Abstract
Background:
Although suturing is an essential competency for medical students, there has been limited research into the skills acquisition process over the course of medical school curriculum. This study aimed to determine whether suturing ability improved over the course of clerkship and whether an interest in a surgical discipline was associated with improved skill acquisition.
Methods:
The suturing ability of third-year medical students at a large Canadian medical school was assessed at the beginning of clerkship (August 2018) as well as before and after their surgery rotation by 2 expert reviewers using a validated, objective scoring system as well as a qualitative assessment, both in person and via blinded video recordings. Students were randomly allocated to 4 groups for their clerkship year by the medical school.
Results:
Of 133 eligible students, 115 (86.5%) completed the study. Median suturing assessment scores improved significantly after the surgery rotation (214.5 [interquartile range (IQR) 191.1–235.0] v. 238.0 [IQR 223.5–255.0], p = 0.001). Groups that had completed a procedural rotation (emergency medicine, obstetrics and gynecology) between clerkship and starting their surgery rotation had improved scores between these time points (p < 0.05), whereas scores decreased for groups that did not have a procedural rotation between assessments. Regardless of previous rotations, suturing scores were similar between groups after the surgery rotation. The 21 students (18.3%) who were interested in a surgical discipline had higher suturing scores than students who were not interested in surgery at the beginning of clerkship (229.1 [IQR 220.2–253.0] v. 208.0 [IQR 185.0–228.0], p < 0.001) and after the surgery rotation (252.0 [IQR 227.0–268.0] v. 235.8 [IQR 220.5–251.2], p = 0.02).
Conclusion:
Medical students’ suturing ability improved during the surgery rotation but was also influenced by other procedural rotations and students’ interest in procedure specialties. Skill acquisition by medical students is complex and requires additional investigation.
Abstract
Contexte:
Bien que les sutures soient une compétence essentielle pour les étudiants en médecine, peu d’études ont été menées sur le processus d’acquisition de cette compétence dans le cadre du programme d’études en médecine. Cette étude visait à déterminer s’il y avait amélioration de la compétence en réalisation de sutures des étudiants en médecine au fil du stage clinique et si un intérêt pour les disciplines chirurgicales était associé à l’acquisition de la compétence.
Méthodes:
La compétence en réalisation de sutures d’étudiants de troisième année de médecine d’une grande faculté de médecine canadienne a été évaluée au début de leur stage clinique (août 2018) ainsi qu’avant et après leur stage de chirurgie par 2 évaluateurs experts utilisant un système de notation objectif validé et effectuant une évaluation qualitative, en personne et par enregistrement vidéo en aveugle. Les étudiants ont été répartis aléatoirement par la faculté de médecine en quatre groupes pour leur année de stages.
Résultats:
Des 133 étudiants admissibles, 115 (86,5 %) ont terminé l’étude. Le résultat médian à l’évaluation des sutures a augmenté de façon significative après le stage de chirurgie (214,5, écart interquartile [ÉI] 191,1 à 235,0; c. 238,0, ÉI 223,5 à 255,0; p = 0,001). Les groupes qui avaient effectué un stage en médecine d’urgence ou en obstétrique et gynécologie entre leur stage clinique et le début de leur stage de chirurgie ont réussi à améliorer leur résultat dans l’intervalle (p < 0,05), alors qu’on a observé une baisse des scores dans les groupes qui n’ont pas eu ce type de stage entre les 2 évaluations. Cela dit, après le stage de chirurgie, les résultats des groupes étaient similaires, quels que soient les stages précédents. Les 21 étudiants (18,3 %) qui envisageaient de se spécialiser en chirurgie ont obtenu des scores supérieurs aux étudiants qui n’avaient pas manifesté d’intérêt pour cette discipline, tant au début du stage clinique (229,1 [ÉI 220,2 à 253,0] c. 208,0 [ÉI 185,0 à 228,0]; p < 0,001) qu’après le stage de chirurgie (252,0 [ÉI 227,0 à 268,0] c. 235,8 [ÉI 220,5 à 251,2]; p = 0,02).
Conclusion:
La compétence des étudiants en médecine en réalisation de sutures s’est améliorée durant leur stage de chirurgie, mais elle est aussi influencée par d’autres stages pratiques et par l’intérêt des étudiants pour les disciplines de médecine chirurgicale. L’acquisition de compétences par les étudiants en médecine est un processus complexe qui doit être étudié davantage.
There is a growing movement toward competency-based medical education, including in technical skills, at all levels of training. This includes undergraduate medical education, where several skills have been identified as essential to the graduating medical student. Suturing is considered a core skill in which each graduating medical student should have achieved competence.1 Medical students frequently cite technical skills training as inadequate and report being anxious regarding their competency in this area.2,3
Despite the importance of medical students’ suturing ability, there is limited research into how a medical student becomes competent in suturing or obtains technical skills in general. Although both preceptors and students acknowledge formal evaluation of the ability to suture as very important, most students do not undergo it.4 The surgery rotation is commonly regarded as an ideal rotation for students to learn these skills, although other rotations such as emergency medicine and obstetrics and gynecology also involve suturing and technical skills. There are several factors that may affect a student’s ability to obtain technical experience during the surgical rotation, including the number of other learners, the student’s interest in technical procedures, and the specific surgical team they are assigned to.
The purpose of this study was to determine whether medical students’ suturing assessment scores improved over the course of clerkship and whether interest in a surgical discipline correlated with improved skill acquisition. We hypothesized that suturing ability would vary throughout the year and would improve over the course of the surgery rotation. Furthermore, we hypothesized that rotations other than surgery might affect suturing ability as well as a student’s interest in a surgical discipline.
Methods
Setting
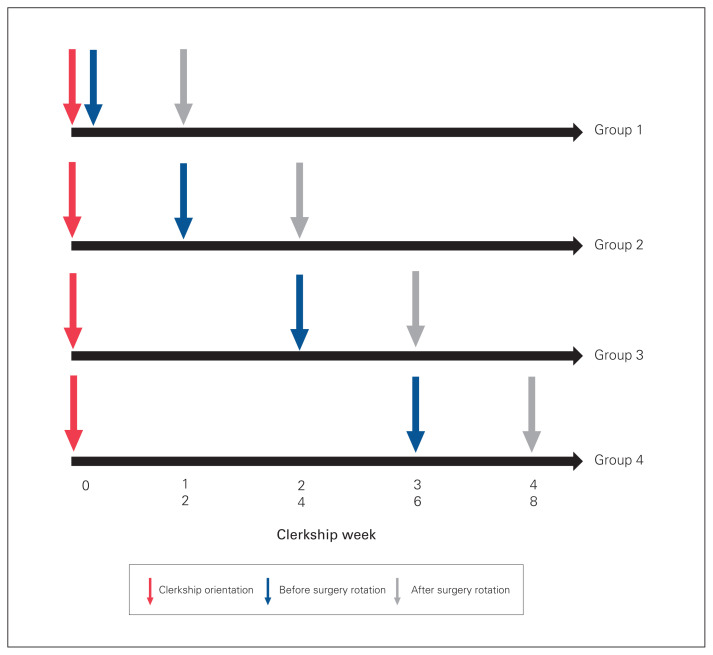
This study was performed at the Schulich School of Medicine & Dentistry, Western University, London, Ontario, Canada, during 1 complete academic year (August 2018–August 2019). Our medical school is affiliated with the London Health Sciences Centre, a tertiary academic health sciences centre with a catchment population of about 2 million and a full complement of subspecialty training programs. Students complete core rotations in internal medicine (including emergency medicine) (12 wk), surgery (12 wk), obstetrics and gynecology (6 wk), family medicine (6 wk), psychiatry (6 wk) and pediatrics (6 wk), at least 1 of which must include 4 weeks in a community setting. The clerkship group is split into 4 blocks, each of which completes a different rotation order (Figure 1). The study protocol was approved by the Western University Health Sciences Research Ethics Board and the Lawson Health Research Institute (HSREB #111997).
Fig. 1.
Assessment time points for the 4 groups.
Participants
All third-year medical students were invited to participate in the study during their general clerkship orientation at the start of their clerkship year. Dedicated didactic and hands-on suturing teaching occurred only during this general clerkship orientation, in late August 2018. The initial suturing assessment was also completed during this orientation. Suturing kits containing instruments and sutures could be purchased by students if desired.
Students were randomly allocated to 4 groups for their clerkship year by the medical school, labelled in this study as groups 1–4 according to chronological order. There were no control groups.
Outcome
Suturing skill was assessed on the first day and the last day of the surgery rotation by 2 reviewers (staff surgeons [A.B., S.J.] or senior surgical residents [E.W., R.R.-E., N.C.]), both in person and via blinded video recording. The reviewers used an objective, validated suturing score that includes 11 key technique points, a qualitative assessment of ability to suture and a time component.5 Time was measured with hand-held electronic timers, and time scores were derived by subtracting the time used from the maximum allotted time of 5 minutes, then subtracting 10 points for each error (from a maximum of 8 errors). Participants were given clear instructions regarding expectations before beginning the session.
Statistical analysis
We used descriptive statistics to characterize the students across demographic and clerkship variables. We used the χ2 test and Fisher exact test to analyze categoric variables, and the Kruskal–Wallis test to compare continuous variables between students interested and not interested in surgery. When analyzing differences in suturing score overall and at each time point for each clerkship rotation group, we completed repeated-measure analysis of variance using generalized linear models with the Tukey post hoc test. Differences were considered statistically significantly if p < 0.05. We performed the analysis and all statistical tests using SAS software, version 9.4 (SAS Institute).
Results
Of 133 eligible students, 115 (86.5%) completed the study. The baseline characteristics of the students are presented in Table 1. Only 4 students (3.5%) stated they had sutured more than once or a few times.
Table 1.
Baseline characteristics of third-year medical students by interest in surgical specialty
| Characteristic | No. (%) of students* | p value | ||
|---|---|---|---|---|
| Overall n = 114† |
Interested in surgery n = 21 |
Not interested in surgery n = 93 |
||
| Age, median (IQR), yr | 24.0 (24.0–26.0) | 24.0 (24.0–26.0) | 24.0 (24.0–26.0) | 1.00 |
| Gender | 0.5 | |||
| Male | 62 (54.4) | 10 (47.6) | 52 (55.9) | |
| Female | 52 (45.6) | 11 (52.4) | 41 (44.1) | |
| Handedness | 0.4 | |||
| Right | 104 (91.2) | 18 (85.7) | 86 (92.5) | |
| Left | 10 (8.8) | 3 (14.3) | 7 (7.5) | |
| Other technical skill (e.g., piano, guitar) | 0.002 | |||
| Yes | 39 (34.2) | 13 (61.9) | 26 (28.0) | |
| No | 74 (64.9) | 7 (33.3) | 67 (72.0) | |
| No response | 1 (0.9) | 1 (4.8) | 0 (0.0) | |
| Previous experience suturing | 1.00 | |||
| Yes | 99 (86.8) | 19 (90.5) | 80 (86.0) | |
| No | 14 (12.3) | 2 (9.5) | 12 (12.9) | |
| No response | 1 (0.9) | 0 (0.0) | 1 (1.1) | |
| Degree of previous suturing experience | 0.2 | |||
| Once/few times | 96 (84.2) | 17 (81.0) | 79 (84.9) | |
| Every month | 3 (2.6) | 1 (4.8) | 2 (2.2) | |
| Every week | 1 (0.9) | 1 (4.8) | 0 (0.0) | |
| No response | 14 (12.3) | 2 (9.5) | 12 (12.9) | |
| Owns suturing kit | 0.006 | |||
| Yes | 40 (35.1) | 13 (61.9) | 27 (29.0) | |
| No | 71 (62.3) | 8 (38.1) | 63 (67.7) | |
| No response | 3 (2.6) | 0 (0.0) | 3 (3.2) | |
IQR = interquartile range.
Except where noted otherwise.
One student did not provide answers to the questionnaire.
Twenty-one students (18.3%) were interested in a surgical discipline at the start of their clerkship year. There were no significant differences between these students and those not interested in surgery in age, gender, handedness or previous suturing experience. However, students interested in surgery were more likely than those not interested in surgery to have a previous technical skill (e.g., playing piano or guitar, 62% v. 28%, p = 0.002) and to own a suturing kit (62% v. 29%, p = 0.006).
There was good correlation in scores between in-person and video reviewers (Pearson r > 0.8 for all groups).
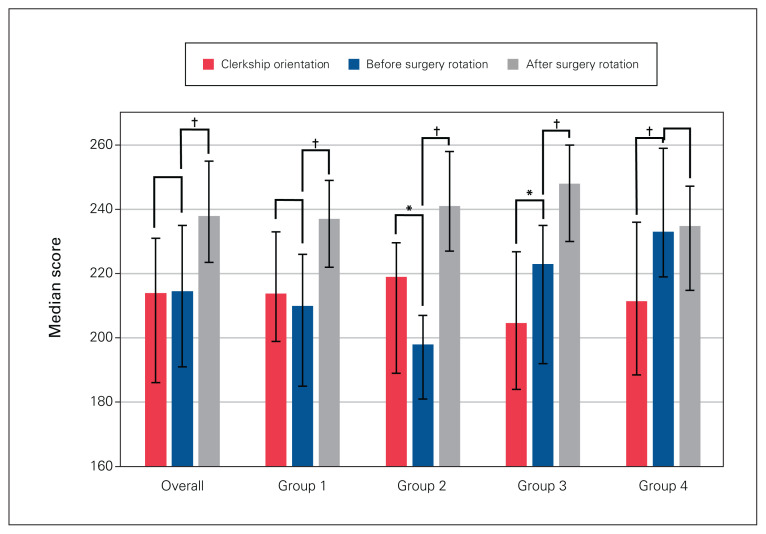
There was no change in median suturing scores between clerkship orientation and the first day of the surgery rotation (Figure 2). Median scores improved significantly after the rotation (214.5 [interquartile range (IQR) 191.1–235.0] before the rotation v. 238.0 [IQR 223.5–255.0] after the rotation, p = 0.001) (Table 2). For group 1, there were no differences in suturing scores between orientation and before the surgery rotation; scores improved significantly after the rotation (p < 0.001). For group 2, there was a significant decrease in scores between orientation and before the surgery rotation (p = 0.02), and a significant improvement in scores after the rotation (p < 0.001). For group 3, scores improved significantly between orientation and before the surgery rotation (p = 0.01) and after the rotation (p < 0.001). For group 4, scores improved significantly between orientation and before the surgery rotation (p < 0.001); there was no difference in scores between the start and end of the rotation.
Fig. 2.
Overall suturing scores and scores per block at clerkship orientation, and before and after the surgery rotation. *p < 0.05, †p < 0.001. Error bars represent interquartile ranges.
Table 2.
Suturing scores across clerkship blocks
| Time | Median suturing score (IQR) | p value | ||||
|---|---|---|---|---|---|---|
| Overall n = 115 |
Block 1 n = 33 |
Block 2 n = 29 |
Block 3 n = 25 |
Block 4 n = 28 |
||
| Orientation | 213.9 (186.1–231.0) | 213.8 (198.9–233.0) | 219.0 (189.0–229.6) | 204.7 (184.0–226.8) | 211.5 (188.5–236.0) | 0.4 |
| Before surgery rotation | 214.5 (191.0–235.0) | 210.0 (185.0–226.0) | 198.0 (181.0–207.0) | 223.0 (192.0–235.0) | 233.0 (219.0–259.0) | 0.001 |
| After surgery rotation | 238.0 (223.5–255.0) | 237.0 (222.0–249.0) | 241.0 (227.0–258.0) | 248.0 (230.0–260.0) | 234.8 (214.8–247.2) | 0.2 |
IQR = interquartile range.
There were no differences in suturing ability between groups at orientation (p = 0.4). Groups 1 and 2 had significantly lower median suturing scores than group 4 before the surgery rotation, and group 2 had lower median scores than group 3 before the rotation (p < 0.05). There were no significant between-group differences at the postrotation assessment (p = 0.2).
Students interested in a surgical career had higher median suturing scores than those not interested in surgery at orientation (p = 0.001) and after the surgery rotation (p = 0.02) but not before the rotation (p = 0.2) (Table 3).
Table 3.
Suturing ability of students interested in surgery versus those not interested in surgery
| Time; outcome | No. (%) of students* | p value | ||
|---|---|---|---|---|
| Overall n = 114 |
Interested in surgery n = 21 |
Not interested in surgery n = 93 |
||
| Orientation | ||||
| Median suturing score (IQR) | 213.9 (186.1–231.0) | 229.1 (220.2–253.0) | 208 (185.0–228.0) | 0.001 |
| Able to suture | 109 (95.6) | 21 (100.0) | 88 (94.6) | 0.6 |
| Before surgery rotation | ||||
| Median suturing score (IQR) | 214.5 (191.0–235.0) | 226.5 (195.5–251.0) | 214.0 (190.0–231.0) | 0.2 |
| Able to suture | 98 (89.1) | 20 (100.0) | 78 (86.7) | 0.1 |
| After surgery rotation | ||||
| Median suturing score (IQR) | 238.0 (223.5–255.0) | 252.0 (227.0–268.0) | 235.8 (220.5–251.2) | 0.02 |
| Able to suture | 95 (88.0) | 18 (94.7) | 77 (86.5) | 0.5 |
IQR = interquartile range.
Except where noted otherwise.
Discussion
Our study showed that completion of a 12-week surgery rotation led to improvements in suturing scores among third-year medical students. Interestingly, it appeared that students improved a similar amount after completing other rotations with technical instruction (i.e., emergency medicine, obstetrics and gynecology). Students interested in surgery performed better than those not interested in surgery at the beginning of clerkship as well as at the end of the surgery rotation. The latter improved a similar amount over the course of the rotation, although their final scores were still significantly below those of the students interested in surgery.
Several investigators have assessed suturing skill acquisition in a simulation environment.6–9 However, there is limited research into how medical students and other junior learners develop technical skills during their training.7 Although the simulation environment is an important location of learning, it does not replace learning in the clinical environment and does not provide the spaced-repetition model that has been shown to improve retention.10 In a study of German medical students, self-assessed suturing competence improved over the final 3 years of medical school; however, no objective measures were used.11 Cevik and Abu-Zidan12 found that students with suturing experience in the emergency department had significantly higher objective structured clinical examination scores than those who did not have suturing experience. These findings are in agreement with our study, which showed that increased clinical experience on procedural rotations such as surgery translated into improved suturing scores. Foote and colleagues13 reported that the surgery rotation provided the greatest entrustment of medical students with supervised procedures compared to other rotations during clerkship. Students had higher participation for subcuticular suturing during the surgery rotation than during the obstetrics and gynecology rotation. Those authors concluded that targeted areas for increased procedural involvement could be found within all specialties.13
Our group previously examined technical skill proficiency during clerkship.14 We found that the only skills that students felt confident performing independently were sterile technique and basic suturing. We also found that an interest in surgery and completion of procedural observerships before clerkship resulted in a higher likelihood that students would perform more advanced tasks, such as urethral catheterization, endotracheal intubation and injection of local anesthesia.14 These findings align with our current study, which showed that an interest in surgery and completion of other procedural rotations before the surgery rotation resulted in higher suturing scores by the end of the rotation. However, our previous study also identified barriers to the development of technical skill proficiency, such as lack of suitable cases, time constraints and failure to provide opportunities to students.14 It is important to recognize these barriers and attempt to minimize them so as to maximize medical students’ technical skills.
Limitations
The strengths of our study lie in its longitudinal assessment over the course of 1 year, as well as its large sample and high inclusion rate of third-year medical students completing clerkship. Although the assessment used was simple by design, we believe it can be extended to more complex suturing tasks. We deliberately chose this design since it was repeatable and applicable, and facilitated data collection for a large number of students in 1 setting. Furthermore, basic suturing skills are likely the most widely applicable skill for future physicians working in a variety of settings. The inclusion of additional time points of assessment during the year (i.e., after each rotation) and additional tasks would have provided further information regarding skill acquisition. Last, the clerkship experience is highly heterogeneous, with different levels of hands-on exposure for each student on each rotation. Although the assessment tool was chosen for these reasons, further investigation is needed into the skill acquisition process for more complex tasks, surgical or otherwise.
Although 86% of third-year medical students at our academic health sciences centre were assessed during their clerkship year, we were unable to assess the 33 students at our community satellite campus owing to logistical issues. It would have been interesting to compare suturing scores for these 2 groups at similar times. Since there are no residents at the satellite hospital, these students are usually first assist in the operating room, which may result in better suturing skills overall compared to our students at the academic hospitals. Future studies should aim to incorporate these students.
Conclusion
Medical students’ suturing ability improved during a 12-week surgery rotation as well as during other clerkship rotations with procedural components. The building of medical students’ technical skills is not the sole domain of surgeons, and skills training should be encouraged on all procedural rotations to build medical students’ competencies. The creation of a national set of objectives for technical skills training would enable standardization of teaching while possibly increasing opportunities for and decreasing barriers to skills development.
Footnotes
Competing interests: None declared.
Contributors: E. Walser designed the study. N. Carey, R. Ralph-Edwards, B. McNeely and S. Jones acquired the data, which J. Davidson and A. Bütter analysed. E. Walser, J. Davidson and R. Ralph-Edwards wrote the manuscript, which N. Carey, B. McNeely, S. Jones and A. Bütter critically revised. All authors gave final approval of the article to be published.
References
- 1.The Medical Schools Objectives Writing Group. Learning objectives for medical student education — guidelines for medical schools: report I of the Medical School Objectives Project. Acad Med 1999;74: 13–8. [DOI] [PubMed] [Google Scholar]
- 2.Rufai SR, Holland LC, Dimovska EOF, et al. A national survey of undergraduate suture and local anesthetic training in the United Kingdom. J Surg Educ 2016;73:181–4. [DOI] [PubMed] [Google Scholar]
- 3.Sarikaya O, Civaner M, Kalaca S. The anxieties of medical students related to clinical training. Int J Clin Pract 2006;60: 1414–8. [DOI] [PubMed] [Google Scholar]
- 4.Wu EH, Elnicki DM, Alper EJ, et al. Procedural and interpretive skills of medical students: experiences and attitudes of fourth-year students. Acad Med 2008;83:S63–7. [DOI] [PubMed] [Google Scholar]
- 5.Sundhagen HP, Almeland SK, Hansson E. Development and validation of a new assessment tool for suturing skills in medical students. Eur J Plast Surg 2018;41:207–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Routt E, Mansouri Y, De Moll EH, et al. Teaching the simple suture to medical students for long-term retention of skill. JAMA Dermatol 2015;151:761–5. [DOI] [PubMed] [Google Scholar]
- 7.Lemke M, Lia H, Gabinet-Equihua A, et al. Optimizing resource utilization during proficiency-based training of suturing skills in medical students: a randomized controlled trial of faculty-led, peer tutor-led, and holography-augmented methods of teaching. Surg Endosc 2020;34:1678–87. [DOI] [PubMed] [Google Scholar]
- 8.Pender C, Kiselov V, Yu Q, et al. All for knots: evaluating the effectiveness of a proficiency-driven, simulation-based knot tying and suturing curriculum for medical students during their third-year surgery clerkship. Am J Surg 2017;213:362–70. [DOI] [PubMed] [Google Scholar]
- 9.Olasky J, Kim M, Muratore S, et al. ACS/ASE Medical Student Simulation-based Research Collaborative Group. ACS/ASE Medical Student Simulation-based Skills Curriculum Study: implementation phase. J Surg Educ 2019;76:962–9. [DOI] [PubMed] [Google Scholar]
- 10.Augustin M. How to learn effectively in medical school: test yourself, learn actively, and repeat in intervals. Yale J Biol Med 2014;87:207–12. [PMC free article] [PubMed] [Google Scholar]
- 11.Fischer T, Chenot JF, Simmenroth-Nayda A, et al. Learning core clinical skills — a survey at 3 time points during medical education. Med Teach 2007;29:397–9. [DOI] [PubMed] [Google Scholar]
- 12.Cevik AA, Abu-Zidan F. Clinical procedure experience of medical students improves their objective structured clinical examination station scores in emergency medicine clerkship. Cureus 2019;11:e6261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foote DC, Reddy RM, Matusko N, et al. Surgery clerkship offers greater entrustment of medical students with supervised procedures than other clerkships. Am J Surg 2020;220:537–42. [DOI] [PubMed] [Google Scholar]
- 14.Luhoway JA, Ryan JF, Istl AC, et al. Perceived barriers to the development of technical skill proficiency in surgical clerkship. J Surg Educ 2019;76:1267–77. [DOI] [PubMed] [Google Scholar]