Abstract
Objectives: Oral health personnel are limited in their ability to assess the readiness of patients to make changes to improve oral health. We aimed to develop and test the Stages of Change in Oral Health (SOCOH) model, a scaled index of the stages of change – pre-contemplative, contemplative or active – with particular emphasis on pregnancy. Materials and methods: Items were collected in a self-report questionnaire conducted among a convenience sample of 446 mothers (age range: 14–43 years) pregnant with Aboriginal children in South Australia, Australia. Scales representing openness (four items; Cronbach’s alpha = 0.73), value (four items; Cronbach’s alpha = 0.71), inconvenience (six items; Cronbach’s alpha = 0.79) and permissiveness (four items; Cronbach’s alpha = 0.66) were developed. Participants were categorised according to the Stages of Change model and were evaluated against key self-reported oral health outcomes. Results: Some 11.9% of participants were classified as pre-contemplators, 46.4% as contemplators and 41.7% as active. A higher proportion of active participants had a higher education, last visited a dentist less than a year previously, had no dental fear, owned a toothbrush, brushed the previous day, used toothpaste, had no difficulties paying a $100 dental bill, self-reported their dental health as ‘excellent’ and in the previous 12 months did not experience dental pain, embarrassment related to their dental appearance or difficulties eating food. Conclusions: The SOCOH model offers an internally consistent and valid instrument for detailed assessment of the readiness for change in regarding oral health behaviours in pregnancy and has potential benefits for clinical decision making and research.
Key words: Stages of change, oral health, development, evaluation
INTRODUCTION
It is generally perceived that lack of oral health-related knowledge contributes to poor oral health outcomes1. Whilst this may be a contributing factor for some individuals, providing oral health-related knowledge does not appear to be the only solution in improving oral health outcomes. This is probably because many patients are not ready, or able, to alter existing patterns of oral health behaviours2., 3..
There are many theories of health behaviour change. One of the most widely recognised, the Health Belief Model, hypothesises that four motivating factors determine the likelihood of adopting a recommended preventive health action4. These include the perception of: (i) susceptibility to disease; (ii) perseverance of a disease; (iii) benefits of taking action; and (iv) barriers to taking action. There is criticism, however, that this approach is too simplistic and that to understand health-related behaviours, additional factors such as ethnicity, culture, socio-economic status and environment need to be considered5.
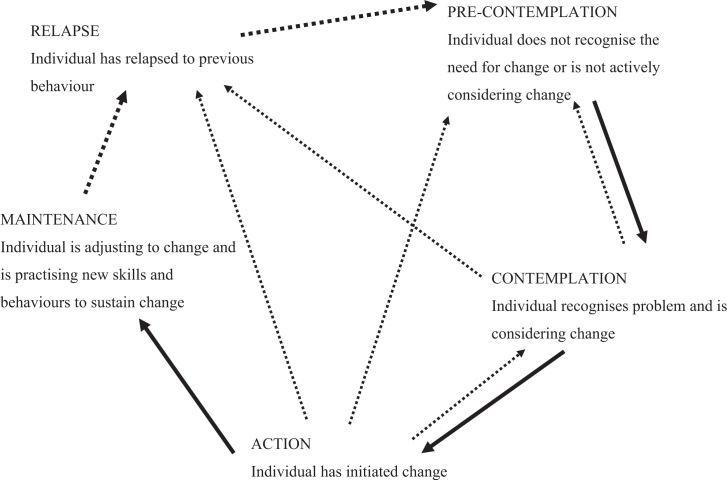
Another relevant model for health-related behaviour is the Trans-Theoretical Model (TTM)6. This model attempts to explain why some people respond quickly to change while others resist. The TTM has five behaviour change stages: ‘pre-contemplation’; ‘contemplation’; ‘action’; ‘maintenance’; and ‘relapse’ (Figure 1). The ‘pre-contemplation’ stage is defined by people not being ready; they are not intending to take action in the foreseeable future and may be unaware that their behaviour is problematic7. ‘Contemplation’ is characterised by ‘people getting ready’; they are beginning to recognise that their behaviour is problematic and are starting to look at the pros and cons of their continued actions. ‘Action’ is defined as people making overt modifications to their problem behaviour or acquiring new healthy behaviours. People in the ‘maintenance’ stage are able to sustain action and are motivated to prevent relapse. At this point, individuals report little temptation and feel confident that they will not return to their old habits as a way of coping. A core construct of TTM is ‘decisional balance’. Decisional balance reflects an individual’s relative weighing of the pros and cons of changing7. The balance between the pros and cons varies depending on which stage of change the individual is in. The cons of changing outweigh the pros in the pre-contemplation stage, the pros surpass the cons in the middle stages, whilst, in the action stage, the pros outweigh the cons8.
Figure 1.
Conceptual schema of ‘Stages of Change’ model (6).
Rollnick et al.9 recommended that, in order to guide individuals along the stages of behavioural change continuum, it was essential to develop ‘stage-appropriate’ interventions tailored to an individual’s specific stage of change. Otherwise, unsolicited offerings of information would potentially be met with resistance and consequently be of limited value9. In the oral health context, assessment of patient readiness to change may be useful in planning how to communicate about non-optimal oral health behaviours. Little work has been done in this field, and of the work that has been done, the emphasis was on parents of children at high risk of early childhood caries (ECC)5., 10.. It could be argued that conducting such research among adult populations at risk of having children with ECC is also beneficial. There is evidence that dental services during pregnancy improve maternal oral health, reduce mother–child transmission of cariogenic bacteria and create opportunities for anticipatory guidance11. However, many women do not see the importance of oral care during pregnancy12, whilst others experience barriers to care, such as not having dental coverage or access to appropriate services13. There are many groups at elevated risk of dental disease during pregnancy, among them Indigenous populations such as Aboriginal groups in Australia. Many reasons have been given for oral health disparities between Australian Aboriginal and non-Aboriginal groups, including financial barriers, inadequate access to dental services, cultural factors, global risk factors and social determinants.
This study had two aims: (i) to develop a Stage of Change in Oral Health (SOCOH) model for pregnancy (SOCOH_preg); and (ii) to evaluate SOCOH_preg against key self-reported oral health outcomes among a convenience sample of women pregnant with Aboriginal children in South Australia, Australia.
METHODS
Conceptual framework
The conceptual framework for SOCOH_preg is underpinned by theoretical constructs of the TTM. This model assumes that change is a process that involves progression through a series of stages (Figure 1)6.
SOCOH_preg development
We established a pregnancy-related SOCOH model specifically for women pregnant with Aboriginal Australian children, based on the work of Weinstein and Riedy10. This included 18 items encompassing four TTM-related domains. Each of these domains evaluated one dimension of behaviour change as theorised by Prochaska and DiClemente6. The domains included: (i) openness to health information (openness); (ii) valuing dental health (value); (iii) inconvenience of implementing healthy oral health behaviours (inconvenience); and (iv) permissiveness regarding consumption of sweet food/beverages (permissiveness). Response options were on a five-point Likert scale, ranging from ‘strongly disagree’ to ‘strongly agree’. Scores were coded from 0 to 4, with high summary scores indicating high levels of the four respective domains.
-
•
The four ‘openness’ items were:
-
•
I would go to the dentist if my midwife, Aboriginal Maternal Infant Care (AMIC) worker or someone close to me told me to do so
-
•
I get advice on taking care of myself during pregnancy from my midwife, AMIC worker or someone close to me
-
•
I feel comfortable asking my midwife, AMIC worker or someone close to me about ways to take care of myself during pregnancy
-
•
It is easy for me to get answers about ways to take care of myself during pregnancy from my midwife, AMIC worker or someone close to me.
The four ‘value’ items were:
-
•
Keeping my teeth healthy is important to me
-
•
I benefit a lot when I clean my teeth
-
•
I like the idea of a dentist working on my teeth to make them strong
-
•
I believe going to the dentist would help my teeth.
The six ‘inconvenience’ items were:
-
•
It is easy for me to forget to brush my teeth
-
•
It would be hard for me to stop snacking on sweet foods and drinks
-
•
I don’t have time to brush every morning and every night
-
•
It is easier to drink sweet drinks like soft drinks rather than water
-
•
It would be hard for me to change how often I brush my teeth
-
•
It is easy for me to go to sleep at night without brushing my teeth.
The four ‘permissiveness’ items were:
-
•
It makes me feel good when I eat or drink something sweet
-
•
Everyone I care about eats or drinks a lot of sweet things
-
•
I feel mean if I don’t allow children to have sweet food
-
•
I don’t like the taste of drinks that are not sweet.
In order to categorise participants as ‘pre-contemplators’, ‘contemplators’ or ‘active’, item responses within each construct were summed. These summed values were ranked and percentiles (tertiles) were calculated for each participant within each construct. The derived percentiles were used to place participants into one of the three stages of change categories (‘pre-contemplation’, ‘contemplation’ or ‘active’; Table 1).
Table 1.
Categorisation of participants to the Stage of Change groups based on construct tertile scores
| Stage | |||
|---|---|---|---|
| Construct | Pre-contemplative | Contemplative | Active |
| Openness | 1 | 2 | 3 |
| Value | 1 | 2 | 3 |
| Inconvenience | x | 2 | 1 |
| Permissiveness | x | 2 | 1 |
1, lowest tertile; not agree with construct. 3, highest tertile; agree with construct. x, not used.
Participants whose scores fell within the lowest tertile on the ‘openness’ and ‘value’ constructs were placed in the ‘pre-contemplation’ group. Scores falling within the lowest tertile on these two constructs meant that participants showed general disagreement with them. More simply, participants were perceived to be not open to receiving pregnancy-related health information or valuing dental health. If this was the case, the scores on the remaining two constructs were discarded. Participants whose scores fell within the middle tertile on the ‘openness’, ‘value’, ‘inconvenience’ or ‘permissiveness’ constructs were placed in the ‘contemplation’ group. Scores falling within the middle tertile on these constructs meant that participants ‘somewhat agreed’, ‘somewhat disagreed’, or ‘neither agreed nor disagreed’, demonstrating general ambivalence with them. Such participants were more likely to contemplate change compared with their ‘pre-contemplative’ counterparts, but were possibly plagued by unknown barriers and obstacles.
Participants whose scores fell within the highest tertile on the ‘openness’ and ‘value’ constructs and the lowest tertile for the ‘inconvenience’ and ‘permissiveness’ constructs were placed in the ‘action’ group. Scores falling within the highest tertile on the ‘openness’ and ‘value’ constructs meant that participants showed strong agreement with them, but strong disagreement with the ‘inconvenience’ and ‘permissiveness’ constructs. Participants in the ‘action’ group were more likely to be open to pregnancy-related health information, to value dental health, to not be inconvenienced or to have difficulty with changing oral health-related behaviours, and were not inappropriately permissive regarding sweet food or beverage consumption.
Study participants
To be eligible, participants needed to be pregnant residents of South Australia, expecting an Aboriginal Australian baby or babies or to have recently delivered an Aboriginal Australian baby or babies (infants <6 weeks of age).
Recruitment
Recruitment occurred from February 2011 to May 2012. Participants were recruited from a range of sources from throughout South Australia, including referrals from Aboriginal groups, community services and hospitals. Promotion of the study occurred via advertisements in community and hospital newsletters, posters in hospitals and community centres and by word of mouth. Questionnaires were completed in the participant’s home or in cafes, libraries, hospitals, community halls, Aboriginal resource centres and workplaces. Participants were provided with written and verbal information about the study before giving consent and received a $50 gift voucher upon completion of the questionnaire in acknowledgement of the time spent in completing the form.
Pilot testing
The SOCOH_preg instrument was pilot tested among the study’s Aboriginal reference group, Aboriginal community members and locally employed AMIC workers. Slight amendments were made to the wording, to improve clarity, but no other changes were made.
Data collection
Data were collected via questionnaires administered by both Aboriginal and non-Aboriginal project officers. The questionnaires were completed either independently by participants or through interview. The project officers had a scripted method of introducing and administering the questionnaire.
Ethics
This study received approval from the University of Adelaide Human Research Ethics Committee, the Aboriginal Health Council of South Australia, the Government of South Australia, the Human Research Ethics Committee of Child, Youth and Women’s Health Service and the Human Research Ethics Committees of the participating Adelaide hospitals. The research was conducted in full accordance with the World Medical Association Declaration of Helsinki. Written informed consent was obtained from all participants.
Content validity
Content validity is a measure of the extent to which an instrument encompasses the relevant aspects of the concepts it aims to measure; the relevance of these aspects is based on the judgments of experts and lay groups14. Content validity in this study was established by means of literature searches, a review of the questionnaire by experts and a review of the questionnaire by the study’s Aboriginal Reference Group. All sources indicated that the SOCOH_preg adequately encompassed the domains under investigation and had a sufficient number of items.
Internal reliability
Exploratory Factor Analysis (factor analysis/correlation, principal components method), followed by orthogonal varimax (Kaiser off) rotation was carried out for the final solution to inform scale construction. Items for the four distinct domains were entered separately.
Internal consistency
Internal consistency is a measure of reliability that assesses the degree to which items are related to each other; it measures a unified construct15. Cronbach’s α was determined for each scale, as a measure of overall item consistency. A Cronbach’s α coefficient of 0.70 or higher is considered satisfactory16.
Discriminative ability
Statistically significant differences in scale scores between relevant oral health-related factors offer evidence of an instrument’s ability to discriminate between groups. Specific oral health-related factors in this study included demography (age, number of weeks pregnant, expecting first child, have other children, care for other children, Aboriginal or Torres Strait Islander), sociodemography (education, income, ownership of a means-tested government health care card, number of people in household the previous night, car ownership), dentate status (number of teeth, experience of extraction), dental cost (avoided dental care because of cost, difficulty paying $100 dental bill), self-rated health (self-rated general health, self-rated oral health), dental perceptions (dental fear, need filling, need extraction, have gum disease) and oral health impairment (toothache, uncomfortable about appearance, unable to eat food). Two summary oral health impairment items were constructed. Oral health impairment_any was considered a response of ‘very often’, ‘often’ or ‘sometimes’ to the items ‘How often in the past year…did you have toothache?’, ‘…did you feel uncomfortable about the way your teeth looked?’ OR ‘…could you not eat some foods or had to eat slowly because of problems with your teeth?’. Oral health impairment_all was considered a response of ‘very often’, ‘often’ or ‘sometimes’ to the items ‘How often in the past year…did you have toothache?’, ‘…did you feel uncomfortable about the way your teeth looked?’ AND ‘…could you not eat some foods or had to eat slowly because of problems with your teeth?’17.
RESULTS
A total of 446 women pregnant with Aboriginal or Torres Strait Islander children completed all components of the SOCOH_preg questionnaire. The age range was 14–43 years, with the median age being 24.9 years. Around four-fifths (79.5%) were 37 weeks pregnant or less and just under two-fifths (38.5%) were pregnant with their first child. Among those who were not pregnant with their first child, 42.8% already had four or more children. Among all participants, 68.2% cared for children who were not their own. Most (83.2%) participants identified as being Aboriginal or Torres Strait Islander, and the highest educational attainment for 71.6% of participants was high school or less. Nearly 90% (85.9%) of participants were unemployed, with 82.2% owning a means-tested government health care card. Over one-third (34.7%) of participants reported five or more people staying in their house the previous night and nearly half (49.1%) did not own a car.
Internal consistency for each of the four constructs was indicated by Cronbach’s alpha, ranging from 0.66 (permissiveness) to 0.79 (inconvenience; Table 2). Mean item scores for the four constructs were as follows: openness, 13.7 (possible range 0–16); value, 14.6 (possible range 0–16); inconvenience, 11.5 (possible range 0–24); and permissiveness, 8.8 (possible range 0–16) (Table 3). Using the algorithm described, 53 (11.9%) participants were described as ‘pre-contemplative’, 207 (46.4%) as ‘contemplative’ and 186 (41.7%) as ‘active’ in regard to the TTM.
Table 2.
Factor analysis of Stages of Change in Oral Health subscales
| Item | Subscale | |||
|---|---|---|---|---|
| Openness | Value | Inconvenience | Permissiveness | |
| I would go to the dentist if told to do so | 0.67 | |||
| I get advice on taking care of myself during pregnancy | 0.76 | |||
| I feel comfortable asking about ways to take care of myself during pregnancy | 0.83 | |||
| It is easy for me to get answers about ways to take care of myself during pregnancy | 0.76 | |||
| Keeping my teeth healthy is important to me | 0.82 | |||
| I benefit a lot when I clean my teeth | 0.80 | |||
| I like the idea of a dentist working on my teeth | 0.69 | |||
| I believe going to the dentist would help my teeth | 0.64 | |||
| It is easy for me to forget to brush my teeth | 0.70 | |||
| It would be hard stop snacking on sweet foods and drinks | 0.65 | |||
| I don’t have time to brush every morning and every night | 0.77 | |||
| It is easier to drink sweet drinks than water | 0.63 | |||
| It would be hard to change how often I brush my teeth | 0.65 | |||
| It is easy to sleep at night without brushing my teeth | 0.75 | |||
| It makes me feel good when I eat or drink something sweet | 0.68 | |||
| Everyone I care about eats or drinks a lot of sweet things | 0.64 | |||
| I feel mean if I don’t allow children to have sweet food | 0.76 | |||
| I don’t like the taste of drinks that are not sweet | 0.74 | |||
| Eigenvalue | 2.29 | 2.20 | 2.96 | 1.99 |
| Variance accounted for (%) | 59.2 | 55.1 | 49.4 | 49.6 |
| Internal reliability (Cronbach’s alpha) | 0.73 | 0.71 | 0.79 | 0.66 |
Table 3.
Descriptive values of Stages of Change in Oral Health subscales
| Openness* Four items Possible range 0–16; high scores = high openness | Value† Four items Possible range 0–16; high scores = high value | Inconvenience‡ Six items Possible range 0–24; high scores = high inconvenience | Permissiveness§ Four items Possible range 0–16; high scores = high permissiveness | |
|---|---|---|---|---|
| Mean (95% CI) | 13.7 (13.4–14.0) | 14.6 (14.4–14.8) | 11.5 (11.0–12.0) | 8.8 (8.4–9.2) |
| SE | 0.13 | 0.09 | 0.27 | 0.19 |
| Median | 15.0 | 16.0 | 12.0 | 9.00 |
| Mode | 16.0 | 16.0 | 12.0 | 6.00 |
| Range | 16.0 | 8.0 | 24.0 | 16.00 |
| Minimum | 0.0 | 8.0 | 0.0 | 0.00 |
| Maximum | 16.0 | 16.0 | 24.0 | 16.00 |
| n lowest tertile (%) | 141 (31.8) | 107 (24.0) | 140 (31.6) | 139 (31.4) |
| n middle tertile (%) | 117 (26.4) | 100 (22.5) | 132 (29.8) | 150 (33.9) |
| n highest tertile (%) | 186 (41.9) | 238 (53.5) | 171 (38.6) | 154 (34.8) |
Openness: lowest tertile, 0–12; middle tertile, 13–15; highest tertile, 16.
Value: lowest tertile, 0–13; middle tertile, 14–15; highest tertile, 16.
Inconvenience: lowest tertile, 0–8; middle tertile, 9–13; highest tertile, 14+.
Permissiveness: lowest tertile, 0–6; middle tertile, 7–10; highest tertile, 11+.
95% CI, 95% confidence interval; SE, standard error.
SOCOH_preg indicated good discriminative ability, with a higher proportion of participants classified as ‘active’ having attained high school or greater education, owning a car, last seeing a dentist <1 year ago, not being scared of the dentist, owning a toothbrush, brushing teeth the previous day, using toothpaste and not experiencing difficulty paying a $100 dental bill (Table 4). Discriminative ability was also indicated with self-rated general and oral health, and oral health impairment, with a higher proportions of participants classified as ‘active’ having ‘excellent, very good or good’ self-rated oral health, no experience of bleeding gums, not feeling uncomfortable about appearance of teeth, not having to avoid food because of problems with teeth and oral health impairment_any (Table 5).
Table 4.
Sociodemographic and dental behaviour characteristics according to Stages of Change groups
| Characteristic | Group | |||
|---|---|---|---|---|
| Total | Pre-contemplative | Contemplative | Active | |
| Total | 446 | 53 (11.9) | 207 (46.4) | 186 (41.7) |
| Age (years) | ||||
| 14–24 years | 221 (52.2) | 28 (53.8) | 98 (51.0) | 95 (53.1) |
| 25+ years | 202 (47.8) | 24 (46.2) | 94 (49.0) | 84 (46.9) |
| Education | ||||
| ≤High school | 317 (71.6) | 42 (80.8) | 154 (74.8) | 121 (65.4)* |
| >High school | 126 (28.4) | 10 (19.2) | 52 (25.2) | 64 (34.6) |
| Income | ||||
| Job | 62 (14.1) | 2 (3.9) | 29 (14.1) | 31 (16.8) |
| Centrelink | 379 (85.9) | 49 (96.1) | 177 (85.9) | 153 (83.2) |
| HCC | ||||
| Yes | 356 (82.2) | 45 (88.2) | 169 (84.5) | 142 (78.0) |
| No | 77 (17.8) | 6 (11.8) | 31 (15.5) | 40 (22.0) |
| Car own | ||||
| Yes | 225 (50.9) | 21 (40.4) | 98 (47.6) | 106 (57.6)* |
| No | 217 (49.1) | 31 (59.6) | 108 (52.4) | 78 (42.4) |
| When last saw dentist | ||||
| <1 year ago | 152 (35.3) | 9 (18.0) | 71 (35.3) | 72 (40.0)* |
| 1+ years ago | 279 (64.7) | 41 (82.0) | 130 (64.7) | 108 (60.0) |
| Where last saw dentist | ||||
| ACHO/public/SDS | 315 (73.9) | 42 (84.0) | 150 (76.1) | 123 (68.7) |
| Private | 111 (26.1) | 8 (16.0) | 47 (23.9) | 56 (31.3) |
| Scared of dentist | ||||
| No | 263 (59.5) | 27 (51.9) | 111 (54.1) | 125 (67.6)* |
| Little bit, fair bit, heaps | 179 (40.5) | 25 (48.1) | 94 (45.9) | 60 (32.4) |
| Own a toothbrush | ||||
| Yes | 416 (93.9) | 43 (82.7) | 197 (95.6) | 176 (95.1)* |
| No | 27 (6.1) | 9 (17.3) | 9 (4.4) | 9 (4.9) |
| Brushed yesterday | ||||
| Yes | 320 (75.1) | 25 (54.3) | 140 (70.0) | 155 (86.1)* |
| No | 106 (24.9) | 21 (45.7) | 60 (30.0) | 25 (13.9) |
| Use toothpaste | ||||
| Yes | 416 (97.7) | 42 (91.3) | 197 (98.5) | 177 (98.3)* |
| No | 10 (2.3) | 4 (8.7) | 3 (1.5) | 3 (1.7) |
| Not gone to dentist because of cost | ||||
| Yes | 157 (35.5) | 20 (38.5) | 72 (35.1) | 65 (35.1) |
| No | 285 (64.5) | 32 (61.5) | 133 (64.9) | 120 (64.9) |
| Hard to pay $100 dental bill? | ||||
| Not hard at all or not very hard | 87 (19.7) | 3 (5.8) | 31 (15.1) | 53 (28.8)* |
| A little bit or very hard, or could not pay | 354 (80.3) | 49 (94.2) | 174 (84.9) | 131 (71.2) |
Values are given as n (%). P < 0.05. ACHO; HCC; SDS.
Table 5.
Self-rated health/oral health and oral health impairment characteristics according to Stages of Change groups
| Characteristic | Group | |||
|---|---|---|---|---|
| Total | Pre-contemplative | Contemplative | Active | |
| How do rate general health | ||||
| Excellent, very good or good | 402 (90.3) | 47 (88.7) | 183 (88.8) | 172 (92.5) |
| Fair or poor | 43 (9.7) | 6 (11.3) | 23 (11.2) | 14 (7.5) |
| How do rate oral health | ||||
| Excellent, very good or good | 204 (45.7) | 16 (30.2) | 86 (41.5) | 102 (54.8)* |
| Fair or poor | 242 (54.3) | 37 (69.8) | 121 (58.5) | 84 (45.2) |
| Compared with general health, how do you rate dental health | ||||
| Excellent, very good or good | 213 (48.2) | 16 (30.2) | 90 (43.9) | 107 (58.2)* |
| Fair or poor | 229 (51.8) | 37 (69.8) | 115 (56.1) | 77 (41.8) |
| Need fillings? | ||||
| Yes | 292 (65.9) | 33 (63.5) | 143 (69.8) | 116 (62.4) |
| No | 151 (34.1) | 19 (36.5) | 62 (30.2) | 70 (37.6) |
| Need teeth pulled out? | ||||
| Yes | 222 (50.3) | 28 (52.8) | 109 (53.4) | 85 (46.2) |
| No | 219 (49.7) | 25 (47.2) | 95 (46.6) | 99 (53.8) |
| Have gum disease/bleeding gums? | ||||
| Yes | 190 (42.8) | 28 (53.8) | 102 (49.3) | 60 (32.4)* |
| No | 254 (57.2) | 24 (46.2) | 105 (50.7) | 125 (67.6) |
| How often during the last year….did you have toothache? | ||||
| Very often, fairly often or sometimes | 245 (54.9) | 30 (56.6) | 121 (58.5) | 94 (50.5) |
| Hardly ever or never | 201 (45.1) | 23 (43.4) | 86 (41.5) | 92 (49.5) |
| ….did you feel uncomfortable about the way your teeth looked? | ||||
| Very often, fairly often or sometimes | 274 (61.6) | 37 (69.8) | 145 (70.4) | 92 (49.5)* |
| Hardly ever or never | 171 (38.4) | 16 (30.2) | 61 (29.6) | 94 (50.5) |
| ….did you have to avoid eating some foods because of problems with your teeth? | ||||
| Very often, fairly often or sometimes | 240 (54.1) | 31 (58.5) | 122 (59.2) | 87 (47.0)* |
| Hardly ever or never | 204 (45.9) | 22 (41.5) | 84 (40.8) | 98 (53.0) |
| In the last year, did you have toothache OR felt uncomfortable about appearance OR avoided foods very often, fairly often or sometimes? | ||||
| Yes | 351 (78.7) | 47 (88.7) | 171 (82.6) | 133 (71.5)* |
| No | 95 (21.3) | 6 (11.3) | 36 (17.4) | 53 (28.5) |
| In the last year, did you have toothache AND felt uncomfortable about appearance AND avoided foods very often, fairly often or sometimes? | ||||
| Yes | 151 (33.9) | 20 (37.7) | 85 (41.6) | 46 (24.7)* |
| No | 295 (66.1) | 33 (62.3) | 122 (58.9) | 140 (75.3) |
P < 0.05.
DISCUSSION
In this study, a SOCOH model for pregnancy with some internally consistent and valid properties was successfully developed. Content and discriminative validity were ascertained, with the model having statistically significant associations with key self-reported oral health outcomes in the expected directions. For example, those classified as ‘pre-contemplators’ and ‘contemplators’ had poorer self-rated oral health and greater oral health impact than those classified as ‘active’. The majority of participants were contemplators, suggesting that they were willing to consider oral health behaviour change. This knowledge may be important for predicting the potential success of an intervention. For example, assessing stage of change in oral health in pregnancy may be valuable in helping participants understand how to change behaviours that place their oral health, and the oral health of their child, at risk.
The scale may be useful for clinicians hoping to ascertain the current motivation, or otherwise, of parents to engage in oral health-promoting behaviours with their children. In other words, being aware of a parent’s stage of change (‘pre-contemplative’, ‘contemplative’ or ‘active’) may aid the clinician in understanding how best to communicate with parents regarding oral health-related behaviours that place their child at risk. Specifically, ‘pre-contemplative’ individuals would be recognised as having low openness to health-related information as well as low value of oral health. Such individuals may be unaware that dental disease is promoted by infectious bacteria that can be transmitted from caretaker to child. However, giving advice at this stage is likely to be counter-productive, as it may engender resistance or cause individuals to think prematurely about barriers to change. Motivational Interviewing may be one approach to use, whereby the clinician asks a series of open-ended questions about the problems parents have had with their teeth and what they wish for in the way of dental health for their child. By the clinician’s use of reflective listening, the parental response may help elicit existence of the problem.
Those designated as ‘contemplative’ would be understood to be open to health information and to value dental health, but to find it inconvenient to implement oral health-protective behaviours and to be permissive with regard to consumption of cariogenic foods and beverages. This is the stage most characterised by ambivalence, with individuals weighing both the ‘pros’ and ‘cons’ of changing their behaviour. For example, they may feel that brushing their teeth every evening will be beneficial for their oral health; however, they also feel that by the time evening comes around they are too exhausted to do so. Tipping the balance in favour of change may involve increasing the pros, reducing the cons, or both. Whilst an advice-giving approach would not be detrimental at this stage, providing individuals with choices or a menu of options to discuss and choose from may be more effective.
Conversely, ‘active’ individuals would be recognised as being open to health-related information, valuing dental health, not being inconvenienced by engaging in oral health-protective behaviours and showing restraint regarding consumption of sweet foods and beverages. An important consideration in the action stage is whether the recommended oral health behaviours are acceptable to the individual. One study examining obesity intervention in children found that if the mother found the intervention interesting she was more willing to implement it and affect change in the child’s dietary-related behaviour18. Interventions that focus on psychological approaches compatible with the Stages of Change Theory, such as Motivational Interviewing, may be the most successful. There are some examples of these in the literature specifically pertaining to oral health19., 20., 21., 22..
It is important to compare our findings with others who have developed ‘Stage of Change’ instruments for specific behaviours and/or population groups. Bradford developed the ‘Stages of Relationship Change Questionnaire’ to assist with assessment of couples’ readiness for relationship therapy23. This was a one-factor instrument that measures change along nine domains of marital functioning. Most in Bradford’s sample (n = 406) were in the early stages of change, with men more often in the stage of ‘pre-contemplation’ and women more often in ‘contemplation’. The authors concluded that the instrument was capable of reliably measuring readiness for change and of discriminating between various stages of change with respect to relationship counselling. Mainvil and colleagues developed a scale to measure decisional balance to eat more fruits and vegetables among a representative sample of 2132 adults in New Zealand24. Factor analysis confirmed the existence of three decisional balance subscales, which were labelled ‘health pros’, ‘non-health pros’ and ‘cons’. In general, the subscales followed hypothesised patterns across the stages of change, leading the authors to conclude that the scale was both valid and reliable. Banyard and colleagues developed a ‘Bystander Behaviour and Sexual Violence Stages of Change model’, which encompassed nine items and three subscales (‘pre-contemplation’, ‘contemplation’ and ‘action’)25. Participants who were ‘contemplative’ or ‘active’ were more likely to have engaged in pro-social behaviour to end sexual violence, were less likely to believe rape myths, more likely to feel effective as pro-social bystanders and more likely to see positive reasons to intervene as a bystander in comparison with their ‘pre-contemplative’ counterparts. Individuals with higher contemplation scores also felt more in control in both interpersonal and socio-political situations.
Our study had a number of shortcomings, the largest being the limitation of study participants to women pregnant with Aboriginal children (or having recently given birth to an Aboriginal child). Future research should seek to replicate and extend these findings in a variety of settings and population groups; ideally, nationally representative. Moreover, expansion of the scale to include additional items may facilitate the use of these measures in understanding variability among individuals and their readiness to engage in change efforts to promote oral health. Furthermore, consistent with much previous research on dental disease prevention using behaviour change models, the outcome measures used in this study were predominantly self-reported. Future research, using both clinical and self-reported oral health outcomes, would help to determine the scale’s potential clinical applicability.
In conclusion, our findings indicate some evidence that the Stages of Change theory has utility in understanding the beliefs and behaviours of women who are pregnant with children at high risk of ECC. The SOCOH_preg scale may be helpful in trying to provide a better understanding of, and eventually change, deleterious oral health behaviours among vulnerable populations. Clearly, further validation work is required in other populations, particularly in regard to relapse.
Acknowledgements
Funding was provided by Australia’s National Health and Medical Research Council (NHMRC) International Collaborative Indigenous Health Research Project, grant number 627365. Lisa Jamieson is supported by an NHMRC Career Development Award. We acknowledge and thank the dedicated staff who collected the data; Jessica Merrick, Joanne Hedges, Kirsten Kennington, Louise Bellefemini, Sabina Coulthard and Bev Ellis who conducted data entry. We also acknowledge and thank the study’s Aboriginal Reference Group, key Aboriginal stakeholders from throughout South Australia and the participants, without whom this study would not have been possible.
Competing interests
The authors declare they have no competing interests.
REFERENCES
- 1.Cortés DE, Réategui-Sharpe L, Spiro A, III, et al. Factors affecting children’s oral health: perceptions among Latino parents. J Public Health Dent. 2012;72:82–89. doi: 10.1111/j.1752-7325.2011.00287.x. [DOI] [PubMed] [Google Scholar]
- 2.Benitez C, O’Sullivan D, Tinanoff N. Effect of a preventive approach for the treatment of nursing bottle caries. J Dent Child. 1994;61:46–49. [PubMed] [Google Scholar]
- 3.Harris R, Gamboa A, Dailey Y, et al. One-to-one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database Syst Rev. 2012;3:CD006540. doi: 10.1002/14651858.CD006540.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenstock IM. The health belief model and preventive health behaviour. Health Educ Monogr. 1974;2:354–386. [Google Scholar]
- 5.Amin MS, Harrison RL. A conceptual model of parental behaviour change following a child’s dental general anaesthesia procedure. Pediatr Dent. 2007;29:278–286. [PubMed] [Google Scholar]
- 6.Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy Theory Res Pract. 1982;19:276–288. [Google Scholar]
- 7.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 8.Hall KL, Rossi JS. Meta-analysis Examination of the sting and weak principals across 48 behaviors. Prevent Med. 2008;46:266–274. doi: 10.1016/j.ypmed.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 9.Rollnick S, Heather N, Bell A. Negotiating behavior change in medical settings: the development of brief motivational interviewing. J Ment Health. 1992;1:25–37. [Google Scholar]
- 10.Weinstein P, Riedy CA. The reliability and validity of the RAPIDD scale: readiness assessment of parents concerning infant dental decay. ASDC J Dent Child. 2001;68:129–135. [PubMed] [Google Scholar]
- 11.Li Y, Caufield PW, Dasanayake AP, et al. Mode of delivery and other maternal factors influence the acquisition of Streptococcus mutans in infants. J Dent Res. 2005;84:806–811. doi: 10.1177/154405910508400905. [DOI] [PubMed] [Google Scholar]
- 12.Le M, Riedy C, Weinstein P, et al. Barriers to utilisation of dental services during pregnancy: a qualitative analysis. J Dent Child. 2009;76:46–52. [PMC free article] [PubMed] [Google Scholar]
- 13.Breedlove G. Prioritizing oral health in pregnancy. Kans Nurse. 2004;79:10. [PubMed] [Google Scholar]
- 14.Carmines E, Zeller R. Sage Publications; London: 1986. Reliability and Validity Assessment. [Google Scholar]
- 15.Rosenthal R, Rosnow RL. McGraw-Hill; Boston, MA: 1991. Essentials of Behavioral Research: Methods and Data Analysis. [Google Scholar]
- 16.Nunnally JC, Bernstein IH. Mcgraw-Hill; New York: 1994. Psychometric Theory. [Google Scholar]
- 17.Jamieson LM, Mejía GC, Slade GD, et al. Risk factors for impaired oral health among 18- to 34-year-old Australians. J Public Health Dent. 2010;70:115–123. doi: 10.1111/j.1752-7325.2009.00151.x. [DOI] [PubMed] [Google Scholar]
- 18.Barlow J, Whitlock S, Hanson S, et al. Preventing obesity at weaning: parental views about the EMPOWER programme. Child Care Health Dev. 2010;36:843–849. doi: 10.1111/j.1365-2214.2010.01107.x. [DOI] [PubMed] [Google Scholar]
- 19.Brand V, Bray K, Macneill S, et al. Impact of single-session motivational interviewing on clinical outcomes following periodontal maintenance therapy. Int J Dent Hyg. 2013;11:134–141. doi: 10.1111/idh.12012. [DOI] [PubMed] [Google Scholar]
- 20.Cook PF, Richardson G, Wilson A. Motivational interviewing training to promote Head Start children’s adherence to oral health care recommendations: results of a program evaluation. J Public Health Dent. 2013;73:147–150. doi: 10.1111/j.1752-7325.2012.00357.x. [DOI] [PubMed] [Google Scholar]
- 21.Ismail AI, Ondersma S, Jedele JM, et al. Evaluation of a brief tailored motivational intervention to prevent early childhood caries. Community Dent Oral Epidemiol. 2011;39:433–448. doi: 10.1111/j.1600-0528.2011.00613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jönsson B, Ohrn K, Lindberg P, et al. Evaluation of an individually tailored oral health educational programme on periodontal health. J Clin Periodontol. 2010;37:912–919. doi: 10.1111/j.1600-051X.2010.01590.x. [DOI] [PubMed] [Google Scholar]
- 23.Bradford K. Assessing readiness for couple therapy: the Stages of Relationship Change Questionnaire. J Marital Fam Ther. 2012;38:486–501. doi: 10.1111/j.1752-0606.2010.00211.x. [DOI] [PubMed] [Google Scholar]
- 24.Mainvil LA, Lawson R, Horwath CC, et al. Validated scales to assess adult decisional balance to eat more fruits and vegetables. Appetite. 2010;55:454–465. doi: 10.1016/j.appet.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Banyard VL, Eckstein RP, Moynihan MM. Sexual violence prevention: the role of stages of change. J Interpers Violence. 2010;25:111–135. doi: 10.1177/0886260508329123. [DOI] [PubMed] [Google Scholar]