Abstract
Background
The opioid epidemic worsened during the coronavirus disease 2019 (COVID-19) pandemic. Synthetic opioids (primarily fentanyl) comprise the most common drugs involved in overdose (OD) death. A vaccine that blocks fentanyl from reaching the brain to prevent OD is under development, and insight is needed into its acceptability.
Methods
Using a semi-structured interview guide, persons with opioid use disorder (OUD), family, professionals, and the public were interviewed about attitudes and concerns regarding a fentanyl vaccine. Reactions to fictional clinical vignettes of persons at risk of OUD because of pain and/or substance use histories were collected, analyzed, and quantified for favorability. Interviews were transcribed, coded, and analyzed thematically.
Results
Among N = 64 participants, (70.3% female, average age 32.4 years), attitudes were favorable toward a fentanyl vaccine, with preference for lifelong durability (76% of n = 55 asked). Perceived benefits centered on the potential for a life-saving intervention, suffering averted, healthcare dollars saved, and the utility of a passive harm reduction strategy. Concerns centered on uncertainty regarding vaccine safety, questions about efficacy, worry about implications for future pain management, stigma, and need for supportive counseling and guidance to personalize decision making. Reactions to vignettes revealed complex attitudes toward fentanyl vaccination when considering recipient age, health history, and future risks for addiction and pain.
Conclusions
Positive responses to a fentanyl vaccine were found along with appreciation for the complexity of a vaccine strategy to prevent OD in the setting of pain and uncertain durability. Further research is needed to elucidate operational, ethical, and communications strategies to advance the model.
Keywords: opioid overdose, opioid use disorder, fentanyl vaccine, acceptability, harm reduction
Persons with opioid use disorder and members of the public shared positive attitudes toward a fentanyl vaccine to block overdose, and identified concerns regarding stigma, pain management, and uncertain durability. Findings suggest need for concerted attention to implementation and communications.
Prior to the coronavirus disease 2019 (COVID-19) pandemic, overdose had become the most common cause of death for Americans under 50 years of age [1], and overdose deaths drove decreases in US life expectancy throughout the previous decade [2]. From 1999 to 2021 there were more than 570 000 opioid overdose deaths in the United States [3, 4]. Synthetic opioids (primarily fentanyl) are the most common drugs involved in overdose death [5], and in 2019, they were implicated in more than half of total lethal overdoses [6]. Fatal overdoses have soared during the COVID-19 pandemic, with more than 100 000 overdose deaths from 2020 to 2021 [3], and fentanyl overdose has become the leading cause of death for US adults ages 18–45 years [7]. Efforts to address the overdose crisis have been complicated by the pandemic’s effects on public health and healthcare systems. Rising OD mortality indicates that new efforts to reduce overdose are needed, to complement existing controls [8].
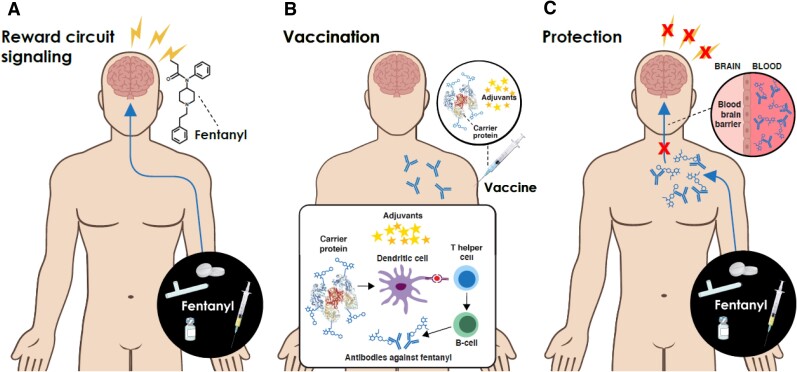
Along with provision of clean drinking water and prudent use of antibiotics, vaccines are the most impactful global public health intervention and are highly effective at reducing morbidity and mortality from infectious disease (ID) [9]. In contrast to well established practices for using vaccines to prevent infectious disease, and proposed therapeutic use of vaccines to treat cancers, vaccination to address behavioral health issues is comparatively rare [10, 11] and public awareness of these efforts is likely minimal. Nevertheless, important efforts are underway to advance a vaccine model to prevent behavioral health issues [12–14]. Under the Helping to End Addiction Long-term (HEAL) Initiative, multiple vaccine strategies are being developed that, if successful, would induce fentanyl antibodies that specifically bind fentanyl (but not other opioids) in the blood, preventing it from crossing the blood brain barrier and reaching the central nervous system where it can cause lethal respiratory suppression (Figure 1) [15, 16]. Prominent among these strategies is the use of vaccine adjuvants, substances which improve vaccine immunogenicity [17]. Patients with opioid use disorder (OUD) are obvious targets for a fentanyl vaccine, as are persons whose substance use presents risk for fentanyl exposure. Adolescents and young adults have rising rates of prescription opioid use and misuse, making them a target group [18, 19]. Youth also have high rates of illicit substance use, including cannabis [20] that may be laced with fentanyl [21]. Another possible target includes the more than 1 in 5 American adults with chronic pain [22]. In 2019, 22.1% of US adults with chronic pain used a prescription opioid in the past 3 months [23]. Of this group, 21–29% use their prescriptions non-medically and 8–12% go on to develop an OUD [24]. Dose escalation may lead to accidental fentanyl overdose; moreover, opioid seeking can lead to use of illicit opioids containing or contaminated with fentanyl.
Figure 1.
Adjuvanted fentanyl vaccine to prevent opioid overdose. A, Fentanyl activates reward circuit signaling, contributing to opioid use disorder (OUD) and overdose risk via lethal respiratory suppression. B, Vaccination using fentanyl (a hapten) chemically linked to a carrier protein (eg, CRM-194). Adjuvants enhance vaccine immunogenicity, via enhancing the quality and quantity of antigen presenting cell maturation and costimulation, T helper-polarizing cytokine production and antibody production, resulting in broad and durable immunity against fentanyl. C, Antibodies prevent fentanyl from crossing the blood brain barrier, binding to opioid receptors, and activating reward circuit signaling processing and risk of lethal respiratory suppression. (Illustration adapted from Banks et al 2020 [15]).
A fentanyl vaccine model would confer passive overdose prevention whereby an at-risk individual would benefit from a reduced risk of overdose, even if they cannot change high-risk behaviors. Passive protection via vaccination may be well suited to ameliorating OD given that substance use and addiction are problems of behavioral regulation [25]. Preventing overdose using a vaccine strategy is a harm reduction approach to protecting health. It is distinct from, and complementary to, both the use of an emergency rescue medication to reverse the effects of an overdose (ie, use of naloxone) and medication for addiction treatment (ie, methadone or buprenorphine or naltrexone), which requires regular engagement with the healthcare system [26–28]. In contrast to vaccine strategies for infectious disease in which there may be no benefit to remaining susceptible, durability of a fentanyl vaccine could impact acceptability for some persons. Patients who develop OUD or misuse prescription opioids because of pain might be hesitant to be vaccinated because vaccination would render fentanyl an ineffective therapeutic agent. As such, limited durability may be preferred. Alternatively, persons who misuse substances including prescription opioids may be poorly connected to the healthcare system and/or nonadherent with requirements to track vaccine efficacy over time [29], impacting their likelihood of obtaining a timely booster. In this case, lifelong durability may be preferred.
Given societal concerns regarding vaccine safety and efficacy [30, 31], and the potential for unique questions and concerns regarding acceptability of a fentanyl vaccine, we investigated attitudes towards use of a fentanyl vaccine to prevent opioid OD. We explored general reactions to a vaccine model for overdose prevention, perceived benefits, risks, and preferences regarding vaccine durability. We also explored reactions to use of a fentanyl vaccine strategy in response to hypothetical clinical vignettes designed to prompt consideration of the suitability of vaccine use for recipients of different ages, health histories, past and potential fentanyl exposure. Findings are relevant to future vaccine development efforts and research to optimize outreach and promotion of a fentanyl vaccine once safety/efficacy are demonstrated.
METHODS
We conducted a qualitative interview study to understand attitudes toward use of a fentanyl vaccine to prevent overdose mortality. Participants from clinical and community settings were interviewed about their reactions to using a fentanyl vaccine to prevent overdose, considering their understanding of and experiences with the opioid epidemic, and potential impacts of fentanyl vaccination on future pain management. The study design and operations followed best practice criteria for data collection and reporting for qualitative research [32]. Conduct of the research was approved by the study site Institutional Review Board (IRB) with a waiver of parental consent for participants younger than 18 years of age. All participants were assented/consented.
Participant Selection
We recruited a cohort of adolescent/young adult (≥15 years) patients with an OUD (“case” participants) from the Boston Children’s Hospital Adolescent Substance Use and Addiction Program (ASAP) or the Boston Medical Center Clinical Addiction Research and Education (CARE) Unit, along with a cohort of adult community stakeholders (“community” participants) including family members of enrolled patients (n = 7), healthcare professionals who work with patients with substance use disorders, and members of the general public. ASAP participants were directly contacted via phone to inform them of the study if they indicated interest to their ASAP clinician. The community and CARE cohort were recruited via flyers distributed through online/physical locations, targeted outreach to specific stakeholder groups and convenience sampling. All participants interviewed were compensated with $25 gift cards.
Data Collection
One-time 60–90-minute-long interviews were conducted in English, by telephone by 2 researchers trained in qualitative interviewing techniques. All interviews were in a private location; remote participants affirmed they were in a private place where they felt comfortable discussing potentially sensitive topics. Seven female researchers, trained in qualitative interviewing techniques using non-directive language, rotated conducting interviews and taking field notes. Interviews were audio-recorded with participant consent, and content was transcribed by study staff or a HIPAA-compliant transcription service. Transcripts were not returned to participants for review.
A semi-structured interview guide was used. Questions were open-ended, with non-judgmental probes and clarifying questions introduced when appropriate. All participants were read a brief, standardized explanation about how vaccines work and how a fentanyl vaccine might work at the start of the interview. Questions covered (1) vaccines—general thoughts and understanding; (2) the opioid epidemic and knowledge of fentanyl; (3) fentanyl vaccine—general thoughts, understanding and concerns; (4) vignette scenarios; (5) implementation and system-level factors. Fictional clinical case vignettes were introduced from a library of vignettes and shared with participants. Not all participants saw each vignette. Participants were asked to indicate whether the individual in the vignette should be offered a fentanyl vaccine and invited to share their reasoning. Recommendations were quantified and reasoning thematically analyzed.
Data Analysis
From 1 November 2019 to 1 December 2021, interviews were conducted, transcribed, and coded using NVivo software [33]. Six research assistants under the direction of ERW created a coding framework, coded interview data, and identified major themes. The team reviewed each full transcript, grouping textual responses into themes and subthemes. Interviews were initially coded by 1 researcher and reviewed by the team. Responses to vignettes were double coded and held to a consensus standard for interpretation of comments on a vaccine recommendation. The full process was iterative so that the coding framework, coding scheme and themes could be refined prospectively. Interviews continued until thematic saturation was achieved on the main topics of this investigation—acceptability of a fentanyl vaccine, benefits and harms, issues of durability and pain, and reactions to using a vaccine approach for the vignette cases. Although all identifiers have been removed from study data, quoted data are annotated with “case” or “community,” gender, and age in years.
RESULTS
Sample Characteristics
In total, we interviewed 64 participants, of which the majority (70%) was female (Table 1). The mean age was 32.4 years (ranging 15–64 years) and, on average, the case group was younger than the community group (ages respectively 20.2 and 33.6 years). Twenty percent of the sample (n = 13) was recruited from a clinical program and had a history of OUD (“cases”), and 80% (n = 51) were recruited from community settings (“community”). Of these, 21.6% (n = 11) reported personal exposure to opioids for a medical procedure, and 47.1% (n = 24) had a family member or friend with a history of OUD or overdose.
Table 1.
Sample Characteristics in Total and for Case and Community Participants
| Total | (%) | Casea | (%) | Communityb (%) | ||
|---|---|---|---|---|---|---|
| N | 64 | 13 | (20.3) | 51 | (79.7) | |
| Biological sex | ||||||
| Male | 19 | (29.7) | 9 | (69.2) | 10 | (19.6) |
| Femalec | 45 | (70.3) | 4 | (30.8) | 41 | (80.4) |
| Gender | ||||||
| Male | 20 | (31.3) | 9 | (69.2) | 11 | (21.6) |
| Female | 42 | (65.6) | 3 | (23.1) | 39 | (76.5) |
| Nonbinary | 2 | (3.1) | 1 | (7.7) | 1 | (2.0) |
| Age | ||||||
| Mean (SD) | 32.4 | (14.8) | 20.2 | (3.7) | 33.6 | (15.3) |
| 15–24 | 30 | (46.9) | 12 | (92.3) | 18 | (35.3) |
| 25–34 | 15 | (23.4) | 1 | (7.7) | 14 | (27.5) |
| 35–44 | 5 | (7.8) | 0 | (0) | 5 | (9.8) |
| 45+ | 14 | (21.9) | 0 | (0) | 14 | (27.5) |
| Recruitment source | ||||||
| Substance use and addiction program | 20 | (31.3) | 13 | (100) | 7d | (13.7) |
| Professional contact | 10 | (15.6) | 0 | (0) | 10 | (19.6) |
| Flyer | 9 | (14.1) | 0 | (0) | 9 | (17.6) |
| 13 | (20.3) | 0 | (0) | 13 | (25.5) | |
| Direct email to organization | 2 | (3.1) | 0 | (0) | 2 | (3.9) |
| Other BCH studies | 10 | (15.6) | 0 | (0) | 10 | (19.6) |
| Exposure to opioids from a medical procedure | 14 | (21.9) | 3 | (23.1) | 11 | (21.6) |
| Indicated friend/family with OUD or had overdosed | 33 | (51.6) | 9 | (69.2) | 24 | (47.1) |
Abbreviations: BCH, Boston Children’s Hospital; OUD, opioid use disorder; SD, standard deviation.
Diagnosed with an OUD.
Stakeholder community cohort.
1 person missing biological sex indicated that their gender was female. Their biological sex has been classified as female.
Parent or grandparent of person with OUD.
THEMES
Vaccine Acceptability
Favorable Attitudes Toward Vaccines in General
Most participants expressed generally favorable attitudes toward vaccines. The plurality reported receipt of routine immunizations including for influenza. A minority (n = 8) reported favorable views of vaccines generally, but hesitancy or avoidance around personal use especially of the flu vaccine. One participant reported concerns about vaccines generally and avoidance personally.
Acceptability of a Fentanyl Vaccine
Attitudes were strongly favorable towards the idea of using a vaccine to prevent fentanyl overdose. Favorable reactions were found among participants in both case and community groups, males and females, younger and older participants. As a 23-year-old male case stated, “so when [the research assistant] first mentioned it to me I was very enthused. I think my first reaction was ‘holy crap that’s amazing’ because it seems like … if it can be done… it would be something that could potentially make a lot of people in my position, make their lives a lot easier, you know.” The novelty of the approach, and excitement concerning the potential for reducing overdoses and saving lives were called out, “If you could do that, that would be like a game changer…because it would save lives,” stated a 59-year-old female from the community. A sense of incredulity was expressed about the vaccine’s efficacy in protecting against a drug as potent as fentanyl, as stated by a 22 year-old male case, “the only thing I’ve heard of is like Narcan that reduces an overdose directly, I’ve never heard of any vaccine that could prevent an overdose …just because of how strong the drug is, I can’t imagine a vaccine being able to just stop an overdose … it’s hard for me to imagine.”
Benefits of a Fentanyl Vaccine
Benefits of a fentanyl vaccine strategy were identified at individual- and societal-levels (Table 2) with potential for helping persons at firsthand risk of OD (ie, substance users and their family members), youth in general, college students, and parents who might have a new tool for protecting their children. High value was placed on the potential to save the lives of persons at risk of overdose through intentional or unintentional fentanyl exposure. Participants commented on the cascading benefits to children from preventing overdose among their parents/guardians. Decreased motivation to use fentanyl and potentially, other opioids or drugs, were hypothesized if fentanyl’s euphoric effects were blocked. Participants perceived strong potential for the vaccine to provide lifesaving support for persons with SUD awaiting treatment or in recovery. Benefits realized at the system- and societal-levels were identified including the opportunity to save healthcare dollars and clinical resources that would otherwise be expended on treating opioid overdoses. Participants speculated on whether a vaccine might reduce demand for fentanyl and disrupt the illicit fentanyl market, perceived as a positive supply-side effect. Finally, the vaccine was understood by some as a new prevention tool for parents, clinical and public health programs wherein vaccination could be promoted as strategy to demotivate drug use early in life (ie, by blocking euphoria) positively altering a drug use trajectory.
Table 2.
Perceived Benefits of a Fentanyl Vaccine
| Perceived Benefits of a Fentanyl Vaccine at the Individual Level |
| Potential to save lives |
| It could save a lot of peoples’ lives that could have overdosed and died from fentanyl if they didn’t have the vaccine. [Case, 17, Female] |
| I think that it can save a lot of lives from being lost. [Case, 18, Female] |
| I hope it comes out as soon as possible ‘cause it would save so many lives. [Community, 32, Female] |
| Reduced use and addiction if euphoria is blocked |
| I mean, the fact that there, if it’s not even crossing the blood-brain barrier and so they can’t even get high that’s potentially will reduce the addiction potential of opioids. And so maybe you’ll have fewer people doing opioids in general because that fentanyl is not getting them high. So, it’s like reducing the overdose risk, but also reducing the risk of addiction in general. [Community, 29, Female] |
| I would say [the potential benefit of this vaccine would be] probably making people less likely to use it [fentanyl], ‘cause if you do use it, you’re not going to get the benefits or effects of it that you’re looking for. So definitely it would deter that. [Case, 25, Female] |
| It can just stop people from being addicts because if they tried to, if they tried to [pause] get high, they can’t unless they want to do it for no reason basically. [Case, 17, Female] |
| If there’s no reason for people to take the drug because they won’t get high anymore, then I think that will definitely lower the rates of people taking it at all. [Community, 15, Female] |
| Reduced overdose risk from unintentional exposure |
| It does protect people who want to, like, if they do use drugs on the streets, they can’t die from laced drugs from fentanyl. [Case, 15, Male] |
| Yeah, I guess I would see the most benefit, I don’t know, I guess I imagined people who…occasional drug users or maybe like, or even just like vaccinating college students who might try things at parties, whatever. I think would hopefully help with…people who are maybe not long-term drug users, but accidentally took fentanyl. And hopefully it would prevent a lot more death that way. [Community, 26, Female] |
| I mean it sounds like a good idea because, I mean, I feel like there’s probably not many people that are like interested in specifically using fentanyl. So even if they like weren’t planning on quitting whatever their other like drug of choice is, they still might be interested in the vaccine because that way they would be protected from like stuff that they didn’t want to be using…for example, like a heroin addict who wasn’t planning on quitting or, like wasn’t ready to quit necessarily, like wouldn’t, they wouldn’t want to get just, like a general vaccine. But if someone told them that they could get something that would, like protect them in case they bought a batch that was, like laced then, like I’m sure that they would be interested. [Case, 18, Male] |
| Potential to provide bridge to treatment |
| I think it could definitely help a lot of people who maybe want to get clean but are still struggling with it. I think it could help a lot, get more people on the right track and away from using fentanyl. [Case, 20, Male] |
| [The fentanyl vaccine is] really just a buying time. You know, like “Here you can… do this to stay safe and stay alive because hopefully you’ll get tired of this and, come around and ask for help and ask for treatment.” [Community, 42, Female] |
| Reduced suffering |
| If it can be done, it seems like it would be something that could potentially make a lot of people in my position, make their lives a lot easier, you know… Not having to worry about that is just, I can’t put a price on it, and I can’t really tell you how important it is to me. [Case, 23, Male] |
| Perceived Benefits of a Fentanyl Vaccine at a Societal Level |
| Reduced burden on healthcare system and workers |
| It could definitely save hospitals and the healthcare system that, you know, when you have an overdose, you know, it’s very, very sad…My daughter’s an ICU nurse and, you know, it’s just so sad to see, you know, these young, young people and middle-aged people on respirators and their families can’t let go and out of guilt out of whatever it is. So, they can live in long-term rehab, although for years and years. So, the money that it could save in the healthcare system that is crippling the healthcare system would be beneficial. [Community, 62, Female] |
| It could definitely help a lot of people, and I don’t know specifically how this would work, but definitely save the healthcare system or society a lot of money in having to deal with when people do become addicted to them and then everything that happens after you’re addicted and seems like that would definitely reduce all of that. [Community, 25, Female] |
| Potential to be proactive, preventive tool |
| I could see this [vaccine] being, leading into other addictive drugs also. And as a parent, way to prevent drug use with their children and cocaine and all that kind of stuff …I think there’s a lot of benefits to that, especially with parents of teenagers and college kids and fear of doing that [drugs]… Convincing somebody once they’re an adult to do it [get a fentanyl vaccine] and they already like the high from that, that’s almost too late… You almost have to do it before or as early teen or something like that, to prevent it [drug use/addiction] as a parent. [Community, 43, Female] |
| If this [vaccine] was available, when my kids were 10 years old at their pediatrician, I don’t care. You’re getting it. You don’t need to know what it is. You’re getting it. [Community, 49, Female] |
| You never know what the fentanyl really is in. Especially if you’re like a parent and you have a teenager, it’s just one of those things. If you have the option to have a preemptive strike then I would do it, you know, if I was a parent, so, I, you know I definitely think it is a great idea. [Case, 24, Male] |
| I’m a very pro-prevention person…Getting them on the front end with education and prevention, but this, this almost seems like an end game prevention tool. Like it’s like saving them from overdosing before they even get to that place. [Community, Female, 55] |
| Potential to disrupt the illicit drug use industry |
| Well, because you’re, you’re preventing overdose deaths, and you’re basically, you’re saving these people’s lives and you’re preventing… I guess they can’t even really get high off of it, so you’re basically stopping the industry. [Community, 24, Female] |
| Well, I mean, if it was distributed enough, I mean, maybe people would stop putting the fentanyl into the, into the heroin cause they know they’re not, you know, people are immune to it, why would you just keep putting it in, like putting in sugar, you know, it’s not doing anything. [Case, 24, Male] |
Questions, Concerns, and Harms
Several potential harms of a fentanyl vaccine were mentioned. Participants commented that disclosure of fentanyl vaccination might provoke negative reactions in healthcare or other settings. Fear of being stigmatized was discussed as a barrier to being vaccinated, and some participants noted that parents might be especially sensitive to this on behalf of a child, which could strengthen their tendency to deny or minimize a child’s substance use problem. Participants expressed confusion about the vaccine model for preventing OD versus treating addiction (Table 3), and bafflement about the application of a vaccine to address a behavioral disorder. One participant shared the concern that recent gains in bringing attention to issues of addiction and the opioid epidemic could be lost by joining the sensitive and potentially stigmatizing issue of opioid use and overdose to public controversy around vaccination which continues to be a sensitive, contentious, and politicized issue in the United States.
Table 3.
Stakeholder’s Questions, Confusion, and Perceived Harms of a Fentanyl Vaccine
| Perceived Harms of Using a Fentanyl Vaccine |
| Concern for stigma, and denial of problem as barriers |
| …there could be certain stigma like, people… thinking, oh, you were a drug addict, and you’re an opioid addict stuff like that. … When they check your [medical] record, then they see you’ve taken the vaccine, they may not really recommend certain treatment for you, because you’ve taken the vaccine. [Community, 25, Male] |
| I feel like if someone were to come in and I saw they had a fentanyl vaccine, there would be a – stigma put on them… If [a doctor] saw I had, like, a fentanyl vaccine, or I had an opioid vaccine, it might be like “oh I wonder if he has any history with this” or “I wonder if he struggles with this – and that’s why he got it”… because [a fentanyl vaccine] it’s not commonplace… people might put a stigma on it ‘cause they don’t know much about it. [Case, 25, Male] |
| [The fentanyl vaccine] might look bad to certain people. But I think it’s a good precaution to take… I think where there’s like a job that they are interviewing for and they saw that they took [the fentanyl vaccine], [the employer] might not trust them as much, or they might think of them in a different way. I think it should be made sure that people can’t judge based on that. [Community, 15, Female] |
| I think… it’s going to take some convincing for people to actually accept [a fentanyl vaccine]. And I think part of that has to with… being stigmatized and marginalized… I think people will be very resistant to [a fentanyl vaccine] like almost in denial in some instances like, oh, well I don’t, it’s not that bad of a problem or my kid with be fine or whatever it is. [Community, 29, Female] |
| I’m sure plenty of teenagers or college students who do drugs do not tell their parents they do drugs. So, I guess I’m worried about like, stigma from people being like, “well, my kid will never use drugs, so why would I get [the vaccine] for them”. [Community, 26, Female] |
| Controversy |
| I think we’re—I think it’s a tough environment right now to introduce a vaccine into—that could be, that could be controversial, given how scientists have for a long time struggled to control the vaccination-related narrative. I worry that, you know, just like how many scientific advances have been sort of … stopped by botched narratives, I think that there’s gonna be… some serious challenges with say, like ‘cause America gives outstretched voices to those who don’t, who are ignorant, as sad as that is. And so, … I actually worry about the vaccine for some reason, getting, that narrative going in such a wrong direction that actually hurts the progress that has already been made in raising awareness of the issue and treating opioid usage. And I just feel like if it goes poorly, it could actually hurt the rest of the field of opioid studies. [Community, 25, Male] |
| Vaccination creating a false sense of security |
| [People who are getting this vaccine] should know that this isn’t just like a guaranteed protection from using recreational – drugs recreationally… people might just hear about it and be like “This will keep me safe from all the chemicals that they’re adding to street drugs. I won’t have to worry about whether it’s authentic or not”. [Case, 18, Female] |
| Let’s say this vaccine comes out, one thing that would worry me is, people that do use drugs recreationally will be like, “Oh, if I take this vaccine, I’ll be safe. I can buy street drugs I won’t have to worry about fentanyl.” [Case, 18, Female] |
| Potential for increase of drug use and exposure to other toxins |
| If the person whoever is using and gets this vaccine, they go to use again and they can’t get high, at what point are they going to stop? Are there any adverse effects when taking those drugs due to the vaccine or are they just injecting themselves in hopes to get high? What other toxins would be in this drug that they may be ingesting, injecting, or whatever and, you know, if they’re trying to get high, you know, maybe they’re just going to keep dosing until they feel something. [Community, 28, Male] |
| I think people would start being careless [if they got the fentanyl vaccine]. It’s a possibility, they think they won’t die from it, but morphine and heroin still cause overdoses. And they still are deadly. Not as deadly, but still, deadly is deadly. [Case, 15, Male] |
| Loss of autonomy and pleasure through vaccination |
| Well, I think that for people who were fentanyl addicts, and they take the vaccine, the fact that they’re not able to get high anymore might make them really upset or very depressed… So, I feel like if you take that away for some people it could like really like mentally hurt them. Because honestly, me thinking about me never doing fentanyl again, it’s kind of sad to me, even though I want to get clean, because it’s so satisfying and like amazing to me. Like, I feel like it’s just disappointing, like really sad… I feel like [never using fentanyl again] would make me really kind of upset that I could never get high like that anymore and feel that joy and that feeling ever again. [Case, 17, Female] |
| I absolutely hated [suboxone] even though I was clean. And I wanted to remain clean. There was some psychological that I really didn’t like that I never, I didn’t have the choice to be clean or not. It was just taken off the table. It’s almost like… I don’t know… it’s somehow related to not being able to, like, kill yourself, basically. Like, you have that option, you always like kinda have that option, even though you know that you’re never going to do it. And then when someone takes that option away from you. I don’t know, there’s something about that option that I really did not like. [Case, 24, Male] |
| Questions, confusion, and misconceptions about a fentanyl vaccine |
| Concerns about the development of new synthetic opioids |
| If [fentanyl] is used in a clinical setting, then wouldn’t it make it kind of obsolete if everyone’s vaccinated against it?… so, if everyone’s vaccinated, oh, then it – yeah, then would they just make a more powerful opioid? [Community, 24, Female] |
| How long before some drug manufacturer changes their chemical composition of fentanyl, just by a little bit, and then all of a sudden, your antibody doesn’t work anymore because antibodies are kind of niche? [Community, 17, Male] |
| Opioids are always gonna be around, people are always gonna use them…will this encourage the production of like more powerful drugs, because then like everyone’s vaccinated against one of the most powerful ones. [Community, 21, Female] |
| Questions about how the vaccine would work in the body |
| So, when you say that it gets too large to enter the brain, I am just unsure how it leaves the system. Like, does it then just leave the system, or does it continue to build up in the body? Just, if not, it sounds like damage to the brain. [Community, 22, Female] |
| The first thing I would ask is how it works. Like does it work like a flu vaccine where you’re injected with a tiny amount of drug and your body becomes used to it? [Case, 22, Male] |
| I guess, I’m curious how it affects people who are already using drugs more maybe, but hopefully, if someone was not or not as often, maybe it would stop someone from developing a more severe addiction as well. [Community, 26, Female] |
| How is this vaccine aimed to work? I mean, I guess I’m kinda confused… I just don’t understand how a vaccination for something like fentanyl would work… because fentanyl’s not a disease. You know what I mean? It’s a medication that’s given… The use of fentanyl, or the use of alcohol, or the use of a barbiturate… somewhere in there is a conscious choice that they should take it and a conscious choice by a doctor that they should prescribe it, so I, I mean it’s not the chicken pox… are you aiming to create a vaccination that eradicates any type of addiction? [Community, 30, Female] |
| I honestly didn’t think that you could make a vaccine for anything that’s not like a virus, just anything not living. So I think it’s kind of incredible that this is even a possibility. [Community, 19, Female] |
| Questions about circumstance for use and eligibility criteria |
| [Asked who should get the vaccine] Who do you identify? Do you identify just IV drug users, but then fentanyl can be given several different ways? You can smoke it. You can snort it. Now it’s compounded and taken as a pill… Is [a fentanyl vaccine given to] the addict that overdoses one time, two times, three times? I don’t know. [Community, 62, Female] |
| Would there be some sort of benefit that if the majority or all of a population were to receive the vaccine, or would it really just be helpful to those who are, I don’t know, at higher risk for being exposed to these drugs and experiencing something negative from these drugs? [Community, 21, Male] |
| How would people be recruited for the vaccine… who would it be targeted for? Are you going to NA groups and like shopping around this vaccine, or are you going to transitional housing programs or [emergency rooms] things like that? I just think it’s hard with a vaccine for people who don’t have a lot of interaction with the healthcare system in preventative ways… If you’re actively using, I don’t think your first priority is to go to your PCP every year… So, how would this be implemented? [Community, 21, Female] |
| Confusion between protection and rescue intervention |
| So, you would take the vaccine. This would be like some syringe that you buy to have ready at hand after you take an opioid recreationally, or this is like a vaccine that many people would get at some, I don’t know, proactive or preemptive date. And then it would prevent overdoses in the future. [Community, 21, Male] |
| Correct me if I misunderstand how this would work, but it seems to me like one of the biggest advantages of a vaccine is (A) in theory, and I don’t know how the science is gonna play out, but I think you’d only have to get it once and (B) I would think that you’d be able to get that vaccine, you know, five minutes after ingesting an opiate, or ingesting fentanyl, because I would, I would assume that, I’d assume that if all its doing is negating your body’s ability to get that into the receptors, I would think that it would be safe to use it… [Case, 23, Male] |
| Misconceptions that vaccine blocks withdrawal, blocks addiction |
| I think it would help people that if doctors prescribe them medications, and they have withdrawal from it. But they wouldn’t have them because they’d have the vaccine. [Community, 16, Female] |
| I think you got a good market for that, the fentanyl vaccine. So, you know, the pain doctors who prescribe it and keep prescribing it could then say, okay, if you want to get off, there’s a vaccine, you know, so they can sell it in one package. You know, like right now you got a sore leg, you can have a pain relief, and then here’s a prevention so that you won’t get addicted to it or have that mental addiction to it. And so there you go. [Community, 58, Female] |
| It can just stop people from being addicts because if they tried to, if they tried to [pause] get high, they can’t unless they want to do it for no reason basically. [Case, 17, Female] |
| Yeah, like I said, it’s [the vaccine is] going to help in reducing drug addiction, drug use, and yeah, probably drug effects. [Community, 35, Male] |
Concern that vaccination could unintentionally increase substance use behaviors was considerable if vaccinated substance users were to increase their fentanyl use to overcome the antibody blockade. Risks for drug overdose and toxicity could increase, some shared, under a false assumption of broad (ie, opioid) rather than narrow (ie, fentanyl) protection (Table 3). Many participants expressed concerns about the loss of fentanyl as a medication for chronic or emergency pain treatment, voicing consternation that a proven therapeutic would be “taken off the table,” possibly for life. Finally, a minority of participants acknowledged that being vaccinated could be experienced as reducing agency and autonomy around an individual’s choice about their health even where choices to use substances are unhealthy and dangerous. Relatedly, loss of pleasure was mentioned as a harm given the potential for partial or full loss of euphoria from fentanyl if vaccinated (Table 3).
Vaccine Durability
Preferences for a vaccine formulation that would provide lifetime protection against fentanyl overdose versus a time-limited formulation that would require booster doses were expressed by a majority (n = 42 of 55 asked, or 76%) for whom a “one and done” approach was considered optimal (Table 4). Many participants noted challenges with respect to engaging persons with SUD in monitoring vaccine efficacy as this population can be disconnected from care and unstable. High adherence and implementation barriers were anticipated related to tracking vaccination among persons with SUD, making receipt of a timely booster problematic and potentially unrealistic. There was concern that vaccinated persons might imperfectly track waning efficacy or miss a booster and overdose if exposed to fentanyl. For some, concern for effective pain management in the future shaped preferences for limited durability. Appreciation for the role of pain as a risk factor leading to misuse of opioids was clear, and there was consensus that exposure to prescription opioids for pain through the medical system or via self-treatment outside of medical management were highly influential drivers of OUD and the opioid epidemic necessitating special consideration for vaccine acceptability. Some participants who had struggled with both OUD and pain shared that they would forego medical use of opioids in the future rather than risk relapse even if it meant living with pain. A minority (n = 11 of 55, 20%) preferred shorter term durability given concern for pain management, erosion of autonomy and agency, and inability to make a commitment to a lifelong fentanyl blocking vaccine. A booster model or being given a choice for lifelong or limited duration vaccines were seen as preferable for these participants.
Table 4.
Stakeholder Opinions About the Durability of a Fentanyl Vaccine and Concerns About Pain Management
| Perceived Benefits of a Lifelong Vaccine (Extended Durability) |
| Ability to cover chronic relapsing course of addiction |
| I feel like if you’re also trying to prevent something like this, a life-long vaccine makes more sense because people go through different cycles of encounters with these kinds of dangers throughout their life, whether knowledgeable or not of the situation. [Community, 25, Female] |
| Lifetime. Once you’re an addict, you’re always an addict, so it’s like, you know, if the addiction isn’t ever going to leave you. Even if you’re in recovery you’re always going to have the work of program and recovery in order to stay in the mindset to not go back. So, you know, a vaccine that was long-term would be in the same vibration and communication of a lifetime of recovery. [Community, 55, Female] |
| I think that having as a lifelong vaccine would be more effective… You’ll find that people who are [using drugs] in their youth sometimes when they get into difficult situations in their later years in life tend to want to go back to getting such – to help them psychologically. [Community, 34, Male] |
| … because [my son] stopped taking it [Vivitrol] just a couple of months before he died. He had been on for almost four years at that point. And he said “I just don’t think I need it anymore” … because it was presented as something …, you probably won’t need this forever… instead of, … you have been an addict, and you will probably need this for your whole life… And I think that it would be the same with fentanyl. [Community, 63, Female] |
| Reduced risk of nonadherence to booster model and logistical challenges |
| Getting [the fentanyl vaccine] annually might be a bit of a deterrent from getting it, you know, people have busy live, it’s hard to get a vaccine for something you don’t even think will be a problem. A lot – most people who develop addictions to fentanyl don’t think they’re – no one plans on getting an addiction. [Community, 21, Male] |
| So, I feel like the one-year thing, also then you have the other issue of like encouraging other people to come back to take another, and the frequency to go back and get another shot, should that be required later on, it becomes harder and harder. [Community, 25, Female] |
| Yeah, I’m more on the camp of the one and done… Follow-up care is always a problem, especially if you’re talking about disadvantaged populations. They’re not even going to get their flu vaccine, you know? I see these kids every day, I see families, like are they really gonna come back and get a, a opioid vaccine every year or every two years or whatever, you know? [Community, 25, Male] |
| Ease of one-time payment |
| Economically, you know, people – especially those who like don’t have health insurance, that seems like a lot easier for them to pay for this vaccine once as opposed to have to get it annually. [Community, 21, Male] |
| Perceived Benefits of a Booster Vaccine (Limited Durability) |
| Ability to use fentanyl for future pain management |
| The only reason… I would be concerned if [the fentanyl vaccine was] for life is if somebody really got into an accident or they did get cancer and [fentanyl] was the only thing available to them to manage the rest of their life… I’d be concerned if it’s like a lifelong vaccine… And the other reason would be people do recover from this, and you know, maybe it doesn’t need to be lifelong… I would be a little apprehensive if it was more lifelong than if it was something that you would take a booster for or that it was yearly or something like that. [Community, Female, 56] |
| If [fentanyl] is used in a clinical setting, then wouldn’t it make it kind of obsolete if everyone’s vaccinated against?… My mom, her surgery they gave her fentanyl, so if everyone’s vaccinated… would they just make a more powerful opioid?… Yeah, then I don’t know if everyone should get vaccinated. [Community, 21, Female] |
| Flexibility in decision making |
| I think the booster where you get a shot every couple of years would be good. Because I think if it was for life, I don’t know if people would want to commit, some people would, but I don’t know if other people would want to commit to something so long lasting… generally speaking, [people] don’t like commitment. So, you know, so that’s why I thought the one that you might do every couple of years would be better than a lifetime one. Because you know, they don’t know “Well, how will I feel in 10 years. I might not want it then”, you know? [Community, 42, Female] |
| You know, you mentioned you’re making a decision of a lifetime. You know, one thing to keep in mind with this high-risk population, especially is that they live day-to-day, they live hour-by-hour. The will not – if you tell them this is forever, you’re going to have a hard time selling that. Even for them taking a Vivitrol shot for a month is sometimes hard to conceive. [Community, 56, Female] |
| Lack of autonomy with lifelong vaccine |
| There’s the [Narcan] shot and [it is] a preventive thing they put in that lasts a month. And you can’t, you can’t get high on any opiates. It’s like, one of the ingredients that’s in suboxone. And that’s that opioid blocker, is the one that they, in the shot. And I absolutely hated that even though I was clean. And I wanted to remain clean. There was some psychological that I really didn’t like that I never, I didn’t have the choice to be clean or not. It was just taken off the table. It’s almost like… I don’t know… it’s somehow related to not being able to, like, kill yourself, basically. Like, you have that option, you always like kinda have that option, even though you know that you’re never going to do it. And then when someone takes that option away from you. I don’t know, there’s something about that option that I really did not like. [Community, 24, Male] |
| Maybe it is better as a booster because then, if someone’s parents vaccinate them against this, then in the future they can stop because they want to. I think people should have the choice and with a lot of vaccine we don’t have the choice because we’re a baby when we get them, or like young. Maybe it would be better if they had a choice. [Community, 23, Female] |
| Concerns about pain |
| Concerns about pain management after vaccination |
| If I was to one day, in like, you know, had a car accident, and I was in severe, severe pain, and if they were going to give me an IV drip of an opioid and it wasn’t going to do anything for me, like it wasn’t going to relieve any pain, I would, I would second-guess about the getting vaccine. [Community, 25, Male] |
| A lot of my clients who do end up having any type of surgery and are offered painkillers, they don’t take them because they’re so afraid it’s going to resume their active use. [Community, 42, Female] |
| If I were to get the vaccine, I would really want someone to sit down with me and say if you needed surgery, this is what we would do for you. Like really just get a specific idea of like what are the alternative protocols, just because so many anesthetic protocols are dependent on fentanyl. Do we know that for sure that there are things that are effective, do we know the dosages of those things? My intuition was that I would want [the vaccine] because I want the safety that it would provide, but I would just want to make sure that if I ever needed surgery or some other treatment that I would be taken care of. [Case, 24, Nonbinary] |
| For an epidural… That’s like a super common procedure for laboring women, right? They all got fentanyl in epidurals, right? So, I told you before I would get this vaccine, if I couldn’t have an epidural for childbirth, I would not take the vaccine. [Control, 31, Female] |
| Special concerns of people with a history of pain |
| I have _____ [condition], which can lead to emergency surgical interventions pretty frequently. Someone with a condition like that might be a bad candidate [for the fentanyl vaccine] just because there’s someone who is going to need frequent, medical interventions where fentanyl can be useful. I think someone with a progressive pain condition… we might want to keep fentanyl open as a treatment option… I think if that person also happened to have an opioid use disorder, it [the fentanyl vaccine] would be a more complicated balancing act conversation with their physician. [Case, 24, nonbinary] |
| So, most people, most of my clients [who have a history of OUD] that have had surgeries, just, you know, struggle through with, like, Tylenol and things like that. Which I always think is so incredible. [Community, 42, Female] |
| I don’t consider myself addicted [to opioids], but I do consider myself dependent… I know I couldn’t stop my medication tomorrow; I’d have to wean off of it… So, I don’t want it [fentanyl] taken away from people, like me, who need it for chronic pain. I think it is a necessity right now because I don’t have an alternative… The medication that I take, it doesn’t take the pain away 100%, but it does take it away enough so I can function. That’s why I think [fentanyl] needs to be available. [Community, 58, Female] |
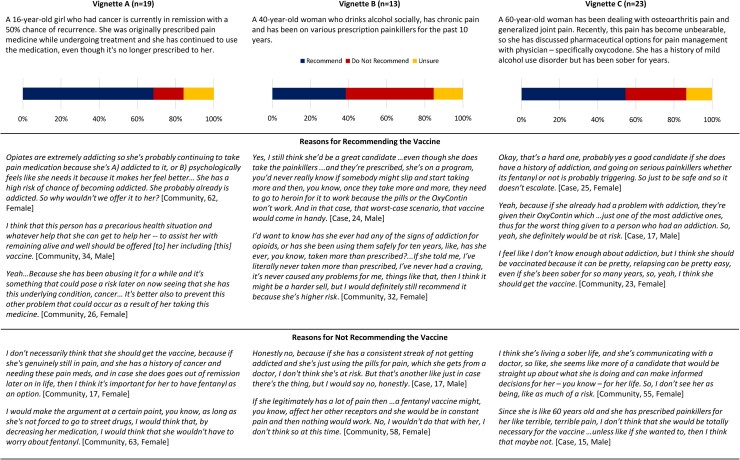
Need for Personalized Decision Making and Support
Reactions to case vignettes (Figure 2, Vignettes A–C), illustrate how views regarding use of a fentanyl vaccine model are situation specific, and preferences reflected concern for accurate understanding of a person’s health profile, substance use history, addiction liability, and experience of pain. Views reflect appreciation for the multidetermined nature of OUD and the importance of personalized decision-making to address views about vaccination, the complexities of pain management, a patient’s social and family history, and assess needs for system-level supports to address fundamental causes of addiction.
Figure 2.
Reactions to vignette scenarios and reasons for recommending or not recommending the fentanyl vaccine.
Vignette A is an adolescent female with a history of cancer and of misuse of prescription pain medications. The plurality of participants queried (68%) recommended her for fentanyl vaccination for reasons reflecting the addictiveness of opioids, her unstable health circumstance and goals of prevention and harm reduction. Opposing views reflected potential need for fentanyl in the future for recurrent cancer pain, and perception that only “street drug” use merits vaccination protection and presumption that medical management and tapering was possible. Vignette B is an adult woman with chronic pain and a history of prescription pain medication use. Perspectives were split and large minorities of queried participants recommended or opposed vaccination (38% and 46%, respectively). Reasons favoring vaccination reflected views that this person would “slip” and escalate use and is at higher risk given pain condition and prior use. Reasons opposing reflect assumptions that she’s not at risk given the medical source supply of her medications and concern for future need for pain management including of other opioids that might be rendered ineffective via fentanyl vaccination. Finally, Vignette C is an older adult woman with worsening pain conditions and a history of mild alcohol use disorder (AUD) followed by sobriety. A majority (55%) favored vaccination given her history of AUD and the addictive liability of oxycodone. Opposing views cited medical management, sobriety, and need for pain treatment options as reasons.
DISCUSSION
In this qualitative investigation, we found that a proposed vaccine to prevent fentanyl overdose was generally highly acceptable to a diverse group of stakeholders of whom half reported a friend/family member with OUD or OD history, and one-fifth reported direct exposure to opioids from a medical procedure. Perspectives reflected an appreciation for addressing the scale of the overdose crisis, the chronic relapsing nature of substance use disorders, easy availability of fentanyl, and high risks for unintended exposure through drug contamination. Acceptability was indicated in recognition of myriad complex pathways leading to fentanyl OD, including intentional drug use, drug contamination, misuse of opioids following medical procedures, and through efforts to manage pain within and outside of the healthcare system. Generally, participants agreed that a fentanyl vaccine could be an important harm reduction strategy and held clear views about its possible benefits, namely potential to save lives, suffering, resources, and provide new tools for prevention.
In contrast to negative views toward other harm reduction efforts that involve substance use such as those aiming to reduce/prevent HIV infection through distributing clean needles or providing access to safe injection sites [34–36], we found modest indication that a fentanyl vaccine might be controversial. Rather, there were perhaps unrealistic expectations for preventing and treating addiction, reducing harms from other opioids and interrupting the supply of illicit drugs. Preventing overdose with other opioids, and the litany of non-fatal morbidities associated with OUD, would not be addressed by fentanyl vaccination. Precautions regarding opioid prescribing and opioid use would need to be utilized despite vaccination, and patients who develop OUD would still need specialized treatment for that disorder. Communications to distinguish a vaccine from a treatment model will be needed, as will public and patient education about the use of a vaccine to treat a behavioral rather than infectious disease condition which was viewed by some with confusion.
Despite favorable attitudes towards a fentanyl vaccine, challenges and potential problems were identified. Participants volunteered that being vaccinated could be stigmatizing and observed that patients who receive a fentanyl vaccine may be assumed (even if incorrectly) to have OUD, leading to negative impacts on care. Concern to avoid stigma coupled with denial could impede vaccine uptake. Although it is possible that a new medical technology such as a fentanyl vaccine could advance the concept of OUD as a medical condition versus a moral weakness, concerns confirm that more explicit effort to address stigma including in medicine are needed.
Participants also discussed the possibility that vaccination could contribute to an increased risk for OD if drug users hold incorrect assumptions about the vaccine’s breadth or timing of protection. Questions that arise with all vaccines, including magnitude and durability of protection, were asked and preferences for lifelong durability expressed to minimize access barriers and avoid need for boosters. Notably, similar logistical concerns were found among pharmacists surveyed about attitudes toward anti-opioid vaccines [37]. It is unlikely that opioid exposure post-vaccination would eliminate a strategy of limited durability for vaccine activity given that haptens alone are inherently inert, and no major adverse events have been observed among more than 1000 patients who have taken anticocaine and antinicotine vaccines over the past 20 years with modest efficacy [38].
Participants were worried also about how vaccination might interfere with chronic pain management. Tension between concerns for preventing OD, on the one hand, and “loss” of fentanyl for pain management due to vaccination on the other, were apparent and suggest the importance of a vaccine strategy that respects patient-centered concerns, supports shared decision making, and offers clarity and options for pain management. It is unlikely that the proposed fentanyl vaccine will complicate either acute or chronic pain management but work to ensure this and offer guidance will be needed. Long term opioid prescribing for pain is becoming less frequent. The public debate about the increases in opioid-related deaths in the last decade and insufficient evidence of long-term efficacy when viewed in light of the risks and harms has led to a significant shift in the ways opioids are prescribed for non-cancer pain, leading to a revised CDC Guideline for Prescribing Opioids for Chronic Pain [38]. This caused the 2019 opioid dispensing rate to fall to its lowest rate in 14 years (still high at 46.7 prescriptions per 100 persons vs 81.3 prescriptions per 100 persons in 2012, the peak of opioid prescribing) [39]. Several medications could be used in place of fentanyl for long-term and acute treatment. Even in the case of an emergency in which a patient could not report their vaccination status, anesthesia would involve a combination of agents titrated to effect. Finally, potential theoretical adverse consequences of eliciting antibodies to endogenous opioids are seen to be very unlikely, as the antibodies targeted to the hapten small molecule pharmacophore (ie, fentanyl) are formulated with immunogenic carrier proteins, forming a unique 3-dimensional structure. As such, as with any traditional vaccine approach, antibodies targeted to epitopes present on the hapten carrier are therefore immunologically unique and should have very limited or no overlap with endogenous opioids peptide families [40]. Furthermore, during the development process of each vaccine product, the epitopes targeted by fentanyl specific antibodies are normally confirmed to have limited or ideally no cross-reactivity in vitro with multiple other small molecule opioids, thus adding confidence to the specificity of the targeted hapten. Here, our findings underscore the importance of accurate information, including options for alternative pain management, when considering vaccination. Reactions to brief vignettes illustrate the complexity of decision-making regarding vaccine candidacy. Results point to the need for individual consideration and assessment to facilitate vaccine decision making.
LIMITATIONS
This is the first study to explore the acceptability to the lay public and to persons with SUD of a fentanyl vaccine strategy to prevent opioid overdose. Though somewhat small and non-representative, our entirely opt-in sample included a range of stakeholders and persons with different relations to OUD/OD and SUD prevention and treatment programs. We note that samples less directly impacted by or interested in OUD and OD may hold different and less favorable views. Qualitative research is vulnerable to reporting and interpretation biases. To protect against bias, we used trained staff, consensus and double coding of data, a structured interview guide, and standardized vignettes. Vignettes were also helpful in “making real” the concept of a novel vaccine, as the study sought to explore reactions to a medical innovation that is under development.
CONCLUSIONS
Initial exploration indicates positive response and appreciation for the complexity of a vaccine strategy to prevent fentanyl overdose, especially in the setting of pain, a risk factor for OUD, and questions about durability. Findings suggest need to focus future research on operational, ethical, and communications issues of a novel fentanyl vaccine in parallel with vaccine discovery and development.
Contributor Information
Elissa R Weitzman, Division of Adolescent/Young Adult Medicine, Boston Children’s Hospital, Boston, Massachusetts, USA; Computational Health Informatics Program, Boston Children’s Hospital, Boston, Massachusetts, USA; Department of Pediatrics, Harvard Medical School, Boston, Massachusetts, USA.
Joe Kossowsky, Department of Pediatrics, Harvard Medical School, Boston, Massachusetts, USA; Department of Anesthesiology, Critical Care and Pain Medicine, Boston Children’s Hospital, Boston, Massachusetts, USA.
Laura M Blakemore, Division of Adolescent/Young Adult Medicine, Boston Children’s Hospital, Boston, Massachusetts, USA.
Rachele Cox, Division of Adolescent/Young Adult Medicine, Boston Children’s Hospital, Boston, Massachusetts, USA.
David J Dowling, Department of Pediatrics, Harvard Medical School, Boston, Massachusetts, USA; Precision Vaccines Program, Boston Children’s Hospital, Boston, Massachusetts, USA; Division of Infectious Diseases, Boston Children’s Hospital, Boston, Massachusetts, USA.
Ofer Levy, Department of Pediatrics, Harvard Medical School, Boston, Massachusetts, USA; Precision Vaccines Program, Boston Children’s Hospital, Boston, Massachusetts, USA; Division of Infectious Diseases, Boston Children’s Hospital, Boston, Massachusetts, USA; Broad Institute of MIT & Harvard, Cambridge, Massachusetts, USA.
Emma W Needles, Adolescent Substance Use and Addiction Program, Division of Developmental Medicine, Boston Children’s Hospital, Boston, Massachusetts, USA.
Sharon Levy, Department of Pediatrics, Harvard Medical School, Boston, Massachusetts, USA; Adolescent Substance Use and Addiction Program, Division of Developmental Medicine, Boston Children’s Hospital, Boston, Massachusetts, USA.
Notes
Acknowledgments . The authors gratefully acknowledge Melissa Brogna, Julie Lunstead, Rebecca H. Atherton, Melanie E. Floyd, and Leslie A. Kenefick for help with research interviews and analysis, Kristin Johnson for Figure 1 artwork, and Gary Fleisher, MD, for expert support of the PVP.
Financial support . Funding for this project was provided by the National Institutes of Health (NIH) Helping to End Addiction Long-term (HEAL) initiative via National Institute of Allergy and Infectious Diseases (NIAID) contracts HHSN272201800047C and 75N93020C00038. The Precision Vaccines Program is supported in part by Boston Children’s Hospital’s Department of Pediatrics and Chief Scientific Office.
Supplement sponsorship . This supplement is sponsored by the Precision Vaccines Program of Boston Children’s Hospital.
References
- 1. Drug Policy Alliance . Drug Overdose | Drug Policy Alliance. 2020. Available at:https://drugpolicy.org/issues/drug-overdose. Accessed 21 February 2021.
- 2. Lozano G. The opioid crisis and life expectancy in the US. University of Pennsylvania, 2020. 1–26. [Google Scholar]
- 3. Drug Overdose Deaths in the U.S. Top 100,000 Annually. 2021. Available at:https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2021/20211117.htm. Accessed 8 December 2021.
- 4. Prevention C for DC and. Synthetic Opioid Overdose Data | Drug Overdose | CDC Injury Center. 2021. Available at: https://www.cdc.gov/drugoverdose/deaths/synthetic/index.html. Accessed 22 December 2021.
- 5. Jones CM, Einstein EB, Compton WM. Changes in synthetic opioid involvement in drug overdose deaths in the United States, 2010–2016. JAMA 2018; 319:1819–21. Available at: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2018.2844. Accessed 31 May 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NIDA . Overdose Death Rates | National Institute on Drug Abuse (NIDA). 2019. Available at: https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates. Accessed 23 February 2021.
- 7. Products - Vital Statistics Rapid Release - Provisional Drug Overdose Data. Available at: https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm. Accessed 26 December 2021.
- 8. Center for Disease Control and Prevention . CDC’s Response to the Opioid Overdose Epidemic. 2019. Available at: https://www.cdc.gov/opioids/strategy.html. Accessed 21 February 2021.
- 9. Soni D, Bobbala S, Li S, Scott EA, Dowling DJ. The sixth revolution in pediatric vaccinology: immunoengineering and delivery systems. Pediatr Res 2021; 89:1364–72. Available at: 10.1038/s41390-020-01112-y. Accessed 21 February 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maurer P, Bachmann MF. Vaccination against nicotine: an emerging therapy for tobacco dependence. Expert Opin Investig Drugs 2007; 16:1775–83. Available at:https://pubmed.ncbi.nlm.nih.gov/17970637/. Accessed 8 December 2021. [DOI] [PubMed] [Google Scholar]
- 11. Cerny EH, Cerny T. Vaccines against nicotine. HumanVaccines 2009; 5:200–5. Available at:https://pubmed.ncbi.nlm.nih.gov/19276649/. Accessed 8 December 2021. [DOI] [PubMed] [Google Scholar]
- 12. Zalewska-Kaszubska J. Is immunotherapy an opportunity for effective treatment of drug addiction? Vaccine 2015; 33:6545–51. Available at:https://pubmed.ncbi.nlm.nih.gov/26432911/. Accessed 18 February 2021. [DOI] [PubMed] [Google Scholar]
- 13. Smith LC, George O. Advances in smoking cessation pharmacotherapy: Non-nicotinic approaches in animal models. Neuropharmacology 2020; 178:108225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Xu A, Kosten TR. Current status of immunotherapies for addiction. Ann N Y Acad Sci 2020; 1489:3–16. Available at:https://onlinelibrary.wiley.com/doi/abs/10.1111/nyas.14329. Accessed 18 February 2021. [DOI] [PubMed] [Google Scholar]
- 15. Banks ML, Olson ME, Janda KD. Immunopharmacotherapies for treating opioid use disorder. Trends in Pharmacol Sci 2018; 39:908–11. Available at:https://pubmed.ncbi.nlm.nih.gov/30343725/. Accessed 17 November 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wandner LD, Aklin WM, Freed MC. Guest editorial: Psychologists aim to HEAL the opioid and pain crises. Am Psychol 2020; 75:866–8. Available at: /record/2020-65461-011. Accessed 21 February 2021. [DOI] [PubMed] [Google Scholar]
- 17. Nanishi E, Dowling DJ, Levy O. Toward precision adjuvants: optimizing science and safety. Curr Opin Pediatr 2020; 32:125–38. Available at:https://pubmed.ncbi.nlm.nih.gov/31904601/. Accessed 26 December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hudgins JD, Porter JJ, Monuteaux MC, Bourgeois FT. Prescription opioid use and misuse among adolescents and young adults in the United States: A national survey study. PLoS Med 2019; 16:e1002922. Available at:https://pubmed.ncbi.nlm.nih.gov/31689290/. Accessed 23 February 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bohm MK, Clayton HB. Nonmedical use of prescription opioids, heroin use, injection drug use, and overdose mortality in U.S. adolescents. J Stud Alcohol Drugs 2020; 81:484–8. Available at:https://pubmed.ncbi.nlm.nih.gov/32800085/. Accessed 23 February 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. NIDA . Marijuana use at historic high among college-aged adults in 2020. Available at:https://www.drugabuse.gov/news-events/news-releases/2021/09/marijuana-use-at-historic-high-among-college-aged-adults-in-2020. Accessed 20 December 2021.
- 21. Kronstrand R, Guerrieri D, Vikingsson S, Wohlfarth A, Gréen H. Fatal poisonings associated with new psychoactive substances. Handb Exp Pharmacol 2018; 252:495–541. Available at:https://pubmed.ncbi.nlm.nih.gov/30105471/. Accessed 8 December 2021. [DOI] [PubMed] [Google Scholar]
- 22. Dahlhamer J, Lucas J, Zelaya C, et al. . Prevalence of chronic pain and high-impact chronic pain among adults—United States, 2016. MMWR Morb Mortal Wkly Rep 2018; 67:1001–6. Available at:http://www.cdc.gov/mmwr/volumes/67/wr/mm6736a2.htm?s_cid=mm6736a2_w. Accessed 17 February 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dahlhamer JM, Connor EM, Bose J, Lucas JW, Zelaya CE. Prescription opioid use among adults with chronic pain: United States, 2019. Natl Health Stat Report 2021; 162:1–9. Available at: https://www.cdc.gov/nchs/products/index.htm. Accessed 8 December 2021. [PubMed] [Google Scholar]
- 24. Vowles KE, McEntee ML, Julnes PS, et al. Rates of opioid misuse, abuse, and addiction in chronic pain: a systematic review and data synthesis. Pain 2015; 156:569–76. Available at:https://pubmed.ncbi.nlm.nih.gov/25785523/. Accessed 18 February 2021. [DOI] [PubMed] [Google Scholar]
- 25. Wills TA, Pokhrel P, Morehouse E, et al. Behavioral and emotional regulation and adolescent substance use problems: a test of moderation effects in a dual-process model. Psychol Addict Behav 2011; 25:279. Available at: https://www.semanticscholar.org/paper/Behavioral-and-emotional-regulation-and-adolescent-Wills-Pokhrel/77a70ba4f7d74b784a7d8027ce37a40ffc52186a. Accessed 8 December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hyshka E, Morris H, Anderson-Baron J, Nixon L, Dong K, Salvalaggio G. Patient perspectives on a harm reduction-oriented addiction medicine consultation team implemented in a large acute care hospital. Drug Alcohol Depend 2019; 204:107523. Available at: https://pubmed.ncbi.nlm.nih.gov/31541875/. Accessed 15 December 2021. [DOI] [PubMed] [Google Scholar]
- 27. Dunleavy K, Hope V, Roy K, Taylor A. The experiences of people who inject drugs of skin and soft tissue infections and harm reduction: A qualitative study. Int J Drug Policy 2019; 65:65–72. Available at:https://pubmed.ncbi.nlm.nih.gov/30665085/. Accessed 15 December 2021. [DOI] [PubMed] [Google Scholar]
- 28. Mahon LR, Hawthorne AN, Lee J, Blue H, Palombi L. Assessing pharmacy student experience with knowledge of and attitudes towards harm reduction: Illuminating barriers to pharmacist-led harm reduction. Harm Reduct J 2018; 15:1–14. Available at:https://link.springer.com/articles/10.1186/s12954-018-0262-6. Accessed 15 December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Knickman J, Krishnan KRR, Pincus HA, et al. . Improving access to effective care for people who have mental health and substance use disorders: a vital direction for health and health care. NAM Perspectives 2016; 6. Available at: https://nam.edu/improving-access-to-effective-care-for-people-who-have-mental-health-and-substance-use-disorders-a-vital-direction-for-health-and-health-care/. Accessed 9 December 2021. [Google Scholar]
- 30. Larson H. Stuck: how vaccine rumors start and why they don’t go away. Oxford University Press, 2020. [Google Scholar]
- 31. The Lancet Child & Adolescent Health . Vaccine hesitancy: a generation at risk. Lancet Child Adolesc Health 2019; 3:281. Available at: www.thelancet.com/child-adolescent. Accessed 23 February 2021. [DOI] [PubMed] [Google Scholar]
- 32. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19:349–57. Available at:https://academic.oup.com/intqhc/article-lookup/doi/10.1093/intqhc/mzm042. Accessed 29 October 2017. [DOI] [PubMed] [Google Scholar]
- 33. QSR International Pty Ltd . Qualitative Data Analysis Software | NVivo. 2020. Available at: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home?_ga=2.203905616.1190173117.1634223163-1109214206.1634223163. Accessed 13 October 2021.
- 34. Lagisetty P, Klasa K, Bush C, Heisler M, Chopra V, Bohnert A. Primary care models for treating opioid use disorders: What actually works? A systematic review. PLoS One 2017; 12:e0186315. Available at: https://pubmed.ncbi.nlm.nih.gov/29040331/. Accessed 15 December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Oesterle TS, Thusius NJ, Rummans TA, Gold MS. Medication-assisted treatment for opioid-use disorder. Mayo Clin Proc 2019; 94:2072–86. Available at:https://pubmed.ncbi.nlm.nih.gov/31543255/. Accessed 15 December 2021. [DOI] [PubMed] [Google Scholar]
- 36. Salsitz E, Wiegand T. Pharmacotherapy of opioid addiction: “Putting a real face on a false demon”. J Med Toxicol 2016; 12:58–63. Available at:https://pubmed.ncbi.nlm.nih.gov/26567033/. Accessed 15 December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wartenweiler V, Chung G, Stewart A, Wenthur C. Pharmacy stakeholder reports on ethical and logistical considerations in anti-opioid vaccine development. BMC Med Ethics 2021; 22:1–18. Available at:https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00599-2. Accessed 21 December 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recommend Rep 2016; 65:1–49. Available at: http://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1er.htm. Accessed 22 April 2019. [DOI] [PubMed] [Google Scholar]
- 39. U.S. Opioid Dispensing Rate Maps | Drug Overdose | CDC Injury Center. Available at: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html. Accessed 21 February 2021.
- 40. Corder G, Castro DC, Bruchas MR, Scherrer G. Endogenous and exogenous opioids in pain HHS public access. Annu Rev Neurosci 2018; 41:453–73. [DOI] [PMC free article] [PubMed] [Google Scholar]