Multiple mesenteric lymphatic cysts: an unusual feature of mesenteric panniculitis (sclerosing mesenteritis) J Comput Assist Tomogr. 1997;21(01):103–105. doi: 10.1097/00004728-199701000-00019. [DOI] [PubMed] [Google Scholar]
- 41.Mata J M, Inaraja L, Martin J, Olazabal A, Castilla M T. CT features of mesenteric panniculitis. J Comput Assist Tomogr. 1987;11(06):1021–1023. doi: 10.1097/00004728-198711000-00018. [DOI] [PubMed] [Google Scholar]
- 42.Seo B K, Ha H K, Kim A Y. Segmental misty mesentery: analysis of CT features and primary causes. Radiology. 2003;226(01):86–94. doi: 10.1148/radiol.2261011547. [DOI] [PubMed] [Google Scholar]
- 43.Mindelzun R E, Jeffrey R B, Jr, Lane M J, Silverman P M. The misty mesentery on CT: differential diagnosis. Am J Roentgenol. 1996;167(01):61–65. doi: 10.2214/ajr.167.1.8659422. [DOI] [PubMed] [Google Scholar]
- 44.Gray H. Elsevier; 2020. Gray's Anatomy, The Anatomical Basis of Clinical Practice. 42nd ed; p. 1606. [Google Scholar]
- 45.Hassan R, Alexander R. Nonpleural mesotheliomas: mesothelioma of the peritoneum, tunica vaginalis, and pericardium. Hematol Oncol Clin North Am. 2005;19(06):1067–1087, vi. doi: 10.1016/j.hoc.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 46.Armed Forces Institute of Pathology . Busch J M, Kruskal J B, Wu B. Best cases from the AFIP. Malignant peritoneal mesothelioma. Radiographics. 2002;22(06):1511–1515. doi: 10.1148/rg.226025125. [DOI] [PubMed] [Google Scholar]
- 47.Pickhardt P J, Bhalla S. Primary neoplasms of peritoneal and sub-peritoneal origin: CT findings. Radiographics. 2005;25(04):983–995. doi: 10.1148/rg.254045140. [DOI] [PubMed] [Google Scholar]
- 48.Park J Y, Kim K W, Kwon H J. Peritoneal mesotheliomas: clinicopathologic features, CT findings, and differential diagnosis. Am J Roentgenol. 2008;191(03):814–825. doi: 10.2214/AJR.07.3628. [DOI] [PubMed] [Google Scholar]
- 49.Weiss S W, Tavassoli F A. Multicystic mesothelioma. An analysis of pathologic findings and biologic behavior in 37 cases. Am J Surg Pathol. 1988;12(10):737–746. [PubMed] [Google Scholar]
- 50.González-Moreno S, Yan H, Alcorn K W, Sugarbaker P H. Malignant transformation of “benign” cystic mesothelioma of the peritoneum. J Surg Oncol. 2002;79(04):243–251. doi: 10.1002/jso.10081. [DOI] [PubMed] [Google Scholar]
- 51.Carr S R, Dinsmore R C, Wilkinson N W. Idiopathic spontaneous intraperitoneal hemorrhage: a clinical update on abdominal apoplexy in the year 2001. Am Surg. 2001;67(04):374–376. [PubMed] [Google Scholar]
- 52.Parker S G, Thompson J N. Spontaneous mesenteric haematoma; diagnosis and management. BMJ Case Rep. 2012;2012:bcr2012006624. doi: 10.1136/bcr-2012-006624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Guglielmo F F, Anupindi S A, Fletcher J G. Small bowel Crohn disease at CT and MR enterography: imaging atlas and glossary of terms. Radiographics. 2020;40(02):354–375. doi: 10.1148/rg.2020190091. [DOI] [PubMed] [Google Scholar]
- 54.Meyers M A, McGuire P V. Spiral CT demonstration of hypervascularity in Crohn disease: “vascular jejunization of the ileum” or the “comb sign”. Abdom Imaging. 1995;20(04):327–332. doi: 10.1007/BF00203365. [DOI] [PubMed] [Google Scholar]
- 55.Koh D M, Miao Y, Chinn R J. MR imaging evaluation of the activity of Crohn's disease. AJR Am J Roentgenol. 2001;177(06):1325–1332. doi: 10.2214/ajr.177.6.1771325. [DOI] [PubMed] [Google Scholar]
- 56.Stenosis Therapy and Anti-Fibrotic Research (STAR) Consortium. . Bettenworth D, Bokemeyer A, Baker M. Assessment of Crohn's disease-associated small bowel strictures and fibrosis on cross-sectional imaging: a systematic review. Gut. 2019;68(06):1115–1126. doi: 10.1136/gutjnl-2018-318081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Seshul M B, Coulam C M. Pseudomyxoma peritonei: computed tomography and sonography. AJR Am J Roentgenol. 1981;136(04):803–806. doi: 10.2214/ajr.136.4.803. [DOI] [PubMed] [Google Scholar]
- 58.Kim Y, Cho O, Song S, Lee H, Rhim H, Koh B. Peritoneal lymphomatosis: CT findings. Abdom Imaging. 1998;23(01):87–90. doi: 10.1007/s002619900292. [DOI] [PubMed] [Google Scholar]
- 59.Karaosmanoglu D, Karcaaltincaba M, Oguz B, Akata D, Ozmen M, Akhan O. CT findings of lymphoma with peritoneal, omental and mesenteric involvement: peritoneal lymphomatosis. Eur J Radiol. 2009;71(02):313–317. doi: 10.1016/j.ejrad.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 60.Yoo E, Kim J H, Kim M J. Greater and lesser omenta: normal anatomy and pathologic processes. Radiographics. 2007;27(03):707–720. doi: 10.1148/rg.273065085. [DOI] [PubMed] [Google Scholar]
- 61.Pai R K, Longacre T A. Pseudomyxoma peritonei syndrome: classification of appendiceal mucinous tumours. Cancer Treat Res. 2007;134:71–107. doi: 10.1007/978-0-387-48993-3_5. [DOI] [PubMed] [Google Scholar]
- 62.Sulkin T V, O'Neill H, Amin A I, Moran B. CT in pseudomyxoma peritonei: a review of 17 cases. Clin Radiol. 2002;57(07):608–613. doi: 10.1053/crad.2002.0942. [DOI] [PubMed] [Google Scholar]
- 63.Sinan T, Sheikh M, Ramadan S, Sahwney S, Behbehani A. CT features in abdominal tuberculosis: 20 years experience. BMC Med Imaging. 2002;2(01):3. doi: 10.1186/1471-2342-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Epstein B M, Mann J H. CT of abdominal tuberculosis. AJR Am J Roentgenol. 1982;139(05):861–866. doi: 10.2214/ajr.139.5.861. [DOI] [PubMed] [Google Scholar]
- 65.Pereira J M, Madureira A J, Vieira A, Ramos I. Abdominal tuberculosis: imaging features. Eur J Radiol. 2005;55(02):173–180. doi: 10.1016/j.ejrad.2005.04.015. [DOI] [PubMed] [Google Scholar]


