Abstract
Study objective
Assess the changes in anxiety, depression, and stress levels over time and identify risk factors among healthcare workers in French emergency departments (EDs) during the first COVID-19 outbreak.
Method
A prospective, multicenter study was conducted in 4 EDs and an emergency medical service (SAMU). During 3 months, participants completed fortnightly questionnaires to assess anxiety, depression, and stress using the Hospital Anxiety and Depression and the Chamoux-Simard scale. The changes in anxiety, depression, and stress levels over time were modelled by a linear mixed model including a period effect and a continuous time effect within periods.
Results
A total of 211 respondents (43.5 %) completed the survey at inclusion. There was a decrease in mean anxiety (from 7.33 to 5.05, p < 0.001), mean depression (from 4.16 to 3.05, p = 0.009), mean stress at work (from 41.2 to 30.2, p = 0.008), and mean stress at home (from 33.0 to 26.0, p = 0.031) at the beginning of each period. The mean anxiety level was higher for administrative staff (+0.53) and lower for paramedics (−0.61, p = 0.047) compared to physicians. The anxiety level increased with the number of day and night shifts (0.13/day, p < 0.001, 0.12/night, p = 0.025) as did stress at work (1.6/day, p < 0.001, 1.1/night, p = 0.007). Reassigned healthcare workers were at higher risk of stress particularly compared to SAMU workers (stress at work: p = 0.015, at home: p = 0.021, in life in general: p = 0.018).
Conclusion
Although anxiety, depression, and stress decreased over time, anxiety was higher among physicians and administrative staff. Reassignment and working hours were identified as potential risk factors for mental health distress in EDs.
Keywords: COVID-19, Healthcare workers, Stress, Emergency department
1. Introduction
1.1. Background
The coronavirus disease 2019 (COVID-19) pandemic was declared on March 11, 2020 by the World Health Organization 1, 2 and France has been one of the most impacted countries in the world [3]. In France, the first outbreak (released from the French health authorities) started at the beginning of March 2020 which led to a national containment from March 17 to May 11, 2020 [4]. Indeed, the numbers of confirmed new cases per day during this period was more common than other periods.
1.2. Importance
During the first outbreak of COVID-19, the French emergency departments (EDs) were on the frontline as they were in charge of patient triage. The role of ED triage was crucial in order to contain and isolate the suspected COVID-19 cases 5, 6, 7. However, the increasing number of patients in EDs translated into overwhelming workload, increased risk of contamination for the staff, and a threat to the mental health of workers. During the severe acute respiratory syndrome (SARS) outbreak, it had been shown that the SARS caused a significant level of distress among ED staff, especially among nurses who felt overwhelmed, and feared for their health due to spread of the virus [8]. In addition, long-term impacts on the mental health of workers, particularly those who had been infected with SARS, had been highlighted 9, 10.
During the COVID-19 pandemic, early preliminary data from China found a depression rate ranging from 12.2 % to 50.3 % and an anxiety rate of 13 to 44.6 % among healthcare workers, especially among nurses and other frontline medical workers [11]. A recent review concerning the mental health of healthcare workers, which included a majority of studies conducted in China reported a prevalence of 23 % for anxiety and 22.8 % for depression [12]. Similar findings were recorded in Italy 13, 14. However, these studies performed only a single measure at a given time without providing follow-up data concerning symptoms of anxiety and depression.
1.3. Goals of this investigation
At the beginning of March, when the number of cases was rapidly increasing in France, we decided to evaluate the consequences of this pandemic on the mental health of healthcare workers in EDs. This study aimed to provide an assessment of the changes in anxiety, depression, and stress levels over time as well as identify risk factors among healthcare workers in French EDs during the first COVID-19 outbreak.
2. Methods
2.1. Study design and setting
This prospective, multicenter study was conducted in 4 French EDs and the emergency medical service (Service d'Aide Médicale Urgente, SAMU) of Lyon, France, The SAMU comprises the Mobile Emergency and Intensive Care Mobile Structures (Structures Mobiles d'Urgence et de Réanimation, SMUR) and the emergency call center. The 4 EDs included 3 university hospitals and 1 general hospital from the Lyon area. The Lyon urban area is the second largest in France and has a population of about 2 million people. The 3 university EDs are urban hospitals which receive >40,000 annual ED visits for two of them and over 80,000 for the third. The ED within the general hospital is suburban and receives about 50,000 annual ED visits. The study was approved by the local ethics committee (N° 20.04.07.74549) and follows the STROBE statement [15]. The study is recorded on ClinicalTrials (Identifier: NCT04383886).
2.2. Participants and time periods studied
Healthcare workers practicing in EDs or in the SAMU (physicians, paramedics, and administrative staff) during the first outbreak and having expressed their non-opposition were included from April 20, 2020, to May 29, 2020. Three different periods representing crucial moments of the first COVID-19 outbreak were released from the French health authorities. The first period, from April 20 to May 10, 2020, is referred to as the critical period as it corresponds to the containment period which was officially applied in France from March 17, to May 11, 2020 [4]. The second period, from May 11, to July 10, 2020 is the post-critical period as it started at the end of containment [4]. The third period, after July 11, 2020, is the normal recovery period as it relates to the official date declaring the end of the state of emergency in France [4].
2.3. Data collection
2.3.1. Inclusion
For each participant, a questionnaire was completed at inclusion. The questionnaire addressed demographic characteristics (age, sex, place of residence, marital status, number of children, history of anxiety, depression, or burn-out disorders, consumption of tobacco, alcohol, coffee, and anxiolytics) use of psychological support, personal organizational characteristics (mode and length of commute, family organization during confinement, temporary accommodation) and professional characteristics (profession, type of hospital, years of professional experience, usual work position and reassignments, managerial responsibility). They also completed specific questionnaires regarding anxiety, depression, and stress. The questionnaire surveys were anonymous and personal information was not disclosed, except for demographic data.
2.3.2. Follow-up
Each participant completed the questionnaires fortnightly to assess anxiety, depression, and stress up to 90 days after inclusion based on self-report. At each measurement time, information concerning the number of work days and/or night shifts worked, COVID-19 infection, and work disability related to infection or that of a loved one over the last 2 weeks was also retrieved. There were 2 follow-ups during the critical period which was the shorter, 4 during the post-critical period and 5 during the normal recovery period which was the longest.
2.3.3. Outcomes
Symptoms of depression, anxiety, and stress for all participants were evaluated using French versions of validated measurement tools.
The Hospital Anxiety and Depression Scale (HADS) is a straightforward tool developed by Zigmond and Snaith for detecting and classifying the severity of anxiety and depression. The HADS consists of two subscales with a total of 14 items, each item scores on a 4 points-scale (0–3). Seven items evaluate depression and another seven assess anxiety. The total score ranges from 0 to 21. A cutoff score of 8 was used on the anxiety or depression subscales as validated in previous study to define the presence of symptoms for anxiety and depression [16]. The HADS has been validated in French [17].
The evaluation of stress is based on the administration of the Chamoux-Simard scale, a questionnaire containing three questions in the form of a Visual Analog Scale (VAS) related to the state of stress at work, at home, and in life in general [18]. This scale have been validated in French cohort [19]. Each response gives an idea of the level of stress felt in each field. This test, inspired by visual pain scales, allows to estimate in a simple way the level of stress by means of a horizontal line of 100 mm, not graduated, on which the level of stress felt is rated from very low to very high. The three questions related to stress are formulated as follows; my state of stress at work is…My state of stress at home is… My state of stress in my life is in general…The subject is considered to be stressed for a VAS score strictly above 60 mm.
2.4. Statistical analysis
Continuous data were described by means (±standard deviation), and categorical ones by frequencies and percentages. The changes in anxiety, depression, and stress levels over time were modelled by a linear mixed model including a period effect and a continuous time effect within periods (and possibly an interaction). Then, the occupation (and possibly an interaction with the period) and the number of work days, night shifts, and 24-hour work shifts were progressively introduced in the model depending on their significance. A random intercept by healthcare worker was added in the model. Once the base model was defined, several other factors were assessed, one at a time: age class, sex, marital status, children, changes in family organization, usual work position, years of professional experience, previous psychiatric history, COVID-19 infection, work disability related to infection or that of a loved one, managerial responsibility. The effect of the factors on anxiety/depression/stress was quantified by slope or difference of means with the associated 95 % Confidence Interval [95 % CI]. No correction for multiple testing was performed. A McNemar test was used to compare between the beginning and the end of the study the consumption of alcohol, anxiolytics, tobacco, and coffee, as well as the use of psychological support. P-values <0.05 were considered significant. The analyses were performed using the SAS 9.3 and R (4.0.2) software (main procedure/package: proc. glimmix/package lme4) [20].
3. Results
In the study, among the 485 healthcare workers asked to participate, 211 (43.5 %) respondents completed the survey at inclusion (HADS: 206 at inclusion, 122 at the last visit; Chamoux-Simard scale: 210 at inclusion, 126 at the last visit). Among all respondents, 158 (74.9 %) were included during the critical period and 53 (25.1 %) during the post-critical period. Out of 210 respondents, 144 (68.6 %) worked in EDs and 116 were paramedics (55.2 %).
During the crisis, 16 (7.6 %) participants had been reassigned to frontline departments. A total of 41 (19.7 %) healthcare workers had managerial responsibilities (Table 1 ). Forty-five (21.4 %) reported having a previous psychiatric history, 24 (11.4 %) had already presented with anxiety, and 18 (8.6 %) with depression symptoms. Only 3 (1.4 %) participants reported using anxiolytics.
Table 1.
Demographic and occupational characteristics of respondents.
| Characteristics | Total (N = 211) |
|---|---|
| Occupation (n = 210) | |
| Physicians | 76 (36.2) |
| Paramedics | 116 (55.2) |
| Administrative staff | 18 (8.6) |
| Age, years (n = 210) | 37.4 ± 9.6 |
| Women | 150 (71.1) |
| Marital status (n = 210) | |
| Married or in a relationship | 159 (75.7) |
| Single | 51 (24.3) |
| Dependent child (n = 210) | 110 (52.4) |
| Number of children (n = 110) | 2.1 ± 1.0 |
| Commute mode (n = 210) | |
| Car | 152 (72.4) |
| Public transportation | 17 (8.1) |
| Active modes of transport (bicycle, scooter, walking) | 41 (19.5) |
| Temporary accommodation (n = 209) | 6 (2.9) |
| Years of professional experience (n = 209) | 11.1 ± 9.0 |
| Usual work position (n = 210) | |
| Emergency department | 144 (68.6) |
| Emergency medical service | 32 (15.2) |
| Both emergency department and emergency medical service | 18 (8.6) |
| Other unit (reassignment) | 16 (7.6) |
| Work rate (%) (n = 208) | 95.8 ± 11.3 |
| Managerial responsibility (n = 208) | 41 (19.7) |
Data are expressed as N (%), or mean ± SD.
Abbreviations: SD (standard deviation).
3.1. Change in anxiety and depression over time
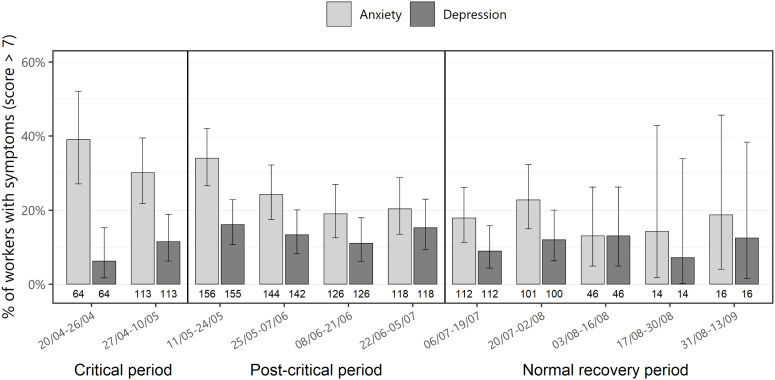
At the beginning of the critical period, 25 (39.1 %) and 4 (6.3 %) healthcare workers had symptoms of anxiety and depression, respectively (Fig. 1 ). According to the models (base models defined in Appendix A), there was a significant decrease in the mean anxiety level (from 7.33 to 5.05, p < 0.001) and mean depression level (from 4.16 to 3.05, p = 0.009) when comparing the beginning of each time period (Table 2 ). Overall, when compared to physicians, the mean anxiety level was higher for administrative staff (+0.53) and lower for paramedics (−0.61, p = 0.047). The changes in anxiety and depression levels over time however, were not significantly different according to the different occupations (p = 0.060 for anxiety, and 0.092 for depression; Supplemental material Fig. S1).
Fig. 1.
Proportion of healthcare workers with anxiety and depression symptoms during the three periods studied (error-bar: 95 % confidence intervals).
Table 2.
Mean levels of anxiety, depression, and stress predicted by the models at the beginning of the three periods.
| Scale | HADS anxiety [95 % CI] | HADS depression [95 % CI] | Stress at work [95 % CI] | Stress at home [95 % CI] | Stress in life in general [95 % CI] |
|---|---|---|---|---|---|
| Period | |||||
| Critical period | 7.33 [6.38; 8.27] | 4.16 [3.62; 4.57] | 41.2 [35.7; 46.7] | 33.0 [26.2; 36.9] | 34.3 [30.5;38.1] |
| Post-critical period | 6.48 [5.73; 7.23] | 3.90 [3.43; 4.37] | 36.5 [33.0; 39.5] | 28.2 [24.8; 31.6] | 31.2 [28.2; 40.0] |
| Recovery period | 5.05 [4.20; 5.91] | 3.05 [2.50; 3.59] | 30.2 [25.6; 24.7] | 26.0 [22.1; 29.9] | 28.5 [24.6; 32.2] |
| F-value | 11.34 | 4.73 | 4.89 | 3.48 | 2.30 |
| p < 0.001 | p = 0.009 | p = 0.008 | p = 0.031 | p = 0.109 | |
The level of anxiety significantly increased with the number of work days (p < 0.001), night shifts (p = 0.025), and the occurrence of 24-hour work shifts during the last 15 days (p = 0.022) (Table 3 ). A threshold of 7 days of work over 2 weeks was found to significantly increase the level of anxiety (+0.49, 95 % CI [0.08; 0.89], p = 0.018).
Table 3.
Association between the number of work days, night shifts, and the occurrence of 24-h work shifts and levels of anxiety, depression, and stress.
| Scale | HADS anxiety [95 % CI] | HADS depression [95 % CI] | Stress at work [95 % CI] | Stress at home [95 % CI] | Stress in life in general [95 % CI] |
|---|---|---|---|---|---|
| During the last 15 days | |||||
| Mean scale increase by work day | 0.13 [0.07; 0.19] p < 0.001 | 0.06 [0.01; 0.02] p = 0.032 | 1.6 [1.1; 2.0] p < 0.001 | [0.6; 1.6] p < 0.001 | 0.9 [0.4; 1.3] p = 0.002 |
| Mean scale increase by night shift | 0.12 [0.02; 0.22] p = 0.025 | – | 1.1 [0.3; 1.9] p = 0.007 | 0.9 [0.1; 1.7] p = 0.025 | [0.4; 1.9] p = 0.003 |
| Increase with the occurrence of at least one 24-hour work shift | 0.30 [0.04; 0.56] p = 0.022 | – | – | – | – |
“−” means that the factor was not included in the model kept.
3.2. Factors associated with anxiety and depression
There was a significant difference in depressive symptoms according to age groups (p = 0.033), mean depression being higher in the 47–63 years age group compared to the 21–30 years (p = 0.033). Mean depression was also higher in men compared to women (p = 0.032). A previous psychiatric history increased the risk of anxiety and depression (p < 0.001) while having children decreased the risk of anxiety (p = 0.048, Table 4 ).
Table 4.
Factors associated with anxiety and depression.
| Variable | Anxiety | Depression |
|---|---|---|
| Age, years | P = 0.129 | P = 0.033 |
| 31–37/21–30 | 0.41 [−0.43, 1.24] | −0.31 [−1.1, 0.48] |
| 38–46/21–30 | 0.07 [−0.75, 0.89] | −0.01 [−0.79, 0.76] |
| 47–63/21–30 | 0.95 [0.08, 1.83] | 0.88 [0.06, 1.71] |
| Sex | P = 0.467 | P = 0.032 |
| Men/Women | −0.25 [−0.91, 0.42] | 0.67 [0.06, 1.28] |
| Marital status | P = 0.579 | P = 0.196 |
| Married or in a relationship/Single | −0.22 [−0.93, 0.49] | −0.45 [−1.12, 0.23] |
| Children | P = 0.048 | P = 0.064 |
| (Yes/No) | −0.6 [−1.19, −0.01] | −0.54 [−1.1, 0.03] |
| Changes in family organization | P = 0.853 | P = 0.893 |
| (Yes/No) | 0.06 [−0.55, 0.67] | 0.04 [−0.54, 0.62] |
| Usual work position | P = 0.793 | P = 0.296 |
| Emergency medical service (SAMU)/reassignment | −0.27 [−1.65, 1.11] | 0.2 [−1.08, 1.49] |
| Emergency department (ED)/reassignment | 0.04 [−1.09, 1.17] | −0.15 [−1.23, 0.93] |
| Both ED and SAMU/reassignment | 0.42 [−1.1, 1.95] | 0.77 [−0.61, 2.16] |
| Professional experience, years | P = 0.072 | P = 0.760 |
| 3–5/0–2 | 1.24 [0.31, 2.17] | 0.26 [−0.63, 1.15] |
| 6–10/0–2 | 0.26 [−0.57, 1.1] | −0.02 [−0.81, 0.77] |
| ≥10/0–2 | 0.37 [−0.4, 1.13] | 0.33 [−0.4, 1.06] |
| Previous psychiatric history | P < 0.001 | P < 0.001 |
| (Yes/No) | 2.32 [1.65, 3] | 1.94 [1.29, 2.59] |
| COVID-19 infection | P = 0.138 | P = 0.155 |
| (Yes/No) | 0.84 [−0.27, 1.95] | 0.77 [−0.29, 1.83] |
| Work disability related to infection or that of a loved one | P = 0.099 | P = 0.673 |
| (Yes/No) | 0.71 [−0.13, 1.56] | 0.18 [−0.64, 0.99] |
| Managerial responsibility | P = 0.988 | P = 0.801 |
| (Yes/No) | 0.01 [−0.78, 0.79] | −0.09 [−0.81, 0.63] |
p<0.05.
3.3. Change over time concerning stress at work, at home, and in life in general
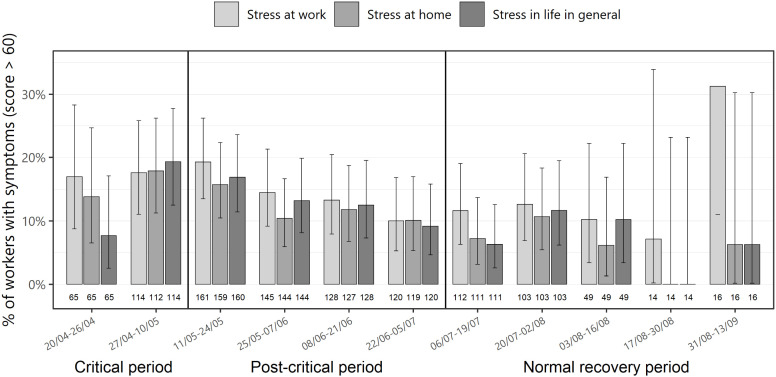
The percentage of healthcare workers with symptoms of stress at work was highest (19.3 %) at the beginning of the post-critical period. The maximum percentages of healthcare workers with symptoms of stress at home and in life in general were 17.9 % and 19.3 %, respectively, during the critical period (Fig. 2 ).
Fig. 2.
Proportion of healthcare workers with stress symptoms at work, at home, and in life in general during the three periods studied (error-bar: 95 % confidence intervals).
According to the models (Table 2), there was a significant decrease in the mean stress at work (from 41.2 to 30.2, p = 0.008) and in the mean stress at home (from 33.0 to 26.0, p = 0.031) at the beginning of each period, but there was no significant difference in the mean level of stress in life in general (from 34.3 to 28.5 p = 0.109). The median levels of stress (for the 3 fields of stress studied) remained under the 60-mm cut-off, whatever the occupation.
The changes in stress levels over time was not significantly different according to the different occupations (p = 0.676 for stress at work, p = 0.598 for stress at home, and p = 0.435 for stress in life in general), but there was a trend toward constant mean stress levels in physicians and a decrease in stress levels for paramedics, whatever the field of stress studied (Supplemental Material Fig. S2).
The levels of stress at work, at home, and in life in general increased significantly with the number of work days and night shifts (Table 3). A threshold of 7 days of work over 2 weeks was found to significantly increase the level of stress at work (+5.0, 95 % CI [1.5; 8.6], p = 0.005) and the level of stress at home (+4.0, 95 % CI [0.5; 7.5]; p = 0.026).
3.4. Factors associated with stress at work, at home, and in life in general
Stress at home and in life in general was significantly different according to age groups (p = 0.004 and 0.019, respectively), mean stress being higher in both the 31–37 years and 47–63 years age groups compared to the 21–30 years group. The usual work position significantly impacted the 3 fields of stress, particularly for SAMU workers who had a decreased risk of stress compared with workers who were reassigned (stress at work: p = 0.015, stress at home: p = 0.021, stress in life in general: 0.018). Stress at work and at home were significantly different according to professional experience (p = 0.034 and 0.024 respectively), mean stress being higher in the 3–5 years group compared to the 0–2 years group. A work disability related to infection or that of a loved one significantly increased stress at home and in life in general (p = 0.027 and p = 0.004, respectively). Managerial responsibility was found to increase the risk of stress in life in general (p = 0.017; Table 5 ).
Table 5.
Factors associated with stress at work, at home, and in life in general.
| Variable | Stress at work | Stress at home | Stress in life in general |
|---|---|---|---|
| Age, years | P = 0.154 | P = 0.004 | P = 0.019 |
| 31–37/21–30 | 6.5 [0.9, 12.1] | 9.6 [4.0, 15.2] | 8.9 [3.3, 14.5] |
| 38–46/21–30 | 2.4 [−3.1, 7.9] | 6.4 [0.9, 11.9] | 4.7 [−0.8, 10.2] |
| 47–63/21–30 | 3.4 [−2.5, 9.2] | 8.6 [2.8, 14.4] | 6.0 [0.2, 11.8] |
| Sex | P = 0.378 | P = 0.273 | P = 0.781 |
| Men/Women | −2.0 [−6.3, 2.4] | 2.4 [−1.9, 6.8] | 0.6 [−3.7, 5.0] |
| Marital status | P = 0.976 | P = 0.336 | P = 0.930 |
| Married or in a relationship/Single | 0.1 [−4.7, 4.8] | 2.4 [−2.4, 7.1] | 0.2 [−4.5, 5.0] |
| Children | P = 0.365 | P = 0.091 | P = 0.792 |
| Yes/No | −1.9 [−5.8, 2.2] | 3.5 [−0.6, 7.5] | 0.5 [−3.5, 4.6] |
| Changes in family organization | P = 0.307 | P = 0.229 | P = 0.989 |
| Yes/No | −2.1 [−6.2, 2.0] | 2.5 [−1.6, 6.6] | 0.0 [−4.1, 4.1] |
| Usual work position | P = 0.015 | P = 0.021 | P = 0.018 |
| Emergency medical service (SAMU)/reassignment | −12.3 [−21.3, −3.3] | −14.1 [−23.1, −5.0] | −14.5 [−23.6, −5.5] |
| Emergency department (ED)/reassignment | −3.6 [−11.2, 4.0] | −7.3 [−14.9, 0.3] | −8.0 [−15.6, −0.4] |
| Both ED and SAMU/reassignment | −2.1 [−11.7, 7.6] | −6.7 [−16.4, 3.1] | −8.5 [−18.3, 1.3] |
| Professional experience, years | P = 0.034 | P = 0.024 | P = 0.161 |
| 3–5/0–2 | 8.8 [2.5, 15.0] | 7.8 [1.5, 14.1] | 7.1 [0.8, 13.4] |
| 6–10/0–2 | 5.6 [0.1, 11.0] | 5.6 [0.00, 11.1] | 2.4 [−3.2, 8.0] |
| ≥10/0–2 | 2.8 [−2.4, 7.9] | 7.0 [1.8, 12.2] | 3.6 [−1.6, 8.8] |
| Previous psychiatric history | P < 0.001 | P < 0.001 | P ≤0.001 |
| Yes/No | 8.8 [4.1, 13.5] | 10.02 [5.4, 14.7] | 11.3 [6.7, 16.0] |
| COVID-19 infection | P = 0.616 | P = 0.589 | P = 0.300 |
| Yes/No | 1.9 [−5.6, 9.5] | 2.1 [−5.5, 9.7] | 4.0 [−3.5, 11.5] |
| Work disability related to infection or that of a loved one | P = 0.095 | P = 0.027 | P = 0.004 |
| Yes/No | 4.9 [−0.84, 10.64] | 6.5 [0.6, 12.2] | 8.5 [2.8, 14.3] |
| Managerial responsibility | P = 0.083 | P = 0.060 | P = 0.017 |
| Yes/No | 4.5 [−0.6, 9.7] | 4.9 [−0.23, 10.0] | 6.3 [1.2, 11.4] |
p<0.05.
3.5. Consumption of tobacco, alcohol, coffee, and anxiolytics
There was no significant difference between inclusion and the end of follow-up in the consumption of alcohol (n = 71, 54.2 % vs n = 73, 55.7 %, respectively, chi-square = 0.05, p = 0.823), anxiolytics (n = 3,1.4 % vs n = 4, 3.1 %, chi-square = 0, p = 1.000), coffee (n = 96, 73.3 % vs n = 94, 71.8 %, chi-square = 0.08, p = 0.773), and tobacco (n = 33, 25.2 % vs n = 34, 26.0 %, chi-square = 0, p = 1.000). In contrast, there was a significant increase in the use of psychological support between inclusion and the end of follow-up (n = 2, 1.5 % vs n = 9, 6.9 %, respectively, p = 0.023).
4. Discussion
The present study found that the healthcare workers in EDs experienced symptoms of anxiety, depression, and stress, especially during the critical period of the pandemic, the levels of which decreased over time except for physicians for whom symptoms seemed to remain constant. The levels of anxiety were higher for administrative staff and physicians compared to paramedics over all the periods. Anxiety, depression, and stress symptoms were found to increase with working time. The present findings also suggest that there are at-risk profiles for healthcare workers in EDs concerning anxiety, depression, and stress symptoms. Depression was more frequent among older men with previous psychiatric history, whereas having children protected against anxiety symptoms. Healthcare workers who were reassigned and older were more exposed to stress, similarly to those with a work disability related to infection or that of a loved one.
Few studies have evaluated the changes over time of anxiety, depression, and stress symptoms experienced by healthcare workers during the COVID-19 pandemic. The majority of studies made a single measure of symptoms among healthcare workers [21]. In the present study, a cohort was followed over time in order to reflect the impact of the first COVID-19 outbreak, which was an unprecedented situation. The findings show that the symptoms of anxiety, depression, and stress (except for stress in life in general) were highest during the critical period which corresponds herein to the beginning of the COVID-19 pandemic in France. One longitudinal study found that anxiety and depression scores were significantly higher during the outbreak period when compared to a similar group assessed after the outbreak period [22]. Another study suggested that anxiety peaked at the start of the outbreak and decreased over time [23]. The fact that the levels of stress in life in general remained high could be explained by the fact that the state of emergency in France was applied until the end of the normal recovery period and disrupted life in general.
Herein, healthcare workers appeared to be differentially affected according to their occupation. More specifically, anxiety was lower in paramedics than among the administrative staff and physicians. This result differs from other studies which found that nurses were particularly at risk of more severe depression and anxiety than doctors 11, 24, 25. Moreover, one study found that medical healthcare workers (doctors and nurses) in direct contact with COVID-19 patients had almost twice the risk of anxiety and depression than non-medical staff at low risk of COVID-19 contact [26]. However, one study also found that the prevalence of anxiety was significantly higher among non-medical healthcare workers compared to medical workers [27]. One possible explanation for these conflicting results is that the present study focused on healthcare workers who by definition are in frontline position. Indeed, the administrative staff dealt with the administrative formalities of the patients in EDs and were in contact with COVID-19 patients. Even if the time of contact with patients was short, they were probably affected by the fear of contamination, and probably less informed about the COVID-19 disease as it has been previously suggested in another study [25]. Similarly, even without considering the context of the pandemic, contact with patients is usually increased for ED doctors due to high patient flow and overcrowding. Moreover, during the pandemic, doctors were more involved than nurses in the constant reorganization of the care pathway required for the management of COVID-19 patients. This may explain the higher rates of stress, anxiety, and depression among doctors and the fact that these symptoms remained high over time.
The present findings also suggest that working time is a crucial risk factor for stress and anxiety. The levels of anxiety and stress at work and at home increased with the number of work days and night shifts, and a significant threshold of 7 days of work over 2 weeks was found to significantly increase anxiety and stress levels. This had been previously demonstrated in the case of nurses [28] and can be explained by the fact that, during this period, healthcare workers were mobilized to assume additional hours of work.
The present study also highlighted that certain healthcare workers might be more vulnerable than others. More specifically, healthcare workers who were reassigned from a workplace other than ED or SAMU were more at risk of stress, suggesting that these professionals were less prepared to face such a crisis. This is supported by another study which found that healthcare workers without experience in a public health emergency were more exposed to adverse mental health outcomes, had lower rates of resilience, and less social support [24]. Moreover, those who worked in the SAMU were the less affected in terms of stress. This could be due to the fact that these professionals are trained to respond to unpredictable and potentially traumatic situations and possibly because their position did not entail managing the overcrowded EDs.
The finding that the older healthcare workers were more exposed to depression and stress, with a higher impact on stress at home and in life general, is consistent with a study which found that the focus of stress was different according to the age group. The older workers were more worried about their own safety whereas younger workers were more anxious about infecting their families [29]. A work disability related to infection or that of a loved one was also found herein to increase stress. Cai et al. also underlined that the safety of family was the most important factor for reducing stress [29].
These findings provide opportunities to improve the mental health management of healthcare workers in the context of a pandemic, particularly regarding the preparation required for reassigning professionals. In EDs, healthcare workers already have experience in traumatic situations, especially those working in the SAMU. The latter could train the professionals who are likely to be reassigned in order to better prepare for future sanitary crises. A second area for improvement concerns the management and organization of human resources and workload, as the need for resting periods appears fundamental during a crisis.
4.1. Limitation
Nevertheless, this study has several limitations. First, the study was conducted only during the first outbreak and over a limited time period. Since then, there have been two other waves of COVID-19 cases in France, which could lead to exhaustion and burn out for healthcare workers. The study of the long-term consequences is underway. Second, some professionals did not complete the study and were perhaps the most distressed. Thus, the levels of stress, anxiety, and depression might have been underestimated. Finally, no adjustment of the multiple tests was performed, and due to the limited sample size, it was not possible to analyze associations between factors and the different scales in fully adjusted models, so the conclusions on risk factors remain exploratory.
5. Conclusion
During the first COVID-19 outbreak, the levels of anxiety, depression, and stress decreased over time among all healthcare workers. The levels of anxiety, however, remained higher for physicians and administrative staff than for paramedics. Workers who were reassigned were particularly at risk of stress and the number of work hours was found to increase anxiety, depression, and stress levels. These findings should be taken into account for the management of healthcare workers during this ongoing pandemic as well as for the prevention against mental health disorders in EDs in general.
Ethics approval and consent to participate
The study was approved by the ethics committee Comité de Protection des Personnes Ile-de-France III (CPP, N° 20.04.07.74549). The study is recorded on ClinicalTrials (Identifier: NCT04383886).
Consent for publication
The participants were informed via a written information and gave their consent.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
The study was supported by the Hospices Civils de Lyon for data management and analysis.
CRediT authorship contribution statement
MD, AT, JB, JH, conceived the study and designed the trial. MD and AT supervised the conduct of the trial and data collection. AT, MD, JB undertook recruitment of participating centers and patients and managed the data, including quality control. FS provided statistical advice on study design and analyzed the data. MD drafted the manuscript, and all authors contributed substantially to its revision. MD takes responsibility for the paper as a whole.
Acknowledgement
-
-
We thank Véréna Landel (Direction de la recherche en santé, Hospices Civils de Lyon) for help in manuscript preparation.
-
-
The authors acknowledge the support of the HCL Covid Task Force.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.08.028.
Appendix A. Definition of the base models for the different scales
All models include a random intercept by worker.
Model for the Chamoux-Simard stress at work scale
Fixed effects: period effect, time effect, interaction between period and time, number of work days, number of night shifts.
Model for the Chamoux-Simard stress at home scale
Fixed effects: period effect, time effect, number of work days, number of night shifts.
Model for the Chamoux-Simard stress in general scale
Fixed effects: period effect, time effect, number of work days, number of night shifts.
Model for the HADS anxiety scale
Fixed effects: period effect, time effect, interaction between period and time, occupation, number of work days, number of night shifts, number of 24-hour work shifts.
Model for the HADS depression scale
Fixed effects: period effect, time effect, number of work days.
Appendix B. Supplementary data
Supplementary figures
References
- 1.WHO WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-mediabriefing-on-covid-19---11-march-2020
- 2.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet Lond. Engl. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. 15 févr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO WHO coronavirus disease 2019 (COVID-19) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- 4.The actions of the French Government during the COVID-19 pandemic. https://www.gouvernement.fr/info-coronavirus/les-actions-du-gouvernement
- 5.Singer A.J., Morley E.J., Meyers K., Fernandes R., Rowe A.L., Viccellio P., et al. Cohort of four thousand four hundred four persons under investigation for COVID-19 in a New York hospital and predictors of ICU care and ventilation. Ann. Emerg. Med. 2020;76(4):394–404. doi: 10.1016/j.annemergmed.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wee L.E., Fua T.P., Chua Y.Y., Ho A.F.W., Sim X.Y.J., Conceicao E.P., et al. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad. Emerg. Med. 2020;27(5):379–387. doi: 10.1111/acem.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O’Reilly G.M., Mitchell R.D., Wu J., Rajiv P., Bannon-Murphy H., Amos T., et al. Epidemiology and clinical features of emergency department patients with suspected COVID -19: results from the first month of the COVID-19 Emergency Department Quality Improvement Project (COVED -2) Emerg. Med. Australas. Oct 2020;32(5):814–822. doi: 10.1111/1742-6723.13573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong T.W., Yau J.K.Y., Chan C.L.W., Kwong R.S.Y., Ho S.M.Y., Lau C.C., et al. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005;12(1):13–18. doi: 10.1097/00063110-200502000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Lancee W.J., Maunder R.G., Goldbloom D.S., Coauthors for the Impact of SARS Study Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008;59(1):91–95. doi: 10.1176/ps.2008.59.1.91. Wash DC. janv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee A.M., Wong J.G.W.S., McAlonan G.M., Cheung V., Cheung C., Sham P.C., et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry Rev. Can. Psychiatr. 2007;52(4):233–240. doi: 10.1177/070674370705200405. avr. [DOI] [PubMed] [Google Scholar]
- 11.Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3(3) doi: 10.1001/jamanetworkopen.2020.3976. 2 mars. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immunol. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. août. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rossi R., Socci V., Pacitti F., Mensi S., Di Marco A., Siracusano A., et al. Mental health outcomes among healthcare workers and the general population during the COVID-19 in Italy. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.608986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rossi R., Socci V., Pacitti F., Di Lorenzo G., Di Marco A., Siracusano A., et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw. Open. 2020;3(5) doi: 10.1001/jamanetworkopen.2020.10185. 15 févr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P., et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet Lond. Engl. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. 20 oct. [DOI] [PubMed] [Google Scholar]
- 16.Zigmond A.S., Snaith R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. juin. [DOI] [PubMed] [Google Scholar]
- 17.Lepine J.P., Godchau M., Brun P. Anxiety and depression in inpatients. Lancet Lond. Engl. 1985;2(8469-70):1425–1426. doi: 10.1016/s0140-6736(85)92589-9. 21 déc. [DOI] [PubMed] [Google Scholar]
- 18.Lesage F.X., Berjot S. Validity of occupational stress assessment using a visual analogue scale. Occup. Med. Oxf. Engl. 2011;61(6):434–436. doi: 10.1093/occmed/kqr037. sept. [DOI] [PubMed] [Google Scholar]
- 19.Lesage F.X., Berjot S., Deschamps F. Clinical stress assessment using a visual analogue scale. Occup. Med. Oxf. Engl. 2012;62(8):600–605. doi: 10.1093/occmed/kqs140. déc. [DOI] [PubMed] [Google Scholar]
- 20.Bates D., Mächler M., Bolker B., Walker S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015;67(1) [cité 24 mai 2022] Disponible sur: http://www.jstatsoft.org/v67/i01/ [Google Scholar]
- 21.De Kock J.H., Latham H.A., Leslie S.J., Grindle M., Munoz S.A., Ellis L., et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. doi: 10.1186/s12889-020-10070-3. 9 janv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu J., Xu Q.H., Wang C.M., Wang J. Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112955. juin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sun N., Wei L., Shi S., Jiao D., Song R., Ma L., et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am. J. Infect. Control. 2020;48(6):592–598. doi: 10.1016/j.ajic.2020.03.018. juin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cai W., Lian B., Song X., Hou T., Deng G., Li H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102111. juin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao J., Wei J., Zhu H., Duan Y., Geng W., Hong X., et al. A study of basic needs and psychological wellbeing of medical workers in the fever clinic of a tertiary general hospital in Beijing during the COVID-19 outbreak. Psychother. Psychosom. 2020;89(4):252–254. doi: 10.1159/000507453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. juin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L., et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020;173(4):317–320. doi: 10.7326/M20-1083. 18 août. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mo Y., Deng L., Zhang L., Lang Q., Liao C., Wang N., et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020;28(5):1002–1009. doi: 10.1111/jonm.13014. juill. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cai H., Tu B., Ma J., Chen L., Fu L., Jiang Y., et al. Psychological impact and coping strategies of frontline medical staff in hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. 2020;26 doi: 10.12659/MSM.924171. 15 avr. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.