Abstract
Fecal microbiota transplantation (FMT) consists of infusion of feces from a donor to a recipient patient in order to restore the resident microbial population. FMT has shown to be a valid clinical option for Clostridioides difficile infections (CDI). However, this approach shows several criticalities, such as the recruiting and screening of voluntary donors. Our aim was to evaluate the therapeutic efficacy of a synthetic bacterial suspension defined “Bacterial Consortium” (BC) infused in the colon of CDI patients. The suspension was composed by 13 microbial species isolated by culturomics protocols from healthy donors' feces. The efficacy of the treatment was assessed both clinically and by metagenomics typing. Fecal samples of the recipient patients were collected before and after infusion. DNA samples obtained from feces at different time points (preinfusion, 7, 15, 30, and 90 days after infusion) were analyzed by next-generation sequencing. Before infusion, patient 1 showed an intestinal microbiota dominated by the phylum Bacteroidetes. Seven days after the infusion, Bacteroidetes decreased, followed by an implementation of Firmicutes and Verrucomicrobia. Patient 2, before infusion, showed a strong abundance of Proteobacteria and a significant deficiency of Bacteroidetes and Verrucomicrobia. Seven days after infusion, Proteobacteria strongly decreased, while Bacteroidetes and Verrucomicrobia increased. Metagenomics data revealed an “awakening” by microbial species absent or low concentrated at time T0 and present after the infusion. In conclusion, the infusion of selected bacteria would act as a trigger factor for “bacterial repopulation” representing an innovative treatment in patients with Clostridioides difficile infections.
1. Introduction
The human gut microbiota is composed by approximately 1014 commensal microorganisms including bacteria, viruses, fungi, and protozoa which represent a real solid organ, with an approximate weight of two kg [1]. Among these, bacteria represent the most studied group. The major representative phyla are Firmicutes and Bacteroidetes [2]. These microbial communities are highly organized and play a key role in modulating host immunity, nutrition, and metabolism and in the health/disease balance. Nowadays, it is well known that many intestinal and extraintestinal disorders are closely related to compositional and functional changes in commensal microbiota [3]. An example is represented by Clostridioides difficile infection (CDI). Clostridioides difficile (C. difficile) is a Gram-positive, sporogenous, motile, obligate anaerobic, and toxin-producing bacterium, originally identified in 1935 as a member of the microbial flora of infants. The strain was called Bacillus difficile for the difficulty of isolating and culturing [4]. CDI is a nosocomial infection mainly due to prolonged exposure to antibiotic therapies or prophylaxis during the hospitalization [5]. Currently, 7 cases are described per 10.000 patients admitted to European hospitals [6]. The statistics are also similar for the American hospitals, in which C. difficile is the main cause of nosocomial infection with 14.000 deaths/year [6, 7]. Currently, the therapeutic CDI approach is based on antibiotic therapy. The drugs of choice are metronidazole, vancomycin, and fidaxomicin [5, 8]. The great impact on public health and the appearance of resistant strains has forced the scientific community to find alternative therapeutic approaches, including the recent fecal microbiota transplantation (FMT). The FMT consists of the infusion of feces from a healthy donor to a recipient patient in order to treat specific diseases associated with alterations of the intestinal microbiota (dysbiosis) [8, 9]. FMT has shown interesting and promising results about the efficacy and management of the patients. But, concerning on procedural safety, potential pathogen transmission, and standardizing workflow, some key points have to be improved [10]. Recruiting of voluntary donors is a very critical aspect in FMT flowchart. In fact, donors' selection is a very hard and rigorous process. At first, each donor undergoes a general questionnaire to exclude intestinal and extraintestinal disorders. Subsequently, on donor stool and blood sample are performed cultural, molecular, and serologic analyses in order to avoid any possible transmission during infusion procedure [10–12]. It is clear that during screening process, a donor may result as unsuitable and, then, his fecal matter is unusable for the therapy. Based on current evidence, FMT represents an alternative safe therapeutic method with few adverse effects. Even so, every patient candidate for FMT needs to be informed about the potential risks before the procedure. Most clinical trials and systemic reviews presented that some minor adverse events, such as abdominal discomfort, diarrhea, constipation, and low-grade fever, were transiently noted after FMT, and uncommon severe side effects were often associated with the possible complications of endoscopy and sedation [13]. Moreover, some case reports describe a small population of patients that experienced IBD flares after FMT. The definite mechanism of IBD flare after FMT is still unclear, although Quera et al. suggested that transient bacteremia may result in altered intestinal permeability, resulting in a flare [14]. To date, long-term, follow-up studies (3–68 months post-FMT, average 17 months post-FMT) have found FMT to be relatively free of adverse effects [15]. The randomized control trial for treatment of rCDI (recurrent Clostridioides difficile) published by Van Nood et al. found that of the 16 patients treated, 15 experienced diarrhea, 5 had abdominal cramping, 3 had belching, and 1 had nausea. These effects were not observed in the control group that received only a bowel lavage; however, the effects were all self-limiting and resolved within 3 h post-FMT [16]. In terms of long-term adverse effects of FMT, there is a theoretical possibility that an infection will be transferred or a chronic disease will be stimulated (e.g., obesity, diabetes, and atherosclerosis) because of the alteration of the gut microbiota. However, long-term, follow-up studies are necessary to assess these risks. Advances in FMT delivery may reduce procedural complications in the future. Overcoming the possible occurrence of such adverse effects, in most cases mild and self-limiting, represents the main challenge for future FMT clinical applications. For these reasons, our study has been directed on the therapeutic efficacy of a synthetic bacterial preparation, called “Bacterial Consortium” (BC), in patients with CDI in substitution of the standard FMT. To this end, more than 60 different species of bacteria, both obligate and facultative anaerobes, normally present in the human intestinal microbiota, were isolated from healthy donors' stool samples (Figure 1). This stool substitute preparation is composed by 13 gut bacteria isolated in pure culture (Table I) from three healthy donors using culturomics' approach. Bacteroides strains were tested for susceptibility and resistance profile to antibiotics based on EUCAST guidelines. Culturomics is a set of culture conditions applied to isolate bacterial strains considered uncultivable [17]. Culture conditions include broth media enrichment, blood cultures' bottle, and selective and nonselective agar media incubated at different temperatures and times and observed from few days to months. Each colony is then identified by MALDI-TOF mass spectrometry [18–20]. Here, we reported the successful outcome of two patients with recurrent CDI unresponsive to conventional therapy and treated with BC infusion. Moreover, we provided the characterization by metagenomics of the recipient gut microbiota at different time points: preinfusion (T0), 7, 14, 30, and 90 days after transplantation (T1, T2, T3, and T4) in order to evaluate the following: (a) the engraftment of the infused bacterial species and (b) the richness and biodiversity of the bacterial communities pre- and post-FMT.
Figure 1.
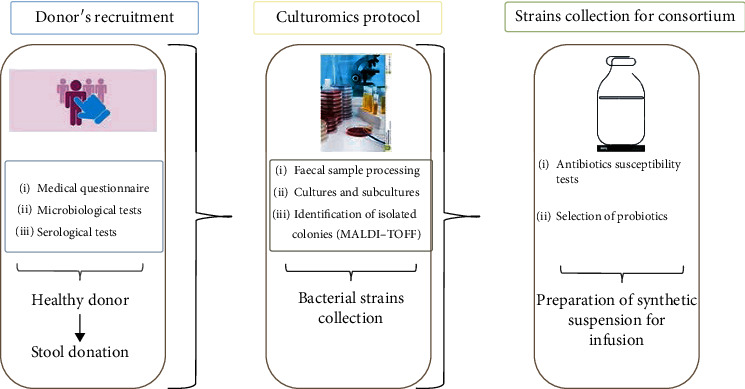
Study design. Candidate donor undergoes multistep screening to exclude risk factors, comorbidities, and any potential pathogen transmission. Subsequently, feces from a “healthy donor” are processed for culturomics in order to collect potential beneficial bacteria.
2. Materials and Methods
2.1. Donors' Recruitment
Three donors (a 45-year-old woman, a 42-year-old woman, and a 43-year-old man) were recruited basing on their medical and clinical history at CEMAD Department in A. Gemelli Hospital (Rome) (protocol code 0021125/16) [8]. The relative fecal samples were analyzed in order to exclude the presence of C. difficile toxin A/B producer (Liaison, DiaSorin Spa, Saluggia VC, Italy) and intestinal pathogens such as Salmonella spp., Campylobacter spp., Shigella spp., Yersinia enterocolitica, protozoa, and helminths. The presence of vancomycin-resistant Enterococci (VRE), methicillin-resistant Staphylococcus aureus (MRSA), and Gram-negative multi-drug-resistant bacteria (MDR) was also excluded by cultural assay. Moreover, RT-PCR Allplex™ Gastrointestinal Panel Assays (Seegene, South Korea) for the comprehensive detection and identification of 25 gastrointestinal pathogens (virus, bacteria, toxins and parasite) were performed in order to declare the stool “pathogens free” and then suitable for infusion.
2.2. Culturomics Protocol
Thirty grams of fecal sample was suspended in 30 mL of saline solution. After the homogenization by Stomacher® 400 Circulator (SEWARD, UK), the fecal suspension was split in two aliquots and centrifuged at 3500 × g for 10 minutes [21]. Supernatants were discarded, and the two pellets were resuspended: one in 15 mL of rumen fluid and the other one in 15 mL of supplemented Brucella Broth (BB, Remel INC., Lenexa, USA). Each enriched suspension (5 mL) was divided into six 2.5 mL aliquots, which were inoculated into a bottle of blood cultures for aerobes and anaerobes (Becton, Dickinson and Company, Benex Limited, Shannon, Ireland). Subsequently, the bottles were incubated at 30°C, 37°C, and 42°C for seven and fourteen days. After incubation period, 10 μL of bacterial enriched suspension was plated on the following agar media and then incubated: TSA (Tryptic Soy Agar, Becton Dickinson, Franklin Lakes, USA), SCH (Schaedler agar, Becton Dickinson, Franklin Lakes, USA), CNA (Columbia agar, Becton Dickinson, Franklin Lakes, USA), and PVX (chocolate agar, bioMérieux, Marcy-l'Étoile, France). Culture conditions are described in Figure 2.
Figure 2.
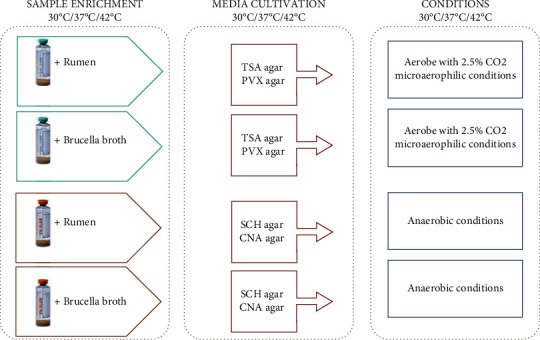
Culturomics protocol conditions used for bacterial isolation and BC synthesis.
2.3. Identification of Isolated Strains
Each colony observed after the incubation phase was first isolated in order to obtain a pure culture and subsequently identified by MALDI-TOF mass spectrometry (Bruker Daltonics, Billerica, MA, USA). The bacterial colonies were “spotted” on the target plate and hydrated with 1 μL of α-cyrano-4-hydroxycinnamic acid (α-CHCA). Before each measurement, the instrument was calibrated using Bacterial Test Standard (BTS, Bruker Daltonics, Billerica, MA, USA). All the bacterial strains analyzed reported an identification reliability score greater than 1.9. Bacterial strains of interest were stored at -80° C and in 10% glycerol suspension. Antibiotic susceptibility tests were performed on the thirteen strains selected in order to avoid the infusion, in the recipient patient, of any MDR microorganisms. MICs were obtained by broth microdilution method (Sensititre™ Anaerobe MIC Plate, Thermo Fisher Scientific, Waltham, Massachusetts, USA) and epsilon test (E-test, bioMerieux, Marcy-l'Étoile, France) (data not shown).
2.4. “Bacterial Consortium” Preparation
The preparation of the synthetic suspension was carried out on the same day on which the infusion was scheduled. The thirteen selected species were cultured under anaerobic conditions 72 h before infusion in order to obtain bacterial suspensions (16 mL of 0.9% saline solution) prepared considering turbidity values (McFarland) between 2.5 and 5 McFarland equal to about 5 × 108-109 CFU/mL. The thirteen suspensions were combined in a single solution with a final volume of 250 mL. The preparation was poured into a sterile glass bottle and incubated for 30 minutes at 37°C.
2.5. Infusion Procedure
The recipient patients (PZ1 = female 80 years; PZ2 = female 70 years) underwent pretreatment with vancomycin (125 mg orally, 4 times/day for 3 days) followed by intestinal washing, on the last day of antibiotic therapy, with Macrogol (SELG ESSE). On day 4, the bacterial suspension synthesized in the laboratory was infused about an hour before surgery. The solution was infused, using 50 mL syringes, at the level of the proximal section of the colon. During the operation, the patient was placed on his right side. The same position was maintained for at least 1 h postsurgery in order to implement the permanence of the infused material in the colon. The whole procedure lasted about 10 minutes. At the end of the entire procedure, the patient was monitored for two hours [5, 8].
2.6. DNA Extraction and Metagenomics Analysis
Metagenomics evaluation was carried out on fecal samples from two recipient patients and collected at different time points: pretransplantation (T0), 7 days (T1), 15 days (T2), 1 month (T3), and 3 months (T4) posttransplantation. Acid nucleic extraction from stool samples was performed using DANAGENE Microbiome Fecal DNA Kit (Danagen, Barcelona, Spain). Briefly, 50-200 mg of fecal matter was weighed and placed into a bead microtube in order to ensure cell lysis. Subsequently, 25 μL of proteinase K was added to the lysate to remove RNase and DNase activities. A washing phase was performed using a DNA column-collection tube. Lastly, 200 μL of Elution Buffer was added in order to obtain the same volume of purified DNA. DNA samples were analyzed using the KIT 16S rRNA MiSeq (Illumina). The amplified target regions correspond to the variable regions V3-V4. In a first phase, the DNA was amplified using two specific primers for the V3-V4 regions, which have structures defined as adapters (forward primer 5′TCGTCGGAGCAGCTGTGTGTATAAGAACACCTGGGNCAG; reverse 5′TCGTCGGCAGCGCTCGGAGATGTTTAGAGAGAGACGACT). Each reaction had a final volume of 25 μL of which are 12.5 μL of 2X Kapa HiFi HotStart mix (Anachem, Dublin, Ireland), 5 μL primer F (1 μM), 5 μL primer R (1 μM), and 2.5 μL of DNA. The amplification reaction was carried out with the following thermal profile: heated lid 110°C, 95°C × 3 min, 95°C 30 sec, 55°C × 30 sec, and 72° × 30 sec for 25 cycles followed by a final extension phase at 72°C × 5 min. The PCR products were visualized by agarose gel electrophoresis (1X TAE, 1.5% agarose, 90 V) and subsequently purified by AMPure XP bead purification (Labplan, Dublin, Ireland). A second PCR was conducted on the purified DNA. Each reaction involved the use of 5 μL of primer index 1 (N7xx), 5 μL of primer index 2 (S5xx), 25 μL of 2X Kapa HiFi, and 10 μL of water. The PCR products were visualized by agarose gel electrophoresis as previously described. The samples were quantified by Qubit (Bio-Sciences, Dublin, Ireland) and then collected in equimolar concentration. The sample pool (4 nM) was denatured using 0.2 N NaOH and subsequently diluted to 4pM and combined with PhiX 4p M. The samples were sequential via the MiSeq platform using 2 × 300 V3 kit cycles following the standard Illumina protocol [22–24].
2.7. Bioinformatics Analyses
Raw sequencing data were demultiplexed and FastQ were analyzed by using Qiime2 pipeline. Briefly, FastQ reads were trimmed to remove Illumina adapters and nonbiological primer sequences and then quality filtered. Amplicon Sequence Variants (ASVs) and chimera removing were performed by DADA2 algorithm. Taxonomic annotation was obtained by using VSearch and SILVA 132 database. Final data were preprocessed removing mitochondrial sequences and taxa represented under 0.01%. Statistical analysis of microbiota diversity was performed in R studio (https://www.rstudio.com/; version 4.0.2) using phyloseq package. Alpha diversity was evaluated by observed richness, Shannon index, and Pielou's evenness on rarefied data. Statistical significance for each time point of the single patient was assessed by Kolmogorov-Smirnov tests, assuming significant results with a p < 0.05.
3. Results
3.1. Culturomics
Through “culturomics,” 60 bacterial species (data not shown) from the stool of the healthy donors have been isolated and collected. Among these, 13 bacterial strains (Table 1) with different microbial properties were selected in order to create a bacterial solution to be infused in CDI patients. Antibiotic susceptibility tests were performed by triplicate E-test on Bacteroides strains and valuated by EUCAST guidelines.
Table 1.
List of bacterial strains isolated by culturomics and relative concentrations in BC and MIC values obtained by Epsilon tests performed in triplicate. MER: meropenem; CLI: clindamycin; MRD: metronidazole; TZP: piperacillin-tazobactam; not applicable: there are no EUCAST clinical breakpoints for these strains.
| Bacterial strain | Concentration (CFU/mL) | MIC values |
|---|---|---|
| Acidaminococcus intestini | 5 × 108 | Not applicable |
| Bacteroides fragilis | 5 × 108 | MER 1 S CLI 64 R MRD 1 S TZP 4 S |
| Bacteroides ovatus | 5 × 108 | MER 0.25 S CLI 4 S MRD 8 R TZP 4 S |
| Bacteroides uniformis | 5 × 108 | MER 0.25 S CLI 2 S MRD 4 S TZP 4 S |
| Bifidobacterium longum | 5 × 108 | Not applicable |
| Clostridium scindens | 5 × 108 | Not applicable |
| Lactobacillus casei | 5 × 108 | Not applicable |
| Lactobacillus gasseri | 5 × 108 | Not applicable |
| Lactobacillus rhamnosus | 5 × 108 | Not applicable |
| Lactobacillus parabuchneri | 5 × 108 | Not applicable |
| Parabacteroides distasonis | 5 × 108 | Not applicable |
| Propionibacterium avidum | 5 × 108 | Not applicable |
| Ruminococcus gnavus | 5 × 108 | Not applicable |
3.2. Clinical Outcome
The patients were monitored two hours following the infusion, and no adverse events were noted. Subsequently, patients were evaluated one week after procedure by anamnestic visit in which no complications such as diarrheal discharge, fever, or abdominal pain were reported. The clinical evaluation was carried out up to three months after the infusion giving positive results.
3.3. Phylum Modulation
Figure 3 shows the time-course modulation of the phyla in PZ 1. Before FMT (T0), its gut microbiota was mainly characterized Bacteroidetes (72%). Firmicutes and Proteobacteria were present with a relative abundance of 12% and 10%, respectively. Verrucomicrobia at T0 were present in percentages close to zero (0.01%). At T1 (7 days), there is a series of changes in the PZ1 microbiota. Specifically, Bacteroidetes underwent a decrease of 25% reaching 47% followed by an increase of Firmicutes (23%) and Verrucomicrobia (from 0.01% to 22%). In the subsequent time points, there appeared a stabilization of the intestinal populations in which Bacteroidetes and Firmicutes (63% and 33%) increased and the Proteobacteria reached minimum values (from 10% at T0 to 4% at T4).
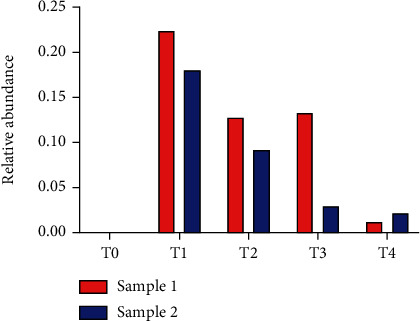
Figure 3.
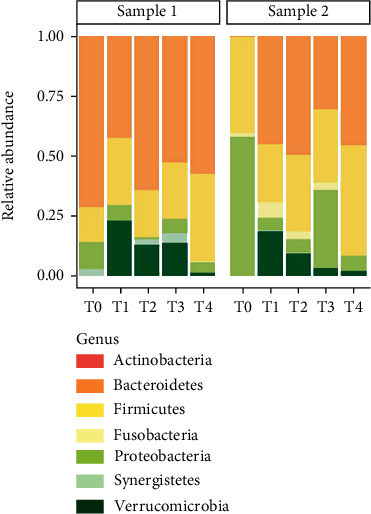
Relative abundance at phylum level in PZ 1 (sample 1) and PZ 2 (sample2).
Regarding the FMT, PZ 2 showed a gut microbial pattern characterized by a strong abundance of Proteobacteria (60%) and Firmicutes (40%) and a significant deficiency of Bacteroidetes (0.05%) and Verrucomicrobia (0.02%). After seven days, Proteobacteria underwent a decline from 60% to 5%, while Bacteroidetes increased to almost 50% of the relative abundance accompanied by an implementation of Verrucomicrobia (17%). Three months after infusion, microbiota appeared stabilized with a prevalence of Bacteroidetes and Firmicutes (50% and 46%).
3.4. Richness and Biodiversity
Figure 4 shows the number and the distribution of microbial species detected in the samples of the two patients at the different time points. At T0, PZ 1 (sample 1) and PZ 2 (sample 2) were characterized by 27 and 46 species, respectively. In the subsequent time points, biodiversity increased passing up to 70 species detected at T4 for both patients (Figure 4(a)). Moreover, diversity along species was evaluated with Shannon and evenness index (Figures 4(b) and 4(c)). Finally, Figure 5 describes the relative abundance of beneficial bacteria such as Akkermansia muciniphila. This bacterium was absent at T0 in both patients. After infusion (in detail at T1), Akkermansia muciniphila raised concentrations of 22% in patient 1 and 17.5% in patient 2.
Figure 4.
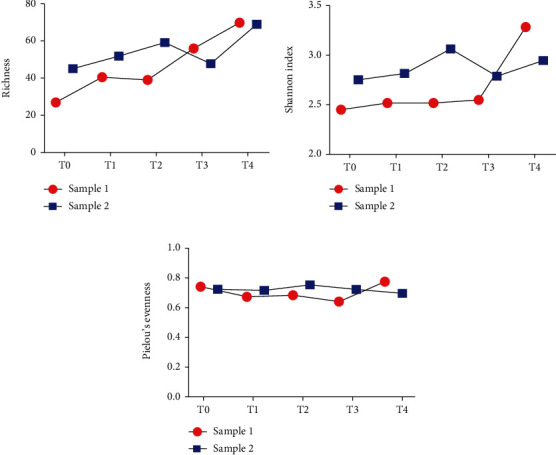
Alpha diversity analysis of fecal bacterial communities after fecal microbiota transplantation. Species richness (a), Shannon diversity index (b), and equitability, as Pielou's evenness values (c) were compared among T0 (before fecal transplantation) and T1-3 (after fecal microbiota transplantation).
Figure 5.
Relative abundance of Akkermansia muciniphila in PZ1 (sample 1) and PZ 2 (sample 2).
4. Discussion
The Clostridioides difficile infection is a nosocomial infection due to prolonged exposure to antibiotics [25, 26]. In the last decade, the CDI is involving also younger people not undergoing antibiotic therapies [7]. The clinical severity ranges from mild to severe diarrhea up to leading to toxic megacolon and intestinal perforation [27–30].The pathogenesis of CDI depends not only on toxins production but also on the intestinal microenvironment. In fact, recently, several studies have shown how different metabolites and several groups of microorganisms may contribute to the inflammatory state described in CDI [31].
Specifically, it has been shown that C. difficile spores' germination is sensitive to the presence of primary bile acids such as cholate and taurocholate produced by the liver and secondary bile acids such as deoxycholate. In fact, these molecules are abundant in healthy subjects compared to subjects with recurrent infection. On the other hand, the inflammatory state of CDI and other inflammatory bowel disorders such as UC and IBD is triggered by the activity and overgrowth of certain microbial groups. It is evident how sulfate-reducing bacteria (SRB), a small group of anaerobic bacteria including Desulfovibrio desulfuricans, appear overexpressed in patients with inflammatory syndromes. These bacteria, being resistant to broad-spectrum antibiotics, may overgrow in patients treated with antibiotic therapy, contributing to intestinal inflammation through the production of high levels of H2S or through their cytotoxic activity against epithelial cells [32, 33]. In this scenario, FMT is thriving as a valid therapeutic approach to CDI with an 80% efficacy when antibiotic therapies fail [5]. The preparation of fresh or frozen fecal suspensions requires the constant and periodic presence of donors. In addition, these donors must result negative for a series of serological and microbiological screening tests [8]. Moreover, stool sample must be processed within six hours after defecation in order to preserve anaerobes [8, 10]. All these aspects make the procedure laborious and poorly standardized. Furthermore, it is essential to know in detail the bacterial composition of the suspension to be infused into the recipient in order to increase the efficacy and especially the safety of the treatment. All these mentioned technical, logistical, and bureaucratic criticalities mean that not all healthcare facilities can offer their patients this important therapeutic option. In this study, our aim was to develop a “home-made” bacterial suspension, defined “Bacterial Consortium,” bypassing all the lacks of classical FMT procedure. In 2013, Petrof et al. have worked on formulating a synthetic ecosystem called RePOOPulate, consisting of a series of bacterial strains previously tested for antibiotic resistance [34]. This preparation was infused by colonoscopy in two patients affected by recurrent CDI with the clinical resolution in both cases [35].
In our work, the first step was the selection of “beneficial bacteria” from the gut of healthy donors. Culturomics was the main strategy to isolate and collect bacterial strains. Of course, this method is very laborious and provides long time to result. But, on the other hand, a very interesting strategy is to describe microbial populations in a specific body district [17, 34]. In fact, thanks to a variety of enrichment factors and growth conditions, it is possible detecting microbial species present in low concentrations [17]. A profoundly different approach is metagenomics. This method is characterized by many strengths and weaknesses. Specifically, metagenomics allows the inclusion of a large number of sample and a “relative” rapid analysis in comparison to culturomics. But, the most crucial weaknesses are represented by (i) the depth limit in detection, (ii) minority populations are insufficiently detected, and (iii) the impossibility to discriminate between live bacteria and transient DNA [36]. This pilot study shows that a “synthetic” suspension may be a valid alternative option to the use of feces from a healthy donor. Considering the definition of recurrent CDI as an infection that recurs within 8 weeks after the onset of a previous episode, both patients were monitored up to three months after the procedure. They did not show diarrhea episodes, gastrointestinal symptoms, and positive laboratory tests during the entire follow up (7, 15, 30, and 90 days). In addition, metagenomics analysis showed a marked gut microbiota shaping after infusion. Specifically, a resettlement of the microbial populations was observed in both patients as demonstrated by the negative result for C. difficile toxin detection and by an increased number of detected bacterial species. Among these species appeared both the strains infused with BC and other species, absent or low concentrated before infusion, such as Akkermansia muciniphila. This bacterium stimulates communication between the bacteria in the intestinal microbiota and improves the function of the gut barrier by enhancing immune response. In addition, it is able to influence the metabolism of sugars and fats generating molecules acting as postbiotics [37]. Moreover, in both patients, the percentage of the phylum Proteobacteria appears dramatically reduced after infusion. The Proteobacteria group is mainly represented by Gram negative bacteria which contribute to the typical CDI inflammatory status [38]. The increase of species reported in Figure 3 is an evidence of a “microbial awakening” in which gut microbiota reverts to eubiosis conditions with an increment of the percentage of Firmicutes and Bacteroidetes. These data suggest a modulatory and stimulatory action of the “Bacterial Consortium” on the resident microbiota damaged by the pathological action of C. difficile. The use of a synthetic preparation, composed exclusively of bacteria, reveals numerous potential advantages. First of all, knowing the real composition of the infused suspension offers more control over procedure and consequently a wider safety standard compared to the infusion of fecal matter. Furthermore, knowing the bacterial components infused ensures a high degree of methodological reproducibility. The efficiency of the classic FMT is strongly influenced by the sampling and delivery phase of the feces in the laboratory. Using cultivable bacteria could allow to bypass this logistic problem and to have stable bacterial strains whenever necessary.
5. Conclusion
This study shows some limits, especially the restricted number of recruited patients, but the principal aim of this explorative pilot study was the development of efficacious alternative to FMT. Our future proposal will be enrolling more patients in order to extend this therapeutic option not only to CDI but also for other gastrointestinal disorders. In the personalized medicine era, “Bacterial Consortium,” supported by culturomics and metagenomics, could be a revolutionary choice to treat patients with intestinal dysbiosis and hopefully extraintestinal disorders.
Data Availability
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the local Ethics Committee (protocol code 0021125/16).
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
GQ, GI, GC, and LM contributed to the study conception. GQ, LM, and AA drafted the manuscript. AG, GF, CA, and FI performed material preparation and data collection. GC, GI, SB, and MS contributed in patient's recruiting and clinical management. DF performed metagenomics and statistical analysis. LM and AA were the supervisors in writing and corrections. Giovanni Cammarota and Luca Masucci. These authors contributed equally to this work.
References
- 1.Rinninella E., Raoul P., Cintoni M., et al. What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms . 2019;7(1):14–22. doi: 10.3390/microorganisms7010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chattopadhyay I., Dhar R., Pethusamy K., et al. Exploring the role of gut microbiome in colon cancer. Applied Biochemistry and Biotechnology . 2021;193(6):1780–1799. doi: 10.1007/s12010-021-03498-9. [DOI] [PubMed] [Google Scholar]
- 3.Quaranta G., Sanguinetti M., Masucci L. Fecal microbiota transplantation: a potential tool for treatment of human female reproductive tract diseases. Frontiers in Immunology . 2019;10:p. 2653. doi: 10.3389/fimmu.2019.02653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall I. C., O’Toole E. Intestinal flora in new-born infants. American Journal of Diseases of Children . 1935;49(2):390–402. doi: 10.1001/archpedi.1935.01970020105010. [DOI] [Google Scholar]
- 5.Ianiro G., Masucci L., Quaranta G., et al. Randomised clinical trial: faecal microbiota transplantation by colonoscopy plus vancomycin for the treatment of severe refractory Clostridium difficile infection—single versus multiple infusions. Alimentary Pharmacology & Therapeutics . 2018;48(2):152–159. doi: 10.1111/apt.14816. [DOI] [PubMed] [Google Scholar]
- 6.Lessa F. C., Winston L. G., Clifford McDonald L. Burden ofClostridium difficileinfection in the United States. The New England Journal of Medicine . 2015;372(9):825–834. doi: 10.1056/NEJMoa1408913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He M., Miyajima F., Roberts P., et al. Emergence and global spread of epidemic healthcare-associated Clostridium difficile. Nature Genetics . 2013;45(1):109–113. doi: 10.1038/ng.2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cammarota G., Ianiro G., Tilg H., et al. European consensus conference on faecal microbiota transplantation in clinical practice. Gut . 2017;66(4):569–580. doi: 10.1136/gutjnl-2016-313017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aron-Wisnewsky J., Clément K., Nieuwdorp M. Fecal microbiota transplantation: a future therapeutic option for obesity/diabetes? Current Diabetes Reports . 2019;19(8):p. 51. doi: 10.1007/s11892-019-1180-z. [DOI] [PubMed] [Google Scholar]
- 10.Quaranta G., Fancello G., Ianiro G., et al. Laboratory handling practice for faecal microbiota transplantation. Journal of Applied Microbiology . 2020;128(3):893–898. doi: 10.1111/jam.14522. [DOI] [PubMed] [Google Scholar]
- 11.Ramai D., Zakhia K., Ofosu A., Ofori E., Reddy M. Fecal microbiota transplantation: donor relation, fresh or frozen, delivery methods, cost-effectiveness. Annals of Gastroenterology . 2019;32(1):30–38. doi: 10.20524/aog.2018.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filip M., Tzaneva V., Dumitrascu D. L. Fecal transplantation: digestive and extradigestive clinical applications. Clujul Medical . 2018;91(3):259–265. doi: 10.15386/cjmed-946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cammarota G., Ianiro G., Gasbarrini A. Fecal microbiota transplantation for the treatment of Clostridium difficile infection. Journal of Clinical Gastroenterology . 2014;48(8):693–702. doi: 10.1097/MCG.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 14.Quera R., Espinoza R., Estay C., Rivera D. Bacteremia as an adverse event of fecal microbiota transplantation in a patient with Crohn's disease and recurrent Clostridium difficile infection. Journal of Crohn's & Colitis . 2014;8(3):252–253. doi: 10.1016/j.crohns.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Brandt L., Aroniadis O., Mellow M., et al. Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection. The American Journal of Gastroenterology . 2012;107(7):1079–1087. doi: 10.1038/ajg.2012.60. [DOI] [PubMed] [Google Scholar]
- 16.Van Nood E., Vrieze A., Nieuwdorp M., et al. Duodenal infusion of donor feces for recurrentClostridium difficile. The New England Journal of Medicine . 2013;368(5):407–415. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- 17.Lagier J. C., Dubourg G., Million M., et al. Culturing the human microbiota and culturomics. Nature Reviews. Microbiology . 2018;16(9):540–550. doi: 10.1038/s41579-018-0041-0. [DOI] [PubMed] [Google Scholar]
- 18.Martellacci L., Quaranta G., Fancello G., et al. Characterizing peri-implant and sub-gingival microbiota through culturomics. First isolation of some species in the oral cavity. A pilot study. Pathogens . 2020;9(5):p. 365. doi: 10.3390/pathogens9050365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kambouris M. E., Pavlidis C., Skoufas E., et al. Culturomics: a new kid on the block of OMICS to enable personalized medicine. Omics: A Journal of Integrative Biology . 2018;22(2):108–118. doi: 10.1089/omi.2017.0017. [DOI] [PubMed] [Google Scholar]
- 20.Bilen M. Strategies and advancements in human microbiome description and the importance of culturomics. Microbial Pathogenesis . 2020;149, article 104460 doi: 10.1016/j.micpath.2020.104460. [DOI] [PubMed] [Google Scholar]
- 21.Lin H., Guo Q., Wen Z., et al. The multiple effects of fecal microbiota transplantation on diarrhea-predominant irritable bowel syndrome (IBS-D) patients with anxiety and depression behaviors. Microbial Cell Factories . 2021;20(1):p. 233. doi: 10.1186/s12934-021-01720-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caporaso J. G., Lauber C. L., Walters W. A., et al. Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. The ISME Journal . 2012;6(8):1621–1624. doi: 10.1038/ismej.2012.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pichler M., Coskun Ö. K., Ortega-Arbulú A. S., et al. A 16SrRNAgene sequencing and analysis protocol for the Illumina MiniSeq platform. Microbiology . 2018;7(6, article e00611) doi: 10.1002/mbo3.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Silverman M. A., Green J. L. Insight into host-microbe interactions using microbial flow cytometry coupled to next-generation sequencing. Journal of the Pediatric Infectious Diseases Society . 2021;10(Supplement_4):S106–S111. doi: 10.1093/jpids/piab092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goelz H., Wetzel S., Mehrbarzin N., Utzolino S., Häcker G., Badr M. T. Next- and third-generation sequencing outperforms culture-based methods in the diagnosis of ascitic fluid bacterial infections of ICU patients. Cell . 2021;10(11):p. 3226. doi: 10.3390/cells10113226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yoon H., Shim H. I., Seol M., et al. Factors related to outcomes of fecal microbiota transplantation in patients withClostridioides difficileinfection. Gut Liver . 2021;15(1):61–69. doi: 10.5009/gnl20135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hajiagha M. N., Taghizadeh S., Asgharzadeh M., et al. Gut microbiota and human body interactions; its impact on health: a review. Current Pharmaceutical Biotechnology . 2022;23 doi: 10.2174/1389201022666210104115836. [DOI] [PubMed] [Google Scholar]
- 28.Chen C. C., Chiu C. H. Current and future applications of fecal microbiota transplantation for children. Biomedical Journal . 2022;45(1):11–18. doi: 10.1016/j.bj.2021.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baunwall S. M. D., Terveer E. M., Dahlerup J. F., et al. The use of faecal microbiota transplantation (FMT) in Europe: a Europe-wide survey. The Lancet Regional Health-Europe . 2021;9, article 100181 doi: 10.1016/j.lanepe.2021.100181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jouhten H., Ronkainen A., Aakko J., et al. Cultivation and genomics prove long-term colonization of donor's bifidobacteria in recurrent Clostridioides difficile patients treated with fecal microbiota transplantation. Frontiers in Microbiology . 2020;11 doi: 10.3389/fmicb.2020.01663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Masucci L., Quaranta G. Fecal microbiota transplantation: what’s new? Microorganisms . 2022;10(1):p. 23. doi: 10.3390/microorganisms10010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abbas A., Zackular J. P. Microbe-microbe interactions during _Clostridioides difficile_ infection. Current Opinion in Microbiology . 2020;53:19–25. doi: 10.1016/j.mib.2020.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ribeiro Figliuolo V., Coutinho-Silva R., Melo Coutinho C. M. L. Contribution of sulfate-reducing bacteria to homeostasis disruption during intestinal inflammation. Life Sciences . 2018;215(215):145–151. doi: 10.1016/j.lfs.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Petrof E. O., Gloor G. B., Vanner S. J., et al. Stool substitute transplant therapy for the eradication of Clostridium difficile infection: ‘RePOOPulating’ the gut. Microbiome . 2013;1(1) doi: 10.1186/2049-2618-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Allen-Vercoe E., Petrof E. O. Artificial stool transplantation: progress towards a safer, more effective and acceptable alternative. Expert Review of Gastroenterology and Hepatology . 2013;7(4):291–293. doi: 10.1586/egh.13.16. [DOI] [PubMed] [Google Scholar]
- 36.Bilen M., Dufour J. C., Lagier J. C., et al. The contribution of culturomics to the repertoire of isolated human bacterial and archaeal species. Microbiome . 2018;6(1):p. 94. doi: 10.1186/s40168-018-0485-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dubourg G., Baron S., Cadoret F., et al. From culturomics to clinical microbiology and forward. Emerging Infectious Diseases . 2018;24(9):1683–1690. doi: 10.3201/eid2409.170995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Macchione I. G., Lopetuso L. R., Ianiro G., et al. Akkermansia muciniphila: key player in metabolic and gastrointestinal disorders. European Review for Medical and Pharmacological Sciences . 2019;23(18):8075–8083. doi: 10.26355/eurrev_201909_19024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.


