Abstract
Objective: The aim of this study was to analyse the potential health effects of occupational exposure of denturists in the Łódź province. Methods: The survey was performed among 103 denturists working in 24 dental laboratories in the Łódź province using the questionnaire prepared by the authors. Results: The most common health problems associated with work (occurring daily or at least once a week) were: back pain (69.8%); chronic fatigue syndrome (61.6%); irritation, itching and rashes on the hands (51.2%); restlessness and aggression (43.0%); and watery and itchy eyes (41.9%). Psychosocial and ergonomic hazards associated with work organisation (72.2%) were the most common work environment factors related to the denturist profession. Conclusions: Analyses of denturists’ occupational exposure in the Łódź province and epidemiological estimates of the health effects suggest the need for preventive measures.
Key words: Denturist, occupational hazards, work environment factors, occupational exposure, health problems
INTRODUCTION
The work of denturists (i.e. clinical dental technicians) is associated with exposure to a number of physical, chemical, biological, ergonomic and psychosocial factors that result in risks for health problems, such as occupational or work-related diseases, accidents and injuries.
The most common hazards occurring in the workplace of a denturist include the following: cuts from sharp and/or moving parts; burns; electric shocks; and a number of consequences from fires and/or explosions1.
Sharp, protruding parts, pressurised fluids, slippery uneven surfaces, moving machine parts, tools and work pieces are examples of the mechanical hazards encountered. Procedures intended to impart the required shape and the desired physical and chemical properties to manufactured products are those associated with the highest risk in comparison with other risk factors of injury or accident at work among denturists. The particles dispersed during processing of material typically result in closed or open trauma to the eyeball. The risks of mechanical injury to the eyes are greatest during the grinding of metals and metal alloys, the mechanical treatment of acrylic resin and the cutting of orthodontic wire2., 3..
Minor skin injuries, such as burns, bruises and cuts, are seen as inevitable and not posing a significant risk to human health, despite their high incidence among denturists4.
Denturists are exposed to the following thermal hazards: open flame; infrared radiation (from molten metal and metal alloys during the processes of casting and soldering); splashes of molten metal; and direct contact with hot objects5. Infrared radiation (heat) is mostly absorbed in the superficial layers of the skin and the eyeball and prolonged exposure to high-intensity radiation may result in thermal erythema or skin burns, cataracts, iritis, conjunctivitis, palpebral and corneal irritation and marginal blepharitis.
Chemical burns associated with the denturist’s job arise from contact of the skin or mucous membranes with formulations containing corrosive chemicals, such as acids, bases or salts of heavy metals (e.g. hydrochloric acid, hydrofluoric acid and boric acid).
Noise exposure among denturists results from the use of devices that generate noise at both audible and inaudible sound frequencies. The average noise levels in denturist laboratories range from 65 dB to 83 dB but the sound pressures produced when fabricating prosthetic devices are much higher6., 7., 8.. Prolonged occupational exposure to noises from several sources deployed in a single room represents a real risk for hearing-organ damage in denturists, particularly those who do not use personal protective equipment (PPE)9., 10..
The average daily exposure time of denturists to the mechanical vibrations specified above is approximately 4 hours. The sources of the vibration include the following: prosthetic pneumatic turbines; gypsum model cutting saws; gypsum trimming cutters; polishing grinders; vacuum stirrers; and chipping chisels11.
Ocular disorders, including conjunctivitis, dry eye syndrome and watery eyes, are the most common symptoms reported by denturists; over 78.71% of denturists experience at least one of these problems12. Numerous allergies that typically manifest as conjunctivitis and keratitis result from direct contact of the affected tissues with the environment and the allergic substances found in it to cause burning, itching, lacrimation, photophobia and, in their advanced form, vision disorders13. Common symptoms of dry eye syndrome include itching, burning, redness, sensation of foreign bodies under the eyelids and double vision14.
Despite the use of exhaust systems, denturist room atmospheres are periodically polluted with dusts and vapours of, for example, cobalt, methyl methacrylate or other acrylic compounds, pumice stone suspensions, concentrated acid and alkali fumes and disinfectants, resulting in or contributing to the development of, for example, contact allergies, immediate-type allergies, asthma, chronic obstructive pulmonary disease, pneumoconiosis and other lung diseases, such as fibrosis or even cancer15., 16., 17..
Biological contaminants represent another group of harmful agents in the environment. Hepatitis B virus (HBV) infection is a major occupational hazard for denturists. A significantly higher frequency of serological markers of HBV has been recorded in denturists (2.7%) compared with the general population (0.8%)18. It seems reasonable to expect that the adverse health effects of hepatitis C virus (HCV) infections will be seen, as a vaccine is not available, and the period of preclinical symptoms may be several years. This long asymptomatic period of the majority of HCV infections may cause severe underestimation of the risk of developing HCV in the population of denturists.
The problems attributable to the harmful physical, chemical and biological factors described above are further aggravated by ergonomic and psychosocial factors. The effects of prolonged forced body positions, repetitive activities that lead to monotony, annoying microclimate conditions, the need for continuous concentration on very small details, the need to follow restrictive technological procedures, emotional stress associated with the final result of the work (i.e. the need to satisfy the dentist placing the order) and fear of infection, in combination with limited ability to apply protective measures (gloves, masks, goggles, etc.) results not only in chronic disorders of the musculoskeletal system but also in dysfunction of the peripheral nervous system and the development of stress, chronic fatigue and burnout.
Pain in the cervical and lumbosacral spine is characteristic of denturists. A relationship has been found between the occurrence of back pain and tingling in the arms and fingers, with the daily working time of denturists (average 12–13 hours)19. Carpal tunnel syndrome, manifest as persistent numbness, tingling and radiating pain in the wrist, difficulty in picking up and holding objects and reduced dexterity, is one of the most frequently recognised work-related medical conditions in this occupational group20.
In the past two decades, very unfavourable organisational and economic changes in the Polish model of dental care have occurred. Very low public expenditure for the dental health sector (approximately 19 USD/person/year) has resulted in the rapid reduction of the public sector and spontaneous development of the private sector. The very limited scope of the dental services offered by the public sector and the several-month wait times have resulted in over 70% of patients using paid dental services (particularly prosthetic services) offered by private dental offices. Dentists in the private sector almost exclusively perform curative dentistry procedures, which results in the cooperation of denturists with private dentists financially attractive. However, for financial reasons, only approximately 30% of people requiring prosthetic treatment decide to pay for prosthetic services in private clinics, which results in lower demand for denturist services and severe competition in this professional milieu. Over 70% of technicians are employed under interim contracts or are self-employed. Therefore, the long list of harmful physical, chemical and biological agents and conditions associated with the denturist’s job also includes adverse psychosocial factors.
Aim and research problems
The main aims of this study were to analyse and evaluate the prevalence of adverse health effects of occupational exposure to harmful agents among denturists in the Łódź province of Poland and to analyse and evaluate the use of preventive measures and compliance with safety rules among those denturists.
These aims were achieved by providing answers to the following questions:
-
•
What are the work-related health problems that are most frequently reported by denturists?
-
•
What types of occupational hazards are most common in the denturist workplace?
-
•
Does the use of PPE reduce the frequency of injuries and accidents in the workplace?
-
•
Is working in awkward postures related to the frequency of musculoskeletal disorders in the form of increased tension in the muscles of the head, neck and pectoral girdle, and to back pain?
-
•
Does excessive noise in the denturist laboratory result in tinnitus and feelings of pressure within the ear and head?
-
•
Does exposure to methyl methacrylate result in irritation, itching or eczema on the skin or hands?
-
•
Is insufficient lighting related to the frequency of lacrimation, itchy eyes or conjunctival hyperaemia and swelling?
METHODS
A diagnostic questionnaire survey was the main research tool.
The questionnaire was divided into three parts. The first part consisted of analysis and assessment of the somatic and psychosomatic ailments related to the denturists’ job; the second part included analysis and evaluation of the harmful agents associated with the denturists’ workplace; and the third part contained analysis and evaluation of the application of preventive measures and compliance with safety rules among denturists.
The study was anonymous and voluntary, and was performed via direct interviews between April 2014 and July 2014 in 24 denturist laboratories located in 13 communities of the Łódź province. The 254 denturist laboratories in the area of the Łódź province identified in the database of the Business Activity Central Register and Information Record as of 4 July 2014 were used as the sampling frame. The search criteria were based on code PKD 32.50.Z – production of medical (including dental) materials, instruments and products.
A group of 35 denturist laboratories was randomly selected. The ‘success ratio’ was 68.57%, and 24 denturist laboratories were recruited for the study. Written, informed consent was obtained from all owners of the dental technology laboratories and from the respondents before their participation in the survey. All technicians employed initially participated in the study. As many as 112 occupationally active denturists were recruited for the study, and 103 (91.96%) were ultimately included (nine people withdrew from the study).
The study protocol was approved by the Bioethics Committee of the Medical University of Łódź (document no. RNN/360/14/KB of 05.13.2014), in full accordance with the Declaration of Helsinki of the World Medical Association.
The analysis and interpretation of the data were performed with Microsoft Excel 2010. A chi-square (χ2) test was used to evaluate the research hypothesis, and the Yule coefficient φ was applied to examine the strength of the association. The level of statistical significance was set at P ≤ 0.05.
RESULTS
Characteristics of the study group
In the group of respondents, 57 (55%) were women and 46 (45%) were men, and the age-range of the participants was 22–57 years. The arithmetic mean age was 34 years, and the median and mode were 33 and 29 years, respectively.
Among the respondents, 31.1% and 5.8% were under the age of 30 years and above the age of 45 years, respectively. Nearly two-thirds (63.1%) of the respondents were 30–45 years of age. Women dominated the age group under 30 years (21.4%) and the age group 30–45 years (32%), and men dominated in the age group > 45 years (3.9%). In terms of education, the dominant group included denturists with secondary vocational education (28.2%), followed by higher undergraduate/engineering (23.3%) and postsecondary education (21.4%). The respondents with basic vocational education were the least numerous (5.8%). For the women, 14.6% had post-secondary/college education, and 13.6% had a bachelor’s degree/engineer education. Compared with the women, the men more frequently had had secondary (17.5%) and basic (4.9%) vocational education. Almost four times more women (10.7%) than men (2.9%) had a college education. More than half (56.3%) of the respondents worked in towns with 10,000–100,000 residents. Of the 42 people who worked in towns with over 500,000 residents, 59.5% were women. Among respondents, 39.8% were denturists employed in fixed-term, full-time jobs, and more than one-third were self-employed and running their own businesses.
Nearly half of the respondents (48.5%) had worked as denturists for over 10 years, and among these respondents, 26.2% had worked for longer than 15 years. The duration of employment of one-third (33%) of the respondents was 5–10 years. As many as 80.6% of the respondents reported spending more than 8 hours per day performing their occupational duties, and nearly one-third (31.1%) of these respondents worked for longer than 10 hours per day.
Occupational exposure and health effects among denturists
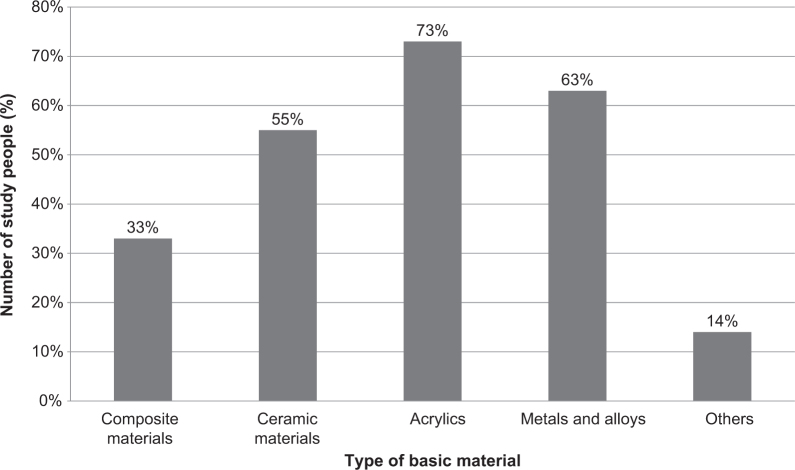
The data revealed that 73% of the denturists came into contact with acrylic plastics, 63% with metals and their alloys, 55% with ceramics and 33% with composite materials. Contact with other materials (e.g. zirconium, acetate and polyamide plastics) was reported by 13.6% of participants (Figure 1).
Figure 1.
Percentage of respondents in contact with the basic materials used in their workplace (n = 103; percentage values do not sum to 100 as multiple answers were possible).
More than half of the respondents came into contact with three or more potentially hazardous basic materials in the workplace. 36.9% of denturists were exposed to two such materials. Only one in eight (12.6%) respondents came into contact with a single material.
A considerable majority of the denturists (83.5%) reported health complaints associated with their occupation within the previous 12 months. Half of the woman (50.5%) and one-third of man (33.0%) experienced health effects of occupational exposure. The men were 2.4 times more likely than the women to report no health complaints associated with occupational exposure (11.7% vs. 4.9%).
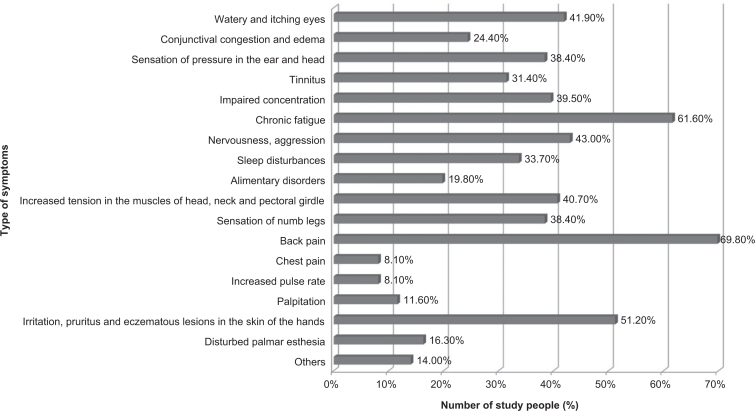
The most frequently experienced (daily or at least once a week) work-related health problems included: low back pain (69.8%); chronic fatigue (61.6%); dermal irritation, itching and eczematous changes (51.2%); nervousness and aggression (43.0%); and watery and itchy eyes (41.9%) (Figure 2). 44.2% of respondents simultaneously experienced four to six symptoms, 36 (41.8%) experienced one to three or seven to nine symptoms, and one in seven of the 86 (13.9%) reported more than 10 symptoms. The women frequently complained of backache (46.5%); chronic fatigue (37.2%); irritation, itching and eczematous changes in the skin of the hands (30.2%); and increased muscle tension in the head, neck and shoulder girdle (25.6%). The most common health effects of occupational exposure in the men included chronic fatigue (24.4%); back pain (23.3%); irritation, itching and eczematous changes in the skin of the hands (20.9%); and nervousness and aggression (19.8%). Sleep disorders were slightly more common among the men (17.4%) than the women (16.4%). Of the 86 respondents who experienced health problems, 12 (13.9%) reported other symptoms, such as choking cough, cramps in the feet and calves as a result of varicose veins, headaches and dizziness, and sore throat.
Figure 2.
Work-related somatic/psychosomatic symptoms experienced most commonly by denturists (n = 86; percentage values do not sum to 100 as multiple answers were possible).
An association was identified between working in awkward postures and the occurrence of musculoskeletal disorders in the form of increased tension in the muscles of the head, neck and shoulder girdle or back pain (χ2 = 39.05 > χ2 p, ƴ = 3.8415). To investigate the strength of this association, the Yule strength factor φ was calculated (φ = 0.61) and revealed that the strength of the association between working in an awkward posture and the occurrence of musculoskeletal disorders in the form of increased tension of the muscles of head, neck and shoulder girdle or back pain was significant.
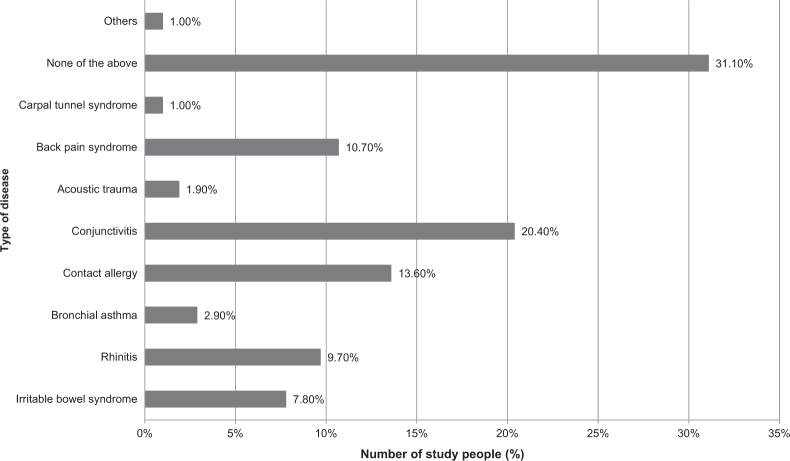
Of the 103 people who participated in the study, 32 (31.1%) reported that they had received a diagnosis of one of the diseases listed in Figure 3 within the previous 12 months. One in five (20.4%) of the participants had been diagnosed with conjunctivitis, one in seven (13.6%) had contact allergies and one in nine (10.7%) denturists experienced back pain. One person reported a diagnosis of carpal tunnel syndrome, and another reported some other type of disease (i.e. gastric ulcer). Among the 71 denturists, 26 (36.6%) declared that they had been diagnosed, within the previous 12 months, with one of the specified disorders, and 45 (63.4%) reported diagnoses of more than one of the disorders.
Figure 3.
Frequency of the diagnoses of selected diseases among denturists (n = 103; percentage values do not sum to 100 as multiple answers were possible).
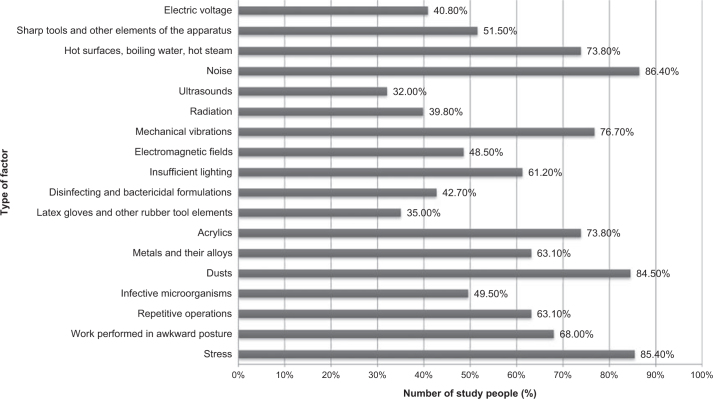
The factors that were most frequently reported to be present in the work environment were ergonomic and psychosocial factors related to work organisation (72.2%), chemicals and dusts (59.8%) and physical factors (57.4%). The awareness of occupational exposure to biological agents (49.5%) seemed to be inadequate. The most frequently identified dangerous and harmful factors in the denturists’ workplaces were: noise (86.4%), stress (85.4%), dusts (84.5%), mechanical vibration (76.7%), acrylics (73.8%) and hot surfaces, boiling water and hot steam (73.8%) (Figure 4). The association between noise in technical laboratories and the occurrence of tinnitus or feelings of pressure in the head and ear was significant (χ2 = 56.1 > χ2 p, ƴ = 3.8415). To investigate the strength of this association, the Yule factor φ was calculated (φ = 0.73), and the strength of the dependence of the occurrence of tinnitus or feelings of pressure in the head and ear on noise in technical laboratories was considerable.
Figure 4.
Examples of harmful factors found in the denturists’ workplace (n = 103; percentage values do not sum to 100 as multiple answers were possible).
We also identified a significant correlation between occupational exposure to the methyl methacrylate present in the acrylic plastics and the incidence of dermal irritation, itching or the eczematous lesions on the skin of the hands (χ2 = 15.79 > χ2 p, ƴ = 3.8415). To assess the strength of the interaction between these specified characteristics, the Yule coefficient φ was calculated (φ = 0.75), and the strength of the association between occupational exposure to methyl methacrylate found in acrylic materials with irritation, itching or eczema on the skin of the hands was considerable.
Insufficient lighting in the workplace was reported by 61.2% of denturists. There was no correlation between low light intensity and the occurrence of eye lacrimation and itching or conjunctival hyperaemia and oedema (χ2 = 0.79 < χ2 p, ƴ = 3.8415).
The denturists were least concerned with exposure to potentially harmful factors such as ultrasound (32.0%), latex gloves and other rubber tools or parts (35.0%) and radiation (39.8%).
Over half (56.3%) of the participating denturists, including 30 women (29.1%) and 28 men (27%), reported experiencing an injury in the workplace within the month preceding the survey. Of these respondents, 48 (82.7%) worked longer than 8 hours per day, and of these respondents, 14 (24.1%) worked longer than 10 hours per day. The most common injuries experienced in the denturist workplace, by both men and women, include cuts or punctures (62.1%) and burns (46.6%). Two (3.4%) subjects reported acoustic trauma. Of the 58 people who experienced trauma in the workplace within the past 12 month, only one in four (22.4%) reported the occurrence of the injury in writing. Thirteen (22.4%) of the 58 denturists who had experienced an injury in the workplace within the last 12 months reported work absences because of the aforementioned injuries. The average duration of sick leave as a result of injury was up to 9 days for nine denturists, 10–29 days for three and more than 30 days for one.
Safety and hygiene rules in the denturists’ workplace
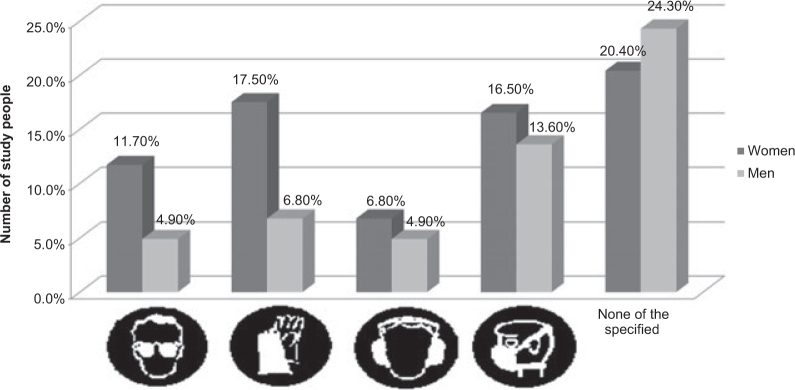
Among the 103 participating denturists, 46 (44.7%), including 21 (20.4%) women and 25 (24.3%) men, declared that they had not seen any of the listed signs pertaining to labour hygiene and safety in their workplace (Figure 5). The greatest number of denturists (31; 30.1%) declared that they had noticed a sign indicating the mandatory use of respiratory protection equipment, and 25 (24.3%) had noticed a sign indicating the mandatory use of hand protection equipment.
Figure 5.
Knowledge of the signs indicating the need to obey the safety and hygiene rules in the denturists’ workplace (n = 103; percentage values do not sum to 100 as multiple answers were possible).
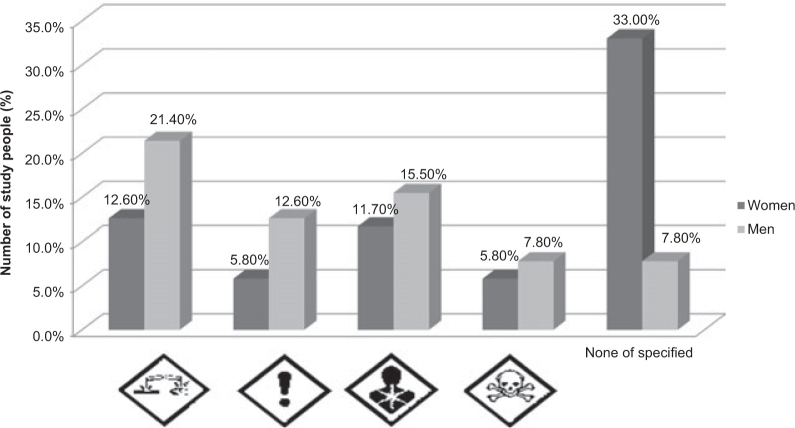
Moreover, 42 (40.8%) subjects, including 34 (80.9%) women and eight (19.1%) men, declared that none of the listed signs about the risk to human health were present at their workplace (Figure 6). The greatest numbers of subjects identified ‘Corrosive activity’ (21.4% of men and 12.6% of women) and ‘Health hazard’ (15.5% of men and 11.7% of women) signs. The men exhibited a 1.6-fold better knowledge of the signs indicating risks to human health than the women.
Figure 6.
Knowledge of the signs indicating the types of hazards to health (n = 103; percentage values do not sum to 100 as multiple answers were possible).
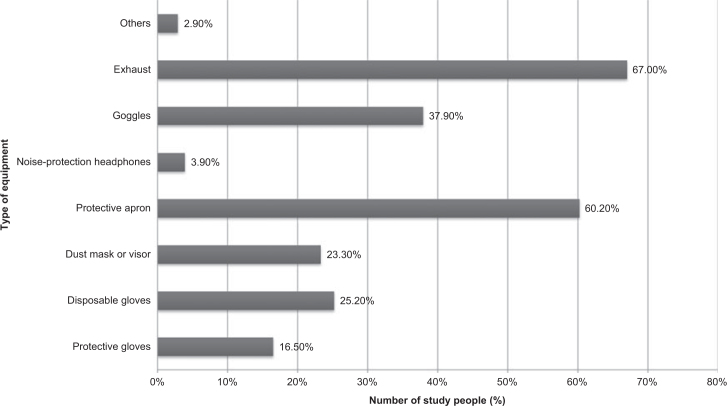
Seventy-five (72.8%) respondents, including 46 (44.7%) women and 29 (28.2%) men, declared that they utilised PPE in the workplace. Trauma was experienced by 23 (82.1%) of 28 respondents who did not apply safety measures and did not use PPE in the workplace and by 35 (46.7%) of 75 respondents who applied the measures and used the PPE. The risk of injury was 1.8-fold higher among the participants who did not comply with the safety measures and did not use PPE. The most commonly used safety measures and PPE in the workplace included exhaust systems (67.0%) and aprons (60.2%) (Figure 7). Protective glasses were used by slightly more than one-third (37.9%, n = 39) of respondents. Every fourth respondent used disposable gloves, every fifth used dust masks or protective visors, and every eighth wore gloves. Only four (3.9%) denturists used ear protection equipment. Among all respondents, three (2.9%) reported using other PPE, such as goggles and earplugs.
Figure 7.
Personal protective equipment (PPE) most frequently employed by denturists in their workplaces (n = 75; percentage values do not sum to 100 as multiple answers were possible).
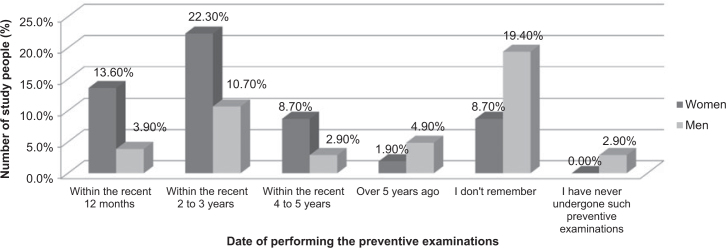
Nearly one-third (28.2%) of the respondents did not remember the date of their most recent preventive (pre-employment, periodic or follow-up) examination, and three declared that they had never undergone such an examination (Figure 8). The greatest numbers of denturists had undergone preventive examinations within the last 2–3 years (33.0%) or the last year (17.5%). Twelve and seven subjects had undergone preventive examinations within the last 4–5 years and more than 5 years ago, respectively. The women attended follow-up examinations more often than the men.
Figure 8.
Frequency of preventive examinations of denturists according to sex (n = 103; percentage values do not sum to 100 as multiple answers were possible).
Nearly half (45.6%) of the respondents [25 (24.3%) women and 22 (21.3%) men] rated their health as very good (14.6%) or good (38.8%). Every third respondent (35.9%) rated his/her health as average. Very poor or poor health was reported by four (3.9%) and 12 (6.8%) participants, respectively, and in equal proportions among women and men. Very poor or poor health was reported only by the participants who also reported work-related health problems.
DISCUSSION
The results of this study revealed that a considerable majority of the denturists experienced health problems resulting from various aspects of the work environment. Similar results have been reported in studies from Egypt12, Norway21 and South Korea22.
The symptoms that were experienced often (daily or at least once a week) included backache (69.8%); chronic fatigue (61.6%); irritation, itching and eczematous changes in the skin (51.2%); nervousness and aggression (43.0%); and watery/itching eyes (41.9%). Conjunctivitis was diagnosed in every fifth (20.4%) participant, contact allergies in every seventh (13.6%) and back pain syndrome in every ninth (10.7%). One person confirmed a diagnosis of carpal tunnel syndrome. Previous research has reported similar findings. Musculoskeletal pain was reported by 72.9% (n = 155) of denturists, dermatological changes in the hands by 60.65%, and dry eye syndrome and watery eyes by 78.71%12. Nakládalová 23 reported the results of tests performed in a group of 120 denturists; 63 (52.5%) complained of back pain, and carpal tunnel syndrome was diagnosed in four (3.3%). Jacobsen and Peterson21 examined a group of 201 denturists in Norway and found that 39% reported musculoskeletal problems and 28% complained of job-related dermal lesions.
In our earlier study, we demonstrated that the most common health-affecting circumstances of the denturist work environment include ergonomic and psychosocial factors and those related to work organisation (72.2%). Long-term exposure to stress was reported by 85.4% of the respondents. The results of other studies confirm that the denturist profession is highly stressful24. It is reasonable to assume that psychosocial factors affect the development of musculoskeletal disorders.
According to our results, the awareness of occupational exposure to biological agents seems to be inadequate (49.5%). This is corroborated by the results of another study, which found that only 13.1% of denturists disinfect dental impressions and that the same proportion uses disposable gloves25. Another publication reported that none of 155 denturists who participated in the study used disinfectant soap12.
Over half (56.3%) of the denturists had experienced injuries in the workplace within the previous month. The most common injuries in both men and women included puncture, cutting or piercing (62.1%) and burns (46.6%). In the study by Khalid, as many as 42.3% of the denturists reported eye injuries as a result of foreign bodies within the previous month2. Only one person in four submitted a written report about their injury. Moreover, every fourth respondent reported being on sick leave as a result of these injuries. It should be remembered that any claim is effective only after the accident or injury at work has been reported in writing to the respective authority. Therefore, it is reasonable to assume that the reportability of injuries at work and sick leave depend on the severity and type of injury experienced.
Interesting results were obtained regarding the subjects’ knowledge of the signs used to indicate the necessity of obeying work hygiene and safety rules and to indicate the types of hazards to human health. In denturist laboratories, exposure to dangerous and harmful agents often occurs only when performing certain procedures, or only in specific areas, which is why particularly dangerous areas in which the use of personal protective equipment is required are marked with suitable symbols or signs. Compared with men, women exhibited a 1.7-fold better knowledge of the mandatory symbols/signs used in the denturist workplace to ensure work safety. Nearly half of the denturists reported not seeing any of the listed symbols/signs in the workplace. However, the signs indicating inhalation, mutagenic, carcinogenic to reproductive cells, carcinogenic and aspiration hazards are placed on phosphate-bonded investment (refractory) materials; the skin corrosion and severe damage to eyes signs are placed on disinfectants; the acute toxicity sign is located on fluids used for electrolytic polishing of dental alloys; and skin irritation, eye irritation and irritation to the respiratory tract signs are located on the components of liquid acrylics. Compared with the women, the men exhibited a 1.6-fold better knowledge of the signs indicating danger to human health.
As many as 27.2% of the denturists did not apply any safety measures or utilise any personal protective equipment in the workplace. The risk of injury was 1.8-fold higher among those who did not follow safety recommendations or use personal protective equipment in the workplace. The results of the present study differ slightly from those obtained by Hamid and Mostafa who reported that 61.29% of denturists use a protective apron, 18.07% wear disposable gloves, 7.47% wear protective glasses and only 2.28% use protective masks12.
According to the results of this research, nearly one-third of denturists do not remember when they performed preventive (pre-employment or follow-up) examinations. It is reasonable to assume that the neglect of regular, extensive preventive examinations resulted in the frequent disorders that were diagnosed in this group.
A considerable association was demonstrated between working in an awkward position and the frequency of musculoskeletal disorders in the form of increased tension of the muscles of the head, neck and shoulder girdle or back pain. In another study, a correlation between back pain and tingling in the arms and fingers to daily working time, among denturists who worked more than 12–13 hours per day, was demonstrated19.
A considerable association between excessive noise in the laboratories and the occurrence of tinnitus or a feeling of pressure in the ear and head was demonstrated. It should be remembered that prolonged exposure to noise is not only annoying but also harmful. In the study by Hamid and Mostafa12 up to 77.42% of the denturists reported experiencing hearing problems. The results of a study conducted in Riyadh among 204 dental personnel, including 29 denturists, indicated that 16.67% of the respondents complained of tinnitus, 14.71% had difficulty understanding speech and 30.88% had difficulty understanding speech when there was noise10.
An association between occupational exposure to the methyl methacrylate and the frequency of irritation, itching or eczema of the skin of the hands was observed. This association has been confirmed by the results of clinical trials, including that of Rustemeyer and Frosch. These authors examined a group of 55 denturists exposed to methyl methacrylate and observed allergic contact dermatitis in 63.6% of the study subjects, eczematous lesions caused by contact with irritants in 23.6% and both types of contact dermatitis in 3.6%26.
The research hypothesis regarding the existence of a statistically significant correlation between low lighting and the occurrence of tearing and itching or conjunctival hyperaemia and oedema was rejected. It is believed that insufficient lighting is one of many risk factors for eye fatigue and ocular diseases. It should be noted that determination of the true influence of these variables on pain will be possible only through comparative studies of randomly selected experimental groups and controls. Denturists perform dozens of different tasks at different locations that require different types of light (i.e. variations in illumination angle, intensity and colour) during the workday. Therefore, even when the theoretically ‘good lighting’ of the entire laboratory meets the required technical standards, many technicians still indicate inadequate lighting during the manufacture of specific restorations.
Limitations
The questionnaire was developed based on the literature which deals with risk factors to which dental technicians are exposed in the workplace. We are unaware of any recent epidemiological studies on the spread of infection related to dental technicians’ work in Poland, and a broader investigation is needed.
CONCLUSIONS
The vast majority of denturists experience work-associated health problems. The most frequently reported work-related health problems include occupational musculoskeletal symptoms, such as back pain. The most common occupational hazards associated with the denturist’s job, as listed in the safety data sheet, include ergonomic and psychosocial factors and those related to work organisation. The use of personal protective equipment reduces the frequency of accidents and injuries. There is a statistically significant association between working in awkward postures and musculoskeletal disorders. Excessive noise in the denturist laboratory is the source of tinnitus and feeling of pressure in the ear and head. Occupational exposure to methyl methacrylate causes irritation, itching and/or eczematous lesions in the skin. These results highlight the need to intensify preventive measures to protect denturists from the effects of agents that are harmful to their health. Further research is necessary.
Acknowledgements
The authors thank the owners of the prosthetic laboratories for support which allowed the study to be conducted. The authors declare that the study received no financial support.
Conflicts of interest
The authors whose names are listed above certify that they have no affiliations with or involvement in any organisation or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.
References
- 1.PN-N-18002:2011 Systemy zarzadzania bezpieczenstwem i higiena pracy. Ogólne wytyczne do oceny ryzyka zawodowego. 2011. [Labor safety and hygiene management systems. General guidelines for the assessment of occupational risk, 2011.] (in Polish)
- 2.Khalid A. Prevalence of ocular injuries, conjunctivitis and use of eye protection among dental personnel in Riyadh, Saudi Arabia. Int Dent J. 2001;51:89–94. doi: 10.1002/j.1875-595x.2001.tb00828.x. [DOI] [PubMed] [Google Scholar]
- 3.Harley JL. Eye and facial injuries resulting from dental procedures. Dent Clin North Am. 1978;22:505–515. [PubMed] [Google Scholar]
- 4.McDonald RI, Walsh LJ, Savage NW. Analysis of workplace injuries in a dental school environment. Aust Dent J. 1997;42:109–113. doi: 10.1111/j.1834-7819.1997.tb00105.x. [DOI] [PubMed] [Google Scholar]
- 5.Staffanou RS, Ditmars DL, Drucker C, et al. Eye protection from light radiation. J Prosthet Dent. 1976;35:682–688. doi: 10.1016/0022-3913(76)90328-0. [DOI] [PubMed] [Google Scholar]
- 6.Sun J, Yao JJ, Tan Y, et al. Noise level in dental laboratory practice. Shanghai Kou Qiang Yi Xue. 2009;18:576–579. (in Chinese) [PubMed] [Google Scholar]
- 7.Kilpatrick HC. Decibel ratings of dental office sounds. J Prosthet Dent. 1981;45:175–178. doi: 10.1016/0022-3913(81)90336-x. [DOI] [PubMed] [Google Scholar]
- 8.Bahannan S, Abd El-Hamid A, Bahnassy A. Noise level of dental handpieces and laboratory engines. J Prosthet Dent. 1993;70:356–360. doi: 10.1016/0022-3913(93)90222-a. [DOI] [PubMed] [Google Scholar]
- 9.Setcos JC, Mahyuddin A. Noise levels encountered in dental clinical and laboratory practice. Int J Prosthodont. 1998;11:150–157. [PubMed] [Google Scholar]
- 10.Khalid A. Hearing problem among dental personnel. JPDA. 2005;14:17–24. [Google Scholar]
- 11.Nishiwaki Y. Cross-sectional study of health effects of methyl methacrylate monomer among Dental Laboratory Technicians. J Occup Health. 2001;43:375–378. [Google Scholar]
- 12.Hamida A, Mostafa A. Occupational health problems among a group of dental laboratory technicians in Alexandria City. Mansoura University. Conference paper. International Alexandria Conference 2002
- 13.Bogacka E, Groblewska A. Zapalenia spojówek – alergia czy zespół suchego oka? [Conjunctivitis – allergy or dry eye syndrome] Post Dermatol Alergol. 2009;26:372–374. (in Polish) [Google Scholar]
- 14.Prost M. Diagnostyka zaburzeń przed ocznego filmu łzowego. [Diagnosing of pre-ocular tear film abnormalities] Klin Oczna. 1991;93:29–30. (in Polish) [PubMed] [Google Scholar]
- 15.Leghissa P, Ferrari MT, Piazzolla S, et al. Cobalt exposure evaluation in dental prostheses production. Sci Total Environ. 1994;150:253–257. doi: 10.1016/0048-9697(94)90162-7. [DOI] [PubMed] [Google Scholar]
- 16.Farli M, Gasperini M, Francalanci M, et al. Occupational contact dermatitis in two dental technicians. Contact Dermatitis. 1990;22:282–287. doi: 10.1111/j.1600-0536.1990.tb01597.x. [DOI] [PubMed] [Google Scholar]
- 17.Murer AJ, Poulsen OM, Tuchsen F, et al. Rapid increase in skin problems among dental technician trainees working with acrylates. Contact Dermatitis. 1995;33:106–111. doi: 10.1111/j.1600-0536.1995.tb00510.x. [DOI] [PubMed] [Google Scholar]
- 18.Wilcox CW, Mayhew RB, Lagree JD, et al. Incidence of hepatitis B exposure among USAF dental laboratory technicians. Am J Dent. 1990;3:236–238. [PubMed] [Google Scholar]
- 19.Mori C. Three-years follow up study of health conditions among dental technicians. J Kurume Med Assoc. 1995;58:13–24. [Google Scholar]
- 20.Palmer KT, Clare H, Coggon D. Carpal tunnel syndrome and its relation to occupation: a systemic literature review. Occup Med. 2007;57:57–66. doi: 10.1093/occmed/kql125. [DOI] [PubMed] [Google Scholar]
- 21.Jacobsen N, Pettersen AH. Self-reported occupation-related health complaints among dental laboratory technicians. Quintessence Int. 1993;24:409–415. [PubMed] [Google Scholar]
- 22.In-ho J, Hyun-Soo B, Sook-Jeong L. The relationship between musculoskeletal symptoms and job stress of dental laboratories in workers. JCIT. 2013;8:317–323. [Google Scholar]
- 23.Nakládalová M. State of health in dental technicians with regard to vibration exposure and overload of upper extremities. Cent Eur J Public Health. 1995;3:129–131. [PubMed] [Google Scholar]
- 24.Locker D, Burman D, Otchere D. Work-related stress and its predictors among Canadian dental assistants. Community Dent Oral Epidemiol. 1989;17:263–266. doi: 10.1111/j.1600-0528.1989.tb00630.x. [DOI] [PubMed] [Google Scholar]
- 25.Frątczak B. O niektórych problemach związanych z dezynfekcją w gabinetach i pracowniach protetycznych na podstawie badań ankietowych lekarzy i techników dentystycznych [Remarks on some problems with disinfection in dental prosthetic laboratories based on questionnaire surveys among dentists and dental technicians] Prot Stom. 1994;6:319–323. (in Polish) [Google Scholar]
- 26.Rustemeyer T, Frosch PJ. Occupational skin diseases in dental laboratory technicians. Clinical picture and causative factors. Contact Dermatitis. 1996;34:125–133. doi: 10.1111/j.1600-0536.1996.tb02144.x. [DOI] [PubMed] [Google Scholar]