Abstract
Background
Respiratory syncytial virus (RSV) is the leading cause of hospitalizations in United States infants aged <1 year, but research has focused on select populations.
Methods
National (Nationwide) Inpatient Sample and National Emergency Department (ED) Sample data (2011–2019) were used to report RSV hospitalization (RSVH), bronchiolitis hospitalization (BH), and ED visit counts, percentage of total hospitalizations/visits, and rates per 1000 live births along with inpatient mortality, mechanical ventilation (MV), and total charges (2020 US dollars).
Results
Average annual RSVH and RSV ED visits were 56 927 (range, 43 845–66 155) and 131 999 (range, 89 809–177 680), respectively. RSVH rates remained constant over time (P = .5), whereas ED visit rates increased (P = .004). From 2011 through 2019, Medicaid infants had the highest average rates (RSVH: 22.3 [95% confidence interval {CI}, 21.5–23.1] per 1000; ED visits: 55.9 [95% CI, 52.4–59.4] per 1000) compared to infants with private or other/unknown insurance (RSVH: P < .0001; ED visits: P < .0001). From 2011 through 2019, for all races and ethnicities, Medicaid infants had higher average RSVH rates (up to 7 times) compared to infants with private or other/unknown insurance. RSVH mortality remained constant over time (P = .8), whereas MV use (2019: 13% of RSVH, P < .0001) and mean charge during hospitalization (2019: $21 513, P < .0001) increased. Bronchiolitis patterns were similar.
Conclusions
This study highlights the importance of ensuring access to RSV preventive measures for all infants.
Keywords: birth month, bronchiolitis hospitalizations, emergency department, infants, Medicaid, respiratory syncytial virus, RSV, RSV hospitalizations
In the United States (US), respiratory syncytial virus (RSV) is the leading cause of hospitalizations among infants aged <1 year [1–4]. Compared with non-RSV-hospitalized infants, increased healthcare utilization (HCU) was observed among RSV-hospitalized infants, with increased use of mechanical ventilation (MV) [5]. However, RSV immunization strategies are limited with palivizumab as the only available immunoprophylaxis. Palivizumab is recommended for select populations, that is, premature infants born ≤28 weeks’ gestational age (wGA), or those with chronic lung disease of prematurity (CLD) or hemodynamically significant congenital heart disease (hs-CHD) [6]. Because palivizumab is the only available option, it is not surprising that the literature is focused on populations who are currently or formerly eligible to receive palivizumab (eg, infants born 29–34 wGA) [7]. For the broader groups of infants including late preterm to full term and those without comorbid conditions, RSV epidemiology data are limited, and there are no immunization options available [7].
Currently, several RSV passive and active immunization strategies are in development [8], including maternal vaccines and long-acting monoclonal antibodies, and offer potential hope to lessen the impacts of RSV [9–11]. As new RSV immunization products may soon become available, it is important to describe RSV epidemiology and associated HCU for all infants and across all healthcare settings to contextualize their potential benefits.
Data from the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project (HCUP) [12–15], which include the Kids’ Inpatient Database (KID), the National (Nationwide) Inpatient Sample (NIS), and the Nationwide Emergency Department Sample (NEDS) databases, provide an opportunity to evaluate RSV disease trends in US infants for inpatient and emergency department (ED) settings. Estimating both RSV rates and burden allow policy makers to not only identify those infants most at risk, but also those populations that drive HCU during the RSV season (historically in the winter and early spring months). Hence, we conducted a retrospective study using these datasets to describe both infant burden and rates for RSV hospitalization (RSVH), bronchiolitis hospitalization (BH), and ED visits in addition to inpatient mortality and HCU.
METHODS
Study Design and Data Sources
KID, NIS, and NEDS provide nationally representative data on >7 million pediatric hospitalizations, 35 million hospitalizations, and 145 million ED visits in the US (all sample-weighted numbers) and also include a comprehensive set of sociodemographic variables such as chronological age, insurance payer status, and race/ethnicity [2–4, 16]. NIS and NEDS 2011–2019 data were the primary datasets in this study; 2019 was the most recent data release. KID data are available every 3 years; 2009, 2012, 2016, and 2019 data were used to confirm NIS results.
The US infant births from 2011 through 2019 were obtained from the birth cohort data of the National Center for Health Statistics and National Vital Statistics System [17]. Live births were used as the denominator of hospitalization and ED visit rates.
This study followed HCUP’s data use agreement procedures to safeguard the confidentiality of patients, physicians, and healthcare institutions in the US. Sample sizes ≤10 were not reported. All data were de-identified and thus exempt from federal regulations for the protection of human research participants.
Study Population
The unit of analysis was infant (<1 year) hospitalizations or ED visits. RSV was defined by at least 1 of the following diagnostic codes: RSV (International Classification of Diseases [ICD], Ninth Revision [ICD-9]: 079.6; ICD, Tenth Revision [ICD-10]: B97.4); pneumonia due to RSV (ICD-9: 480.1; ICD-10: J12.1); acute bronchiolitis due to RSV (ICD-9: 466.11; ICD-10: J21.0); and acute bronchitis due to RSV (ICD-10: J20.5). Bronchiolitis was considered to be an upper estimate of RSV because laboratory testing of RSV is not broadly recommended [18] and included all RSV codes as well as unspecified bronchiolitis (ICD-9: 079.6, 466.11, 466.19, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0, J21.8, J21.9).
All newborn birth hospitalizations, the most common reason for inpatient hospital stays among infants [19], were excluded by ICD-9 (V30.XX–V39.XX) and ICD-10 codes (Z38.XX), to describe community-acquired RSV and bronchiolitis in infants [16].
Statistical Analysis
Expressed as weighted numbers and proportions (%) of hospitalizations or ED visits, burden described the absolute representation of each subgroup among all RSVH, BH, RSV ED visits, or bronchiolitis ED visits to identify the subgroups carrying the greatest weight of morbidity due to disease. In contrast, rates were expressed per 1000 live births and described the risk of hospitalization or ED visit for each subgroup to identify the subgroups bearing the greatest risk of morbidity due to disease.
Diagnosis Year
Estimated average annual weighted numbers of infant RSVH, BH, RSV ED visits, and bronchiolitis ED visits were reported using ICD codes in any diagnostic position from 2011 through 2019. Estimated annual RSVH, BH, and RSV/bronchiolitis ED visit rates per 1000 live births and corresponding 95% confidence intervals (CIs) were also provided. For each year (from 2011 through 2019), the percentage of total infant hospitalizations, percentage of total infant ED visits, and RSVH, BH, and RSV/bronchiolitis ED visit rates per 1000 live births were also presented.
Race/Ethnicity and Insurance Payer
The available race/ethnicity groupings in NIS and KID included non-Hispanic white, non-Hispanic black, Hispanic, American Indian/Alaska Native (AI/AN), and Asian and Pacific Islander. For 2011–2019, the percentage of total infant RSVH or BH and hospitalization rates per 1000 live births were reported by each race/ethnicity. NEDS did not have race/ethnicity information from 2011 through 2018; for 2019, race/ethnicity data were not reported by all hospitals [14]. Hence, ED visit proportions and rates by race/ethnicity were not determined.
Insurance payer groups available from NIS, KID, and NEDS were comprised of Medicaid, private insurance, and other/unknown, which included Medicare, self-pay, no charge, other, and unknown payers. For 2011–2019, the weighted numbers, percentage of total infant RSVH or BH, percentage of total infant RSV or bronchiolitis ED visits, and hospitalization or ED visit rates per 1000 live births were reported by each payer. Insurance payer groups in NIS and KID were also stratified by race/ethnicity to report percentage of total infant RSVH and BH, and RSVH and BH rates per 1000 live births.
Chronological Age and Birth Month
Chronological age in months was available in 2011 for NIS and 2009 for KID, but it was not available in other calendar years, nor in NEDS. RSVH and BH were reported as proportions of total infant hospitalizations by age in months and by admission month in 2011. The birth months were calculated using admission month and age in months, and hospitalization rates in each birth month in 2011 were reported.
Inpatient Mortality, Hospitalization Length of Stay, MV Use, and Total Charges During Hospitalization or ED Visit
Hospitalizations and ED visits were further described by inpatient mortality and HCU outcomes (ie, hospitalization length of stay [LOS], MV use, and total charge during hospitalization or ED visit), overall and for each year from 2011 through 2019. Inpatient mortality was calculated as the proportion of deaths among all RSVH or BH. MV use was described as the proportion of RSVH, BH, or RSV or bronchiolitis ED visits with an MV procedure code (Supplementary Table 1). From 2011 through 2019, MV use during hospitalization was also described by insurance payer and race/ethnicity; MV use during ED visit was described by insurance payer only. Inpatient mortality data were not stratified further by insurance payer and race/ethnicity due to the HCUP reporting procedures. The geometric mean and 95% CIs for LOS and total charges, which were standardized to the 2020 US dollar (USD), were provided. For the ED visits, 2 HCUP databases provided the patient records: (1) State Emergency Department Databases, which captured discharge information on ED visits that did not result in hospital admissions; and (2) State Inpatient Databases, which reported data on patients seen initially in the ED and then admitted to the same hospital [14]. Separate total charge data were available for these ED categories and thus were reported as total charge for ED visits without hospital admissions and total charge for ED visits leading to hospital admissions. In addition, for the ED visits leading to hospital admissions, hospitalization LOS data were also available.
Up to 30 codes (ICD-9) or 40 codes (ICD-10) could be listed as the diagnosis reason. In the main analysis, the codes for RSV and bronchiolitis were considered in any diagnostic code position given that the use of primary diagnosis codes could introduce bias if there were inconsistencies in the coding practice by the hospitals or physicians [20]. Sensitivity analyses were done using primary diagnosis codes only for RSV and bronchiolitis.
The nonparametric Mann–Kendall test was used to assess overall time trends in hospitalization and ED visit rates from 2011 through 2019. To compare hospitalization or ED visit rates among Medicaid insured infants to those with private insurance and other/unknown insurance and by race/ethnicity, the χ2 test was used. Time trends were assessed using univariate logistic regression models for inpatient mortality and MV use; univariate linear regression models were used for hospitalization or ED visit total charges and hospitalization LOS.
All analyses were conducted using SAS/STAT software, version 9.4 of the SAS System for Windows (SAS Institute, Cary, North Carolina), with statistical procedures that incorporated the sampling design features of the HCUP data. Data were visualized using GraphPad Prism for Mac (version 9.3.1, GraphPad, San Diego, California) and R 1.4.1717 [21] software.
RESULTS
Infant RSV and Bronchiolitis Hospitalizations and ED Visits, Overall and by Year
From 2011 through 2019, the estimated average annual hospitalizations for RSV and bronchiolitis were 56 927 (range, 43 845–66 155) and 92 648 (range, 77 150–104 735), respectively (data not shown). In the same period, the estimated average annual ED visits for RSV and bronchiolitis were 131 999 (range, 89 809–177 680) and 307 710 (range, 227 512–379 961), respectively (data not shown).
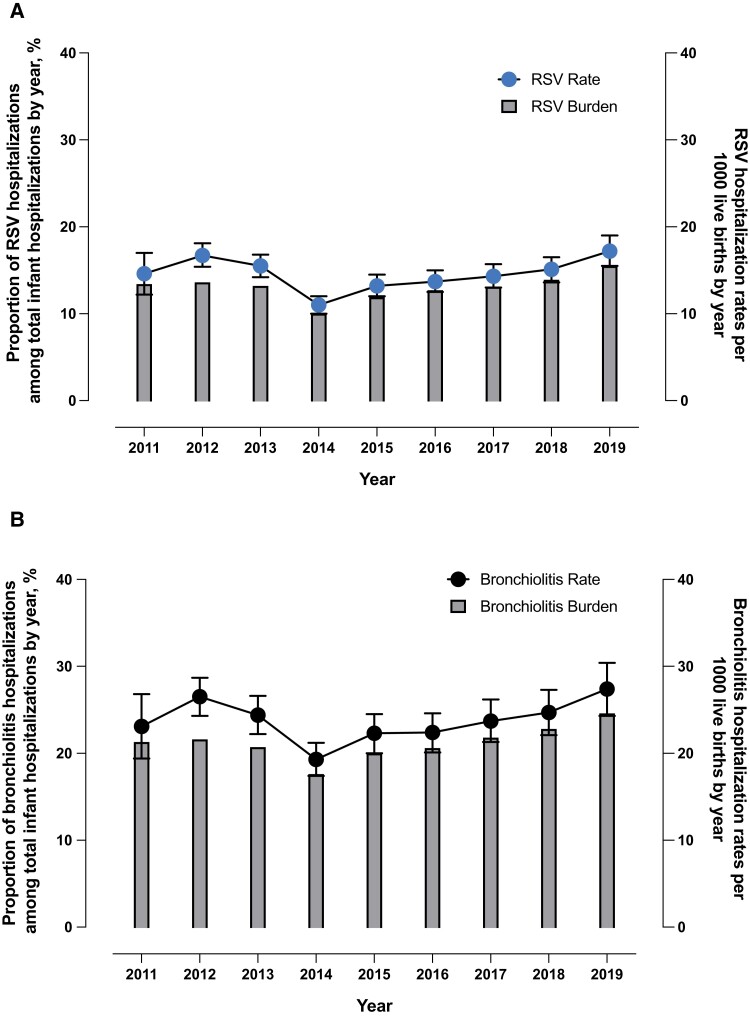
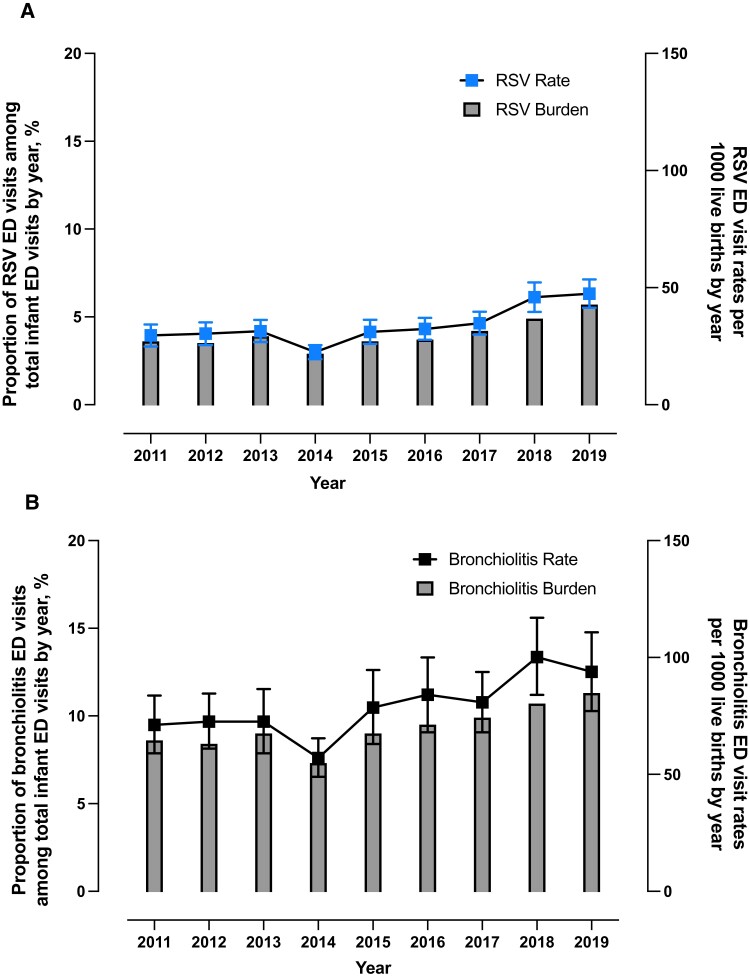
The hospitalization rates remained constant over time from 2011 through 2019 (P = .5 for RSVH; P = .3 for BH) (Figure 1A and 1B). In contrast, RSV and bronchiolitis ED visit rates increased significantly over time (P = .004 for RSV; P = .009 for bronchiolitis) (Figure 2A and 2B). In 2019, RSVH and BH rates were 17.2 (95% CI, 15.5–19.0) and 27.4 (95% CI, 24.3–30.4) per 1000 live births, respectively (Figure 1A and 1B), whereas RSV and bronchiolitis ED visit rates were 47.4 (95% CI, 41.4–53.5) and 93.9 (95% CI, 77.1–110.8) per 1000 live births, respectively (Figure 2A and 2B).
Figure 1.
Respiratory syncytial virus (RSV) (A) and bronchiolitis (B) hospitalization proportions and rates per 1000 live births by admission year, United States infants aged <1 year, National (Nationwide) Inpatient Sample, 2011–2019. To calculate proportions (%), the total number of infant hospitalizations in that year was used as the denominator. RSV and bronchiolitis were defined by International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes: RSV (ICD-9: 079.6, 466.11, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0); bronchiolitis (RSV codes plus unspecified bronchiolitis: ICD-9: 079.6, 466.11, 466.19, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0, J21.8, J21.9). Excludes newborn birth hospitalizations (ICD-9: V30.XX–V39.XX; ICD-10: Z38.XX).
Figure 2.
Respiratory syncytial virus (RSV) (A) and bronchiolitis (B) emergency department (ED) visit burden proportions and rates per 1000 live births by admission year, United States infants aged <1 year, Nationwide Emergency Department Sample, 2011–2019. To calculate proportions (%), the total number of infant ED visits in that year was used as the denominator. RSV and bronchiolitis were defined by International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes: RSV (ICD-9: 079.6, 466.11, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0); bronchiolitis (RSV codes plus unspecified bronchiolitis: ICD-9: 079.6, 466.11, 466.19, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0, J21.8, J21.9). Excludes newborn birth hospitalizations (ICD-9: V30.XX–V39.XX; ICD-10: Z38.XX).
Infant RSV and Bronchiolitis Hospitalizations by Race/Ethnicity and Insurance Payer
From 2011 through 2019, non-Hispanic white (45.7% of total infant RSVH) and Hispanic (22.2%) infants had the highest average RSVH proportions, but AI/AN infants had the highest average rate compared to other groups (19.9 [95% CI, 17.5–22.3] per 1000 live births; P < .0001). Similar patterns were found for BH (Supplementary Figure 1).
From 2011 through 2019, Medicaid infants had the highest average RSVH burden (weighted n = 319 263 [62.3% of total infant RSVH]) compared to those with private (weighted n = 165 767 [32.4%]) and other/unknown insurance (weighted n = 27 316 [5.3%]); similar patterns were observed for BH (Supplementary Figure 2). During the same period, when stratified by race/ethnicity, non-Hispanic white infants with Medicaid (22.4%) and non-Hispanic white infants with private insurance (20.5%) had the highest average RSVH proportions (data not shown).
From 2011 through 2019, Medicaid infants also had the highest average RSVH rate; it was >2-times of other payer groups (Medicaid: 22.3 [95% CI, 21.5–23.1] vs private: 10.3 [95% CI, 9.9–10.7; P < .0001] and other/unknown: 5.8 [95% CI, 5.5–6.1; P < .0001]) per 1000 live births. In the same period, Medicaid infants also had the highest average BH rate (Medicaid: 37.5 [95% CI, 36.0–38.9] vs private: 15.8 [95% CI, 15.2–16.4; P < .0001] and other/unknown: 9.1 [95% CI, 8.6–9.6; P < .0001]) per 1000 live births (Supplementary Figure 2).
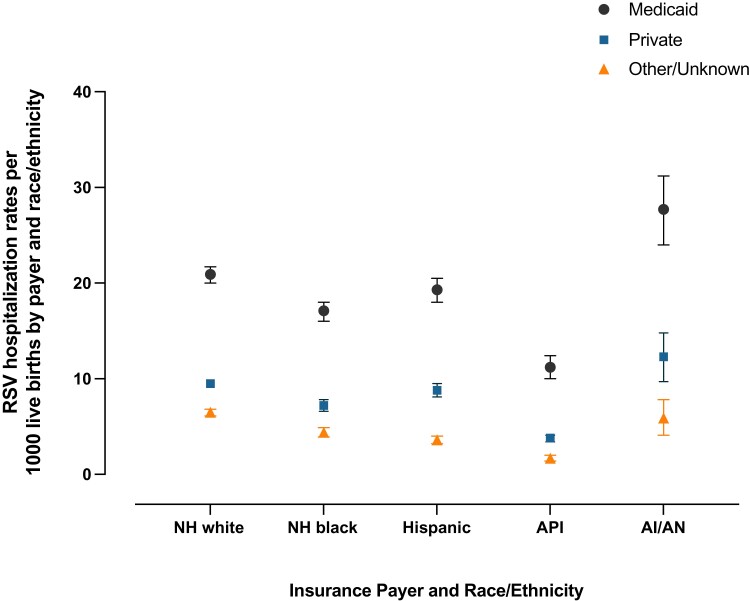
From 2011 through 2019, for all races/ethnicities, Medicaid infants had higher average RSVH rates (up to 7 times) compared to infants with private and other/unknown insurance, with AI/AN Medicaid infants having the highest average rate (27.7 [95% CI, 24.1–31.2] per 1000 live births) (Figure 3). BH rates exhibited similar patterns (Supplementary Figure 3).
Figure 3.
Respiratory syncytial virus (RSV) hospitalization rates per 1000 live births by insurance payer and race/ethnicity, United States infants aged <1 year, National (Nationwide) Inpatient Sample, 2011–2019. RSV was defined by International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes: RSV (ICD-9: 079.6, 466.11, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0). Excludes newborn birth hospitalizations (ICD-9: V30.XX–V39.XX; ICD-10: Z38.XX). Abbreviations: AI/AN, American Indian/Alaska Native; API, Asian and Pacific Islander; NH, non-Hispanic; RSV, respiratory syncytial virus.
Infant RSV and Bronchiolitis ED Visits by Insurance Payer
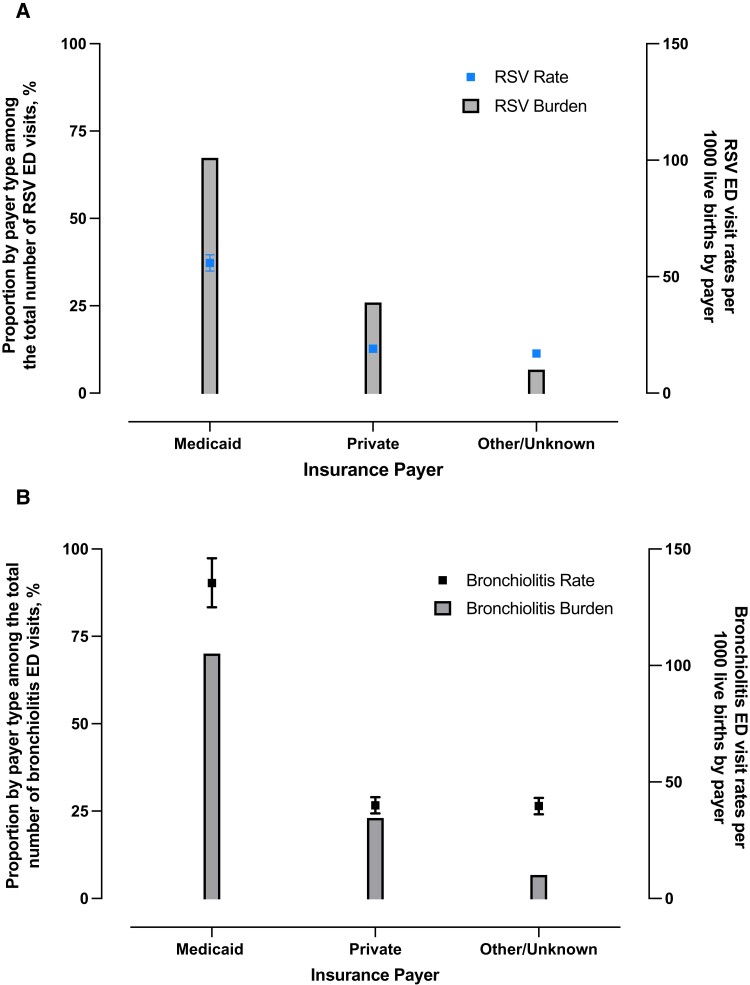
From 2011 through 2019, Medicaid infants had the highest average RSV ED visit proportion (67.3% of total infant RSV ED visits) compared to those with private (25.9%) and other/unknown insurance (6.7%). In the same period, similar patterns were observed for bronchiolitis ED visit proportions (Figure 4A and 4B).
Figure 4.
Respiratory syncytial virus (RSV) (A) and bronchiolitis (B) emergency department (ED) visit proportions and rates per 1000 live births by insurance payer, United States infants aged <1 year, Nationwide Emergency Department Sample, 2011–2019. To calculate proportions (%), the total number of RSV or bronchiolitis ED visits was used as the denominator. RSV and bronchiolitis were defined by International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes: RSV (ICD-9: 079.6, 466.11, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0); bronchiolitis (RSV codes plus unspecified bronchiolitis: ICD-9: 079.6, 466.11, 466.19, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0, J21.8, J21.9). Excludes newborn birth hospitalizations (ICD-9: V30.XX–V39.XX; ICD-10: Z38.XX).
From 2011 through 2019, Medicaid infants also had the highest average RSV ED visit rate (Medicaid: 55.9 [95% CI, 52.4–59.4] vs private: 19.1 [95% CI, 17.7–20.5; P < .0001] and other/unknown: 17.0 [95% CI, 15.7–18.4; P < .0001]) per 1000 live births (Figure 4A). In the same period, Medicaid infants also had the highest average bronchiolitis ED visit rate (Medicaid: 135.4 [95% CI, 124.8–146.0] vs private: 40.0 [95% CI, 36.5–43.5; P < .0001] and other/unknown: 39.7 [95% CI, 36.1–43.2; P < .0001]) per 1000 live births (Figure 4B).
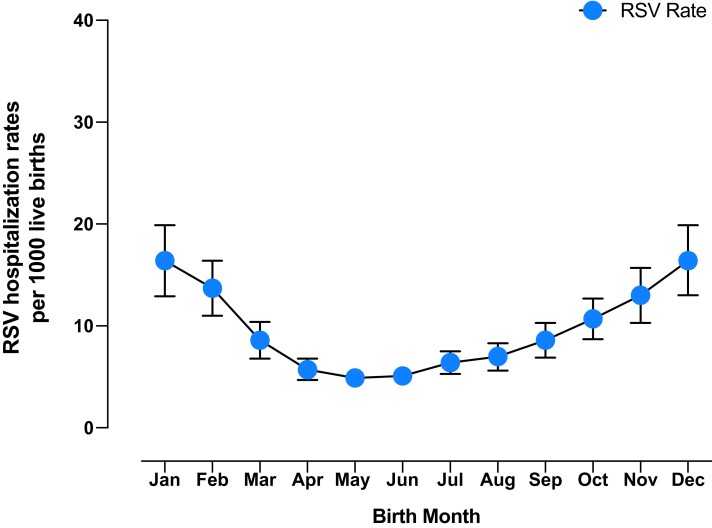
Infant RSV and Bronchiolitis Hospitalizations by Birth Month, Chronological Age, and Admission Month
In 2011, RSVHs and BHs were observed in every birth month, with the highest RSVH rates observed during the birth months of November (15.1 [95% CI, 12.0–18.2]), December (18.8 [95% CI, 14.9–22.7]), January (19.3 [95% CI, 15.2–23.4]), and February (17.1 [95% CI, 13.7–20.4] per 1000 live births) (Figure 5; Supplementary Figure 4). For all ages ≥1 month, >15% of total infant hospitalizations in 2011 were due to RSV during the admission months of January, February, March, and December, with peak RSVH (>40%) in February for ages 1–5 months (Figure 6). For bronchiolitis, 2011 hospitalizations were also highest in the younger age groups, with the highest peak among infants aged 3 months, who accounted for 60% of total infant hospitalizations in February (Supplementary Figure 5).
Figure 5.
Respiratory syncytial virus (RSV) hospitalization rates per 1000 live births by birth month, United States infants aged <1 year, National (Nationwide) Inpatient Sample, 2011. Birth month was available only in 2011. RSV was defined by International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes: RSV (ICD-9: 079.6, 466.11, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0). Excludes newborn birth hospitalizations (ICD-9: V30.XX–V39.XX; ICD-10: Z38.XX).
Figure 6.
Respiratory syncytial virus (RSV) as a proportion of total infant hospitalizations by age (in months) and by admission month, United States infants aged <1 year, National (Nationwide) Inpatient Sample, 2011. Age was available only in 2011. Proportions (%) in each cell were calculated using the total number of infant hospitalizations for chronological age and during each admission month as the denominator. Example interpretation: Of all infants aged 1 month and admitted to the hospital in January, 34.7% were hospitalized due to RSV. RSV was defined by International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes: RSV (ICD-9: 079.6, 466.11, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0). Excludes newborn birth hospitalizations (ICD-9: V30.XX–V39.XX; ICD-10: Z38.XX). Sample sizes ≤10 were not reported, in accordance with the Agency for Healthcare Research and Quality's Healthcare Cost and Utilization Project.
Inpatient RSV and Bronchiolitis Mortality, Hospitalization LOS, MV Use, and Total Charge During Hospitalization or ED Visit
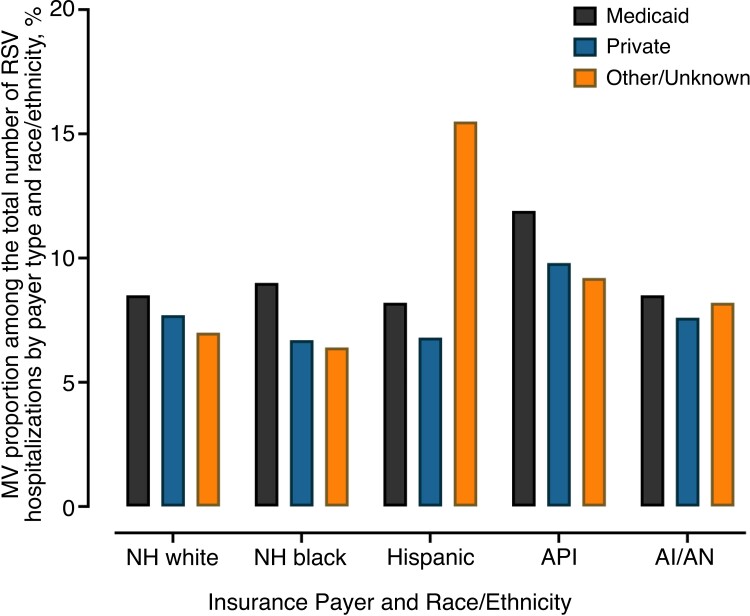
Inpatient RSV mortality was constant over time from 2011 (weighted n = 61 [0.11%]; standard error [SE], 0.03) of RSVH) to 2019 (weighted n = 55 [0.09%]; SE, 0.02; P = .8) (data not shown). In 2011, hospitalization LOS was 2.5 days (95% CI, 2.4–2.6 days); in 2019, it increased to 2.8 days (95% CI, 2.7–2.9 days; P < .0001). MV use was increased from 4.8% (SE, 0.8) of RSVH in 2011 to 12.8% (SE, 1.0) in 2019 (P < .0001). From 2011 through 2019, Medicaid infants had higher average MV use proportions compared to infants with private and other/unknown insurance across nearly all races/ethnicities except Hispanics (Figure 7). Standardized to 2020 USD, the total charge during hospitalization also increased from $11 273 (95% CI, $10 275–$12 369) in 2011 to $21 513 (95% CI, $20 280–$22 820) in 2019 (P < .0001). Inpatient bronchiolitis mortality increased over time from 2011 (weighted n = 81 [0.09%] of BH; SE, 0.03) to 2019 (weighted n = 160 [0.16%] of BH; SE, 0.03) (P = .01). Hospitalization LOS, MV use, and total charges for bronchiolitis were similar to those for RSV (data not shown).
Figure 7.
Mechanical ventilation (MV) proportions among respiratory syncytial virus (RSV) hospitalizations by insurance payer and race/ethnicity, United States infants aged <1 year, National (Nationwide) Inpatient Sample, 2011–2018. To calculate proportions (%), the total number of infant RSV hospitalizations regardless of MV use for that insurance payer and race/ethnicity was used as the denominator. RSV was defined by International Classification of Diseases, Ninth and Tenth Revision (ICD-9 and ICD-10) diagnosis codes: RSV (ICD-9: 079.6, 466.11, 480.1; ICD-10: B97.4, J12.1, J20.5, J21.0). Excludes newborn birth hospitalizations (ICD-9: V30.XX–V39.XX; ICD-10: Z38.XX). Abbreviations: AI/AN, American Indian/Alaska Native; API, Asian and Pacific Islander; MV, mechanical ventilation; NH, non-Hispanic; RSV, respiratory syncytial virus.
For RSV ED visits, MV use increased from 2.5% (SE, 0.4) in 2011 to 3.3% (SE, 0.9) in 2019 (P = .046) (data not shown). From 2011 through 2019, Medicaid infants had higher average MV use proportions in the ED (1.9% of total RSV ED visits) compared to private (0.89%) and other/unknown insurance (0.14%) (data not shown). Among RSV ED visits leading to hospital admissions, hospitalization LOS was increased from 2.6 days (95% CI, 2.4–2.7 days) in 2011 to 2.7 days (95% CI, 2.5–3.0 days) in 2019 (P < .0001). Standardized to 2020 USD, the total charge for RSV ED visits without hospital admissions was $1433 (95% CI, $1337–$1537) in 2011, which increased to $2237 (95% CI, $2074–$2414) in 2019 (P < .0001). The total charge for RSV ED visits leading to hospital admissions increased from $13 880 (95% CI, $12 649–$15 231) in 2011 to $21 964 (95% CI, $19 631–$24 573) in 2019 (P < .0001). MV use and total charges for bronchiolitis ED visits without hospital admissions or leading to hospital admissions were similar to those for RSV (data not shown).
Sensitivity and confirmatory analyses in KID 2009, 2012, 2016, and 2019 provided similar results (see Supplementary Materials for details).
DISCUSSION
This retrospective study is based on the most recent, largest publicly available all-payer databases in the US to describe infant RSV and bronchiolitis burden, rates, and HCU in inpatient hospital and ED settings. To our knowledge, this is the first study since 2000 to provide infant RSV epidemiology data for the ED setting based on nationally representative data [7]. We found that infant RSVH rates have remained stable over time, whereas RSV ED visit rates have increased. In addition, inpatient RSV mortality has remained constant over time, while MV use and the total charges associated with RSV have increased, highlighting the impacts of this serious illness on infants.
We also observed that by race/ethnicity and insurance payer, Medicaid infants generally had the highest average hospitalization burden, rates, and MV use over the entire study period (2011–2019), suggesting that the effects of RSV may be most pronounced in this population. To our knowledge, Sangaré et al (2006) is the only published study to evaluate hospitalizations by insurance payer and race/ethnicity from 1999 to 2003 in California and reported that Medi-Cal infants had higher RSVH rates compared to non–Medi-Cal infants for all races/ethnicities [7, 22]. As health equity is a critical domain for policy discussions, continued monitoring of infants with Medicaid insurance in all healthcare settings is needed.
As this study provides the most recent national estimates of RSVH and RSV ED visits, an update of the Centers for Disease Control and Prevention’s (CDC) RSV immunization strategy impact model may be warranted. Compared to the CDC model’s estimated annual infant RSVH (n = 33 180 [range, 24 760–42 900]) [23], we found that the estimated annual average infant RSVH from 2011 through 2019 (n = 56 927 [range, 43 845–66 155]) was 1.7 times higher than the CDC point estimate and also exceeded its upper limit range. This may be due to variations in time, geographical locations, and study population characteristics. The CDC model was based on hospitalized infants with laboratory-confirmed RSV from the 2000–2009 New Vaccine Surveillance Network in 3 states [23, 24]. In contrast, this study utilized 2011–2019 data from a 20%-stratified sample of all hospital discharges in US community hospitals, which represented 97% of the US population [15]. From the 2014–2015 Influenza Hospitalization Surveillance Network conducted in 4 states, infant RSVH was 44 731 [25], which was higher than the CDC’s estimate. An update of the CDC model using these recent RSV estimates may enhance the assessments of existing and potentially new immunization strategies.
Palivizumab is the only existing immunoprophylaxis for RSV, but its benefit remains restricted to a limited population, that is, premature infants born ≤28 wGA, or those with CLD or hs-CHD, per recommended use [6]. Hence, consideration of the size of the infant population not eligible for palivizumab may be important to substantially reduce the impacts of RSV. The US natality data from the CDC Wide-ranging Online Data for Epidemiologic Research (WONDER) database reported that preterm births (born <37 wGA) represented 10% of 3.7 million total live births from 2016 to 2019; <28 wGA infants represented 0.66%; CHD at birth (indicated as cyanotic CHD) represented 0.06% [26]. Full-term infants and those without comorbidity conditions, who are not eligible for palivizumab, comprise much of the infant population in the US. Future RSV immunization strategies should consider all infants.
This study has some limitations. First, the unit of analysis in this study was hospitalizations or ED visits and not the number of infants. An infant could have contributed multiple hospitalizations or ED visits for RSV and bronchiolitis. Second, diagnosis based on ICD codes may not be able to accurately determine outcomes with potential errors in coding [27]. Although the codes for bronchiolitis were utilized, RSV-coded cases were likely to be underestimated because testing is not universally recommended in the US [18]. Third, only the total charges (amount set by the health provider) were reported, which may be different from the total costs (amount paid by the patient). Fourth, this study was limited to infants aged <1 year, but the impact of RSV is also notable for children aged ≥1 year [25, 28]. wGA data were also limited; risk and burden by gestational age could not be assessed. Additionally, this study described inpatient mortality, but deaths outside the inpatient setting accounted for >21% of infant RSV deaths [29, 30]. Thus, the true healthcare burden of RSV is likely to be higher than the reported results herein, and its public health impact underestimated.
A major strength of this study was the use of a cohort design with nationally representative sampling of community hospitals in the US. Infant hospitalization and ED visit numbers were large and robust, which allowed detection of significant trends in the dataset overall and within important subgroups by sociodemographic variables. Importantly, the datasets were comprehensive, allowing for complete reporting of all outcomes related to hospitalizations and ED visits including inpatient mortality, MV use, and total charges.
In conclusion, this study provides recent national estimates of RSV burden and risk for all infants in the inpatient and ED settings, noting significantly higher burden and risk for Medicaid-insured infants. With significant increases observed over time in MV use and total charges associated with RSV, HCU is not negligible in the US infant population. These findings highlight the need to focus on early detection of RSV and ensure access to RSV preventive measures to mitigate disease severity for all infants.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online (http://jid.oxfordjournals.org/). Supplementary materials consist of data provided by the author that are published to benefit the reader. The posted materials are not copyedited. The contents of all supplementary data are the sole responsibility of the authors. Questions or messages regarding errors should be addressed to the author.
Supplementary Material
Contributor Information
Mina Suh, EpidStrategies, a Division of ToxStrategies, Rockville, Maryland, USA.
Naimisha Movva, EpidStrategies, a Division of ToxStrategies, Rockville, Maryland, USA.
Xiaohui Jiang, EpidStrategies, a Division of ToxStrategies, Rockville, Maryland, USA.
Heidi Reichert, EpidStrategies, a Division of ToxStrategies, Rockville, Maryland, USA.
Lauren C Bylsma, EpidStrategies, a Division of ToxStrategies, Rockville, Maryland, USA.
Jon P Fryzek, EpidStrategies, a Division of ToxStrategies, Rockville, Maryland, USA.
Christopher B Nelson, Sanofi, Swiftwater, Pennsylvania, USA.
Notes
Acknowledgments. Editorial assistance was provided by inScience Communications (Philadelphia, Pennsylvania). This work was performed in accordance with current Good Publication Practice guidelines.
Financial support. This collaborative study with EpidStrategies was funded/sponsored by Sanofi and AstraZeneca.
Supplement sponsorship. This article appears as part of the supplement “Respiratory Syncytial Virus Disease Among US Infants,” sponsored by Sanofi and AstraZeneca.
References
- 1. Suh M, Movva N, Jiang X, et al. . Respiratory syncytial virus is the leading cause of United States infant hospitalizations, 2009–2019: a study of the National (Nationwide) Inpatient Sample. J Infect Dis 2022; 226(S2):S154–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Leader S, Kohlhase K. Recent trends in severe respiratory syncytial virus (RSV) among US infants, 1997 to 2000. J Pediatr 2003; 143:S127–32. [DOI] [PubMed] [Google Scholar]
- 3. Holman RC, Curns AT, Cheek JE, et al. . Respiratory syncytial virus hospitalizations among American Indian and Alaska Native infants and the general United States infant population. Pediatrics 2004; 114:e437–44. [DOI] [PubMed] [Google Scholar]
- 4. Yorita KL, Holman RC, Sejvar JJ, Steiner CA, Schonberger LB. Infectious disease hospitalizations among infants in the United States. Pediatrics 2008; 121:244–52. [DOI] [PubMed] [Google Scholar]
- 5. Ledbetter J, Brannman L, Wade SW, Gonzales T, Kong AM. Healthcare resource utilization and costs in the 12 months following hospitalization for respiratory syncytial virus or unspecified bronchiolitis among infants. J Med Econ 2020; 23:139–47. [DOI] [PubMed] [Google Scholar]
- 6. American Academy of Pediatrics Committee on Infectious Diseases, American Academy of Pediatrics Bronchiolitis Guidelines Committee . Updated guidance for palivizumab prophylaxis among infants and young children at increased risk of hospitalization for respiratory syncytial virus infection. Pediatrics 2014; 134:e620–38. [DOI] [PubMed] [Google Scholar]
- 7. Suh M, Movva N, Bylsma L, et al. . A systematic literature review of the burden of respiratory syncytial virus and health care utilization among United States infants younger than 1 year. J Infect Dis 2022; 226(S2):S195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Karron RA. Preventing respiratory syncytial virus (RSV) disease in children. Science 2021; 372:686–7. [DOI] [PubMed] [Google Scholar]
- 9. Domachowske J, Madhi SA, Simões EAF, et al. . Safety of nirsevimab for RSV in infants with heart or lung disease or prematurity. N Engl J Med 2022; 386:892–4. [DOI] [PubMed] [Google Scholar]
- 10. Hammitt LL, Dagan R, Yuan Y, et al. . Nirsevimab for prevention of RSV in healthy late-preterm and term infants. N Engl J Med 2022; 386:837–46. [DOI] [PubMed] [Google Scholar]
- 11. ClinicalTrials.gov . A trial to evaluate the efficacy and safety of RSVpreF in infants born to women vaccinated during pregnancy. ClinicalTrials.gov Identifier: NCT04424316.https://clinicaltrials.gov/ct2/show/NCT04424316?type=Intr&cond=rsv&phase=2&draw=3. Accessed 4 April 2022.
- 12. Healthcare Cost and Utilization Project . Overview of HCUP. https://www.hcup-us.ahrq.gov/overview.jsp. Accessed 27 January 2022.
- 13. Healthcare Cost and Utilization Project . KID overview. https://www.hcup-us.ahrq.gov/kidoverview.jsp. Accessed 27 January 2022.
- 14. Healthcare Cost and Utilization Project . Overview of the National Emergency Department Sample (NEDS). https://www.hcup-us.ahrq.gov/nedsoverview.jsp. Accessed 27 January 2022.
- 15. Healthcare Cost and Utilization Project . Overview of the National (Nationwide) Inpatient Sample (NIS). https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 27 January 2022.
- 16. Doucette A, Jiang X, Fryzek J, Coalson J, McLaurin K, Ambrose CS. Trends in respiratory syncytial virus and bronchiolitis hospitalization rates in high-risk infants in a United States nationally representative database, 1997–2012. PLoS One 2016; 11:e0152208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention, National Center for Health Statistics . National Vital Statistics System: birth data. https://www.cdc.gov/nchs/nvss/births.htm. Accessed 27 January 2022. [Google Scholar]
- 18. American Academy of Pediatrics . Respiratory syncytial virus. In: Pickerling LK, Baker CJ, Kimberlin DW, Long SS, eds. Red book: 2012 report of the Committee on Infectious Diseases. 29th ed. Elk Grove Village, IL: American Academy of Pediatrics, 2012:609–18. [Google Scholar]
- 19. McDermott KW, Elixhauser A, Sun R. Trends in hospital inpatient stays in the United States, 2005–2014. HCUP Statistical Brief #225. Rockville, MD: Agency for Healthcare Research and Quality, 2017. [Google Scholar]
- 20. O'Malley KJ, Cook KF, Price MD, Wildes KR, Hurdle JF, Ashton CM. Measuring diagnoses: ICD code accuracy. Health Serv Res 2005; 40:1620–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. R Core Team . A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2021. [Google Scholar]
- 22. Sangaré L, Curtis MP, Ahmad S. Hospitalization for respiratory syncytial virus among California infants: disparities related to race, insurance, and geography. J Pediatr 2006; 149:373–7. [DOI] [PubMed] [Google Scholar]
- 23. Rainisch G, Adhikari B, Meltzer MI, Langley G. Estimating the impact of multiple immunization products on medically-attended respiratory syncytial virus (RSV) infections in infants. Vaccine 2020; 38:251–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hall CB, Weinberg GA, Blumkin AK, et al. . Respiratory syncytial virus-associated hospitalizations among children less than 24 months of age. Pediatrics 2013; 132:e341–8. [DOI] [PubMed] [Google Scholar]
- 25. Arriola CS, Kim L, Langley G, et al. . Estimated burden of community-onset respiratory syncytial virus-associated hospitalizations among children aged <2 years in the United States, 2014–15. J Pediatric Infect Dis Soc 2020; 9:587–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Centers for Disease Control and Prevention, National Center for Health Statistics Division of Vital Statistics . Natality public-use data 2016–2019, on CDC WONDER online database, October 2020. http://wonder.cdc.gov/natality-expanded-current.html. Accessed 27 January 2022.
- 27. Walsh P, Rothenberg SJ. Which ICD-9-CM codes should be used for bronchiolitis research? BMC Med Res Methodol 2018; 18:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Rha B, Curns AT, Lively JY, et al. . Respiratory syncytial virus-associated hospitalizations among young children: 2015–2016. Pediatrics 2020; 146:e20193611. [DOI] [PubMed] [Google Scholar]
- 29. Hansen CL, Chaves SS, Demont C, Viboud C. Mortality associated with influenza and respiratory syncytial virus in the US, 1999–2018. JAMA Netw Open 2022; 5:e220527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Reichert H, Suh M, Jiang X, et al. . Mortality associated with respiratory syncytial virus, bronchiolitis, and influenza among infants in the United States: a birth cohort study from 1999 to 2018. J Infect Dis 2022; 226(S2):S246–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.