PURPOSE:
Lack of collection of sexual orientation and gender identity (SOGI) data in oncology practices limits assessment of sexual and gender minority (SGM) cancer patients' experiences and restricts opportunities to improve health outcomes of SGM patients. Despite national calls for routine SOGI data collection, individual-level and institutional barriers hinder progress. This study aimed to identify these barriers in oncology.
METHODS:
An online survey of ASCO members and others assessed SOGI data collection in oncology practices, institutional characteristics related to SOGI data collection, respondents' attitudes about SOGI data and SGM patients, and respondent demographics. Logistic regression calculated adjusted odds ratios (ORs) and 95% CIs for factors associated with sexual orientation (SO) and gender identity (GI) data collection.
RESULTS:
Less than half of 257 respondents reported institutional SO and GI data collection (40% and 46%, respectively), whereas over a third reported no institutional data collection (34% and 32%, respectively) and the remainder were unsure (21% and 17%, respectively). Most respondents felt that knowing both SO and GI was important for quality care (77% and 85%, respectively). Collection of SO and GI was significantly associated in separate models with leadership support (ORs = 8.01 and 6.02, respectively), having resources for SOGI data collection (ORs = 10.6 and 18.7, respectively), and respondents' belief that knowing patient SO and GI is important (ORs = 4.28 and 2.76, respectively). Themes from qualitative comments mirrored the key factors identified in our quantitative analysis.
CONCLUSION:
Three self-reinforcing factors emerged as critical drivers for collecting SOGI data: leadership support, dedicated resources, and individual respondents' attitudes. Policy mandates, implementation science, and clinical reimbursement are strategies to advance meaningful data collection and use in clinical practice.
INTRODUCTION
Sexual and gender minority (SGM) populations (eg, lesbian, gay, bisexual, transgender, gender nonbinary, two-spirit, those who partner with others of the same gender, and those whose gender identity [GI] differs from their sex assigned at birth) experience disparities across the cancer control continuum, from risk reduction through end-of-life.1-4 SGM people may experience greater cancer risk than the general population because of higher rates of smoking.5,6 Sexual minority people with breast cancer are diagnosed at later stages and at younger ages than heterosexual/cisgender counterparts (H/C; ie, those who partner with others of the opposite gender and whose GI matches their sex assigned at birth).7 Sexual minority people with prostate cancer report greater psychologic distress and sexual dysfunction following treatment than H/C patients with prostate cancer.8,9 Gender minority patients with cancer report that providers question their gender-affirming treatment decisions.1 On the basis of these and other studies, the National Institutes of Health have declared SGM people as a health disparities population, and national organizations such as the National Academies of Science, Engineering, and Medicine, American Medical Association, and ASCO have called for increased attention to SGM patients in health care settings in general and oncology practice specifically.10
A foundational requirement to address and monitor SGM cancer disparities is collection of sexual orientation and gender identity (SOGI) data in oncology practice and research. Systematic collection of SOGI data by health systems would allow cancer registries to document disparities in cancer incidence and mortality affecting SGM populations; encourage clinical trialists to assess differences in treatment outcome by sexual orientation (SO) and GI; enable appropriate notation of patients' caregivers and pronouns in electronic medical records; and support providers in referring SGM patients to tailored support resources. All of these efforts are currently hindered by lack of systematic SOGI data collection.11,12
Despite recommendations by national organizations and despite empirical evidence showing that the majority of both SGM and H/C patients are willing to report SOGI data, most oncology practices do not systematically collect it.11,13,14 The overall aim of this study was to assess individual and institutional factors associated with collection of SOGI data in oncology settings, including clinical practice and research. A secondary aim was to assess provider knowledge, attitudes, and behaviors about SOGI data collection, including beliefs about the value of collecting SOGI data as a component of providing high-quality cancer care.
METHODS
Survey Development
Researchers convened by the SGM Task Force of the ASCO Health Equity Committee developed a survey that drew questions from validated questionnaires and prior instruments used in cancer settings.15 The task force also created an expanded set of de novo items asking about institutional policies regarding SO and GI data collection (assessed separately); individual respondents' knowledge, beliefs, and attitudes regarding SOGI data collection; and the importance of using SOGI data in delivering cancer care. The survey used skip logic to tailor questions for clinicians versus researchers. In total, the survey contained 54 items, including 15 for participant demographics and two for open-ended comments about barriers and facilitators to collection of SOGI data.
Data Collection and Eligibility
The online survey was coded in Research Electronic Data Capture, a secure, web-based software platform for data collection,16 and distributed between October and November 2020. Current ASCO members were invited to participate via direct e-mail communications. Advertisement of the survey was also distributed via outreach to specific ASCO committee members, social media, and listservs. Unique URLs captured the source through which respondents accessed the survey. Two reminders were sent to ASCO members. No incentives were provided.
Anyone who reported working at an institution that provided clinical care to patients with cancer or reported working in cancer research (via initial screening questions) was eligible to participate. Responses were collected anonymously, and completion of demographic characteristics was optional.
Ethical Review
Per ASCO internal policies, this study was considered health care operations quality improvement. Thus, no institutional review board approval was sought.
Data Analysis
Quantitative.
Individual survey items were analyzed using descriptive statistics. Univariable and multivariable polytomous logistic regression models were used to determine factors significantly associated with the study's primary outcomes: respondents' report of SO and/or GI data collection at their institutions (yes/no/unsure). Specifically, logistic regression was used to quantify the magnitude of associations between SO and GI data collection and independent individual-level factors (eg, respondent role, level of patient contact, understanding of how to collect SOGI data, positive emotions regarding SOGI data collection, belief in the importance of knowing SOGI data for clinical practice, confidence in applying SOGI data to relevant clinical decisions, and demographics) and institutional factors (eg, leadership support for SOGI data collection, institutional resources dedicated to SOGI data collection, practice type, and practice size). Factors associated with the primary outcomes at P < .10 in univariable models were included in multivariable models for SO and GI data collection separately and were then manually deleted in step-wise manner from each model until all covariates remaining in the model had P < .05. The results are presented as odds ratios (ORs) with 95% CIs and P values.
Qualitative.
Limited qualitative data were collected as part of this survey to ASCO members, consisting of responses to two open-ended questions. Three coders (G.P.Q., M.L.P.-C., and S.M.) established a code list and coded data for the first 50 responses to each question. Coders met and obtained consensus on a codebook and then independently coded the remaining responses in Excel using content analysis and constant comparison methods. Inter-rater reliability was 0.95.
RESULTS
Respondent Demographics
A total of 257 respondents completed the survey. The majority of respondents (82%) had a clinical role (Table 1). More than half worked at a university hospital (54%) but almost a quarter worked at community or private hospitals (24%). The majority identified as female (56%). Most identified as heterosexual (78%), although a significant portion identified as gay (9%), lesbian (4%), or bisexual (3%), with 1% identifying as queer, 1% self-defining an SO, and 3% preferring not to answer. The majority identified as White (70%), with smaller percentages identifying as Asian (15%), Black (3%), and Hispanic (10%). Most respondents considered themselves politically liberal (69%).
TABLE 1.
Respondent Characteristics (N = 257)
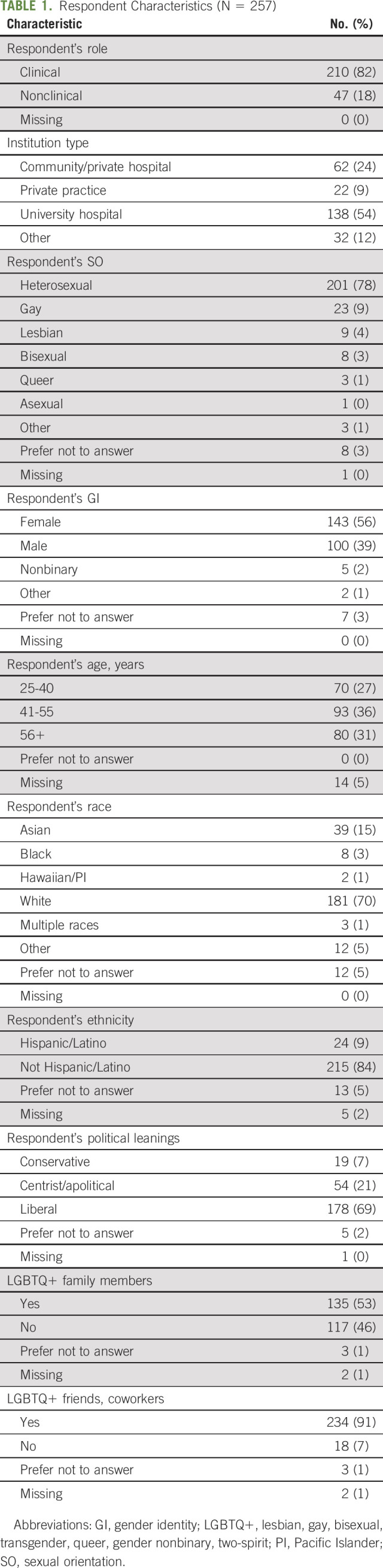
Less than half of respondents reported that their institutions collected SO or GI data (40% and 46%, respectively). By contrast, over a third reported that their institutions did not collect SO or GI data (34% and 32%, respectively), and the remaining fifth were unsure (21% and 17%, respectively). Although the majority believed it was important to know patients' SO and GI (68% and 74%, respectively) to provide quality care, some respondents disagreed that it was important (17% and 12%, respectively). Respondents who identified as gay or lesbian were more likely to agree that it was important to know both patients' SO and GI than respondents of other SOs. Respondents who preferred not to identify their race and who identified as politically conservative were more likely to disagree that it was important to know patients' SO (data not shown).
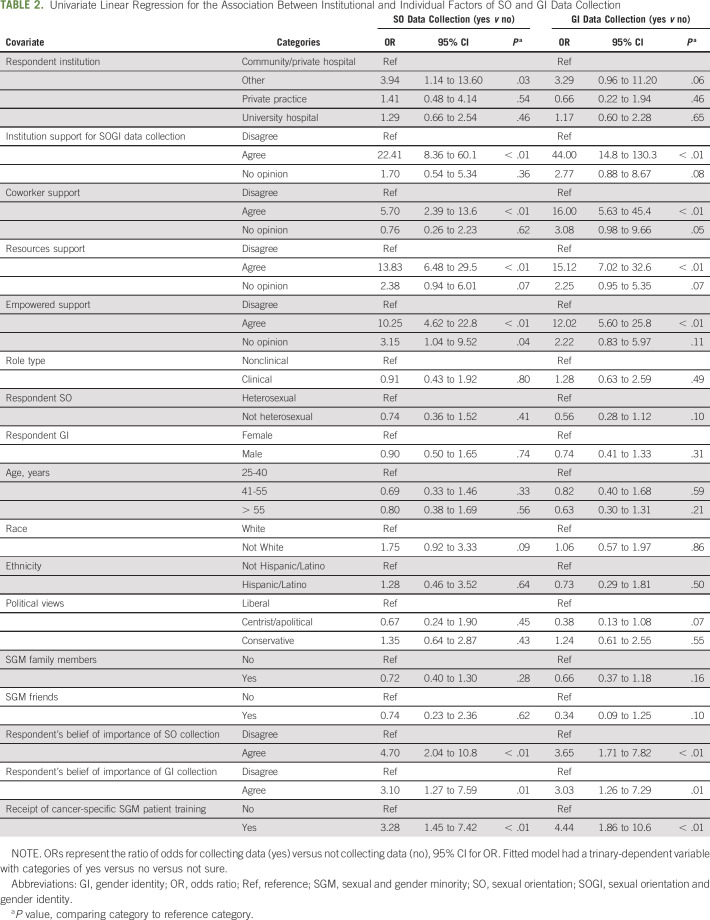
Univariable Models
In unadjusted univariable models, nine factors were significantly associated with SO data collection at P < .10: type of cancer care institution, leadership support, coworker support, resources, feeling empowered; and respondent's race, belief that knowing SO is important for providing quality care, belief that knowing GI is important for providing quality care, and receipt of cancer-specific SGM patient training. These factors were included in the full (multivariable) model for SO. In unadjusted models, 11 factors were significantly associated with GI data collection at P < .10: type of cancer care institution, leadership support, coworker support, resources and feeling empowered to collect SOGI data; respondent's SO, political views, report of SGM friends, belief that knowing SO is important for providing quality care, belief that knowing GI is important for providing quality care, and receipt of cancer-specific SGM patient training. These factors were included in the full (multivariable) model for GI (Table 2).
TABLE 2.
Univariate Linear Regression for the Association Between Institutional and Individual Factors of SO and GI Data Collection
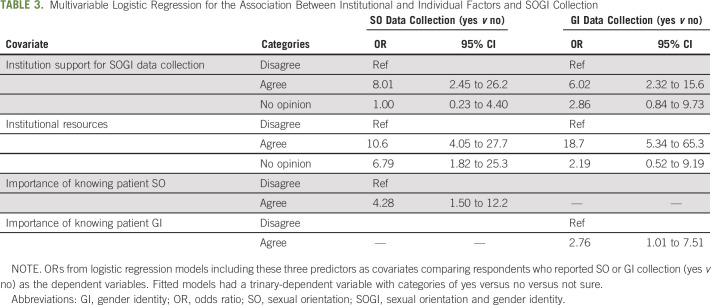
Multivariable Models
In multivariable logistic regression models predicting SO and GI data collection, strong correlations between covariates reduced statistical significance of some covariates such that they were no longer statistically significant at P < .05. These covariates were removed from the models. In the final adjusted model for institutional SO data collection (Table 2), having leadership support for SOGI data collection (OR = 8.01; 95% CI, 2.45 to 26.2), having dedicated institutional resources (OR = 10.6; 95% CI, 4.05 to 27.7), and the respondent's belief in importance of knowing patients' SO (OR = 4.28; 95% CI, 1.50 to 12.2) remained significantly associated with SO data collection. Similarly, in the final adjusted model for institutional GI data collection, having leadership support (OR = 6.02; 95% CI, 2.32 to 15.6), having dedicated institutional resources (OR = 18.7; 95% CI, 5.34 to 65.3), and the respondent's belief in the importance of knowing patients' GI (OR = 2.76; 95% CI, 1.01 to 7.51) remained significantly associated with GI data collection.
Qualitative Themes
A total of 152 people provided qualitative responses to two open-ended questions in the survey about barriers and facilitators to SOGI data collection (Table 3). Barriers included institutional culture, with respondents stating SOGI data collection was not part of the culture/not required and that there was no messaging from the health system that patient-specific SOGI answers matter (ie, have any impact on clinical care or outcomes, or are even important to delivering person-centered care). Respondents also described provider beliefs and discomfort as a barrier, citing “lack of individual understanding of SOGI nomenclature (ie, what's gender queer v gender diverse, etc) that may factor in to (providers') comfort level asking questions of a patient on their SOGI” and “lack of understanding on the true impact of SOGI on clinical outcomes.” Patient discomfort was also cited, with respondents voicing “concerns of patients regarding possible prejudices” if they disclosed SOGI. Practical barriers included the electronic medical record, with respondents saying there was “no innate field for data” in their practices' systems, as well as lack of training, resources, and time, with respondents saying they had no time for the discussion or training on how to approach patients about their SOGI.
TABLE 3.
Multivariable Logistic Regression for the Association Between Institutional and Individual Factors and SOGI Collection
Facilitators included robust protocols, with automatic processes, standardized fields, and a process where this (SOGI data collection) occurs up front for all patients regardless of preference. Several respondents commented on the need for culture change, “with more representation of queer/trans people among staff and safe spaces to be who we are.” Respondents noted the importance of training on how to collect and what to do with SOGI data, as well as improving community trust, particularly in conservative regions of the country. Of note, three respondents made negatively biased comments about SGM patients. For example, one provider noted, “Sexual deviants should receive treatment for their condition.”
DISCUSSION
In this study, we used an online survey disseminated to ASCO members and others recruited via social media to identify individual-level and institutional barriers and facilitators to SOGI data collection in oncology. A key finding was that institutional SOGI data collection was significantly associated with a respondent's belief that knowing patient SOGI is an important component for providing high-quality care. We found that SO and GI data collection was significantly associated with both leadership support and dedicated resources for SOGI data collection. Together, these individual and institutional factors could be the target of quality improvement initiatives to implement collection of SOGI data within oncology settings.
Themes from qualitative comments mirrored the key factors identified in our quantitative analysis. Respondents commented on their own perceptions of the importance of SOGI data collection, workplace culture including leadership support, and the presence/absence of resources that affected the success of SOGI data collection. Respondents also provided additional details about types of resources that could facilitate SOGI data collection in oncology, including detailed protocols for data collection, designated space in electronic health records (EHRs) to document SOGI, and training to increase provider and staff cultural competence. Notably, in 2015, the Centers for Medicare and Medicaid Services and the Office of the National Coordinator for Health Information Technology mandated SOGI documentation capability in EHRs for stage 3 of Meaningful Use. Yet, most institutions and providers are not systematically using these capabilities.17 This suggests that institutional leadership must play a role in incentivizing and/or requiring collection of these data in practice.
The need for additional training about SGM patients' cancer disparities and experiences of discrimination is underscored by our finding that some respondents did not see value in collecting SOGI data as a way to improve cancer care. Although providers' demographic characteristics may predict such beliefs,18 SGM-specific training19 and exposure to SGM persons19 also predicted increased SGM-specific health care knowledge, better attitudes of providers toward SGM patients, and lower expressed transphobia and homophobia.20 With 7.1% of Americans identifying as SGM in a recent national poll,21 and growing numbers of young adults disclosing their SGM identities, the mandate for all oncology providers and staff to receive training in the care of SGM patients is urgent. This training should incorporate evidence-based tools to reduce implicit bias toward SGM patients and their families, up-to-date information on cancer-related disparities experienced by SGM patients, and best practices for supporting SGM people facing cancer.22,23 Such training should also inform professionals about barriers and facilitators to SOGI data collection and provide practical guidance to collect these data effectively. Importantly, the National Academies of Science, Engineering, and Medicine recently released guidance on how to collect SOGI data on the basis of evidence to date.24 Given the distinct needs reported by transgender and gender diverse patients, and the unknown risks of hormonal therapy on oncology management decisions, trainings would also benefit from an explicit focus on GI, and more research is needed in general on the optimal management for gender diverse patients on hormonal therapies with cancer.25
In addition to perceived lack of value in collecting SOGI, more than 30% of respondents believed that their patients would be uncomfortable if asked about their SOGI. However, this belief is refuted by a growing body of research. One study reported the majority of both SGM and H/C patients would agree to disclose SO (95%) and GI (99%) in emergency medicine settings,26 and another study of oncology patients found that the majority of patients across multiple demographic groups had favorable perceptions of being asked SOGI questions.26,27 Importantly, preliminary evidence suggests that disclosure of SOGI to cancer care providers improves self-reported health among SGM cancer patients.28 Furthermore, although some patients may feel uncomfortable being asked about SOGI, asking will help to normalize collecting these data to reduce discomfort for H/C individuals in the long term. In short, the risk of alienating a minority of patients by asking about SOGI must be evaluated against the benefits of improving care for SGM patients, documenting SGM disparities, and reducing these disparities through research-driven and SGM-specific interventions.
It is important to note that some SGM patients may have experienced lived or community-level discrimination in health care settings, leading to mistrust of health care systems and reticence to disclose SOGI to health care providers.5 By not systematically collecting SOGI data on all patients, we may reinforce mistrust, place the onus of disclosure on SGM patients, and exacerbate stigma. Furthermore, growing numbers of studies have shown that nondisclosure of SOGI status is associated with delays in seeking care29 and poorer mental health among SGM patients.30 These sequelae may contribute to SGM disparities in areas of the country that are historically conservative, and where institutional efforts to collect SOGI data are less common. Given the lack of nationwide protections for SGM people from job and housing loss at the time of writing this article, and the recent surge in legislation limiting access to medical care for transgender patients, SGM patients' hesitance to voluntarily disclose SOGI in the absence of institutional efforts to collect, protect, and act on these data is understandable. It is important to note that SOGI data disclosure is a proxy for patient comfort with their health care team and ability to show up as a whole person for cancer care. Ultimately, social interventions to normalize sexual and gender diversity are needed to advance health equity among SGM persons.
Our study shows that factors that predict SOGI data collection are linked and self-reinforcing, regardless of the geographic context. The results show that the absence or insufficient provision of leadership support, lack of dedicated resources, and disagreement that knowledge of SOGI is an important component of patient-centered care were common features of institutions without efforts to collect SOGI data. These barriers hinder SOGI data collection. Our qualitative data suggest that systematic collection of SOGI data may also be constrained by difficulty implementing, locating, and consistently using SOGI data collection fields in EHRs, lack of institutional procedures and assigned personnel for collecting SOGI data, as well as individual barriers, such as bias or uncertainty about how best to discuss SOGI on the part of providers. Thus, in addition to training, mandates from leadership to collect SOGI data are a necessary first step in conveying institutional commitment to this process. Broader system-level policies tying reimbursement and accreditation to completeness of SOGI data collection would lend further weight to such mandates, particularly if endorsed by payors such as the Center for Medicare and Medicaid Studies. Finally, implementation science studies are needed to determine the best way to integrate SOGI data into oncology clinic workflows to ensure that data are collected and used effectively.
Limitations of the current study include a convenience sampling strategy and limited sample size, although the sample had statistical power to detect significant associations. Because of snowball sampling, no response rate can be calculated for our study. In our study, the proportion of SGM-identifying respondents was higher than national averages (9% v 5.6%), indicating a degree of selection bias. The majority (53%) of respondents reported SGM family members, and 94% reported SGM coworkers, further underscoring that this sample was likely enriched for individuals primed to care about SOGI data collection on the basis of their personal identities or relationships. The proportion of non-White respondents was low, indicating the need to recruit more diverse samples to understand the perspectives of racial and ethnically diverse populations regarding SOGI data collection. In addition to identifying factors associated with institutional SOGI data collection, a strength of the study was the insight derived from responses to open-ended questions about barriers and facilitators to SOGI data collection. These data reinforced quantitative findings and encourage future inquiry. However, the qualitative data collected in this study were limited to two open-ended survey questions; more in-depth qualitative research into this topic is needed.
In conclusion, many national organizations have responded to growing awareness of health disparities affecting minoritized populations by strengthening their commitment to eliminating structural barriers to health equity. Failure to collect SOGI data is one such structural barrier. Evidence strongly suggests that SOGI data collection is acceptable to patients in health care settings.13,14,26 Unfortunately, the continued failure of many oncology practices and research studies to systematically collect SOGI data perpetuates invisibility of SGM patients and, potentially, fuels disparities.4
We identified several factors independently associated with both SO and GI data collection: leadership support and dedicated resources for SOGI data collection, and individual respondents' belief that SOGI data are important for patient care in oncology. These factors suggest that multilevel interventions are needed to support systematic SOGI data collection. Such interventions, on the basis of our qualitative data, must address lack of knowledge SGM disparities, mitigate the impact of implicit biases on SOGI data collection, improve workflows for SOGI documentation, and commit educational and other resources to this effort. Without such interventions, goals to advance cancer-related health equity for SGM people cannot be achieved.
ACKNOWLEDGMENT
The authors would like to thank Kim Smith, Senior Program Manager at ASCO, for her administrative support, and acknowledge the contributions of the members of the ASCO Health Equity Committee and Sexual and Gender Minority Task Force. The authors would also like to thank all the survey respondents, especially those who chose to disclose their sexual and gender minority status.
Gwendolyn P. Quinn
Honoraria: Flo Health
Research Funding: Pfizer (Inst)
Matthew B. Schabath
Research Funding: Bristol Myers Squibb
Shail Maingi
Employment: Merck (I)
Stock and Other Ownership Interests: Merck (I)
Shine Chang
Leadership: IBS Corp (I)
Stock and Other Ownership Interests: Anthem Inc, Walgreens
No other potential conflicts of interest were reported.
SUPPORT
This work was made possible through logistical and biostatistical support of American Society of Clinical Oncology.
C.S.K. and M.L.P.-C. equally contributed as first authors to this work.
AUTHOR CONTRIBUTIONS
Conception and design: Charles S. Kamen, Mandi L. Pratt-Chapman, Stephen C. Meersman, Gwendolyn P. Quinn, Matthew B. Schabath, Shail Maingi, Janette K. Merrill, Shine Chang
Administrative support: Stephen C. Meersman, Janette K. Merrill
Collection and assembly of data: Charles S. Kamen, Mandi L. Pratt-Chapman, Stephen C. Meersman, Gwendolyn P. Quinn, Janette K. Merrill, Shine Chang
Data analysis and interpretation: Charles S. Kamen, Mandi L. Pratt-Chapman, Gwendolyn P. Quinn, Matthew B. Schabath, Shail Maingi, Elizabeth Garrett-Mayer, Melinda Kaltenbaugh, Caroline Schenkel, Shine Chang
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Sexual Orientation and Gender Identity Data Collection in Oncology Practice: Findings of an ASCO Survey
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/op/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Gwendolyn P. Quinn
Honoraria: Flo Health
Research Funding: Pfizer (Inst)
Matthew B. Schabath
Research Funding: Bristol Myers Squibb
Shail Maingi
Employment: Merck (I)
Stock and Other Ownership Interests: Merck (I)
Shine Chang
Leadership: IBS Corp (I)
Stock and Other Ownership Interests: Anthem Inc, Walgreens
No other potential conflicts of interest were reported.
REFERENCES
- 1.Pratt-Chapman ML, Alpert AB, Castillo DA: Health outcomes of sexual and gender minorities after cancer: A systematic review. Syst Rev 10:183, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gibson AW, Radix AE, Maingi S, et al. : Cancer care in lesbian, gay, bisexual, transgender and queer populations. Future Oncol 13:1333-1344, 2017 [DOI] [PubMed] [Google Scholar]
- 3.Kent EE, Wheldon CW, Smith AW, et al. : Care delivery, patient experiences, and health outcomes among sexual and gender minority patients with cancer and survivors: A scoping review. Cancer 125:4371-4379, 2019 [DOI] [PubMed] [Google Scholar]
- 4.Burkhalter JE, Margolies L, Sigurdsson HO, et al. : The national LGBT cancer action plan: A white paper of the 2014 national summit on cancer in the LGBT communities. LGBT Health 3:19-31, 2016 [Google Scholar]
- 5.Blosnich J, Lee JG, Horn K: A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control 22:66-73, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamen C, Blosnich JR, Lytle M, et al. : Cigarette smoking disparities among sexual minority cancer survivors. Prev Med Rep 2:283-286, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boehmer U: Breast cancer in lesbian and bisexual women, in Boehmer U, Elk R. (eds): Cancer and the LGBT Community: Unique Perspectives From Risk to Survivorship. Cham, Switzerland, Springer, 2015, pp 141-157 [Google Scholar]
- 8.Ussher JM, Perz J, Kellett A, et al. : Health-related quality of life, psychological distress, and sexual changes following prostate cancer: A comparison of gay and bisexual men with heterosexual men. J Sex Med 13:425-434, 2016 [DOI] [PubMed] [Google Scholar]
- 9.Ussher JM, Perz J, Rose D, et al. : Threat of sexual disqualification: The consequences of erectile dysfunction and other sexual changes for gay and bisexual men with prostate cancer. Arch Sex Behav 46:2043-2057, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Griggs J, Maingi S, Blinder V, et al. : American Society of Clinical Oncology position statement: Strategies for reducing cancer health disparities among sexual and gender minority populations. J Clin Oncol 35:2203-2208, 2017 [DOI] [PubMed] [Google Scholar]
- 11.Cahill S, Singal R, Grasso C, et al. : Do ask, do tell: High levels of acceptability by patients of routine collection of sexual orientation and gender identity data in four diverse American community health centers. PLoS One 9:e107104, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haider A, Adler RR, Schneider E, et al. : Assessment of patient-centered approaches to collect sexual orientation and gender identity information in the emergency department: The EQUALITY study. JAMA Netw Open 1:e186506, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cathcart-Rake EJ, Zemla T, Jatoi A, et al. : Acquisition of sexual orientation and gender identity data among NCI Community Oncology Research Program practice groups. Cancer 125:1313-1318, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haider AH, Schneider EB, Kodadek LM, et al. : Emergency department query for patient-centered approaches to sexual orientation and gender identity: The EQUALITY study. JAMA Intern Med 177:819-828, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schabath MB, Blackburn CA, Sutter ME, et al. : National survey of oncologists at National Cancer Institute-designated comprehensive cancer centers: Attitudes, knowledge, and practice behaviors about LGBTQ patients with cancer. J Clin Oncol 37:547-558, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patridge EF, Bardyn TP: Research electronic data capture (REDCap). J Med Libr Assoc 106:142-144, 2018 [Google Scholar]
- 17.Centers for Medicare & Medicaid Services : Medicare and Medicaid programs; electronic health record incentive program-stage 3 and modifications to meaningful use in 2015 through 2017. Final rules with comment period. Fed Regist 80:62761-62955, 2015 [PubMed] [Google Scholar]
- 18.Taskiran Eskici G, Alan H, Eskin Bacaksiz F, et al. : Under the same rainbow: A study on homophobia and discrimination among private sector health care professionals. J Nurs Manag 29:3-15, 2021 [DOI] [PubMed] [Google Scholar]
- 19.Nowaskie DZ, Patel AU, Fang RC: A multicenter, multidisciplinary evaluation of 1701 healthcare professional students' LGBT cultural competency: Comparisons between dental, medical, occupational therapy, pharmacy, physical therapy, physician assistant, and social work students. PLoS One 15:e0237670, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cakir H, Harmanci Seren AK: Are nurses homophobic? A survey study in public hospitals in Turkey. J Nurs Scholarsh 52:613-622, 2020 [DOI] [PubMed] [Google Scholar]
- 21.Jones JM: LGBT identification in U.S. ticks up to 7.1%. Gallup, 2022 [Google Scholar]
- 22.Capers Q, IV: How clinicians and educators can mitigate implicit bias in patient care and candidate selection in medical education. ATS Sch 1:211-217, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morris M, Cooper RL, Ramesh A, et al. : Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: A systematic review. BMC Med Educ 19:1-13, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dalke K: Measuring Sex, Gender Identity, and Sexual Orientation. Washington, DC, National Academies Press. 2022 [PubMed] [Google Scholar]
- 25.Alpert AB, Gampa V, Lytle MC, et al. : I'm not putting on that floral gown: Enforcement and resistance of gender expectations for transgender people with cancer. Patient Educ Couns 104:2552-2558, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rosser BS, Polter EJ, Chandiramani N, et al. : Acceptability and feasibility of collecting sexual orientation and expanded gender identity data in urology and oncology clinics. LGBT Health 8:420-426, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alexander K, Walters CB, Banerjee SC: Oncology patients' preferences regarding sexual orientation and gender identity (SOGI) disclosure and room sharing. Patient Educ Couns 103:1041-1048, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kamen C, Margolies L, Smith-Stoner M, et al. : Correlates and Outcomes of Lesbian, Gay, Bisexual, and Transgender (LGBT) Identity Disclosure to Cancer Care Providers. Miami, FL, Multinational Association of Supportive Care in Cancer, 2014 [Google Scholar]
- 29.Brooks H, Llewellyn CD, Nadarzynski T, et al. : Sexual orientation disclosure in health care: A systematic review. Br J Gen Pract 68:e187-e196, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Durso LE, Meyer IH: Patterns and predictors of disclosure of sexual orientation to healthcare providers among lesbians, gay men, and bisexuals. Sex Res Social Policy 10:35-42, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]