Opinion statement
The COVID pandemic has transformed our approach to patient care, research, and training in cardio-oncology. While the early phases of the COVID pandemic were exceptionally frightening, we now can reflect on the innovative changes that brought more effective and patient-centered care to our doorsteps: expansion of telemedicine, integration of digital health, wider adoption of cardiac biomarkers, consolidation, and coordination of cardio-oncology testing. Normally, it takes years for health care systems to adopt new technology or modify patient care pathways; however, COVID pushed healthcare providers and the health systems to change at warp speed. All of these innovations have improved our efficacy and provided a more “patient-centered” approach for our cardio-oncology patients. The changes we have made in cardio-oncology will likely remain well beyond the pandemic and continue to grow improving the cardiovascular care of oncology patients.
Keywords: Cardio-oncology, Onco-cardiology, SARS-CoV-2, Telemedicine, Digital health
Introduction
Winston Churchill famously coined the phrase—“Never let a good crisis go to waste” [1]. On March 11, 2020, the World Health Organization declared COVID-19 a global pandemic forcing the world and the healthcare system to rapidly pivot and modify health care delivery. The COVID-19 pandemic and its impact on patients with cancer and cardiovascular disease (CVD) have highlighted the unique vulnerability of this population against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the agent responsible for COVID-19 [2•]. Indeed, not only are patients with cancer and CVD at higher risk of contracting the infection, but data also supports these patients have more severe disease courses and unfavorable outcomes. Cancer patients have compromised immunity and early data out of Wuhan, China demonstrated that cancer patients have an up to five times higher susceptibility to contract SARS-COV-2 [3]. Additionally, data demonstrated that underlying cardiovascular disease was a significant risk factor for being hospitalized with severe cases of COVID infection [4].
Beyond the direct consequences of COVID-19 infection, the pandemic created an enormous impact on the healthcare systems, causing significant delays in screening programs and non-urgent tests as well as stagnating clinical trials. To overcome setbacks from COVID-19 many healthcare systems and scientific committees presented innovative strategies to keep patients as safe as possible while maintaining access. Below, we highlighted some of the various strategies that the cardio-oncology community has implemented: flexible monitoring protocols that include targeted use of cardiac imaging, increased use of biomarkers, expansion of telemedicine, and incorporation of digital health data to enhance the care of this vulnerable population.
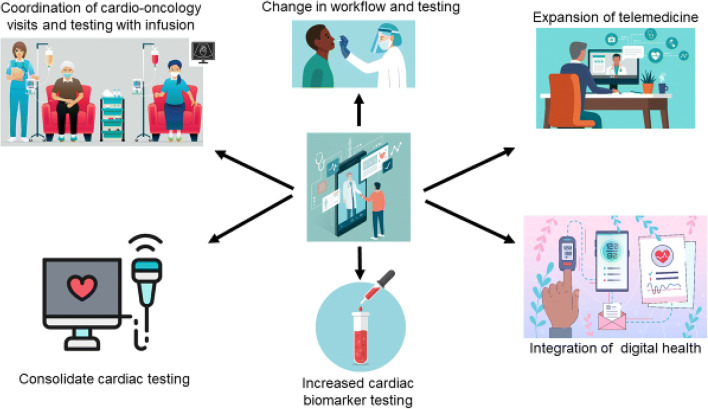
Despite being in the pandemic for over 2 years, approval of vaccines, and boosters, cardio-oncology patients will remain at higher risk than due to a blunted immune response. Many of the principles adopted by the cardio-oncology community during COVID will remain as it continues to make efficient and effective co-management possible through various channels: telemedicine to improve access to patients overburdened with appointments, decreased testing in asymptomatic patients through the incorporation of high sensitivity biomarkers, and integrating digital health data (Fig. 1). Even though we have better therapies and an improved understanding of COVID, the cardio-oncology community will remain nimble and likely continue to pivot as COVID variants emerge and the landscape continues to evolve.
Fig. 1.
Innovative changes in cardio-oncology during COVID-19 pandemic resulted in changes in the clinical workflow and testing for COVID. Clinical practice has seen the expansion of telemedicine and integration of digital health to identify cardiac issues. To decrease burden and exposure, there has been a conscious effort to consolidate cardiac testing and in turn the adoption of more cardiac biomarkers in asymptomatic patients. Additionally, significant efforts have been made to coordinate cardio-oncology visits or testing when patients are already scheduled for infusion or other necessary testing (images from Shutterstock).
Global perspective of cardio-oncology care during the pandemic
During the first part of the pandemic caring for patients with COVID-19 was especially challenging due to critical supply shortages leading to scarce testing and personal protective equipment (PPE), further complicated by, at times, inadequate support in healthcare leadership. In order to understand the global impact of the pandemic, the cardio-oncology community conducted a survey of international colleagues between March and April of 2020 composed of 43 countries. More than 85% of both cardiologists and oncologists adopted telemedicine during the pandemic. Telemedicine was more commonly adopted in academic settings 90.3% versus non- academic affiliated doctors 80.2%. Despite the different technical and operational obstacles of technology, telemedicine was still feasible in many different areas of the world with reports of adoption of telemedicine 88% in the USA, 81% in Europe, and 64% in Latin America [5]. Early on in the pandemic, the international survey demonstrated both cardiologists and oncologists re-scheduled or delayed clinic visits. However, oncologists had a significant lower percentage of altering clinic visits and diagnostic testing (31% versus 81%), likely due to the fact cancer treatment and work-up cannot wait. Oncologists did report treatment modifications were made to balance increased risk of exposure (reported by 72% of oncologists) [5]. Locally, it was observed that if an oncology patient could be changed to a longer time interval between chemotherapy infusions or switched to an oral agent with equal efficacy, these changes were made to minimize COVID exposure.
Data in early 2020 demonstrated that with spread of SARS-CoV-2 in the USA, there were fewer admissions for CVD and a 43% reduction in hospitalization for acute coronary syndrome, acute heart failure, and stroke [6, 7]. It was noted that during the lockdown period, both the USA and Europe saw a dramatic decline in patients presenting with ST elevation myocardial infarction (STEMI), resulting in late presenting myocardial infarctions with higher mortality [8•]. While the lockdown was necessary to preserve PPE, testing, and supplies, the world grappled with how to modify patient care protocols and learn how best to treat this novel disease. Looking back now, we have created a rebound effect of more severe cardiac and (?) cancer-related issues due to the physical lockdown and decreased demand for testing and procedures due to fear COVID.
Triage of patients and cardiac imaging
Triage of patient care
Triage of patient care during the pandemic has largely been dictated by local COVID infectivity rates and hospital volumes. As cardio-oncology is a relatively new field that is not bound by traditional patient care pathways, the practice of cardio-oncology can vary widely by healthcare setting. While there is inherently no one-size-fits all approach to cardio-oncology, some techniques that have been proposed in triaging cardio-oncology patients during the COVID pandemic include the following:
Developing institution-specific triage algorithms to determine whether a patient is most appropriate for an in-person or virtual cardio-oncology visit [9•]
Triaging cardio-oncology patients taking into account cardiovascular disease-related risk, cancer-related risk, and COVID 19-related risk [10•]
Delaying elective electrophysiology and interventional cardiology procedures in cardio-oncology patients
Triage of surveillance cardiac imaging
As a field, contemporary cardio-oncology is largely guided by expert consensus. In an effort to balance the added value of routine cardiac surveillance imaging versus the potential spread of COVID-19, Calvillo-Argüelles et al. in JACC: Cardio-Oncology propose a strategy that prioritizes utilizing cardiac imaging for those at highest risk of cardiotoxicity [11]. Calvillo-Argüelles et al. suggests that baseline cardiac imaging prior to initiation of anthracyclines or trastuzumab may be reserved for those with significant cardiovascular disease, heart failure symptoms, two or more risk factors of cancer therapy–related cardiac dysfunction, high doses of anthracyclines or in the case of trastuzumab, any exposure to anthracyclines. During treatment with anthracyclines, cardiac imaging could be reserved for those with symptoms, doxorubicin-equivalent dosing > 400 mg/m2, doxorubicin-equivalent dosing 250 mg/m2 with existing cardiovascular disease or several risk factors with need for additional anthracycline therapy or per institutional guideline in the setting of diagnosed cancer therapy–related cardiac dysfunction. While the Food and Drug Administration package insert recommends cardiac imaging every 3 months during treatment with trastuzumab, Calvillo-Argüelles et al. suggest that during the COVID-19 pandemic, this strategy is reasonable for those with prior anthracycline exposure, cardiovascular risk factors with normal left ventricular ejection fraction and those with baseline cardiovascular disease, signs of heart failure on exam, or symptoms of prior low normal or reduced left ventricular ejection fraction. For patients who have not received anthracyclines or without cardiovascular disease risk factors imaging at 6 and 12 months of trastuzumab may be reasonable. For patients with metastatic disease, in the first-year cardiac imaging every 6 months for the first year and then no additional imaging is needed if the imaging results were normal and patients are asymptomatic. Finally, in patients who develop cancer treatment–related cardiac dysfunction from trastuzumab, repeat cardiac imaging is reasonable to guide cancer therapy or cardiac medications. Routine post-anthracycline or trastuzumab cardiac imaging could be postponed unless there are heart failure symptoms or change in cardiac status.
The Internal Cardio-Oncology Society (ICOS) COVID guidelines suggest that biomarkers can be used as a surrogate for cardiac imaging in certain scenarios [10•]. As general principles, ICOS recommends cardiac imaging if the results will alter management, focused imaging studies to decease exposure time and that a cardiac biomarker approach utilizing troponin and/or natriuretic peptides and accurate symptom assessment can provide adequate cardiac surveillance obviating the need for cardiac imaging. Recommendations for baseline cardiac imaging for patients on anthracyclines and trastuzumab are largely similar to Calvillo-Argüelles et al. ICOS recommends post-anthracycline cardiac imaging in patients with heart failure symptoms, baseline cardiovascular disease, several cardiovascular disease risk factors, persistently elevated cardiac biomarkers, and or continued treatment with anthracyclines > 250 mg m2 doxorubicin-equivalent dosing. Routine cardiac surveillance of survivors beyond the acute period should be postponed absent heart failure or prior heart failure diagnosis. For patients received HER-2-targeted therapy, ICOS recommends that cardiac biomarkers can help identify patients who do not need cardiac imaging to monitor for cardiac safety. ICOS suggests that patients with low cardiovascular risk, asymptomatic, and with stable or normal biomarkers during monitoring, cardiac imaging can be deferred.
Other imaging adaptions made during the COVID pandemic include the use of cardiac computed tomography (CT) in lieu of transesophageal echocardiography and point-of-care ultrasound. Patients in atrial fibrillation who need cardioversion, often undergo a transesophageal echocardiogram (TEE) to exclude left atrial appendage clot. As TEE is an aerosolizing procedure and during lockdown cardiac procedure were delayed, cardiac CT offered a non-invasive and effective way to exclude left atrial appendage clot and expedite patient care. Point-of-care ultrasound allows for bedside assessment of left ventricular function and the American Society of Echocardiography published a statement of its use in patients with COVID or suspected COVID as a screening tool potentially obviating the need for TTE [12].
Changing workflow and workforce
COVID has affected outpatient clinical operations in several ways including pre-clinical screening and temperature checks, the need for physical distance in waiting rooms and clinic rooms, wearing of personal protective equipment like fask masks and eye shields, and additional cleaning procedures between patients. Providers have had to find ways to effectively communicate with patients while both wearing masks or when meeting virtually [13]. Providers may also be spending time after clinic hours talking to family members who were unable to attend a visit due to visitor restrictions. In order to minimize the number of healthcare workers in clinic, staff such as nurses and pharmacists may work remotely which inherently makes patient care more cumbersome for providers seeing patients in-person. At other times of the pandemic, outpatient staff were redeployed to inpatient units due to staffing shortages and a high COVID inpatient census. At times when hospitals were over capacity due to COVID admissions, inpatient cardiology issues like acute heart failure exacerbations had to be managed in the outpatient setting adding to the demands put on healthcare workers. Turnover of clinical staff due to COVID-19 has been high leading to disruption of clinical teams taking care of patients [14].
Expansion of telemedicine
With the onset of the COVID-19 pandemic, the utilization and development of telemedicine/telehealth in many medical specialties expanded exponentially. The rapid expansion was made feasible by the temporary changes in medical licensure board, federal policy changes with reimbursement in Medicare and Medicaid and the rapid deployment of secure mobile platforms [15]. Without a pandemic, telemedicine would not have evolved quickly as the regulatory issues were slow to respond. The growth of telemedicine is seen by some physicians, academic centers, and policymakers as a “silver lining” of the COVID pandemic, and Congress is considering many bills that would facilitate the long-term use of telemedicine [15]. We believe that state licensure reforms will be critical to enabling increased use of these services to subspecialties like cardio-oncology.
Early in 2020, the American Medical Association defined “telehealth” as: (1) real-time audio and visual connections between patients and physicians in different locations; (2) image and data collection store-and-forwarded for later interpretation; (3) remote patient monitoring tools, including mobile health (mHealth) tools, wearables, and devices; and (4) virtual check-ins through patient portals and messaging technologies (e-messaging) that interface with the electronic health records [16]. While telehealth has been part of managing many chronic medical conditions prior to the pandemic (HTN, CHF, arrhythmia, and others), the pandemic has brought to surface numerous challenges that are specific to oncologic patients with cardiac disease, which necessitated accelerated innovation and flexibility managing these patients. Telemedicine is an effective way to avoid potential spread through asymptomatic carriers, and protect patients and healthcare workers alike. At the same time, it allows for continued delivery of medical care and surveillance in a patient population where treatment is time-sensitive and cannot be safely disrupted or postponed. Oncology care generally cannot be delayed, and thus effective and timely co-management of cardiovascular issues remains essential even during periods of lockdown and COVID surges. Many practices and professional societies in cardio-oncology devised protocols to reduce number of surveillance imaging tests, and to risk stratify patients into either virtual, physical, or hybrid clinics [9•].
Telemedicine has many advantages to improve coordination and efficient delivery of care, making it more “patient-centered.” Patient visits with multiple medical specialists to determine the best treatment plan is often standard practice for cancer patients. Planning these visits without having to account for time lost and transportation is feasible with telemedicine visits, thereby adding to patient convenience, safety, and more efficient finalization of treatment plans. Multi-disciplinary case discussions and exchange of patient information among oncologists and cardiologists can simultaneously occur through telemedicine by obtaining multiple medical opinions during one session.
While telemedicine has offered numerous advantages to our practice in cardio-oncology, there are some limitations that the provider needs to be highlighted (Table 1 Comparison of various forms of clinical encounters). Identification of the suitable patient for telemedicine must occur to ensure optimal standard of care, and appropriate triaging must be in place. Physical exams may be incomplete and may have to be approximated with digitally obtained data. Standardized protocols for triaging, imaging/testing frequency have to be developed; however, there is need for more systemic large volume datasets for validation. In summary, the implementation of telemedicine has allowed for continued delivery of care for cardio-oncolgy patients, improved integration into oncology, and development of flexible care strategies that allow for optimal medical care. While more specific data and randomized studies are needed to determine a suitable and safe standard of care, there is a role for continued use of telemedicine in cardio-oncology during this pandemic and beyond [17].
Table 1.
Types of cardio-oncology clinical encounters
| Type of provider visit | Description | Advantages | Disadvantages |
|---|---|---|---|
| Coordinated Visits | *In-person visit coordinated with patients during infusion appointments | *Patient-centered care to reduce patient burden of appointment and exposure |
*Potential decreased privacy in infusion centers *Fragments the physicians schedule *Requires RN to help coordinate cardiology appointment when patient is at infusion |
| Video visit | Live streaming: provides limited but direct visual communication between the patient and the provider |
*Flexibility for patients and providers and reduced burden of travel for patients *Personal visual contact of patient in own environment *Direct overall assessment of patient’s condition *Thorough medication reconciliation with visual confirmation *Ideal for “return” patients without major active symptoms |
*More technology required *May promote health inequity in areas with diminished internet *Inability to perform a complete physical examination *Reimbursement likely to change over time |
| Telephone visit | *Telephone appointment: a dedicated time for phone call for real-time communication |
*Efficient and direct communication *Flexible location *Low technical demand |
*Time commitment and lower reimbursement *No visual assessment of the patient *Inability to perform a physical examination |
| E-consultation | *Virtual chart review to address a focused question. |
*Allows providers to use EMR to address question *Provides timely response *Does not require an patient appointment |
*Does not provide bi-directional conversation *No visual assessment of the patient *Inability to perform a physical examination |
| E-messaging | *Patient-initiated communication about a medical issues with patient’s consent to respond and bill for time time required to address issue |
*Bi-directional communication in the electronic health records *Efficient way to address straightforward problems *Improves patient access to the providers |
*No visual assessment of the patient *Inability to perform a physical examination |
As we look toward the future, the use of telemedicine and expanding its bandwidth will allow us to server larger and more diverse demographic cardiology-oncology population. In a recent editorial by Drs. Peter Block and Harold Jordon, they commented “If COVID-19 did one good thing it has made us all recognize that telehealth has enormous capabilities, and that virtual care might make a big dent in the inability of underserved populations to access health care” [18].
Utility of biomarkers during the pandemic
During the pandemic, we were forced to adapt our clinical practice in order to minimize the risk of exposing our patients to COVID-19. In order to provide regular monitoring to our cardio-oncology patients, biomarkers such as troponin and NT-proBNP are used to monitor and identify high-risk individuals who need further cardiac imaging. Biomarkers can be obtained during clinic or infusion visits. They are less invasive, with low cost and low risk of COVID-19 exposure. Even though there is no robust data to support use of biomarkers for surveillance of cardiotoxicity, this was helpful to monitor our patients during the pandemic. There is a need for biomarker research to assess the effect of chemotherapy and also, to potentially develop novel biomarkers to help detect pre-clinical LV dysfunction similar to what global longitudinal strain (GLS) in ECHO offers these patients [9•].
Cardiotoxicities such as myocarditis, pericarditis, cardiomyopathy, myocardial ischemia, conduction disturbances, coagulopathy, and cytokine release syndrome are seen in both, COVID-19 and cardio-oncology patients. In our cardio-oncology patients who were infected with COVID-19, the use of biomarkers was complicated due to similar CV side effects of COVID-19 and cardiotoxicity from chemotherapy medications. A strong collaboration among oncology and cardiology services to co-manage this group of high-risk patients is essential to find the right balance to provide appropriate care with the limited and restricted use of resources during pandemic [19].
Growth and incorporation of wearable devices and remote digital health
COVID-19 catalyzed the transformation of disease prevention, monitoring, and care delivery by the design and implementation of digital health (DH) services and products. (e.g., comprising apps, platforms, and websites) providing health-related surveillance, knowledge, literature, research, education as well as delivery of care [20]. From a CVD standpoint, heart rate and rhythm, blood pressure, weight, physical activity, and blood glucose are among the most commonly tracked data. There are exciting opportunities for growth and use of DH in cardio-oncology of which we now present a few [21•].
Atrial fibrillation and arrhythmias
The increased risk of development of atrial fibrillation (AF) in cancer patients is well described and related to both the underlying pathophysiologic mechanisms of cancer itself, and therapies administered [22]. Smartphone, wearable-based photoplethysmography (PPG) and hand-held single- or multiple-lead ECG recording devices are all options to diagnose cardiac arrhythmias. The sensitivity and specificity of the most-researched smartphone PPG and hand-held ECG recorders are high, e.g., the AliveCor ECG recorder is reported to have a 98% and 97% sensitivity and specificity respectively [23]. In addition to detecting AF, such tools facilitate detection of ECG abnormalities due to electrolyte imbalances or drug-related side effects, e.g., QT prolongation. These wearables and devices can reliably detect arrhythmias and obviate the need for in-person clinic visit. These applications have significant diagnostic potential and utility in time of reducing clinic visit and restricted travel during the COVID pandemic [24].
Heart failure/pulmonary hypertension
DH interventions to improve risk stratification and management of HF are mainly mediated and focused on weight monitoring and may be assisted by educational materials such as videos, reminders for appointments and medications and symptom diaries. These can be provided either via platforms, e.g., The Heart Failure Matters program, introduced by the European Society of Cardiology which engages people at home or by RPM tools. In the case of the latter, patients are equipped with a scale and sometimes a blood pressure (BP) cuff, which can either transmit values wirelessly over bluetooth to the RPM platform or the patients themselves manually enter their values. Depending on the vendor/technology, healthcare providers can be notified when weight and/or BP/HR thresholds are exceeded. Use of such DH tools was found to correlate with improved LVEF, BNP levels, weights, and quality-of -life indices [25, 26]. In those with pulmonary hypertension, a wearable accelerometer combined with text-based behavioral change intervention showed improvement in exercise tolerance at a 12-week follow-up [27]. In this era of social distancing, telemedicine and remote monitoring is emerging as an important tool for the management of heart failure patients. While many of these technologies are not new, their potential importance has been highlighted during the current COVID-19 pandemic. In general, these strategies appear to be safe; however, additional data will be needed to determine their effectiveness with respect to both process and outcomes measures [28].
Monitoring cardiovascular risk factors
The field of “healthy lifestyle” building (i.e., improving physical activity, weight, blood pressure, diabetes, and diet) has seen a tremendous expansion in the number of DH solutions and increased use during COVID. Fitness and diet apps (Apple Health, myfitness pal), websites, and wearables (e.g., Fitbit and Apple Watch), tele-coaching, and text messages are widely available. Some of them have been correlated with increased activity (more steps and more moderate-vigorous exercise) [29, 30] and can provide a more accurate way in measuring the amount of exercise [31]. Personalization via text messages was associated with increased amount of activity compared to activity tracking alone [32]. The use of weight loss DH solutions has only been shown to help with short- but not long-term (over 12 months) success [33, 34]. Hypertension is the most common comorbid condition in cancer patients [35]. A wealth of DH intervention is available to help with management of hypertension (HTN) including new generation wrist-worn ambulatory BP monitors [36–38], apps to help with journaling/tracking values, remote patient monitoring solutions [39–41], and medication reminders via texts. Related to these are also the vast market of apps promoting a low salt diet [34]. The role of diabetes (DM) as an adverse prognosticator in cancer has been well described [42, 43]. Similarly to HTN, the DH market targeting patients with DM is vast and continuously growing [44]. Smartphone apps, RPM tools [45, 46], and new generation blood glucose (BGlu) monitors, e.g., transdermal patches and non-invasive spectroscopy [47] are now available to personalize DM education, tracking BGlu, medication administration, diet, weight, and may even allow for real-time, continuous BGlu tracking obviating the need for manual measurement and recording [48]. The integration of DH into cardiovascular risk factor management has the potential to impact to cardio-oncology patients leading to better outcomes.
Cardiac rehabilitation
Facilitating access to cardiac rehab programs is another benefit of DH. Cardiac rehab apps offer educational, motivational, behavioral, and exercise guidance and can also help to keep track of participant activity and dietary patterns. Tele-rehab at home correlates with improved functional capacity, mental health, and weight loss [49]. Added to traditional cardiac rehab, tele-rehab was found to lead to more weight loss [50]. Although many center-based traditional cardiac rehab centers shut down during the COVID-19 crisis, remote cardiac rehab remains a viable alternative, allowing patients to exercise in their own homes while being supervised by a physician or other health care professional [51].
Training in cardio-oncology
The COVID-19 pandemic transformed medical education, including academic health systems [52, 53•]. For many years, the aging population, exceptionally high healthcare costs, and technological advances have been pressuring the medical system to redesign curricula, especially among developed nations. However, the pace of adaption was slow due to concern on lack of appropriate transition from traditional courses and practices. The emergence of the COVID-19 pandemic and public health response immediately changed long-established medical education practices. The virtual clinics and teaching, simulation-based training, and personalized competency goals have replaced the conventional in-person clinics and volume-based assessments [54].
Not limited to clinical care, the American College of Cardiology (ACC) Cardio-Oncology Leadership Council has proposed a standardized training structure for cardio-oncology [55]. This suggested standardized training utilized the Core Cardiology Training Symposium (COCATS) structure. One can gain COCATS levels I and II experience during their general cardiology training [55]. Moreover, one can attain an advanced cardio-oncology fellowship with 1 year of dedicated training (COCATS level III) [55]. There are four components involved in the advanced cardio-oncology training: (1) inpatient, (2) outpatient clinical experience, (3) didactics, and (4) research.
Clinical experience through outpatient and inpatient exposure is a crucial element of cardio-oncology training. The ACC Cardio-Oncology Leadership Council recommends at least 40 half-day clinics and 100 unique inpatient encounters for each trainee to earn COCATS level III [55]. In the COVID-19 era, where there is avoidance of unnecessary physical encounters, telehealth or telemedicine has become the mode of communication. Cardio-oncology has taken telemedicine one step ahead with a multi-disciplinary approach to improve patient care. Nowadays, each trainee can facilitate multimodality learning through three-way telehealth visits incorporating patient, oncologist, and cardiologist. The remote monitoring system, which is a part of telemedicine, has allowed the cardio-oncology trainee to frequently assess sign and symptoms of cardiotoxicity. Moreover, the amalgam of COVID-19, sequela of cancer, and cardiotoxicity has equipped cardio-oncology trainees for personalized patient care.
Traditional in-person meetings or conferences are for didactic training prior to the COVID-19 pandemic. After the implementation of social distancing, virtual meetings and video conferences have taken over the formal didactic training. Not only restricted to institutional experts, trainees now have access to professionals all over the world through virtual platforms. One such example is weekly webinars organized by the International Cardio-Oncology Society (ICOS). The ACC Cardio-Oncology Leadership Council advocates each trainee to participate in virtual webinars including attending annual cardio-oncology conferences [55]. Lastly, the social media platforms such as Twitter also provide widespread network coverage and proficient access to new cardio-oncology publications.
Research is also an integral part of cardio-oncology training, which weighs equally in clinical exposure and didactics. For each advanced cardio-oncology trainee, the ACC Cardio-Oncology Leadership Council endorses regular participation or completion of at least one research project [55]. As the COVID-19 pandemic impacted research activities, one can overlook the shortcoming and consider the opportunity for future growth and further development. Setting up as a prominent example, the field of cardio-oncology is pushing for multi-institutional collaboration and data sharing for clinical research. The cardio-oncology fellows can actively engage in multi-center research projects, including collaboration with mentors virtually. Nevertheless, it is worth mentioning that the continuation of the COVID-19 pandemic has impacted physical, academic, as well as mental wellbeing of current cardio-oncology trainees [56]. Education institutions will need to remain vigilant and attentive on the mental and physical wellbeing of trainees to prevent unnecessary burnout [57•]. Initiatives such as virtual meeting on trainee wellbeing, organizing social events, and providing institutional-wide resources on psychological support on overall health will help address the stress pandemic has placed on cardio-oncology trainees and all health care professionals.
In summary, while the pandemic has been met with many challenges, there are positive initiatives that have sprung forward helping to create a more patient-centered experience for cardio-oncology patients and broader educational opportunities for trainees. The expansion of telemedicine, integration of digital health, wider adoption of cardiac biomarkers, consolidation, and coordination of cardio-oncology testing have all shaped the way cardiovascular care is delivered to cardio- oncology patients and likely will remain in place when the pandemic is no longer present.
Declarations
Conflict of Interest
Lavanya Kondapalli declares that she has no conflict of interest. Garima Arora declares that she has no conflict of interest. Riem Hawi declares that she has no conflict of interest. Efstathia Andrikopoulou declares that she has no conflict of interest. Courtney Estes declares that she has no conflict of interest. Nirav Patel declares that he has no conflict of interest. Carrie Lenneman declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Cardio-oncology
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Best Quotations [March 1, 2022]. Available from: https://best-quotations.com/authquotes.php?auth=15.
- 2.• Baldassarre LA, Yang EH, Cheng RK, DeCara JM, Dent S, Liu JE, et al. Cardiovascular care of the oncology patient during COVID-19: an expert consensus document from the ACC Cardio-Oncology and Imaging Councils. J Natl Cancer Inst. 2021;113(5):513-22. The paper describes the difficulties of diagnosing the etiology of cardiovascular complications in patients with cancer and COVID-19, along with weighing the advantages against risks of exposure, with the modification of existing cardiovascular treatments and cardiotoxicity surveillance in patients with cancer during the COVID-19. (Baldassarre). [DOI] [PMC free article] [PubMed]
- 3.Feng RM, Zong YN, Cao SM, Xu RH. Current cancer situation in China: good or bad news from the 2018 Global Cancer Statistics? Cancer Commun. 2019;39(1):22. doi: 10.1186/s40880-019-0368-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganatra S, Dani SS, Shah S, Asnani A, Neilan TG, Lenihan D, Ky B, Barac A, Hayek SS, Leja M, Herrmann J, Thavendiranathan P, Fradley M, Bang V, Shreyder K, Parikh R, Patel R, Singh A, Brar S, et al. Management of cardiovascular disease during coronavirus disease (COVID-19) pandemic. Trends Cardiovasc Med. 2020;30(6):315–25. [DOI] [PMC free article] [PubMed]
- 5.Sadler D, DeCara JM, Herrmann J, Arnold A, Ghosh AK, Abdel-Qadir H, et al. Perspectives on the COVID-19 pandemic impact on cardio-oncology: results from the COVID-19 International Collaborative Network survey. Cardio-oncology. 2020;6(1):28. doi: 10.1186/s40959-020-00085-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mahmud E, Dauerman HL, Welt FGP, Messenger JC, Rao SV, Grines C, Mattu A, Kirtane AJ, Jauhar R, Meraj P, Rokos IC, Rumsfeld JS, Henry TD. Management of acute myocardial infarction during the COVID-19 pandemic: a position statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP) J Am Coll Cardiol. 2020;76(11):1375–1384. doi: 10.1016/j.jacc.2020.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, Bhatt DL, et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol. 2020;76(3):280–288. doi: 10.1016/j.jacc.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.• Bisceglia I, Gabrielli D, Canale ML, Gallucci G, Parrini I, Turazza FM, et al. ANMCO POSITION PAPER: cardio-oncology in the COVID era (CO and CO). European Heart Journal Supplements: J European Soc Cardio. 2021;23(Suppl C):C128-C53. The COVID-19 pandemic and its impact on patients with cancer and cardiovascular disease have confirmed the particular vulnerability of cardio-oncology population. The article present optimal medical strategies for the cardio-oncology health care providers to manage the effect of COVID. (Bisceglia). [DOI] [PMC free article] [PubMed]
- 9.• Addison D, Campbell CM, Guha A, Ghosh AK, Dent SF, Jneid H. Cardio-oncology in the era of the COVID-19 Pandemic and beyond. J Am Heart Assoc. 2020;9(19):e017787. The article evaluates the implications of the pandemic on the practice and training of cardio-oncology and the relationship between comorbid diseases and clinical outcomes. (Addison). [DOI] [PMC free article] [PubMed]
- 10.• Lenihan D, Carver J, Porter C, Liu JE, Dent S, Thavendiranathan P, et al. Cardio-oncology care in the era of the coronavirus disease 2019 (COVID-19) pandemic: an International Cardio-Oncology Society (ICOS) statement. CA Cancer J Clin. 2020;70(6):480-504. The manuscript outlines the strategic adjustment is to minimize the risk of COVID-19 infection while not becoming negligent of CVD and its important impact on the overall outcomes of patients who are being treated for cancer. (Lenihan). [DOI] [PMC free article] [PubMed]
- 11.Calvillo-Arguelles O, Abdel-Qadir H, Ky B, Liu JE, Lopez-Mattei JC, Amir E, et al. Modified routine cardiac imaging surveillance of adult cancer patients and survivors during the COVID-19 pandemic. JACC CardioOncol. 2020;2(2):345–349. doi: 10.1016/j.jaccao.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johri AM, Galen B, Kirkpatrick JN, Lanspa M, Mulvagh S, Thamman R. ASE Statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr. 2020;33(6):670–673. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pennell NA, Dillmon M, Levit LA, Moushey EA, Alva AS, Blau S, Cannon TL, Dickson NR, Diehn M, Gonen M, Gonzalez MM, Hensold JO, Hinyard LJ, King T, Lindsey SC, Magnuson A, Marron J, McAneny BL, McDonnell TM, et al. American Society of Clinical Oncology road to recovery report: learning from the COVID-19 Experience to improve clinical research and cancer care. J Clin Oncol. 2021;39(2):155–69. [DOI] [PMC free article] [PubMed]
- 14.Lavoie-Tremblay M, Gelinas C, Aube T, Tchouaket E, Tremblay D, Gagnon MP, et al. Influence of caring for COVID-19 patients on nurse’s turnover, work satisfaction and quality of care. J Nurs Manag. 2022;30(1):33–43. doi: 10.1111/jonm.13462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mehrotra A, Nimgaonkar A, Richman B. Telemedicine and medical licensure - potential paths for reform. N Engl J Med. 2021;384(8):687–690. doi: 10.1056/NEJMp2031608. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan B. Revisiting health information technology ethical, legal, and social issues and evaluation: telehealth/telemedicine and COVID-19. Int J Med Inform. 2020;143:104239. doi: 10.1016/j.ijmedinf.2020.104239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Parikh A, Kumar AA, Jahangir E. Cardio-oncology care in the time of COVID-19 and the role of telehealth. JACC CardioOncol. 2020;2(2):356–358. doi: 10.1016/j.jaccao.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Block P, Harold JG. A world that is greatly out of balance in matters of health is neither stable nor secure American College of Cardiology Magazine [December 16. 2021]. Available from: https://www.acc.org/Latest-in-Cardiology/Articles/2021/12/01/01/42/Guest-Editorial-Reflections-on-2021-COVID-19-CVD-and-Health-Inequity.
- 19.Bisceglia I, Canale ML, Gallucci G, Turazza FM, Lestuzzi C, Parrini I, Russo G, Maurea N, Quagliariello V, Oliva S, di Fusco SA, Lucà F, Tarantini L, Trambaiolo P, Moreo A, Geraci G, Gabrielli D, Gulizia MM, Oliva F, Colivicchi F. Cardio-Oncology in the COVID Era (Co & Co): The never ending story. Front Cardiovasc Med. 2022;9:821193. doi: 10.3389/fcvm.2022.821193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization . e-Health [Accessed February 9th 2022]. Available from: www.emro.who.int/health-topics/ehealth/.
- 21.• Fonseka LN, Woo BK. Consumer wearables and the integration of new objective measures in oncology: patient and provider perspectives. JMIR mHealth uHealth. 2021;9(7):e28664. The authors review the recent literature on consumer-grade wearables and its current applications in cancer from the perspective of both the patient and the provider. The relevant studies suggested that these devices offer benefits, such as improved medication adherence and accuracy of symptom tracking over self-reported data that increase patient empowerment. (Fonseka). [DOI] [PMC free article] [PubMed]
- 22.Leiva O, AbdelHameid D, Connors JM, Cannon CP, Bhatt DL. Common pathophysiology in cancer, atrial fibrillation, atherosclerosis, and thrombosis: JACC: cardiooncology state-of-the-art review. JACC CardioOncol. 2021;3(5):619–634. doi: 10.1016/j.jaccao.2021.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Halcox JPJ, Wareham K, Cardew A, Gilmore M, Barry JP, Phillips C, Gravenor MB. Assessment of remote heart rhythm sampling using the AliveCor heart monitor to screen for atrial fibrillation: the REHEARSE-AF study. Circulation. 2017;136(19):1784–1794. doi: 10.1161/CIRCULATIONAHA.117.030583. [DOI] [PubMed] [Google Scholar]
- 24.Kaushik A, Patel S, Dubey K. Digital cardiovascular care in COVID-19 pandemic: a potential alternative? J Card Surg. 2020;35(12):3545–3550. doi: 10.1111/jocs.15094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dendale P, De Keulenaer G, Troisfontaines P, Weytjens C, Mullens W, Elegeert I, et al. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail. 2012;14(3):333–340. doi: 10.1093/eurjhf/hfr144. [DOI] [PubMed] [Google Scholar]
- 26.Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Mobile phone-based telemonitoring for heart failure management: a randomized controlled trial. J Med Internet Res. 2012;14(1):e31. doi: 10.2196/jmir.1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brooks GC, Vittinghoff E, Iyer S, Tandon D, Kuhar P, Madsen KA, Marcus GM, Pletcher MJ, Olgin JE. Accuracy and usability of a self-administered 6-minute walk test smartphone application. Circ Heart Fail. 2015;8(5):905–913. doi: 10.1161/CIRCHEARTFAILURE.115.002062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oseran AS, Afari ME, Barrett CD, Lewis GD, Thomas SS. Beyond the stethoscope: managing ambulatory heart failure during the COVID-19 pandemic. ESC Heart Fail. 2021;8(2):999–1006. doi: 10.1002/ehf2.13201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maddison R, Pfaeffli L, Whittaker R, Stewart R, Kerr A, Jiang Y, Kira G, Leung W, Dalleck L, Carter K, Rawstorn J. A mobile phone intervention increases physical activity in people with cardiovascular disease: results from the HEART randomized controlled trial. Eur J Prev Cardiol. 2015;22(6):701–709. doi: 10.1177/2047487314535076. [DOI] [PubMed] [Google Scholar]
- 30.Cadmus-Bertram LA, Marcus BH, Patterson RE, Parker BA, Morey BL. Randomized trial of a fitbit-based physical activity intervention for women. Am J Prev Med. 2015;49(3):414–418. doi: 10.1016/j.amepre.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bittel AJ, Elazzazi A, Bittel DC. Accuracy and precision of an accelerometer-based smartphone app designed to monitor and record angular movement over time. Telemedicine Journal and e-health: J Americ Telemed Assoc. 2016;22(4):302–9. [DOI] [PubMed]
- 32.Martin SS, Feldman DI, Blumenthal RS, Jones SR, Post WS, McKibben RA, et al. mActive: a randomized clinical trial of an automated mHealth intervention for physical activity promotion. J Am Heart Assoc. 2015;4(11):e002239. doi: 10.1161/JAHA.115.002239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Godino JG, Merchant G, Norman GJ, Donohue MC, Marshall SJ, Fowler JH, Calfas KJ, Huang JS, Rock CL, Griswold WG, Gupta A, Raab F, Fogg BJ, Robinson TN, Patrick K. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): a 2 year, parallel-group, randomised, controlled trial. Lancet Diabetes Endocrinol. 2016;4(9):747–755. doi: 10.1016/S2213-8587(16)30105-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spring B, Pellegrini C, McFadden HG, Pfammatter AF, Stump TK, Siddique J, et al. Multicomponent mHealth intervention for large, sustained change in multiple diet and activity risk behaviors: the make better choices 2 randomized controlled trial. J Med Internet Res. 2018;20(6):e10528. doi: 10.2196/10528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL., Jr Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA. 2004;291(20):2441–2447. doi: 10.1001/jama.291.20.2441. [DOI] [PubMed] [Google Scholar]
- 36.Moon JH, Kang MK, Choi CE, Min J, Lee HY, Lim S. Validation of a wearable cuff-less wristwatch-type blood pressure monitoring device. Sci Rep. 2020;10(1):19015. doi: 10.1038/s41598-020-75892-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kario K, Shimbo D, Tomitani N, Kanegae H, Schwartz JE, Williams B. The first study comparing a wearable watch-type blood pressure monitor with a conventional ambulatory blood pressure monitor on in-office and out-of-office settings. J Clin Hypertens. 2020;22(2):135–141. doi: 10.1111/jch.13799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kario K. Management of hypertension in the digital era: small wearable monitoring devices for remote blood pressure monitoring. Hypertension. 2020;76(3):640–650. doi: 10.1161/HYPERTENSIONAHA.120.14742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burke LE, Ma J, Azar KM, Bennett GG, Peterson ED, Zheng Y, Riley W, Stephens J, Shah SH, Suffoletto B, Turan TN, Spring B, Steinberger J, Quinn CC, American Heart Association Publications Committee of the Council on Epidemiology and Prevention, Behavior Change Committee of the Council on Cardiometabolic Health, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, Council on Quality of Care and Outcomes Research, and Stroke Council Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2015;132(12):1157–1213. doi: 10.1161/CIR.0000000000000232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57(1):29–38. doi: 10.1161/HYPERTENSIONAHA.110.160911. [DOI] [PubMed] [Google Scholar]
- 41.Tucker KL, Sheppard JP, Stevens R, Bosworth HB, Bove A, Bray EP, Earle K, George J, Godwin M, Green BB, Hebert P, Hobbs FDR, Kantola I, Kerry SM, Leiva A, Magid DJ, Mant J, Margolis KL, McKinstry B, et al. Self-monitoring of blood pressure in hypertension: a systematic review and individual patient data meta-analysis. PLoS Med. 2017;14(9):e1002389. [DOI] [PMC free article] [PubMed]
- 42.Barone BB, Yeh HC, Snyder CF, Peairs KS, Stein KB, Derr RL, Wolff AC, Brancati FL. Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: a systematic review and meta-analysis. JAMA. 2008;300(23):2754–2764. doi: 10.1001/jama.2008.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shin DW, Ahn E, Kim H, Park S, Kim YA, Yun YH. Non-cancer mortality among long-term survivors of adult cancer in Korea: national cancer registry study. Cancer Causes Control CCC. 2010;21(6):919–929. doi: 10.1007/s10552-010-9521-x. [DOI] [PubMed] [Google Scholar]
- 44.Rhee SY, Kim C, Shin DW, Steinhubl SR. Present and future of digital health in diabetes and metabolic disease. Diabetes Metab J. 2020;44(6):819–827. doi: 10.4093/dmj.2020.0088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Painter SL, Lu W, Schneider J, James R, Shah B. Drivers of weight loss in a CDC-recognized digital diabetes prevention program. BMJ Open Diabetes Res Care. 2020;8(1):e001132. doi: 10.1136/bmjdrc-2019-001132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sepah SC, Jiang L, Ellis RJ, McDermott K, Peters AL. Engagement and outcomes in a digital diabetes prevention program: 3-year update. BMJ Open Diabetes Res Care. 2017;5(1):e000422. doi: 10.1136/bmjdrc-2017-000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Singh SP, Mukherjee S, Galindo LH, So PTC, Dasari RR, Khan UZ, Kannan R, Upendran A, Kang JW. Evaluation of accuracy dependence of Raman spectroscopic models on the ratio of calibration and validation points for non-invasive glucose sensing. Anal Bioanal Chem. 2018;410(25):6469–6475. doi: 10.1007/s00216-018-1244-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Klonoff DC. The current status of mHealth for diabetes: will it be the next big thing? J Diabetes Sci Technol. 2013;7(3):749–758. doi: 10.1177/193229681300700321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Varnfield M, Karunanithi M, Lee CK, Honeyman E, Arnold D, Ding H, Smith C, Walters DL. Smartphone-based home care model improved use of cardiac rehabilitation in postmyocardial infarction patients: results from a randomised controlled trial. Heart. 2014;100(22):1770–1779. doi: 10.1136/heartjnl-2014-305783. [DOI] [PubMed] [Google Scholar]
- 50.Widmer RJ, Allison TG, Lennon R, Lopez-Jimenez F, Lerman LO, Lerman A. Digital health intervention during cardiac rehabilitation: a randomized controlled trial. Am Heart J. 2017;188:65–72. doi: 10.1016/j.ahj.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 51.Pecci C, Ajmal M. Cardiac rehab in the COVID-19 pandemic. Am J Med. 2021;134(5):559–560. doi: 10.1016/j.amjmed.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Goddard AF, Patel M. The changing face of medical professionalism and the impact of COVID-19. Lancet. 2021;397(10278):950–952. doi: 10.1016/S0140-6736(21)00436-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.• Lucey CR, Johnston SC. The transformational effects of COVID-19 on medical education. JAMA. 2020;324(11):1033-4. The paper reveals that the COVID-19 pandemic was a catalyst for the transformation of medical education bringing to light the importance of addressing public health issues; improve health care systems; incorporate data and technology in service to patient care and eliminate health care disparities in medicine. (Lucey). [DOI] [PubMed]
- 54.Kotta PA, Corso B, Brailovsky Y, Oliveros E. The impact of 2020 and the future of cardiology training: how do we innovate? JACC Case Rep. 2021;3(4):697–700. doi: 10.1016/j.jaccas.2021.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Alvarez-Cardona JA, Ray J, Carver J, Zaha V, Cheng R, Yang E, Mitchell JD, Stockerl-Goldstein K, Kondapalli L, Dent S, Arnold A, Brown SA, Leja M, Barac A, Lenihan DJ, Herrmann J, Cardio-Oncology Leadership Council Cardio-Oncology education and training: JACC council perspectives. J Am Coll Cardiol. 2020;76(19):2267–2281. doi: 10.1016/j.jacc.2020.08.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Velazquez AI, Durani U, Weeks LD, Major A, Reynolds R, Kumbamu A, et al. Impact of COVID-19 on hematology-oncology fellowship programs: a quantitative and qualitative survey assessment of fellowship program directors. JCO Oncol Pract. 2022;11:OP2100634. doi: 10.1200/OP.21.00634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.• Feldman S, Liu J, Steingart R, Gupta D. Cardio-oncology Training in the COVID-19 Era. Curr Treat Options in Oncol. 2021;22(7):58. The article details how the COVID-19 pandemic has impacted all aspects of cardio-oncology training, how programs and trainees can adapt to these challenges, and how lessons learned from the COVID-19 era can continue to positively impact cardio-oncology training for the foreseeable future. (Feldman). [DOI] [PMC free article] [PubMed]