Abstract
BACKGROUND
Von Meyenburg complex (VMC) (i.e., biliary hamartoma) is a rare congenital disorder characterized by multiple dilated cystic bile ducts, without clear trends in sex or age predominance. Due to the low number of published cases and the lack of recognized guidelines, the management of such patients remains a clinical challenge.
CASE SUMMARY
We present a case of symptomatic VMC that was diagnosed after imaging and histopathological examinations. Considering the patient’s condition, a conservative treatment strategy was chosen. Instrumental, laboratory, and clinical follow-up demonstrated the stable condition of the patient receiving conservative treatment.
CONCLUSION
VMC is a potentially non-life threatening condition, but its recognition is crucial for the management of patients.
Keywords: Biliary hamartoma, Von Meyenburg complex, Liver polycystic disease, Ultrasonography imaging, Magnetic resonance imaging, Case report
Core Tip: Von Meyenburg complex (VMC) is a congenital bile duct malformation, which is asymptomatic and non-life threatening in most cases. As such, it remains underdiagnosed. Here, we report the features of VMC detected in a symptomatic patient by contrast-enhanced ultrasonography and magnetic resonance imaging. The prescribed treatment gradually improved the patient’s condition. Throughout the surveillance period, the patient remained asymptomatic. In reporting this case study, we highlight the need for thorough differential diagnosis of VMC as well as a personalized treatment approach that considers disease complications, if present.
INTRODUCTION
Biliary hamartoma or Von Meyenburg complex (VMC) is a congenital disorder that is characterized by multiple dilated cystic bile ducts. The discovery of such lesions in most cases is incidental, with an estimated incidence in the general population of 6%[1]. The formation of hamartomas has a genetic background and consists of remodeling of primitive ductal plate configurations[1]. The distinctive feature of these cystic hepatic lesions is that they do not communicate with biliary tracts, and are usually small (up to 1.5 cm), dimensionally similar with each other, and countless, producing a “starry sky” configuration[1]. Although in most cases hamartomas do not cause symptoms, VMC can have diverse clinical presentations, such as abdominal pain, fever, jaundice[2], and in rare cases, severe portal hypertension[3]. The condition can be diagnosed by ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI), contrast-enhanced magnetic resonance cholangiopancreatography (MRCP) in particular, where it appears as multiple irregularly-shaped lesions of about 10 mm diameter[2]. Multiple liver cystic lesions may cause diagnostic uncertainties, such as when mimicking liver metastasis on imaging[4]. In such cases, liver biopsy with subsequent histopathological evaluation is recommended[1]. Notably, blood analysis has not proven to be very useful due to the variability of findings and low specificity.
Complications of the condition include possible calcifications[5], portal hypertension[3], recurrent cholangitis with infectious complications[2] and malignization[1]. Currently no specific treatment is available, except treatment for symptomatic patients developing the abovementioned complications. Surveillance by US, MRI and/or MRCP is necessary, but clinical recommendations lack data on the frequency of check-ups[1].
Considering the variability of symptoms, imaging results, and possible inconclusiveness of histological evaluation, the knowledge of differential diagnostic features of the condition is essential to establish the correct diagnosis.
Here, we present a clinical case report, which is discussed from the point of differential diagnosis in order to combine the latest knowledge of clinicians, radiologists, and pathologists on biliary hamartoma.
CASE PRESENTATION
Chief complaints
A 57-year-old Caucasian woman complained of pain in the right hypochondriac region.
History of present illness
Fifteen days after a trip to Egypt, the patient was referred to a local hospital where her temperature was recorded at 38.5 °C. Laboratory examination showed increased cholestasis indices (alkaline phosphatase and gamma-glutamyl transferase > 5-6 times higher than the normal range) and acute inflammation of gall bladder as discovered during US. The patient was transferred to our unit for a second opinion.
History of past illness
The patient’s medical history was unremarkable.
Personal and family history
The patient’s family history was unremarkable.
Physical examination
Physical examination did not reveal any abnormality apart from painful sensations during palpation of the right hypochondriac area.
Laboratory examinations
Increased cholestasis indices were confirmed, and erythrocyte sedimentation rate and C-reactive protein were notably increased. Antinuclear, antimitochondrial, anti-smooth muscle actin, perinuclear anti-neutrophil cytoplasmic, and anti-Saccharomyces cerevisiae antibodies, and viral hepatitis markers were negative. Alpha fetoprotein, carcinoembryonic antigen, and carbohydrate antigen 19-9 were within normal limits.
Imaging examinations
Abdominal US scanning showed a coarse echostructure with irregularity of the liver surface, similar to that of a cirrhotic liver. Considering the marked inhomogeneity of the liver structure revealed by US scan, further contrast-enhanced US (CEUS) was performed (Figure 1), which showed some small areas of contrast washout during the portal phase. Due to the high suspicion of cirrhosis associated with neoplastic areas, an US-guided liver biopsy was performed (Figure 2). Histological examination hypothesized the diagnosis of liver hamartomas (small clusters of dilated biliary ducts surrounded by fibrous stroma with epithelial lining of biliary ducts formed by a single layer of cuboidal or flattened biliary epithelium) (Figure 3). Consequent MR cholangiography sequences enhanced with gadolinium-based contrast showed multiple hypointense nodular lesions on T1-weighted images, hyperintense lesions on T2-weighted images, and no enhancement in arterial phase after Gadolinium infusion. The lesions did not communicate with the biliary tract and a typical “starry sky” image was recorded (Figure 4). Based on the above-mentioned findings, the diagnosis of biliary hamartoma, first described by Von Meyenburg in 1918, was established.
Figure 1.
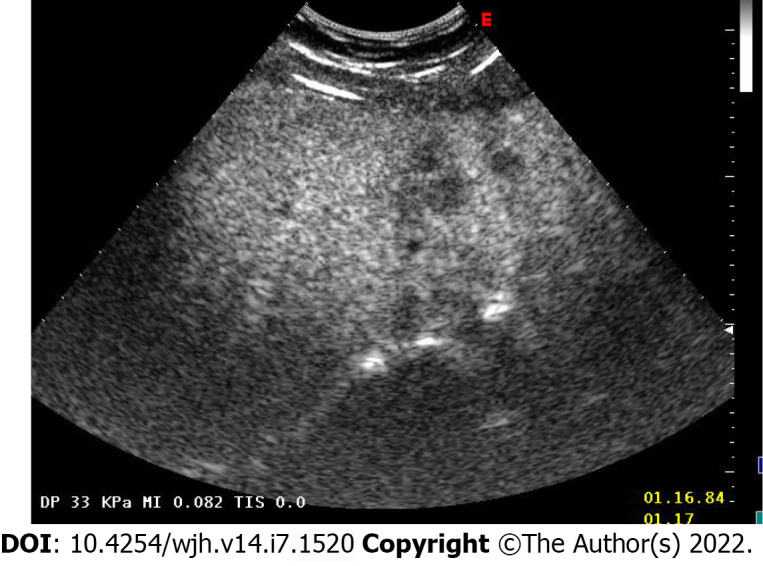
Abdominal contrast-enhanced ultrasound imaging of the patient. Marked echostructural inhomogeneity of the liver.
Figure 2.
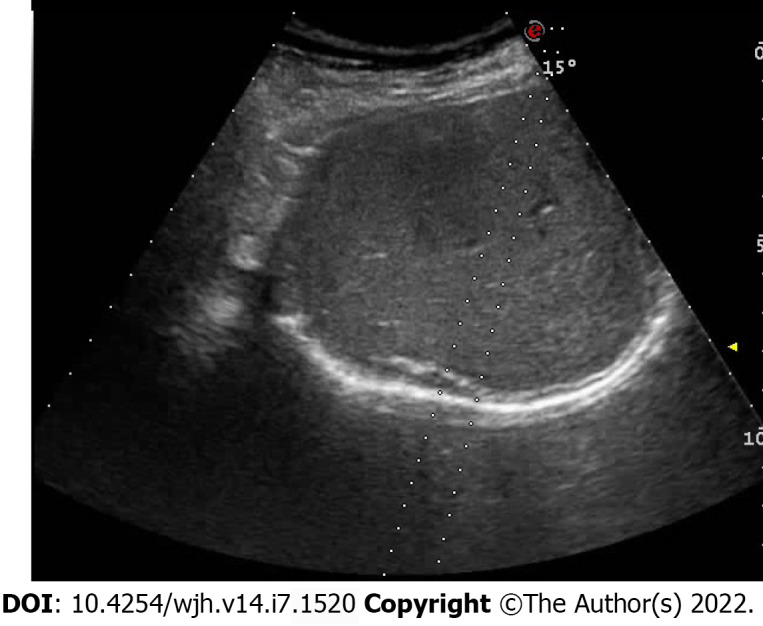
Ultrasound-controlled multiple needle liver biopsy. The procedure was performed to obtain hepatic tissue for histopathological examination.
Figure 3.
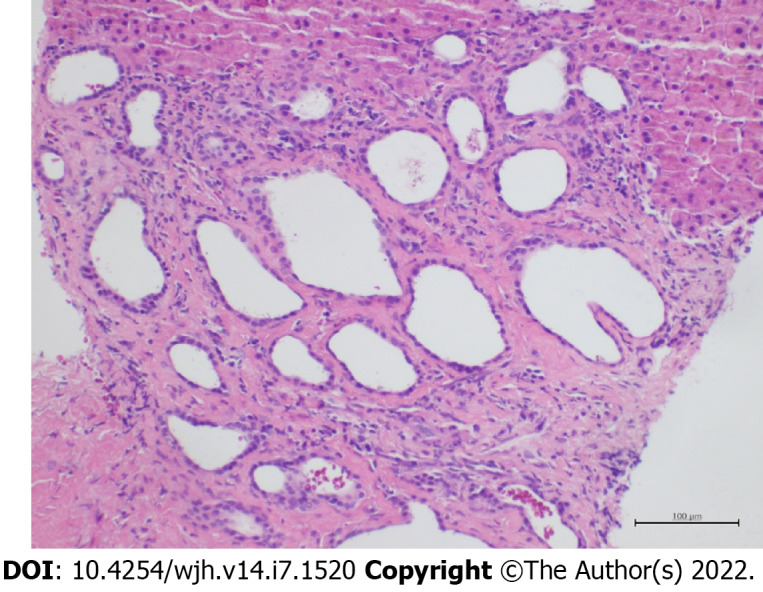
Histopathological examination of the punctured liver biopsy specimen. Microphotograph of histological appearance of liver biopsy specimen showing in the peri-portal region a group of ductal structures embedded in a hyalinized stroma. The ductal structures appear variably dilated and focal microcystic. These ducts are lined with a cubic or flattened biliary epithelium. (hematoxylin-eosin staining, magnification × 20).
Figure 4.
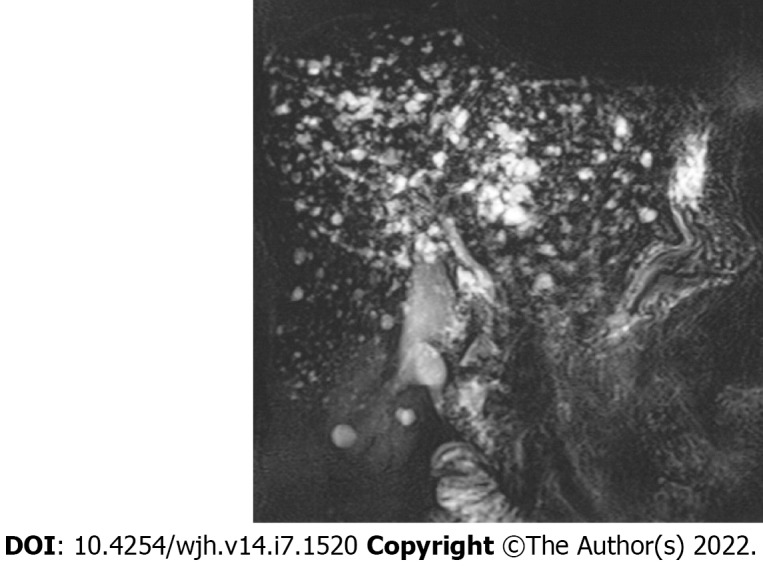
Gadolinium contrast-enhanced magnetic resonance cholangiography. Multiple lesions were hyperintense on coronal thick slab T2 MIP. No communication between hamartomas and biliary ducts; noticeable typical formation of a “starry sky.”
FINAL DIAGNOSIS
VMC (i.e., biliary hamartoma).
TREATMENT
The proposed treatment approach was conservative and included biliary salts (ursodeoxycholic acid 15 mg/kg of body weight), daily, with approved prolongation at each subsequent follow-up visit.
OUTCOME AND FOLLOW-UP
Further clinical, laboratory, and instrumental check-ups performed every 6 mo to date, showed a clinically stable condition with no progression noted on US imaging, as well as normal serum liver tests.
DISCUSSION
Biliary hamartoma or VMC belongs to a heterogeneous group of congenital diseases defined as “fibrocystic liver diseases.” Such diseases are caused by anomalous development of ductal plate during embryogenesis. In addition to VMC, other fibrocystic diseases include congenital liver fibrosis, Caroli’s disease (CD), polycystic liver disease (PCLD), and choledochal cysts[6].
From the embryogenetic point of view, in VMC as well as PCLD, malformation of the ductal plate is involved in little intrahepatic biliary tracts causing loss of continuity with the remaining biliary tree[7]. The consequence of such malformation is the absence of communication between typical cysts of the PCLD or VMC and biliary tree, which is different from some other “fibropolycystic liver diseases,” such as CD. In CD, communication between cystic formations and the biliary tree is preserved since malformation of the ductal plate takes place at another time during embryogenetic development, hence involving other biliary ducts than those in PCLD or VMC.
The diagnosis of PCLD can be made by the identification of more than 20 Liver cysts on imaging modalities such as US, CT, and/or MRI, which do not communicate with the biliary tree. In cases where doubts exist regarding whether there is communication between cystic formation and the biliary tree, and consequently, the differential diagnosis among PCLD, VMC and CD is not possible, liver-specific contrast-enhanced MR cholangiography (functional MRI) will be of use. On such images, in the liver phase, biliary tracts are opacified with the contrast, and consequently, in the absence of communication between biliary tracts and cysts, the latter will not be contrasted, unlike biliary tracts. While in the case of communication between cystic lesions and the intrahepatic biliary tree, the cystic formation is opacified, allowing the diagnosis of CD to be established[5]. In our presented case, MR cholangiography sequences allowed us to exclude CD, as the communication between cystic formation and biliary ducts was not preserved. Contrast-enhanced CT or MRI allowed us to study the vessels as well, allowing identification of the last distinctive feature of VMC and PCLD from CD (i.e., “central dot sign” - tiny dots with strong contrast enhancement of the portal vein in the venous phase within the dilated hepatic bile duct).
In biliary hamartoma as well as PCLD, cystic hepatic lesions that characterize the disease do not communicate with biliary tracts; however in VMC, such findings are usually smaller (up to 1.5 cm), countless, and dimensionally similar with each other compared with typical cystic formations in PCLD[4]. Therefore, in MR cholangiography, in addition to the lack of communication between hamartomas and biliary tracts, the typical formation of VMC is defined as a “starry sky,” as can be seen in Figure 4.
Moreover, in the case of a patient who has liver lesions suspected of VMC or PCLD, it is necessary to obtain a thorough family history, as in approximately 90% of cases, PCLD is associated with autosomal dominant polycystic kidney disease (ADPKD) or autosomal dominant polycystic liver disease (ADPLD), which should be excluded to confirm isolated PCLD due to an inheritance pattern of ADPKD/ADPLD being autosomal-dominant[8,9]. The diagnosis of ADPLD in the setting of liver cysts is based on a family history of polycystic liver with a requisite number of liver cysts for a given age. Notably, liver cysts in ADPLD are often greater in quantity and size than those in ADPKD; hence, studies emphasize the necessity of the differential diagnosis between ADPKD and ADPLD as well[9]. An Italian study group reported a clinical case of a 54-year-old kidney transplant recipient with ADPKD in whom VMC was not previously recognized but visualized on routine ultrasound scan and confirmed with MRI 4 years after renal transplantation[10]. The authors emphasized that the similar pathological pathways of the two conditions as well as immunosuppressive therapy in the patient could lead to increased risk of malignization of the lesions; thus, thorough surveillance of such patients, preferentially by CEUS or MRI over routine US, is recommended[10]. It is worth mentioning that the use of contraceptive steroids or female hormone replacement therapy by postmenopausal women is another independent risk factor for developing PCLD, which should be considered during medical history collection while no similar considerations have been published for VMC[8].
In Table 1, we present the main differential diagnostic criteria of PCLD, CD, and VMC using a PubMed search with terms such as ‘biliary hamartoma,’ ‘Von Meyenburg complex,’ ‘Caroli’s disease,’ and ‘polycystic liver disease.’
Table 1.
Differential diagnosis criteria of polycystic liver disease, Caroli’s disease, and biliary hamartoma
|
|
Polycystic liver disease
|
Caroli’s disease
|
Biliary hamartoma (VMC)
|
| Epidemiology | From 1 to 10 cases per 1000000; M:F = 1:6[13] | From 0.01 to 1 in 1000000[7,14]; M:F = 1:1[14] | In up to 5.6% of autopsies, an estimated 6% of the general population[1]; M:F = 1:1 |
| Symptoms associated with a disease | 20% of patients have dyspnea, early satiety, abdominal distension, malnutrition, gastroesophageal reflux, hepatomegaly, portal hypertension, ascites, and variceal hemorrhage[15] | Rarely portal hypertension or hepatomegaly, fever, hepatolithiasis, and gallbladder stones[16] | Normally absent; In rare cases, fever, jaundice, abdominal pain, and variceal hemorrhage[11] |
| Blood examination findings | Elevated GGT, ALP, AST, and total bilirubin are reported in some serious cases[15]; Possible elevation of CA19-9[17] | Transaminase levels may be slightly elevated; Thrombocytopenia and leukopenia if portal hypertension and/or hypersplenism are present; Leukocytosis and erythrocyte sedimentation rate may indicate cholangitis[16] | Possible elevation of liver enzymes (ALT, AST, ALP) and bilirubin; Rarely increased CA19-9[18] |
| Ultrasound/contrast-enhanced ultrasound | Hyperechoic areas in the subcapsular portion of the liver[11]; More than 20 hepatic cysts[19]; Larger in size compared to VMC[11]; Rarely uniform cysts, varying from < 1 mm to ≥ 12 cm in diameter; Diffuse dilatation of intra- and extrahepatic bile ducts[11] | Intrahepatic cystic anechoic areas in which fibrovascular bundles (composed of portal vein and hepatic arteries, which can be demonstrated by Doppler ultrasonography), stones and linear bridging or septum may be present[16]; Saccular or fusiform cystic dilatations of the intrahepatic bile ducts up to 5 cm in diameter often containing calculi[11] | Hypo- or hyperechoic lesions with comet-tail echoes, dot-sign; Small well-circumscribed lesions scattered throughout the liver with hypoechoic, hyperechoic, or mixed echogenicity depending on solid, cystic, or mixed components, respectively[12,19]; Hamartomas are relatively uniform in size[11] |
| Contrast-enhanced MRI, magnetic resonance cholangiopancreatography | Biliary ducts are not opacified with contrast; Cysts are round and smooth and are deformed but do not communicate with bile ducts[16]; Possible calcification of the walls of hepatic cysts[11] | Multiple small cystic formation is opacified with contrast; Present communication between the sacculi and bile ducts and diverticulum-like sacculi of the intrahepatic biliary tree; Cystic spaces are irregular in shape and communicate with biliary tree; Intrahepatic bile duct ectasia; Central dot sign[11,16] | Hypointense on T1-weighted images and hyperintense on T2-weighted sequences; Signal intensity is similar to the spleen but less intense than that of liver cysts[20]; MRI with gadolinium shows no communication between hamartomas and biliary ducts; Typical formation “starry sky”; Central dot sign[11] |
| Histological/ cytological evaluation | Multiple diffuse cystic lesions resembling solitary cysts, lined by cuboidal to flat biliary epithelium surrounded by fibrous stroma, with straw-colored fluid; 40% have identifiable VMCs[21] | Dilated bile ducts lined by cuboidal or columnar epithelium with fibrotic duct wall[22] | Bile ducts lined by cuboidal or flattened epithelium; Small to medium size[12]: Class 1: Mostly solid lesions with narrowing of biliary ducts; Class 2: Mixed solid/cystic lesions; Class 3: Mostly cystic lesions with ectasia of biliary ductsCytology findings of VMCs and bile duct adenomas are similar[12] |
| Treatment approach | No approved treatment; Optional pharmacological treatments of somatostatin receptor antagonists, mTOR inhibitor, vasopressin-2-receptor antagonists, estrogen receptor antagonists;surgical therapy: percutaneous cyst aspiration and sclerotherapy, laparoscopic cyst fenestration, segmental hepatic resection, and liver transplantation[15] | No specific treatment; Cholangitis must be handled with antibiotics, while cholestasis can be treated with ursodeoxycholic acid[23]; Antibiotics may stabilize the acute cholangitis; Drainage procedures with ERCP or PTC are important and sphincterotomy can aid biliary drainage and stone removal or subsequent passage and may decrease bouts of cholangitis; Lobectomy and liver transplantation[16,23] | VMC is considered a benign lesion that does not need any specific treatment unless complicated; In that case, a symptomatic treatment is prescribed (ursodeoxycholic acid or antibiotics)[12] |
| Complications, progression to cancer risk | Hemorrhage, infection, rupture, portal hypertension, jaundice, and end-stage liver disease[11,24]; Malignization is extremely rare[11] | Portal hypertension, cholangitis, sepsis, choledocholithiasis, hepatic abscess, cholangiocarcinoma and portal hypertension; Cholangiocarcinoma due to chronic inflammation of the biliary tree has been reported in 7%-14% of patients[11,16,23] | Rarely persistent upper right quadrant pain; Rare calcifications, portal hypertension infectious cholangitis[2,3,5]; Lesions do not tend to grow[4]; Less than 3% probability of developing cholangiocarcinoma[1] |
ALP: Alkaline phosphatase; ALT: Alanine transaminase; AST: Aspartate aminotransferase; CA19-9: Carbohydrate antigen 19-9; ERCP: Endoscopic retrograde cholangiopancreatography; F: Female; GGT: Gamma-glutamyl transferase; M: Male; MRI: Magnetic resonance imaging; mTOR: Mammalian target of rapamycin; PTC: Percutaneous transhepatic cholangiography; VMC: Von Meyenburg complex.
By contrast, peribiliary cysts are cystic formations that are small in size (up to 20 mm) and localized along intrahepatic biliary ducts of the large caliber, in peribiliary spaces, with possible involvement of extrahepatic biliary tracts. Peribiliary cysts in the majority of cases are associated with liver cirrhosis, portal hypertension, portal thrombosis, and polycystic disease predominantly of the kidneys[3]. These little cysts do not show communication with corresponding biliary ducts; therefore, functional MR cholangiography is an accurate method to exclude biliary-cyst communication[3,11].
Liver-specific contrast-enhanced functional MR cholangiography is the most sensitive method for the diagnosis of intra- and extrahepatic biliary pathways and liver cystic lesions, allowing evaluation of their connection with the biliary tree[1,3,11].
While most patients with VMC remain asymptomatic, the elevation of inflammatory factors and liver function parameters (i.e., gamma-glutamyl transferase, alkaline phosphatase, aspartate aminotransferase, alanine aminotransferase) in serum could represent the only available biomarkers suggestive of the pathology. The approach to management of patients with VMC varies from regular follow-up, as in cases with asymptomatic course, to active treatment, as in cases of symptomatic or complicated disease course and which might include administration of ursodeoxycholic acid and/or antibiotics[12], as in our presented case.
CONCLUSION
Biliary hamartoma is a predominantly asymptomatic liver formation that is often diagnosed incidentally. Some studies have proven that with time, the function of the affected liver can be altered, although the formation bears a low risk of malignization. Thus, the knowledge of diagnostic features and differential diagnostic criteria are crucial for choosing the correct surveillance method, as currently no available international guidelines exist for standardizing the clinical diagnoses or guiding clinicians in the treatment approach and follow-up for VMC.
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: All authors have no conflicts of interest to declare.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: April 4, 2022
First decision: April 28, 2022
Article in press: June 13, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jugovic D, Germany; Yu A, China S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
Contributor Information
Kateryna Priadko, Department of Precision Medicine and Hepato-Gastroenterology Unit, University Hospital and Università degli Studi della Campania Luigi Vanvitelli, Naples 80138, Italy. kateryna.priadko@unicampania.it.
Marco Niosi, Department of Precision Medicine and Hepato-Gastroenterology Unit, University Hospital and Università degli Studi della Campania Luigi Vanvitelli, Naples 80138, Italy.
Luigi Maria Vitale, Department of Precision Medicine and Hepato-Gastroenterology Unit, University Hospital and Università degli Studi della Campania Luigi Vanvitelli, Naples 80138, Italy.
Chiara De Sio, Internal Medicine Unit, Camilliani Hospital, Casoria 80026, Italy.
Marco Romano, Department of Precision Medicine and Hepato-Gastroenterology Unit, University Hospital and Università degli Studi della Campania Luigi Vanvitelli, Naples 80138, Italy.
Ilario De Sio, Department of Precision Medicine and Hepato-Gastroenterology Unit, University Hospital and Università degli Studi della Campania Luigi Vanvitelli, Naples 80138, Italy.
References
- 1.Kakar S, Borhani AA, Malik SM. A liver full of stars: Hepatostellular! Electronic clinical challenges and images in GI . 2017;153:E8–9. doi: 10.1053/j.gastro.2017.03.058. [DOI] [PubMed] [Google Scholar]
- 2.Sinakos E, Papalavrentios L, Chourmouzi D, Dimopoulou D, Drevelegas A, Akriviadis E. The clinical presentation of Von Meyenburg complexes. Hippokratia . 2011;15:170–173. [PMC free article] [PubMed] [Google Scholar]
- 3.Yoshida S, Kurokohchi K, Ueno T, Yoshino M, Shimada M, Masaki T. Hepatic von Meyenburg complex: a trigger of severe portal hypertension. Liver Int . 2009;29:614–615. doi: 10.1111/j.1478-3231.2008.01903.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monteiro de Barros J, Stell D, Bracey TS, Mavroeidis VK. Diffuse liver hamartomatosis (diffuse von Meyenburg complexes) mimicking hepatic metastases on a background of previous cancer. Ann R Coll Surg Engl . 2020;102:e1–e4. doi: 10.1308/rcsann.2020.0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gil-Bello D, Ballesteros E, Sanfeliu E, Andreu FJ. Calcification in biliary hamartomatosis. Br J Radiol . 2012;85:E99–101. doi: 10.1259/bjr/95019559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horn SR, Stoltzfus KC, Lehrer EJ, Dawson LA, Tchelebi L, Gusani NJ, Sharma NK, Chen H, Trifiletti DM, Zaorsky NG. Epidemiology of liver metastases. Cancer Epidemiol . 2020;67:101760. doi: 10.1016/j.canep.2020.101760. [DOI] [PubMed] [Google Scholar]
- 7.Umar J, Kudaravalli P, John S. Caroli Disease. Treasure Island (FL): StatPearls Publishing; 2021. [cited 20 April 2022]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513307/
- 8.Everson GT. Polycystic liver disease. Gastroenterol Hepatol (N Y) . 2008;4:179–181. [PMC free article] [PubMed] [Google Scholar]
- 9.Patel A, Chapman AB, Mikolajczyk AE. A Practical Approach to Polycystic Liver Disease. Clin Liver Dis (Hoboken) . 2019;14:176–179. doi: 10.1002/cld.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leonardi G, Simeoni M, Bozzo M, Caglioti A, Fuiano G. Diagnosis of Biliary Hamartomatosis in Kidney Transplant Recipient affected by ADPKD. G Ital Nefrol . 2019;36 [PubMed] [Google Scholar]
- 11.Brancatelli G, Federle MP, Vilgrain V, Vullierme MP, Marin D, Lagalla R. Fibropolycystic Liver Disease: CT and MR Imaging Findings. Radiographics . 2005;25:659 – 670. doi: 10.1148/rg.253045114. [DOI] [PubMed] [Google Scholar]
- 12.Joneja U. Von Meyenburg complex. PathologyOutlines.com website 2020. [cited 20 April 2022]. Available from: https://www.pathologyoutlines.com/topic/Livermeyenburgcomplex.html .
- 13.Kothadia JP, Kreitman K, Shah JM. Polycystic Liver Disease. Treasure Island (FL): StatPearls Publishing, 2021. [cited 20 April 2022]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549882/ [PubMed]
- 14.Yonem O, Bayraktar Y. Clinical characteristics of Caroli's disease. World J Gastroenterol . 2007;13:1930–1933.. doi: 10.3748/wjg.v13.i13.1930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang ZY, Wang ZM, Huang Y. Polycystic liver disease: Classification, diagnosis, treatment process, and clinical management. World J Hepatol . 2020;12:72–83. doi: 10.4254/wjh.v12.i3.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yonem O, Bayraktar Y. Clinical characteristics of Caroli's syndrome. World J Gastroenterol . 2007;13:1934–1937. doi: 10.3748/wjg.v13.i13.1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neuville M F, Krzesinski J M, Jouret F. Serum levels of carbohydrate antigen 19-9 do not systematically increase in case of liver cyst infection in patients with autosomal dominant polycystic kidney disease. Clin Kidney J . 2020;13:482–483. doi: 10.1093/ckj/sfz119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jáquez-Quintana JO, Reyes-Cabello EA, Bosques-Padilla FJ. Multiple Biliary Hamartomas, The ‘‘Von Meyenburg Complexes’’. Annals of Hepatology . 2017;16:812–813. doi: 10.5604/01.3001.0010.2822. [DOI] [PubMed] [Google Scholar]
- 19.Vachha B, Sun MRM, Siewert B, Eisenberg RL. Cystic lesions of the liver. Am J Roentgenol . 2011;196:355–366.. doi: 10.2214/AJR.10.5292. [DOI] [PubMed] [Google Scholar]
- 20.Boraschi P, Scalise P, Tarantini G, Colombatto P, Donati F. MR imaging features of multiple biliary hamartomas (Von Meyenburg Complex): A pictorial review and differential diagnosis. J Med Imaging Radiat Oncol . 2021;65:323–330. doi: 10.1111/1754-9485.13173. [DOI] [PubMed] [Google Scholar]
- 21.Arora K. Polycystic liver disease / duct plate malformation. Pathology Outlines.com website 2012. [cited 20 April 2022]. Available from: https://www.pathologyoutlines.com/topic/Liverpolycysticliverdisease.html .
- 22.Arora K. Caroli disease. Pathology Outlines.com website 2012. [cited 20 April 2022]. Available from: https://www.pathologyoutlines.com/topic/Livercarolisdisease.html .
- 23.Acioli ML, Costa LR, de Miranda Henriques MS. Diffuse Caroli's disease with atypical presentation: a case report. Ann Gastroenterol . 2014;27:79–81. [PMC free article] [PubMed] [Google Scholar]
- 24.Cnossen WR, Drenth JP. Polycystic liver disease: an overview of pathogenesis, clinical manifestations and management. Orphanet J Rare Dis . 2014;9:69.. doi: 10.1186/1750-1172-9-69. [DOI] [PMC free article] [PubMed] [Google Scholar]


