Abstract
Objectives: Growth in rates of preventive services has been linked to trends in retention of teeth and the emergence of minimal intervention approaches. In this study, we examined associations between patient-level characteristics and rates of the preventive services dental/prophylaxis and application of remineralisation agents. Methods: A random sample of dentists in Australia was posted a self-administered questionnaire in 2009–2010. A service log was used to collect data on preventive services and patient characteristics. Results: Responses were obtained from 1,148 dentists (response rate = 67%). Preventive service rate models, adjusted according to the age and gender of patients, indicated that insured patients had higher rates of prophylaxis [rate ratio (RR) = 1.39; 95% confidence interval (95% CI): 1.21–1.59) and remineralisation services (RR = 1.85; 95% CI: 1.46–2.33), and that emergency visits had lower rates for prophylaxis (RR = 0.26; 95% CI: 0.20–0.35) and remineralisation services (RR = 0.23; 95% CI: 0.14–0.38). Those who had 20 teeth or more demonstrated higher rates of prophylaxis (RR = 1.41; 95% CI: 1.13–1.75) and remineralisation services (RR = 1.45; 95% CI: 1.02–2.08). Those with decayed teeth had lower rates of prophylaxis (RR = 0.54; 95% CI: 0.46–0.63) and remineralisation services (RR = 0.66; 95% CI: 0.53–0.82). Conclusions: Preventive services were associated with patient age, characteristics of visits and oral health. Patients who were worse off, in terms of attending an emergency visit for the relief of pain and having decayed teeth, had lower rates of preventive care. The findings indicate that patients most in need are missing out on the benefits of preventive dental services.
Key words: Dental services, preventive services, dental prophylaxis, remineralisation services, private general practice
INTRODUCTION
Over the last few decades, dentistry has witnessed a paradigm shift from a surgical model to an evidence-based medical model that is focused more on the diagnosis, early intervention and prevention of oral disease1., 2.. Preventive care is argued as a foundational principle in modern dentistry1. Newer patient-management approaches, such as minimal intervention dentistry, encourage the least invasive treatment options, accommodating both prevention control and treatment principles3. Preventive care can include services such as dental prophylaxis (removal of plaque and calculus), remineralisation procedures (topical fluoride application), dietary advice, oral hygiene instructions and application of fissure sealants. The move towards prevention is a cost-effective approach to enhance oral health with the aim to promote retention of a natural dentition4.
Long-term patterns of attendance for routine dental care may have better oral health outcomes in terms of less tooth loss and less dental caries, and higher levels of self-rated oral health and oral health-related quality of life5., 6., 7., supporting the role of regular dental visiting for preventive check-ups8. In contrast, experience of adverse dental episodes, such as visits to a dentist for relief of pain, may lead to higher oral health impacts later in life that may be cumulative over the life course9. This probably reflects the different pattern of treatment received by adults, attending for dental problems, who have a mix of services that comprise less preventive care, such as scale and clean services, and more treatment, such as fillings, root canal treatments and extractions10.
In Australia, the rates of preventive dental services have an increased trend with time, with preventive services being one of the most frequent dental service areas, along with diagnostic and restorative services11. A rise in the provision of preventive services has been observed for both dental prophylaxis and remineralisation services12. Given the high frequency of preventive services in Australia, and their increasing rate, it is important to investigate preventive services in order to improve knowledge of the characteristics related to variation in preventive care and to understand possible influences on preventive services into the future. The study objective was to assess the rates of two preventive services – dental prophylaxis and remineralisation agents – according to the patient-level characteristics of demographics, factors related to visits and oral health.
METHODS
Australian dentists were randomly sampled from State or Territory dental registers in 1983–1984 using a sampling fraction of 10% for male dentists and 40% for female dentists (as female dentists comprised a lower percentage of registered dentists). A sample supplementation procedure was used across successive study waves to provide representative cross-sectional estimates, using the original sample fractions for newly registered dentists. Participants in these samples were posted a questionnaire in 1983–1984, 1988–1989, 1993–1994, 1998–1999, 2003–2004 and 2009–201013., 14., 15., with the analysis based on the most recent data. Weighted data, based on dental board registration statistics from 200916, provided representative estimates according to the age and gender distribution of dentists working in private practice.
Responding dentists logged services from a typical day. The numbers of patients logged by each dentist depended on their activity on that day, and dentists could choose which typical day to have in their log. Instructions indicated to dentists to log services for all patients, irrespective of how the patient was charged. Preventive service items were coded into groupings of dental prophylaxis, application of remineralisation agents and other preventive services, using the Australian Dental Association schedule17. Dental prophylaxis comprised service items that included removal of plaque and removal of calculus, and service items in the remineralisation agents category included topical and concentrated applications of remineralisation and/or cariostatic agents. Other preventive items included dietary advice, oral hygiene instruction and provision of mouthguards. The category of other preventive services was excluded from the analysis on the basis that it was a small proportion of preventive services.
The characteristics of patients covering demographics, visit factors and oral health status were recorded in the service log. These characteristics included the age and gender of the patient, whether they had insurance and the reason for the visit (emergency visits were classified as involving relief of pain). The oral health variables, number of teeth and number of decayed teeth for each patient were determined by the responding dentist. For analytical purposes, we coded the number of teeth into two categories – 20 teeth or more, or fewer than 20 teeth18., 19.; and decayed teeth were coded into categories that comprised the presence of any decayed teeth or having no decay.
Weighted data were used to produce estimates and tests of statistical significance. Statistical procedures were used to account for design effects (i.e. the clustering of patient-level observations within dentists). This enabled analysis of patient-level characteristics, such as demographics, visit factors and oral health, while accounting for the clustered nature of the data. Service rates per visit were determined by dividing the number of services by the number of visits provided in the typical day, and were presented descriptively as means. Statistical comparisons used Poisson regression with services per visit as the outcome and P < 0.05 as the significance level, using survey procedures (SAS statistical software, version 9.3), with dentist as the cluster variable. Indicator variables were used for the independent variables (coded as 1 or 0) in the adjusted models. The findings from the adjusted models were presented as rate ratios that reflect the rate of services relative to the rate provided in the reference category for each independent variable. The Ethics Committee of the Australian Institute of Health and Welfare provided ethical clearance. The research conforms to the Declaration of Helsinki, with consent implied through the return of completed questionnaires. Patient data collected in the service log were anonymous to the researchers and responding dentist data were de-identified before analysis.
RESULTS
Questionnaires were obtained from 1,148 dentists (response rate = 67%). Table 1 shows that the 45–64 years age group comprised the largest proportion (36.0%) of patients, and that there was a slightly higher percentage of male (55.7%) than female (44.4%) patients. Private dental insurance was held by a majority of patients (62.0%) and most had made visits for reasons that were non-emergency in nature (78.3%). Patients with 20 teeth or more were in the majority (88.1%) and those with one or more decayed tooth accounted for around half of the sample (48.3%).
Table 1.
Distributions of explanatory variables and bivariate associations with preventive services
| Variable | Distribution | Prophylaxis services |
Remineralisation services |
||
|---|---|---|---|---|---|
| (%) | Mean | SE | Mean | SE | |
| Patient age | ** | ** | |||
| 5–11 years | 5.1 | 0.37 | 0.04 | 0.28 | 0.04 |
| 12–17 years | 7.7 | 0.47 | 0.04 | 0.24 | 0.03 |
| 18–24 years | 7.4 | 0.40 | 0.03 | 0.18 | 0.02 |
| 25–44 years | 27.9 | 0.39 | 0.03 | 0.14 | 0.01 |
| 45–64 years | 36.0 | 0.29 | 0.02 | 0.10 | 0.01 |
| 65+ years | 15.8 | 0.23 | 0.02 | 0.08 | 0.01 |
| Sex of patient | * | ||||
| Male | 55.7 | 0.31 | 0.01 | 0.13 | 0.01 |
| Female | 44.4 | 0.35 | 0.02 | 0.14 | 0.01 |
| Insurance status | ** | ** | |||
| Insured | 62.0 | 0.39 | 0.02 | 0.17 | 0.01 |
| Uninsured | 38.0 | 0.24 | 0.01 | 0.08 | 0.01 |
| Reason for visit | ** | ** | |||
| Emergency | 21.7 | 0.09 | 0.01 | 0.03 | 0.01 |
| Non-emergency | 78.3 | 0.41 | 0.02 | 0.17 | 0.01 |
| Number of teeth | ** | ** | |||
| < 20 teeth | 11.9 | 0.18 | 0.02 | 0.07 | 0.01 |
| 20+ teeth | 88.1 | 0.36 | 0.02 | 0.14 | 0.01 |
| Decayed teeth | ** | ** | |||
| No decayed teeth | 51.7 | 0.44 | 0.02 | 0.17 | 0.01 |
| 1+ decayed tooth | 48.3 | 0.21 | 0.01 | 0.09 | 0.01 |
P < 0.05; **P < 0.01 (Poisson regression).
SE, standard error.
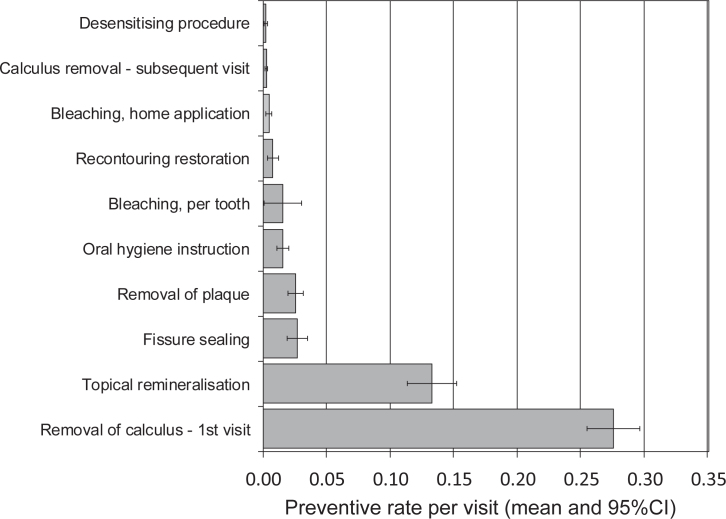
Removal of calculus and topical remineralisation were the most commonly provided preventive service items (Figure 1). Much lower rates were observed for the remaining preventive service items, with the next highest being for fissure sealing, then for removal of plaque and then for oral hygiene instruction.
Figure 1.
Rates of preventive services per visit for the most common preventive procedures. 95% CI, 95% confidence interval.
Both prophylaxis and remineralisation services were inversely related to the age of the patient, with lower rates observed among older patients (Table 1). Although the number of remineralisation services per visit were not related to gender of the patient, there were higher prophylaxis service rates for female patients than for male patients. Higher rates of both prophylaxis and remineralisation services were observed for patients with insurance coverage and for patients making visits for non-emergency reasons. Patients who had more teeth and patients with no decay present had higher rates of prophylaxis and remineralisation services.
Table 2 shows that in models of preventive services the rates of prophylaxis services were significantly lower for older patients ≥ 65 years of age [rate ratio (RR) = 0.76; 95% confidence interval (95% CI): 0.59–0.97] compared with the reference category of those 5–11 years of age. The rates of remineralisation services were significantly lower among patients in the age categories 25–44 (RR = 0.58; 95% CI: 0.42–0.79), 45–64 (RR = 0.44; 95% CI: 0.32–0.60) and ≥65 (RR = 0.40; 95% CI: 0.26–0.60) years, in comparison with the reference category of 5–11 years. The rates of preventive services were not related to patient gender. Insured patients had significantly higher rates of prophylaxis (RR = 1.39; 95% CI: 1.21–1.59) and remineralisation services (RR = 1.85; 95% CI: 1.46–2.33), and there were significantly lower rates of prophylaxis (RR = 0.26; 95% CI: 0.20–0.35) and remineralisation services (RR = 0.23; 95% CI: 0.14–0.38) for emergency visits. Having 20 or more teeth was associated with significantly higher rates of prophylaxis (RR = 1.41; 95% CI: 1.13–1.75) and remineralisation services (RR = 1.45; 95% CI: 1.02–2.08). Significantly lower rates of prophylaxis (RR = 0.54; 95% CI: 0.46–0.63) and remineralisation services (RR = 0.66; 95% CI: 0.53–0.82) were related to the presence of decayed teeth.
Table 2.
Adjusted models of preventive service rates
| Variable | Prophylaxis services |
Remineralisation services |
||
|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | |
| Patient age | ||||
| 5–11 years | Ref | Ref | ||
| 12–17 years | 1.08 | 0.85–1.36 | 0.77 | 0.56–1.06 |
| 18–24 years | 1.11 | 0.88–1.39 | 0.71 | 0.50–1.03 |
| 25–44 years | 1.18 | 0.91–1.54 | 0.58** | 0.42–0.79 |
| 45–64 years | 0.88 | 0.72–1.09 | 0.44** | 0.32–0.60 |
| 65+ years | 0.76* | 0.59–0.97 | 0.40** | 0.26–0.60 |
| Sex of patient | ||||
| Male | 0.95 | 0.84–1.07 | 0.99 | 0.86–1.13 |
| Female | Ref | Ref | ||
| Insurance status | ||||
| Insured | 1.39** | 1.21–1.59 | 1.85** | 1.46–2.33 |
| Uninsured | Ref | Ref | ||
| Reason for visit | ||||
| Emergency | 0.26** | 0.20–0.35 | 0.23** | 0.14–0.38 |
| Non-emergency | Ref | Ref | ||
| Number of teeth | ||||
| < 20 teeth | Ref | Ref | ||
| 20+ teeth | 1.41** | 1.13–1.75 | 1.45* | 1.02–2.08 |
| Decayed teeth | ||||
| No decayed teeth | Ref | Ref | ||
| &geq 1 decayed tooth | 0.54** | 0.46–0.63 | 0.66** | 0.53–0.82 |
P < 0.05; **P < 0.01 (Poisson regression).
95% CI, 95% confidence interval; Ref, reference category; RR, rate ratio.
DISCUSSION
The study findings indicate that the rates of the two most common categories of preventive services, prophylaxis and remineralisation, demonstrated variation according to characteristics spanning patient demographics, visit factors and oral health. A common pattern was observed for both prophylaxis and remineralisation services, comprising lower rates for older patients, those attending for emergency reasons and those with decayed teeth. In contrast, higher rates were observed for prophylaxis and remineralisation services for insured patients and those with a higher number of natural teeth.
The findings come from a national survey that was drawn from a sampling frame that may be considered comprehensive, and the response rate was adequate. The findings are weighted to produce representative estimates of private general practice in Australia. The majority (78%) of Australian dentists work in private practice only, and 88% of the population ≥ 5 years of age who made a dental visit in the last year reported last visiting a private dentist20. However, a potential limitation is that dental service rates vary between the private and public sectors21 and according to the geographical location22., 23., as these may reflect different delivery systems with potentially different patient pools and disease patterns. For example, the percentage of people who attend a public sector dentist tends to be higher among lower-income groups; and public dental care is reported to have higher levels of emergency care and service profiles, with higher extraction rates, than the private sector21. Further research is required to investigate whether similar patterns of preventive services apply to public sector and rural locations. An additional consideration is that of bias emanating from the collection of data on services using a self-selection method based on a typical day. However, significant differences in service rates were not found when data that were collected over a sampling period of 10 days were assessed against estimates from a single typical day24.
Rates of prophylaxis services were lowest in the older age group, which could reflect the higher rates of tooth loss among older adults. However, the lower rate of dental prophylaxis persisted in the adjusted model that included number of teeth. This could indicate other potential reasons for such age-related service patterns, such as routines in clinical decision making and in practice styles of dental providers24., 25.. The rates of remineralisation services were also lower among older age groups and exhibited a consistent gradient in service rates from children to younger and middle-aged adult age groups and finally to older adults. This is not consistent with the prevalence of decay in adults, which has been shown to occur at a similar level across all adult age groups in Australia26. Therefore, it is possible that minimal intervention dentistry in adults could be expanded. Minimal intervention approaches involve an evidence-based rationale for preventive and cause-related management of oral diseases27. However, initial and cavitated carious lesions tend to be treated similarly through restorative interventions28., 29.. This may reflect difficulties in adopting evidence-based preventive care, which requires considerable effort, motivation and coordination by a dental practice30, and account for the substantial variation reported in practice patterns of dentists related to preventive dentistry31.
In this study, it was found that having dental insurance was related to higher rates of dental prophylaxis services as well as of remineralisation services. Insurance is generally considered as an enabling variable that can facilitate access32 and is also consistent with more favourable service patterns, such as more preventive care but lower likelihood of extractions33. Those on lower incomes tend to have lower coverage for dental insurance than those on higher incomes34, and increases in income-related inequality in dental care use have been reported35. However, benefits from insurance may be greater among lower socio-economic status groups in terms of visiting and oral health36., 37., so policies that could improve insurance coverage for those on lower incomes may be beneficial.
Emergency visits for the relief of pain tend to be more prevalent among lower income groups, but adjusted models have shown lack of insurance and the presence of oral health impacts to be significantly associated with visits because of an emergency38. In this study, emergency visits and worse oral health status were related to lower preventive service rates. Visit patterns for relief of pain may work against preventive treatment decisions and create a paradoxical situation in which those who are worse off in relation to oral health and dental-care access are less likely to receive preventive services. Oral health inequalities have been demonstrated in relation to tooth loss, periodontal disease and caries for measures of social position, such as education, occupation and income39., 40., 41.. Oral health policy to maintain good oral health recognises the need for services, such as promotion of health, prevention and early intervention, that are appropriate and affordable, as well as for treatment, across the whole population42.
CONCLUSIONS
Preventive services were related to the age of the patient, characteristics of visits and to oral health. The similar pattern of associations for both prophylaxis and remineralisation services suggests that patients who are better off in relation to possessing dental insurance and having a higher number of teeth, have a greater likelihood of receiving dental care of a preventive nature. In contrast, those worse off, in terms of attending for an emergency visit for relief of pain and having decayed teeth, have a lower likelihood of receipt of preventive services. This could indicate that those most in need are missing out on the benefits of preventive dental care. It is important for dentistry to focus on prevention and to support the concept of a healthy dentition for life.
Acknowledgements
This work was supported by the Australian Government Department of Health and Ageing, National Health and Medical Research Council (NHMRC), and Australian Institute of Health and Welfare and was written with support from the NHMRC (1031310). The contents are the responsibility of the administering institution and authors, and do not reflect the views of the NHMRC.
Competing interests
The authors declare no conflicts of interest.
References
- 1.Garcia RI, Sohn W. The paradigm shift to prevention and its relationship to dental education. J Dent Educ. 2012;76:36–45. [PubMed] [Google Scholar]
- 2.Hayashi M, Haapasalo M, Imazato S, et al. Dentistry in the 21st century: challenges of a globalising world. Int Dent J. 2014;64:333–342. doi: 10.1111/idj.12132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Featherstone JD, Domejean S. Minimal intervention dentistry: part 1. From ‘compulsive’ restorative dentistry to rational therapeutic strategies. Br Dent J. 2012;213:441–445. doi: 10.1038/sj.bdj.2012.1007. [DOI] [PubMed] [Google Scholar]
- 4.Seppä L. The future of preventive programs in countries with different systems for dental care. Caries Res. 2001;35:26–29. doi: 10.1159/000049106. [DOI] [PubMed] [Google Scholar]
- 5.Thomson WM, Williams SM, Broadbent JM, et al. Long-term dental visiting patterns and adult oral health. J Dent Res. 2010;89:307–311. doi: 10.1177/0022034509356779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crocombe LA, Broadbent JM, Thomson WM, et al. Dental visiting trajectory patterns and their antecedents. J Pub Health Dent. 2011;71:23–31. doi: 10.1111/j.1752-7325.2010.00196.x. [DOI] [PubMed] [Google Scholar]
- 7.Crocombe LA, Broadbent JM, Thomson WM, et al. Impact of dental visiting trajectory patterns on clinical oral health and oral health-related quality of life. J Pub Health Dent. 2012;72:36–44. doi: 10.1111/j.1752-7325.2011.00281.x. [DOI] [PubMed] [Google Scholar]
- 8.Astrom AN, Ekback G, Ordell S, et al. Long-term routine dental attendance: influence on both tooth loss and oral health-related quality of life in Swedish older adults. Community Dent Oral Epidemiol. 2014;42:460–469. doi: 10.1111/cdoe.12105. [DOI] [PubMed] [Google Scholar]
- 9.Brennan DS, Spencer AJ. Dental visiting history between ages 13 and 30 years and oral health-related impact. Community Dent Oral Epidemiol. 2014;42:245–262. doi: 10.1111/cdoe.12077. [DOI] [PubMed] [Google Scholar]
- 10.Australian Institute of Health and Welfare. Harford JE, Islam S. AIHW; Canberra: 2013. Adult oral health and dental visiting in Australia: results from the National Dental Telephone Interview Survey 2010. [Google Scholar]
- 11.Brennan DS, Balasubramanian M, Spencer AJ. Trends in dental service provision in Australia: 1983-84 to 2009-10. Int Dent J. 2015;65:39–44. doi: 10.1111/idj.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brennan DS, Spencer AJ. Diagnostic and preventive services trends: 1983-84 to 1998-99. Aust Dent J. 2003;48:43–49. doi: 10.1111/j.1834-7819.2003.tb00008.x. [DOI] [PubMed] [Google Scholar]
- 13.Spencer AJ, Szuster FSP, Brennan DS. Service-mix provided to patients in Australian private practice. Aust Dent J. 1994;39:316–320. doi: 10.1111/j.1834-7819.1994.tb05569.x. [DOI] [PubMed] [Google Scholar]
- 14.Brennan DS, Spencer AJ, Szuster FSP. Service provision trends between 1983-84 and 1993-94 in Australian private general practice. Aust Dent J. 1998;43:331–336. doi: 10.1111/j.1834-7819.1998.tb00184.x. [DOI] [PubMed] [Google Scholar]
- 15.Brennan DS, Spencer AJ. Trends in service provision among Australian private general dental practitioners over a 20-year period. Int Dent J. 2006;56:215–223. doi: 10.1111/j.1875-595x.2006.tb00097.x. [DOI] [PubMed] [Google Scholar]
- 16.Chrisopoulos S, Nguyen T. AIHW; Canberra: 2012. Trends in the Australian Dental Labour Force, 2000 to 2009: Dental labour force collection, 2009. [Google Scholar]
- 17.Australian Dental Association . 10th ed. ADA; Sydney: 2013. The Australian Schedule Of Dental Services And Glossary. [Google Scholar]
- 18.Elias AC, Sheiham A. The relationship between satisfaction with mouth and number and position of teeth. J Oral Rehab. 1998;25:649–661. doi: 10.1046/j.1365-2842.1998.00313.x. [DOI] [PubMed] [Google Scholar]
- 19.Sheiham A, Steele JG, Marcenes W, et al. The relationship between oral health status and body mass index among older people: a national survey of older people in Great Britain. Br Dent J. 2002;192:703–706. doi: 10.1038/sj.bdj.4801461. [DOI] [PubMed] [Google Scholar]
- 20.Chrisopoulos S, Harford JE. AIHW; Canberra: 2013. Oral health and dental care in Australia: key facts and figures 2012. [Google Scholar]
- 21.Brennan DS, Spencer AJ, Slade GD. Service provision among adult public dental service patients: baseline data from the Commonwealth Dental Health Program. Aust NZ J Pub Health. 1997;21:40–44. doi: 10.1111/j.1467-842x.1997.tb01652.x. [DOI] [PubMed] [Google Scholar]
- 22.Brennan DS, Spencer AJ, Slade GD. Provision of public dental services in urban, rural and remote locations. Community Dent Health. 1996;13:157–162. [PubMed] [Google Scholar]
- 23.Brennan DS, Spencer AJ, Szuster FSP. Rates of dental service provision between capital city and non-capital locations in Australian private general practice. Aust J Rural Health. 1998;6:12–17. doi: 10.1111/j.1440-1584.1998.tb00275.x. [DOI] [PubMed] [Google Scholar]
- 24.Brennan DS, Spencer AJ, Szuster FSP. Dentist service rates and distribution of practice styles over time. Community Dent Oral Epidemiol. 1996;24:145–151. doi: 10.1111/j.1600-0528.1996.tb00832.x. [DOI] [PubMed] [Google Scholar]
- 25.Brennan DS, Spencer AJ. Factors influencing choice of treatment by private general practitioners. Int J Behav Med. 2002;9:94–110. doi: 10.1207/s15327558ijbm0902_02. [DOI] [PubMed] [Google Scholar]
- 26.Slade GD, Spencer AJ, Roberts-Thomson KF, Australia’s dental generations . Australian Institute of Health and Welfare; Canberra: 2007. The National Survey of Adult Oral Health 2004-06. [Google Scholar]
- 27.Banerjee A, Domejean S. The contempory approach to tooth preservation: minimum intervention (MI) caries management in general practice. Prim Dent J. 2013;2:300–307. doi: 10.1308/205016813807440119. [DOI] [PubMed] [Google Scholar]
- 28.Brennan DS, Spencer AJ. Service patterns associated with coronal caries in private general dental practice. J Dent. 2007;35:570–577. doi: 10.1016/j.jdent.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 29.Brennan DS, Balasubramanian M, Spencer AJ. Treatment of caries in relation to lesion severity: implications for minimum intervention dentistry. J Dent. 2015;43:58–65. doi: 10.1016/j.jdent.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 30.Sbaraini A, Carter SM, Evans RW, et al. How do dentists and their teams incorporate evidence about preventive care? An empirical study. Community Dent Oral Epidemiol. 2013;41:401–404. doi: 10.1111/cdoe.12033. [DOI] [PubMed] [Google Scholar]
- 31.Yokoyama Y, Kakudate N, Sumida F, et al. Dentists’ practice patterns regarding caries prevention: results from a dental practice-based research network. BMJ Open. 2013;3:e003227. doi: 10.1136/bmjopen-2013-003227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Teusner DN, Brennan DS, Spencer AJ. Dental insurance, attitudes to dental care and dental visiting. J Pub Health Dent. 2013;73:103–111. doi: 10.1111/j.1752-7325.2012.00345.x. [DOI] [PubMed] [Google Scholar]
- 33.Brennan DS, Spencer AJ, Szuster FSP. Insurance status and provision of dental services in Australian private general practice. Community Dent Oral Epidemiol. 1997;25:423–428. doi: 10.1111/j.1600-0528.1997.tb01733.x. [DOI] [PubMed] [Google Scholar]
- 34.Manski RJ, Macek MD, Moeller JF. Private dental coverage: who has it and how does it influence dental visits and expenditures? J Am Dent Assoc. 2002;133:1551–1559. doi: 10.14219/jada.archive.2002.0087. [DOI] [PubMed] [Google Scholar]
- 35.Fitzgerald EM, Cunich M, Clarke PM. Changes in Inequalities of Access to Dental Care in Australia 1977-2005. Aust Econ Rev. 2011;44:153–166. [Google Scholar]
- 36.Anikeeva O, Brennan DS, Teusner DN. Household income modifies the association of insurance and dental visiting. BMC Health Serv Res. 2013;13:432. doi: 10.1186/1472-6963-13-432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Teusner DN, Anikeeva O, Brennan DS. Self-rated dental health and dental insurance: modification by household income. Health Qual Life Outcomes. 2014;12:67. doi: 10.1186/1477-7525-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brennan DS, Anikeeva O, Teusner DN. Dental visiting by insurance and oral health impact. Aust Dent J. 2013;58:344–349. doi: 10.1111/adj.12082. [DOI] [PubMed] [Google Scholar]
- 39.Schwendicke F, Dorfer CE, Schlattmann P, et al. Socioeconomic inequality and caries: a systematic review and meta-analysis. J Dent Res. 2015;94:10–18. doi: 10.1177/0022034514557546. [DOI] [PubMed] [Google Scholar]
- 40.Peres MA, Luzzi L, Peres KG, et al. Income-related inequalities in inadequate dentition over time in Australia, Brazil and USA adults. Community Dent Oral Epidemiol. 2015;43:217–225. doi: 10.1111/cdoe.12144. [DOI] [PubMed] [Google Scholar]
- 41.Borrell LN, Crawford ND. Socioeconomic position indicators and periodontitis: examing the evidence. Periodontol. 2000;2012:69–83. doi: 10.1111/j.1600-0757.2011.00416.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.National Advisory Committee on Oral Health . Australian Health Ministers’ Conference; Canberra: 2004. Healthy mouths, healthy lives, Australia’s National Oral Health Plan 2004-2013. [Google Scholar]