Abstract
Background:
The indirect consequences of the COVID-19 pandemic in older adults, such as stress, are unknown. We sought to describe the stressors and perceived consequences of the COVID-19 pandemic on older adults in Canada and to evaluate differences by socioeconomic factors.
Methods:
We conducted a cross-sectional study using data from the Canadian Longitudinal Study on Aging COVID-19 Exit Questionnaire (September–December 2020). A 12-item checklist was used to assess stressors (e.g., income loss, separation from family) experienced during the pandemic, and a single question was used to measure perceived consequences. We used a generalized linear model with a binomial distribution and log link to estimate prevalence ratios and 95% confidence intervals (CIs) for the association between socioeconomic factors, stressors and perceived consequences.
Results:
Among the 23 972 older adults (aged 50–96 yr) included in this study, 17 977 (75.5%) reported at least 1 stressor during the pandemic, with 5796 (24.4%) experiencing 3 or more stressors. The consequences of the pandemic were perceived as negative by 23 020 (63.1%) participants. Females were more likely to report most stressors than males, such as separation from family (adjusted prevalence ratio 1.31, 95% CI 1.28–1.35). The perceived consequences of the pandemic varied by region; residents of Quebec were less likely to perceive the consequences of the pandemic as negative (adjusted prevalence ratio 0.87, 95% CI 0.84–0.91) than those of the Atlantic provinces.
Interpretation:
These findings suggest that older adults across Canada experienced stressors and perceived the pandemic consequences as negative, though stressors and perceptions of consequences varied by socioeconomic factors and geography, highlighting inequalities. Future research will be needed to estimate the impact of stress during the pandemic on future health outcomes.
In addition to the direct impacts of the COVID-19 pandemic and the associated public health measures of prevention, the pandemic has had several indirect consequences on population health.1,2 One such indirect consequence of the pandemic is increased stress.3 Stress has a major impact on both physical and mental health, including cardiovascular disease, stroke, diabetes, anxiety and depression. 2,4–6 Measures of stress can include both objective and perceived measures.7,8 Objective measures include economic hardships, loss of possessions, family and social stressors, and loss of daily activities.9 Perceived measures of stress include an individual’s perceived ability to cope with the demands or presence of a disaster.8,10 Previous research on population-level disasters, including earthquakes and floods, has found that exposure to stress during an acute disaster has a profound impact on long-term health outcomes, including chronic diseases.11
Given the dramatic change in daily functioning during the COVID-19 pandemic, several factors (e.g., limited access to physical activity facilities, closures) may contribute to increased incidence of obesity, cardiovascular disease and type 2 diabetes; however, it has been hypothesized that chronic stress, in particular, may influence disease development.12 Like other disasters, the COVID-19 pandemic can be viewed as a stressful event, as it has completely altered the daily activities of individuals across the globe.13
A systematic review from early in the pandemic found a high prevalence of stress that differed by sex, age, unemployment, and presence of chronic or psychiatric illness.14 A study conducted in the United States during the pandemic (April 2020) found that a high proportion of participants (83.7%) experienced stressors, such as changes to social routines;15 another study conducted in China (January–February 2020) found that people reported higher experiences of stress throughout the pandemic, compared with prepandemic levels.16 However, these studies noted limitations, including lack of generalizability and small sample sizes.15,16
Experiences of stress and coping vary among older adults, whereby adults in the oldest age groups have reported less mental health effects early in the pandemic, despite their increased risk for worse health outcomes with COVID-19.17 Experiences of stress also vary by socioeconomic characteristics. 18,19 We sought to describe the prevalence of stressors and the perceived consequences reported by older adults during the COVID-19 pandemic and to evaluate how they differed by socioeconomic factors.
Methods
Study design and data source
We conducted a cross-sectional analysis using data from participants in the Canadian Longitudinal Study on Aging (CLSA). The CLSA is a nationally generalizable study of community-dwelling adults aged 45–85 years at the time of recruitment. Participants were recruited from all 10 Canadian provinces from 2010 to 2015 and will be followed up every 3 years for at least 20 years or until death or loss to follow-up. Data were collected at baseline (2011–2015) and at first follow-up (2015–2018). In April 2020, the CLSA COVID-19 Questionnaire Study was implemented to collect longitudinal, pandemic-related data over a 9-month period by web or phone. A baseline survey was administered from April to June 2020, and the exit survey was administered from September to December 2020. Additional details regarding the CLSA methodology can be found in Appendix 1, Supplementary Information, available at www.cmajopen.ca/content/10/3/E721/suppl/DC1, and have been extensively described.20
Participants
Participants were selected into the CLSA using a population-based sampling strategy.20 Inclusion criteria required that people be able to complete interviews in either English or French, be cognitively able to participate on their own, not be institutionalized and not reside in a Canadian territory or on a Federal First Nations reserve. Individuals who were full-time members of the Canadian Armed Forces were also not eligible to be included in the study. Participants of the CLSA who were still alive, had not withdrawn, did not require a proxy to assist with completion of surveys and had sufficient contact information were eligible to be invited to participate in the CLSA COVID-19 Questionnaire Study.
Outcomes
Two questions in the CLSA COVID-19 Questionnaire Study exit survey (September–December 2020) were used to assess stressors and perceived consequences during the pandemic. To measure stressors (i.e., objective stress), participants were asked if they had experienced any of the following 12 items throughout the pandemic: the participant was ill, someone close to the participant was ill, someone close to the participant died, loss of income, participant was unable to access necessary food and supplies, participant was unable to access health care, participant was unable to access usual prescriptions, participant experienced increased conflict, participant experienced separation from family, participant was responsible for increased caregiving, participant was unable to care for those who require assistance owing to limitations, and participant experienced breakdown in family relationships. Participants could select multiple stressors. Each stressor was considered individually, and the number of stressors was summed to create a total score reflecting the cumulative number of stressors participants had reported.
To assess how participants perceived the consequences of the COVID-19 pandemic (i.e., perceived stress), they were asked a single question: “Taking everything about COVID-19 into account, how would you describe the consequences of COVID-19 on you and your household?” Answers were collected with a 5-point Likert scale that ranged from very negative to very positive. The development of this question was based on the Transactional Model of Stress and Coping,9 which states that when an individual encounters a stressful event, their ability to cope is related to whether a threat is perceived or not. If a threat is perceived, then this leads to increased stress.9 Given the relatively small proportion of participants who reported the extreme response options, we combined the very negative and negative, and positive and very positive responses. We combined neutral responses with positive and very positive responses in the regression analysis to create a binary variable, as we were most interested in understanding negative and very negative outcomes. The measures used for objective stress and perceived stress have been used to measure stress during previous disasters.7,8,21–23
Other variables
From the literature, we selected descriptor variables that may introduce variation in experiences of stress and perceptions of the consequences of the pandemic.15,24,25 We collected participant age group (50–64 yr, 65–74 yr or 75–96 yr), region, urban or rural status (based on postal code),26 and essential worker status from the CLSA COVID-19 Questionnaire Study baseline survey (April–June 2020). We categorized province of residence into regions, including Atlantic (Newfoundland, New Brunswick, Nova Scotia, Prince Edward Island), Quebec, Ontario, Prairies (Manitoba, Saskatchewan, Alberta) and British Columbia. Participants were asked if they usually work at a job outside of their residence and if they were considered an essential worker. We categorized participants as not usually working outside the household, working as an essential worker and working outside the household but not as an essential worker. We collected household income (< $50 000, $50 000–$99 999, $100 000–$149 999 and ≥ $150 000) and marital status (single [never married or never lived with partner], married or living with partner in a common-law relationship, widowed, and divorced or separated) from the first CLSA follow-up (2015–2018). We collected participant sex (male or female), racial background (dichotomized as white or nonwhite) and education level (secondary school graduation or less, some postsecondary education, or postsecondary degree or diploma) from the CLSA baseline survey (2011–2015).
Statistical analysis
We conducted all statistical analyses using SAS 9.4. Descriptive statistics included the frequency of each stressor, the total number of stressors and the distribution of the perceived consequences of the pandemic, overall and by selected socioeconomic variables. To evaluate the association between socioeconomic factors and each of the individual stressors and the binary perceived consequences variable, separately, we used a generalized linear model (PROC GENMOD) with a binomial distribution and log link. For all outcomes, we estimated unadjusted (separately for each socioeconomic factor [sex, age group, urban or rural status, region, essential worker status, household income, marital status, racial background and education]) and fully adjusted (including all socioeconomic factors) prevalence ratios with 95% confidence intervals (95% CIs). To evaluate the association between socioeconomic factors and the total number of stressors (ranging from 0 to 12), we used a generalized linear model (PROC GENMOD) with a negative binomial distribution and log link to estimate prevalence ratios and 95% CIs. We chose a negative binomial distribution as it was a good approximation of the distribution of the total stressor score (Appendix 1, Figure A1). We conducted a complete case analysis as less than 6% of participants were missing data on some variables. Although sampling weights have been developed for the CLSA sample at baseline, these weights cannot be used for the subsample that completed the CLSA COVID-19 Questionnaire Study, thus we did not use sampling weights for this analysis.
Ethics approval
Ethics approval for this study was received from the Hamilton Integrated Research Ethics Board.
Results
Overall, 51 338 participants were recruited to the CLSA, of which 44 817 completed the first follow-up. A total of 24 114 participants completed the CLSA COVID-19 exit survey and 23 785 had available data for this study (see flow diagram in Appendix 1, Supplementary Figure A2). The fully adjusted models included fewer participants as some were missing data on certain variables. Overall, 8269 (34.8%) were aged 50–64 years, 8705 (36.6%) were aged 65–74 years and 6811 (28.6%) were aged 75–96 years; 12 640 (53.1%) participants were female, and the vast majority were of white racial background (n = 23 091, 97.1%). The complete descriptive characteristics of the study sample can be found in Table 1. Participants of the CLSA COVID-19 Questionnaire Study have previously been compared with the total CLSA study population, and were slightly more educated and had higher income, but few other differences were observed.27
Table 1:
Characteristics of participants from the Canadian Longitudinal Study on Aging (CLSA) COVID-19 Questionnaire Study
| Characteristic | No. (%) of participants n = 23 785 |
|---|---|
| Sex* | |
| Male | 11145 (47.5) |
| Female | 12 640 (52.5) |
| Age group†, yr | |
| 50–64 | 8269 (34.8) |
| 65–74 | 8705 (36.5) |
| 75–96 | 6811 (28.6) |
| Racial background* | |
| White | 23091 (97.2) |
| Nonwhite | 668 (2.8) |
| Missing | 26 |
| Education* | |
| Secondary school graduation or less | 3426 (14.4) |
| Some postsecondary education | 17106 (7.2) |
| Postsecondary degree or diploma | 18609 (78.4) |
| Missing | 44 |
| Total household income‡, $ | |
| < 50 000 | 5663 (25.3) |
| 50 000–99 999 | 8514 (37.9) |
| 100 000–149 999 | 4554 (20.3) |
| ≥ 150 000 | 3726 (16.6) |
| Missing | 1328 |
| Region† | |
| Atlantic§ | 4297 (18.1) |
| Quebec | 4299 (18.1) |
| Ontario | 5509 (23.2) |
| Prairies¶ | 5091 (21.4) |
| British Columbia | 4589 (19.3) |
| Marital status‡ | |
| Single (never married or never lived with partner) | 1992 (8.4) |
| Married or common-law relationship | 16711 (70.3) |
| Widowed | 2311 (9.7) |
| Divorced or separated | 2757 (11.6) |
| Missing | 14 |
| Essential worker status† | |
| Does not work outside the home | 17244 (74.6) |
| Essential worker | 2478 (10.7) |
| Not essential worker | 3392 (14.7) |
| Missing | 671 |
| Urban or rural status† | |
| Urban | 19447 (82.2) |
| Rural | 4214 (17.8) |
| Missing | 124 |
Data collected at CLSA baseline (2011–2015).
Data collected at CLSA COVID-19 Questionnaire baseline survey (April–June 2020).
Data collected at CLSA follow-up 1 (2015–2018).
Newfoundland, New Brunswick, Nova Scotia, Prince Edward Island.
Manitoba, Saskatchewan, Alberta.
Stressors during the COVID-19 pandemic
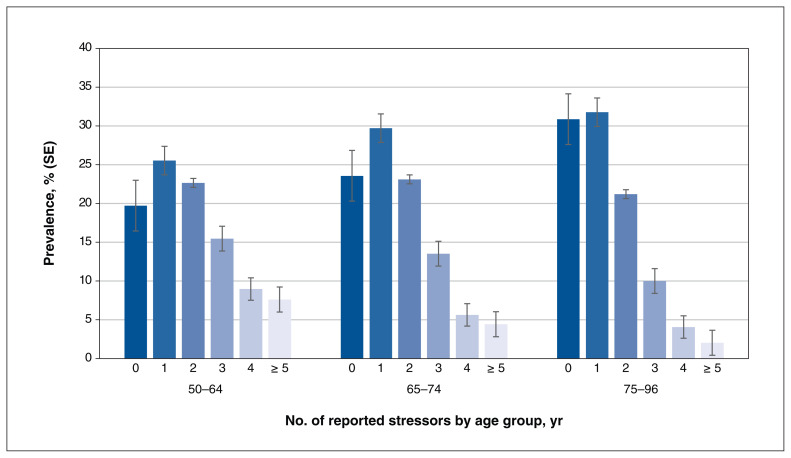
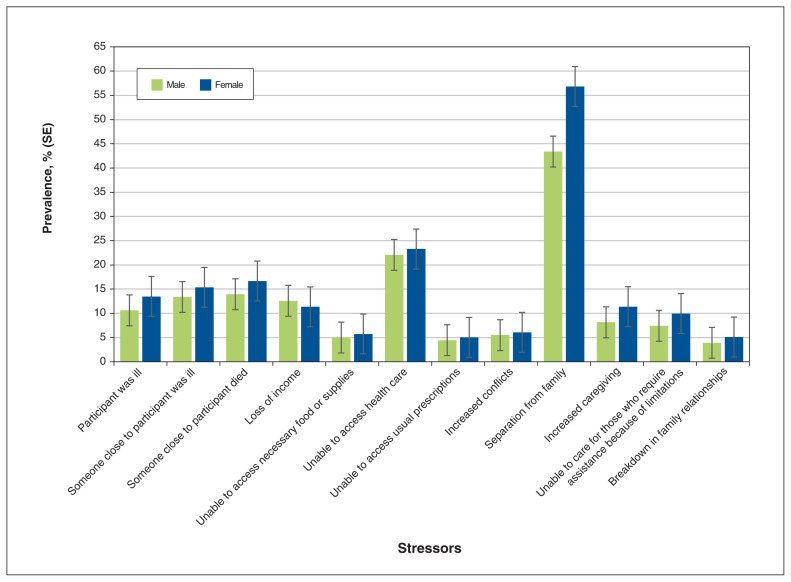
The total number of stressors reported by age group is described in Figure 1. The mean and median number of stressors were 1.7 (standard deviation 1.5) and 1.0 (interquartile range 1.0), respectively. Figure 2 presents the prevalence of each individual stressor at the exit survey by sex. The most frequently reported stressors were being separated from family and being unable to access health care. Appendix 1, Supplemental Table A1 presents the prevalence of each reported stressor by sociodemographic factors.
Figure 1:
Prevalence of total reported stressors with standard error (SE) bars by age group among participants (n = 23 758) of the Canadian Longitudinal Study on Aging (CLSA) at the time of the CLSA COVID-19 Questionnaire Study exit survey (September–December 2020).
Figure 2:
Prevalence of stressors with standard error (SE) bars among participants (n = 23 758) of the Canadian Longitudinal Study on Aging (CLSA), by sex, at the time of the CLSA COVID-19 Questionnaire Study exit survey (September–December 2020).
The adjusted prevalence ratios for the associations between socioeconomic factors and each stressor are presented in Table 2. Females were more likely than males to report most stressors. For example, females were more likely to report increased caregiving and separation from family. Low household income (< $50 000) was associated with an increased likelihood of being unable to access necessary food or supplies, compared with an income of $100 000–$149 999. Most unadjusted associations were similar to adjusted associations (Appendix 1, Supplemental Table A2).
Table 2:
Adjusted associations between socioeconomic characteristics and individual stressors among participants (n = 21 605) of the Canadian Longitudinal Study on Aging (CLSA) at the time of the CLSA COVID-19 Questionnaire Study exit survey (September–December 2020)
| Characteristic | Adjusted PR (95% CI)* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participant was ill | Someone close was ill | Someone close died | Loss of income | Unable to access food or supplies | Unable to access health care | Unable to access prescriptions | Increased conflict | Separation from family | Increased caregiving | Unable to care for those who require assistance | Breakdown in family relationships | |
| Sex | ||||||||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 1.22 (1.14–1.33) | 1.16 (1.09–1.24) | 1.17 (1.10–1.25) | 0.89 (0.83–0.96) | 1.05 (0.93–1.18) | 1.05 (1.00–1.09) | 1.11 (0.98–1.26) | 1.10 (0.98–1.23) | 1.31 (1.28–1.35) | 1.49 (1.37–1.62) | 1.33 (1.22–1.45) | 1.28 (1.12–1.45) |
| Age group, yr | ||||||||||||
| 50–64 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| 65–74 | 0.90 (0.82–0.99) | 0.84 (0.77–0.92) | 0.96 (0.88–1.05) | 0.62 (0.57–0.58) | 0.63 (0.54–0.72) | 0.92 (0.87–0.98) | 0.82 (0.70–0.96) | 0.69 (0.60–0.79) | 1.01 (0.97–1.04) | 0.70 (0.63–0.78) | 0.78 (0.70–0.87) | 0.68 (0.58–0.80) |
| 75–96 | 0.70 (0.62–0.78) | 0.80 (0.72–0.88) | 1.04 (0.95–1.15) | 0.31 (0.26–0.36) | 0.36 (0.29–0.43) | 0.68 (0.63–0.74) | 0.62 (0.51–0.75) | 0.57 (0.47–0.67) | 0.87 (0.83–0.90) | 0.52 (0.46–0.60) | 0.51 (0.44–0.59) | 0.50 (0.41–0.61) |
| Racial background | ||||||||||||
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Nonwhite | 0.82 (0.64–1.04) | 0.90 (0.72–1.10) | 1.34 (1.13–1.57) | 1.08 (0.90–1.28) | 0.95 (0.68–1.29) | 0.81 (0.68–0.94) | 0.83 (0.55–1.19) | 0.81 (0.56–1.12) | 0.81 (0.73–0.88) | 0.88 (0.68–1.11) | 0.95 (0.72–1.21) | 0.93 (0.63–1.33) |
| Education | ||||||||||||
| Secondary school or less | 0.87 (0.77–0.97) | 0.86 (0.77–0.95) | 0.97 (0.88–1.07) | 0.95 (0.85–1.07) | 0.90 (0.75–1.07) | 0.90 (0.84–0.98) | 0.96 (0.79–1.15) | 0.96 (0.81–1.13) | 0.87 (0.83–0.91) | 0.96 (0.84–1.09) | 0.73 (0.66–0.85) | 0.87 (0.71–1.05) |
| Some postsecondary education | 1.01 (0.75–1.15) | 1.09 (0.96–1.23) | 1.05 (0.93–1.18) | 1.02 (0.89–1.16) | 1.14 (0.93–1.38) | 1.01 (0.92–1.10) | 1.20 (0.97–1.47) | 1.01 (0.81–1.23) | 0.97 (0.92–1.01) | 0.89 (0.75–1.04) | 1.01 (0.85–1.18) | 1.12 (0.88–1.40) |
| Postsecondary degree or diploma | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Household income, $ | ||||||||||||
| < 50000 | 1.22 (1.08–1.38) | 1.04 (0.93–1.16) | 1.08 (0.98–1.20) | 1.31 (1.17–1.47) | 1.40 (1.16–1.69) | 1.03 (0.95–1.12) | 1.12 (0.92–1.37) | 1.15 (0.96–1.38) | 0.91 (0.87–0.95) | 0.89 (0.77–1.02) | 1.06 (0.92–1.23) | 1.27 (1.03–1.56) |
| 50000–99999 | 1.04 (0.93–1.15) | 1.02 (0.94–1.12) | 0.99 (0.91–1.09) | 1.03 (0.94–1.14) | 1.10 (0.93–1.29) | 1.03 (0.96–1.10) | 0.96 (0.81–1.14) | 0.97 (0.83–1.12) | 0.99 (0.96–1.03) | 1.04 (0.93–1.16) | 0.97 (0.86–1.09) | 1.04 (0.87–1.24) |
| 100000–149999 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| ≥ 150000 | 1.05 (0.93–1.19) | 1.04 (0.94–1.16) | 0.86 (0.77–0.96) | 0.84 (0.76–0.93) | 1.10 (0.92–1.32) | 0.96 (0.88–1.04) | 0.95 (0.78–1.15) | 0.83 (0.69–0.98) | 1.01 (0.97–1.05) | 1.08 (0.96–1.22) | 0.99 (0.87–1.13) | 0.98 (0.80–1.20) |
| Region | ||||||||||||
| Atlantic | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Quebec | 1.01 (0.89–1.14) | 1.52 (1.37–1.69) | 0.84 (0.76–0.94) | 1.02 (0.90–1.16) | 0.47 (0.37–0.60) | 0.53 (0.48–0.58) | 0.37 (0.28–0.48) | 1.31 (1.07–1.59) | 0.81 (0.77–0.85) | 0.58 (0.49–0.67) | 0.90 (0.76–1.06) | 2.15 (1.74–2.67) |
| Ontario | 1.07 (0.95–1.19) | 1.08 (0.97–1.21) | 0.91 (0.83–1.01) | 1.29 (1.14–1.45) | 1.34 (1.13–1.60) | 1.19 (1.11–1.28) | 1.25 (1.04–1.50) | 1.50 (1.25–1.80) | 1.20 (1.15–1.24) | 1.15 (1.02–1.30) | 1.39 (1.21–1.60) | 1.44 (1.15–1.81) |
| Prairies | 0.96 (0.85–1.08) | 1.16 (1.04–1.30) | 0.88 (0.79–0.97) | 1.50 (1.34–1.68) | 1.19 (0.99–1.42) | 0.70 (0.64–0.76) | 1.11 (0.92–1.34) | 1.40 (1.16–1.69) | 1.15 (1.11–1.20) | 1.08 (0.95–1.22) | 1.32 (1.14–1.52) | 1.47 (1.17–1.84) |
| British Columbia | 1.13 (1.01–1.27) | 1.09 (0.97–1.22) | 0.83 (0.75–0.92) | 1.44 (1.28–1.62) | 1.41 (1.18–1.69) | 1.03 (0.96–1.11) | 1.10 (0.91–1.33) | 1.54 (1.28–1.87) | 1.10 (1.06–1.15) | 1.15 (1.01–1.31) | 1.28 (1.11–1.49) | 1.50 (1.20–1.88) |
| Marital status | ||||||||||||
| Single (never married or never lived with partner) | 1.18 (1.03–1.34) | 0.85 (0.75–0.97) | 0.94 (0.83–1.07) | 0.95 (0.84–1.08) | 1.06 (0.85–1.30) | 1.06 (0.96–1.16) | 1.27 (1.02–1.57) | 0.81 (0.65–1.00) | 0.89 (0.84–0.94) | 0.72 (0.60–0.86) | 0.82 (0.69–0.98) | 0.99 (0.79–1.22) |
| Married or common-law | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Widowed | 1.06 (0.92–1.22) | 0.82 (0.71–0.93) | 1.01 (0.90–1.14) | 0.86 (0.71–1.03) | 0.98 (0.76–1.25) | 0.95 (0.86–1.06) | 0.93 (0.73–1.19) | 0.67 (0.51–0.85) | 1.00 (0.96–1.05) | 0.61 (0.49–0.74) | 0.85 (0.71–1.03) | 0.93 (0.71–1.19) |
| Divorced or separated | 1.15 (1.02–1.29) | 0.81 (0.72–0.91) | 1.00 (0.90–1.11) | 1.12 (1.01–1.24) | 1.35 (1.13–1.59) | 1.08 (0.99–1.16) | 1.13 (0.92–1.37) | 0.91 (0.76–1.09) | 1.04 (1.00–1.08) | 0.80 (0.69–0.96) | 0.91 (0.78–1.05) | 1.00 (0.81–1.21) |
| Essential worker status | ||||||||||||
| Does not work outside the home | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Essential worker | 0.95 (0.83–1.07) | 1.08 (0.97–1.20) | 1.00 (0.89–1.12) | 1.61 (1.43–1.80) | 1.01 (0.85–1.20) | 0.92 (0.85–1.00) | 1.01 (0.83–1.23) | 1.19 (1.00–1.40) | 0.93 (0.88–0.97) | 1.04 (0.92–1.18) | 1.02 (0.89–1.17) | 1.25 (1.03–1.51) |
| Not essential worker | 0.89 (0.80–1.00) | 1.00 (0.90–1.10) | 0.94 (0.85–1.04) | 3.04 (2.78–3.32) | 0.79 (0.67–0.94) | 0.88 (0.82–0.95) | 0.86 (0.72–1.04) | 1.12 (0.96–1.31) | 0.98 (0.94–1.02) | 1.11 (0.99–1.24) | 1.03 (0.90–1.16) | 1.10 (0.92–1.31) |
| Urban or rural status | ||||||||||||
| Urban | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural | 1.02 (0.93–1.12) | 0.92 (0.85–1.01) | 1.03 (0.95–1.12) | 1.03 (0.94–1.13) | 0.97 (0.83–1.13) | 1.01 (0.95–1.08) | 1.05 (0.89–1.22) | 1.00 (0.87–1.16) | 0.96 (0.93–1.00) | 0.98 (0.89–1.09) | 1.02 (0.91–1.14) | 1.02 (0.87–1.20) |
Note: CI = confidence interval, PR = prevalence ratio.
Adjusted for all other variables listed in the table (sex, age group, racial background, education, household income, region, marital status, essential worker status and urban or rural status).
The adjusted prevalence ratios for the association between each socioeconomic variable and the number of stressors are presented in Table 3. Adults aged 65 years and older (v. those aged 50–64 yr), those who resided in Quebec (v. those in the Atlantic) and those who had a secondary school education or less (v. those with a postsecondary degree or diploma) reported fewer stressors. Participants who resided in Ontario and BC reported more stressors than those in the Atlantic provinces. Unadjusted results were very similar to the adjusted results and can be found in Appendix 1, Supplemental Table A3.
Table 3:
Adjusted associations between socioeconomic characteristics and total number of stressors* among participants (n = 21 605) of the Canadian Longitudinal Study on Aging (CLSA) at the time of the CLSA COVID-19 Questionnaire exit survey (September–December 2020)
| Characteristic | Adjusted PR (95% CI)† |
|---|---|
| Sex | |
| Male | 1.00 |
| Female | 1.20 (1.17–1.23) |
| Age group, yr | |
| 50–64 | 1.00 |
| 65–74 | 0.86 (0.84–0.89) |
| 75–96 | 0.70 (0.67–0.73) |
| Racial background | |
| White | 1.00 |
| Nonwhite | 0.91 (0.85–0.98) |
| Education | |
| Secondary school graduation or less | 0.89 (0.86–0.92) |
| Some postsecondary education | 0.99 (0.95–1.04) |
| Postsecondary degree or diploma | 1.00 |
| Household income, $ | |
| < 50000 | 1.04 (1.00–1.08) |
| 50 000–99 999 | 1.01 (0.98–1.05) |
| 100 000–149 999 | 1.00 |
| ≥ 150000 | 0.99 (0.95–1.02) |
| Region | |
| Atlantic | 1.00 |
| Quebec | 0.86 (0.82–0.89) |
| Ontario | 1.17 (1.13–1.22) |
| Prairies | 1.07 (1.03–1.11) |
| British Columbia | 1.12 (1.07–1.16) |
| Marital status | |
| Single (never married or never lived with partner) | 0.94 (0.90–0.98) |
| Married or common-law relationship | 1.00 |
| Widowed | 0.92 (0.88–0.97) |
| Divorced or separated | 1.02 (0.98–1.06) |
| Essential worker status | |
| Does not work outside the home | 1.00 |
| Essential worker | 1.02 (0.98–1.06) |
| Not essential worker | 1.08 (1.05–1.12) |
| Urban or rural status | |
| Urban | 1.00 |
| Rural | 0.99 (0.96–1.02) |
Note: CI = confidence interval, PR = prevalence ratio.
The total number of stressors was calculated by summing reported stressors (range 0–12).
Adjusted for all other variables listed in the table: sex, age group, racial background, education, household income, region, marital status, essential worker status and urban or rural status.
Perceived consequences of the COVID-19 pandemic
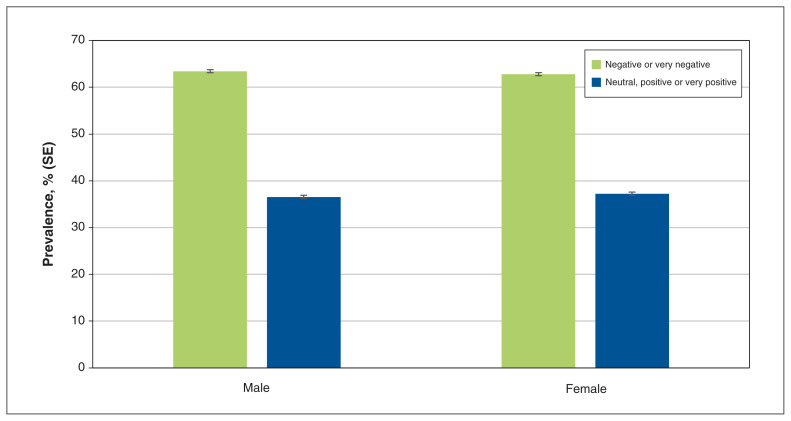
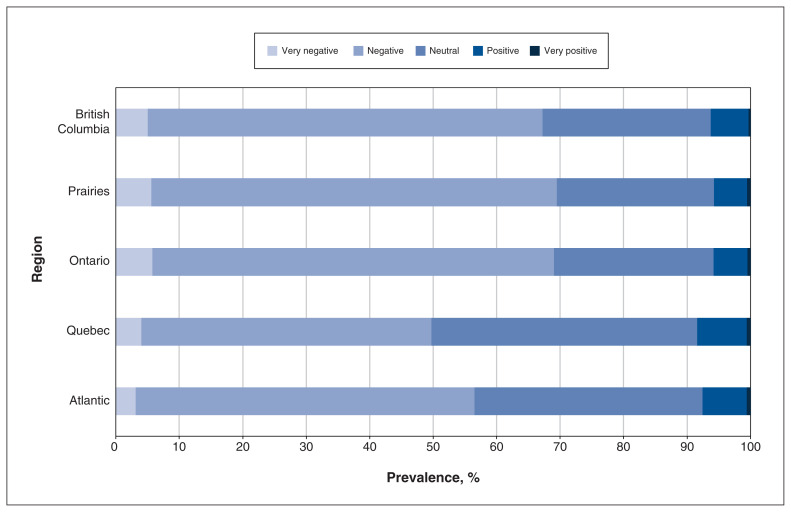
Almost two-thirds (n = 14 520, 63.1%) of the sample (n = 23 020) perceived the consequences of the pandemic as negative or very negative when surveyed between September and December 2020 (Figure 3). The distribution of the self-reported consequences of the COVID-19 pandemic by socioeconomic variables is presented in Appendix 1, Supplemental Table A4. Perceptions of the pandemic’s consequences varied across Canada, with the greatest proportion of participants perceiving consequences as negative or very negative in BC, Ontario and the Prairies (Figure 4). Several socioeconomic characteristics were associated with perceiving the consequences of the COVID-19 pandemic as negative or very negative (Table 4). Adults aged 75–96 years (v. those aged 50–64 yr), nonwhite adults (v. white) and those who resided in a rural setting (v. urban setting) were less likely to perceive the pandemic as negative or very negative. Unadjusted results can be found in Appendix 1, Supplemental Table A5.
Figure 3:
Perceived consequences of the COVID-19 pandemic experienced by participants of the Canadian Longitudinal Study on Aging (CLSA) (n = 23 020), by sex, at the time of the CLSA COVID-19 Questionnaire exit survey (September–December 2020), with standard error (SE) bars.
Figure 4:
Perceived consequences of the COVID-19 pandemic experienced by participants (n = 23 020) of the Canadian Longitudinal Study on Aging (CLSA) at the time of the CLSA COVID-19 Questionnaire exit survey (September–December 2020), by region.
Table 4:
Adjusted associations between socioeconomic characteristics and perception of the consequences of the COVID-19 pandemic among participants (n = 20 982) of the Canadian Longitudinal Study on Aging (CLSA) at the time of the CLSA COVID-19 Questionnaire exit survey (September–December 2020)
| Characteristic | Adjusted PR (95% CI)* |
|---|---|
| Sex | |
| Male | 1.00 |
| Female | 0.98 (0.97–1.01) |
| Age group, yr | |
| 50–64 | 1.00 |
| 65–74 | 0.98 (0.95–1.00) |
| 75–96 | 0.93 (0.90–0.95) |
| Racial background | |
| White | 1.00 |
| Nonwhite | 0.89 (0.83–0.95) |
| Education | |
| Secondary school graduation or less | 0.90 (0.87–0.93) |
| Some postsecondary education | 0.97 (0.93–1.01) |
| Postsecondary degree or diploma | 1.00 |
| Household income, $ | |
| < 50000 | 0.94 (0.91–0.97) |
| 50 000–99 999 | 0.98 (0.96–1.01) |
| 100 000–149 999 | 1.00 |
| ≥ 150000 | 0.99 (0.96–1.03) |
| Region | |
| Atlantic | 1.00 |
| Quebec | 0.87 (0.84–0.91) |
| Ontario | 1.20 (1.16–1.24) |
| Prairies | 1.21 (1.17–1.25) |
| British Columbia | 1.17 (1.13–1.21) |
| Marital status | |
| Single (never married or never lived with partner) | 0.99 (0.95–1.03) |
| Married or common-law relationship | 1.00 |
| Widowed | 1.04 (1.00–1.08) |
| Divorced or separated | 1.02 (0.99–1.05) |
| Essential worker status | |
| Does not work outside the home | 1.00 |
| Essential worker | 0.92 (0.89–0.95) |
| Not essential worker | 0.96 (0.93–0.99) |
| Urban or rural status | |
| Urban | 1.00 |
| Rural | 0.93 (0.90–0.96) |
Note: CI = confidence interval, PR = prevalence ratio.
Adjusted for all other variables listed in the table: sex, age group, racial background, education, household income, region, marital status, essential worker status and urban or rural status.
Interpretation
In this study, we describe the stressors and perceptions of the consequences experienced by older adults during the COVID-19 pandemic at a national level. Many studies have focused on the perception of the threat of the pandemic,25,28,29 and not broadly on how people would describe their perception of the consequences of the COVID-19 pandemic on their household. Our findings suggest that participants aged 50–96 years in Canada have been affected substantially by the consequences of the pandemic, with 75.7% of respondents experiencing at least 1 stressor and 63.1% reporting they perceived the consequences of the pandemic as negative or very negative. Conversely, about 6.7% of participants perceived the pandemic as positive or very positive, and about 24.3% reported experiencing no stressors. The prevalence of stressors and perceptions of consequences of the pandemic varied by socioeconomic factors, with adults aged 50–64 years and females more likely to experience most of the stressors.
Few Canadian studies have described stress during the pandemic. A national online survey of 2000 adults early in the pandemic found that 45% of adults agreed the pandemic was stressful and, consistent with our study results, participants in Ontario were more likely to report stress than those in other regions.25 The variation in the perception of the consequences of the pandemic may be related to different public health responses and preventive measures that were implemented by different provinces.30 A study conducted in the US found that people reported experiencing a high number of stressors during the pandemic,15 and the most commonly reported stressors were reading or hearing others talk about the severity and contagiousness of COVID-19 (96.6%) and uncertainty regarding requirements for quarantine and social distancing (88.3%). Although these specific stressors were different than what we measured, the overall report of increases in stress related to changes in daily routines is consistent.
Strengths of our study included that the CLSA is a nationally generalizable sample with a population-based sampling strategy. Surveys were collected by both phone and web to accommodate participants with limited internet access. Further, the longitudinal data, with extensive prepandemic data collected at CLSA baseline (2011–2015) and the first follow-up (2015–2018), allowed for a comprehensive assessment of sociodemographic factors. Future waves of data collected by the CLSA20 will allow for longitudinal research on how the experiences of stress during the pandemic affect both short- and long-term health outcomes. The CLSA COVID-19 Questionnaire Study collected in-depth information on stressors and perceptions of consequences during the pandemic in a large sample of older adults in Canada.
Limitations
The CLSA COVID-19 Questionnaire Study did not include a scale for perceived stress. Furthermore, the stressor list was developed early in the pandemic and may not include all possible stressors (e.g., loss of job, inability to attend community centres or places of worship) that may have been experienced. Although the outcome measures have been widely used to assess objective and subjective reactions to stressful events in previous disaster research7,8,21,22 and were modified from gold-standard measurement tools,7 they have not yet been validated in the current CLSA sample. Further, study participants were primarily white and were limited to community-dwelling adults at baseline. Only a small proportion of participants moved into long-term care for subsequent follow-up by CLSA surveys. This may potentially introduce a selection bias, with results that are not representative of all Canadian adults 50 years of age and older. Data from this study were collected in the first 2 waves of the pandemic in Canada, with the stress measures collected from September to December 2020, before the general population was eligible for vaccination. After December 2020, Canada had subsequent waves of the pandemic.31 The results from this study may vary from the experiences of stressors or the overall perception of the pandemic during subsequent waves or when people were eligible to be vaccinated, as this may have affected the stress experienced by Canadians.
Conclusion
Understanding the indirect impact of the pandemic on Canadian adults is critical. Stress is one indirect factor that may have a profound effect on the long-term health consequences of Canadians. Both acute and chronic stress are established risk factors for mental health, chronic diseases and death. Describing the prevalence of stressors by socioeconomic factors is crucial to identify health inequalities and to prevent further disparities. As the pandemic continues to progress, and as future follow-ups of the CLSA are collected and become available, continued investigation of the impact of stress during the pandemic on long-term health outcomes will be possible.
Supplementary Material
Acknowledgements
This research was made possible using the data/biospecimens collected by the Canadian Longitudinal Study on Aging (CLSA). Funding for the CLSA is provided by the Government of Canada through the Canadian Institutes of Health Research (CIHR) under grant reference LSA 94473 and the Canada Foundation for Innovation, as well as the following provinces: Newfoundland, Nova Scotia, Quebec, Ontario, Manitoba, Alberta and British Columbia. This research has been conducted using the CLSA (Baseline Tracking Dataset version 3.7, Baseline Comprehensive Dataset version 5.1, Follow-up 1 Tracking Dataset version 2.2, Follow-up 1 Comprehensive Dataset version 3.0, COVID-19 questionnaire data) under Application 21CON001. The CLSA is led by Drs. Parminder Raina, Christina Wolfson and Susan Kirkland.
Footnotes
Competing interests: Laura Anderson reports grants from the Canadian Institutes of Health Research, the Cancer Research Society and the Canadian Cancer Society. Lauren Griffith is supported by the McLaughlin Foundation Professorship in Population and Public Health. Parminder Raina holds the Raymond and Margaret Labarge Chair in Research and Knowledge Application for Optimal Aging, is the Scientific Director of the McMaster Institute for Research on Aging and the Labarge Centre for Mobility in Aging and holds a Tier 1 Canada Research Chair in Geroscience.
This article has been peer reviewed.
Canadian Longitudinal Study on Aging Team: Andrew Costa and Cynthia Balion (McMaster University); Yukiko Asada (Dalhousie University); Benoît Cossette and Melanie Levasseur (University of Sherbrooke); Scott Hofer and Theone Paterson (University of Victoria); David Hogan and Jacqueline McMillan (University of Calgary); Teresa Liu-Ambrose (University of British Columbia); Verena Menec and Philip St. John (University of Manitoba); Gerald Mugford and Zhiwei Gao (Memorial University of Newfoundland); Vanessa Taler and Patrick Davidson (University of Ottawa); Andrew Wister and Theodore Cosco (Simon Fraser University)
Contributors: Vanessa De Rubeis, Laura Anderson, Margaret de Groh, Ying Jiang, Nicole Basta, Susan Kirkland, Christina Wolfson, Lauren Griffith and Parminder Raina conceived and designed the study. Vanessa De Rubeis, Laura Anderson, Jayati Khattar and Urun Erbas Oz analyzed and interpreted the data. Vanessa De Rubeis and Laura Anderson drafted the manuscript. All of the authors revised it critically for important intellectual content, gave final approval of the version to be published and agreed to be accountable for all aspects of the work. The members of the Canadian Longitudinal Study on Aging team have contributed to the collection of the data across Canada.
Funding: Funding for this study was obtained from the Public Health Agency of Canada (PHAC). Funding for the support of the CLSA COVID-19 Questionnaire Study is provided by the Juravinski Research Institute, Faculty of Health Sciences, McMaster University, the Provost Fund from McMaster University, the McMaster Institute for Research on Aging, the PHAC and the Nova Scotia COVID-19 Health Research Coalition.
Data sharing: Data are available from the Canadian Longitudinal Study on Aging (www.clsa-elcv.ca) for researchers who meet the criteria for access to de-identified CLSA data.
Disclaimer: The opinions expressed in this manuscript are the author’s own and do not reflect the views of the Canadian Longitudinal Study on Aging.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/10/3/E721/suppl/DC1.
References
- 1.Tran BX, Nguyen HT, Le HT, et al. Impact of COVID-19 on economic well-being and quality of life of the Vietnamese during the national social distancing. Front Psychol. 2020;11:565153. doi: 10.3389/fpsyg.2020.565153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bridgland VME, Moeck EK, Green DM, et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS One. 2021;16:e0240146. doi: 10.1371/journal.pone.0240146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gasteiger N, Vedhara K, Massey A, et al. Depression, anxiety and stress during the COVID-19 pandemic: results from a New Zealand cohort study on mental well-being. BMJ Open. 2021;11:e045325. doi: 10.1136/bmjopen-2020-045325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mattioli AV, Puviani MB, Nasi M, et al. COVID-19 pandemic: the effects of quarantine on cardiovascular risk. Eur J Clin Nutr. 2020;74:852–5. doi: 10.1038/s41430-020-0646-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mattioli AV, Nasi M, Cocchi C, et al. COVID-19 outbreak: impact of the quarantine-induced stress on cardiovascular disease risk burden. Future Cardiol. 2020;16:539–42. doi: 10.2217/fca-2020-0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.King S, Laplante DP. The effects of prenatal maternal stress on children’s cognitive development: Project Ice Storm. Stress. 2005;8:35–45. doi: 10.1080/10253890500108391. [DOI] [PubMed] [Google Scholar]
- 8.Cao-Lei L, Elgbeili G, Massart R, et al. Pregnant women’s cognitive appraisal of a natural disaster affects DNA methylation in their children 13 years later: Project Ice Storm. Transl Psychiatry. 2015;5:e515. doi: 10.1038/tp.2015.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lock S, Rubin GJ, Murray V, et al. Secondary stressors and extreme events and disasters: a systematic review of primary research from 2010–2011. PLoS Curr. 2012;4 doi: 10.1371/currents.dis.a9b76fed1b2dd5c5bfcfc13c87a2f24f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984. pp. 1–460. [Google Scholar]
- 11.De Rubeis V, Lee J, Anwer MS, et al. Impact of disasters, including pandemics, on cardiometabolic outcomes across the life-course: a systematic review. BMJ Open. 2021;11:e047152. doi: 10.1136/bmjopen-2020-047152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clemmensen C, Petersen MB, Sørensen TIA. Will the COVID-19 pandemic worsen the obesity epidemic? Nat Rev Endocrinol. 2020;16:469–70. doi: 10.1038/s41574-020-0387-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen S, Kessler RC, Gordon LU. Measuring stress: a guide for health and social scientists. Oxford (UK): Oxford University Press; 1997. pp. 1–256. [Google Scholar]
- 14.Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park CL, Russell BS, Fendrich M, et al. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020;35:2296–303. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vahia IV, Jeste DV, Reynolds CF., III Older adults and the mental health effects of COVID-19. JAMA. 2020;324:2253–4. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- 18.Salleh MR. Life event, stress and illness. Malays J Med Sci. 2008;15:9–18. [PMC free article] [PubMed] [Google Scholar]
- 19.Nurius PS, Green S, Logan-Greene P, et al. Life course pathways of adverse childhood experiences toward adult psychological well-being: a stress process analysis. Child Abuse Negl. 2015;45:143–53. doi: 10.1016/j.chiabu.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raina P, Wolfson C, Kirkland S, et al. Cohort profile: the Canadian Longitudinal Study on Aging (CLSA) Int J Epidemiol. 2019;48:1752–3j. doi: 10.1093/ije/dyz173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laplante DP, Brunet A, Schmitz N, et al. Project Ice Storm: prenatal maternal stress affects cognitive and linguistic functioning in 5 1/2-year-old children. J Am Acad Child Adolesc Psychiatry. 2008;47:1063–72. doi: 10.1097/CHI.0b013e31817eec80. [DOI] [PubMed] [Google Scholar]
- 22.Dancause KN, Laplante DP, Fraser S, et al. Prenatal exposure to a natural disaster increases risk for obesity in 51/2-year-old children. Pediatr Res. 2012;71:126–31. doi: 10.1038/pr.2011.18. [DOI] [PubMed] [Google Scholar]
- 23.Paquin V, Elgbeili G, Laplante DP, et al. Positive cognitive appraisal “buffers” the long-term effect of peritraumatic distress on maternal anxiety: the Queensland Flood Study. J Affect Disord. 2021;278:5–12. doi: 10.1016/j.jad.2020.09.041. [DOI] [PubMed] [Google Scholar]
- 24.Kowal M, Coll-Martín T, Ikizer G, et al. Who is the most stressed during the COVID-19 pandemic? Data from 26 countries and areas. Appl Psychol Health Well-Being. 2020;12:946–66. doi: 10.1111/aphw.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parsons Leigh J, Fiest K, Brundin-Mather R, et al. A national cross-sectional survey of public perceptions of the COVID-19 pandemic: self-reported beliefs, knowledge, and behaviors. PLoS One. 2020;15:e0241259. doi: 10.1371/journal.pone.0241259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menec VH, Newall NE, Mackenzie CS, et al. Examining individual and geographic factors associated with social isolation and loneliness using Canadian Longitudinal Study on Aging (CLSA) data. PLoS One. 2019;14:e0211143. doi: 10.1371/journal.pone.0211143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Raina P, Wolfson C, Griffith LE, et al. A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nat Aging. 2021;1:1137–47. doi: 10.1038/s43587-021-00128-1. [DOI] [PubMed] [Google Scholar]
- 28.Jaber RM, Mafrachi B, Al-Ani A, et al. Awareness and perception of COVID-19 among the general population: a Middle Eastern survey. PLoS One. 2021;16:e0250461. doi: 10.1371/journal.pone.0250461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Attema AE, L’Haridon O, Raude J, et al. Beliefs and risk perceptions about COVID-19: evidence from two successive French representative surveys during lockdown. Front Psychol. 2021;12:619145. doi: 10.3389/fpsyg.2021.619145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hale T, Angrist N, Goldszmidt R, et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nat Hum Behav. 2021;5:529–38. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- 31.COVID-19 daily epidemiology update. Ottawa: Public Health Agency of Canada; [accessed 2021 July 27]. modified 2022 June 10. Available: https://health-infobase.canada.ca/covid-19/epidemiological-summary-covid-19-cases.html#a4. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.