Abstract
AIM
To investigate the impact of the COVID-19 pandemic on core and higher breast radiology training in the UK from the perspective of trainees and new consultants.
MATERIALS AND METHODS
A survey comprising 25 questions was distributed to UK radiology trainees via the regional Junior Radiologists Forum representatives under the auspices of the British Society of Breast Radiology (BSBR).
RESULTS
Sixty-nine eligible responses were received representing all UK training regions. Fifty-five per cent of respondents completing either a core or higher breast rotation felt that the pandemic had a negative effect on their breast training. There was an overall reduction in exposure to the key breast imaging methods when rotations took place during the pandemic. Completing a core breast rotation during the pandemic was less likely to attract trainees to higher breast training. Three out of four breast radiology consultants in their first year after receiving their Certificate of Completion of Training (CCT) felt the pandemic reduced their preparedness for becoming consultants. Positive outcomes included the increased use of online educational resources and remote multidisciplinary meetings.
CONCLUSIONS
As well as having a negative impact on breast radiology training overall, the pandemic has had a detrimental effect on attracting trainees to breast radiology as a future career. It is of key importance that trainees have a positive core breast rotation as this experience appears central to many trainees' decisions to pursue higher breast training. Increased use of online learning resources has also been positively received and is a valuable approach to learning that can be maintained in the longer term.
Introduction
The disruption of clinical services resulting from the COVID-19 pandemic has been significant and widespread.1 As a consequence of prioritising resources towards frontline acute care, many clinical and ancillary services deemed non-essential have been suspended, including elective procedures, outpatient clinics, and the teaching and training of healthcare professionals. A survey by the General Medical Council has found that postgraduate medical training across all specialties, including clinical radiology, has been disrupted by the pandemic.2 Similarly, a dedicated survey of radiology trainees within a single deanery found a reduction in trainee workload,3 and a survey of the Royal College of Radiologists' (RCR) Junior Radiologists Forum (JRF) reported a decrease in the amount of local and regional teaching for radiology trainees across the UK, and showed that trainees across 76% of training programmes were redeployed to hospital wards at some point.4 Added to this, the FRCR (Fellowship of the Royal College of Radiologists) postgraduate examinations were temporarily suspended.
Although the impact on radiology training has been an unavoidable consequence of the COVID-19 crisis, its effects could be long-lasting; the clinical radiology workforce is already deplete, so maintaining training is critical to ensure the uninterrupted support and development of the highly pressurised imaging services and to avoid further exacerbating the perennial shortfall of clinical radiologists nationwide.5 Breast radiology specifically suffers from a chronic workforce crisis that shows no imminent signs of improving.5 Although there is evidence to show the pandemic has resulted in an overall reduction in subspecialty radiology training,3 the effect on training in individual specialist interest areas has not yet been investigated.
The aim of this study was to investigate the impact of the COVID-19 pandemic on core and higher breast radiology training across the UK from the perspective of trainees and new consultants. Experiences of those who completed their rotations before the pandemic were compared with those who completed it during the pandemic. As well as investigating how training itself was impacted, the survey asked how this affected the likelihood that core trainees might pursue higher training, as well as asking higher trainees in breast radiology and new consultant breast radiologists how this has affected their preparedness for becoming a consultant.
Materials and methods
An online survey comprising 25 questions (Electronic Supplementary Material Appendix S1) was designed using SurveyMonkey and was distributed to UK radiology trainees via the regional JRF representatives under the auspices of the British Society of Breast Radiology (BSBR). Questions 22 and 23 relate to awareness of the BSBR and whether respondents had accessed links to any educational resources or learning modules available on the BSBR website, because these are not directly related to the impact of the pandemic on training, in the interests of relevance and space limitation these are not discussed further.
The survey opened in May 2021 and remained active for 8 weeks. Participation was incentivised by offering three prizes of Amazon vouchers (£100, £50 and £25). Winners were drawn at random. Ethical approval was gained from the University of Sunderland Research Ethics Group.
Results
Response rate
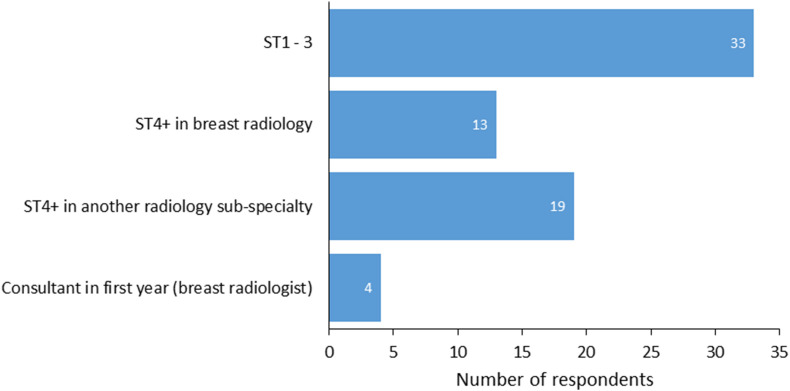
A total of 75 responses were received; six were excluded because of incomplete responses, leaving 69 for subsequent analysis. Of these, 65 were received from current radiology trainees, and four were from UK-based breast radiologists who completed their specialty training in the past year (i.e., having spent some time in training during the pandemic); overall, both core trainees and higher trainees, either in specialist breast training or another specialist area, were well represented as a proportion of all respondents (Fig 1 ), with 48% of respondents in core training (33/69), 46% in higher training (32/69); 13 in breast higher training and 19 in another specialist interest area), and 6% breast radiology consultants in their first year receiving their Certificate of Completion of Training (CCT; 4/69). At least one response was received from each training region (Table 1 ; note that the London training schemes were grouped together as one, as were the Scottish schemes).
Figure 1.
Number of responses by training grade (n=69).
Table 1.
Distribution of respondents by training region.
| Defence Postgraduate Medical Deanery | 0 |
| East Midlands | 5 |
| East of England | 3 |
| Kent, Surrey & Sussex | 1 |
| London | 2 |
| North East and North Cumbria | 15 |
| North West | 11 |
| Northern Ireland | 2 |
| Scotland | 8 |
| South West | 7 |
| Thames Valley | 4 |
| Wales | 3 |
| Wessex | 1 |
| West Midlands | 1 |
| Yorkshire and the Humber | 6 |
| Total | 69 |
Note that the London training schemes were grouped together as one, as were the Scottish training schemes.
Impact of COVID-19 on training experience and workload
Overall, 26% of respondents (18/69) were redeployed to other hospital departments at some point during the pandemic (data not shown); 78% of those redeployed (14/18) were core trainees, with the remainder higher trainees (4/18). The core trainees who were redeployed represented 42% of all core trainee respondents (14/33). None of the breast radiology consultants in their first year post-CCT were redeployed as trainees. Overall at least one respondent was redeployed from six of the 16 regions (38%).
Eighty-six per cent of respondents (59/69) reported having completed a core breast rotation at some point before or during the pandemic; 36% (25/69) completed a core rotation before the pandemic, and 49% (34/69) completed one during the pandemic (data not shown). Reflecting the fact that some core trainees would have made the transition from core to higher training during the pandemic, and that some of the higher breast trainees would have made the transition to becoming a consultant, 13% of respondents (9/69) reporting being in higher breast training at some point before the beginning of the pandemic, with 22% of respondents (15/69) in higher breast training at some point during the pandemic.
To ascertain basic background information about training environments, all respondents were asked how many trainees typically work in their local breast unit in each rotation. Regarding core trainees, of the 69 respondents, three (4%) stated there were typically no core trainees, 55 (80%) said there were one or two, three (4%) said there were three or four, and eight (12%) said they were unsure. Regarding higher trainees, of the 69 respondents, 14 (20%) stated there were typically none, 38 (55%) said there were one or two, two (3%) said there were three or four, and 15 (22%) said they were unsure (data not shown).
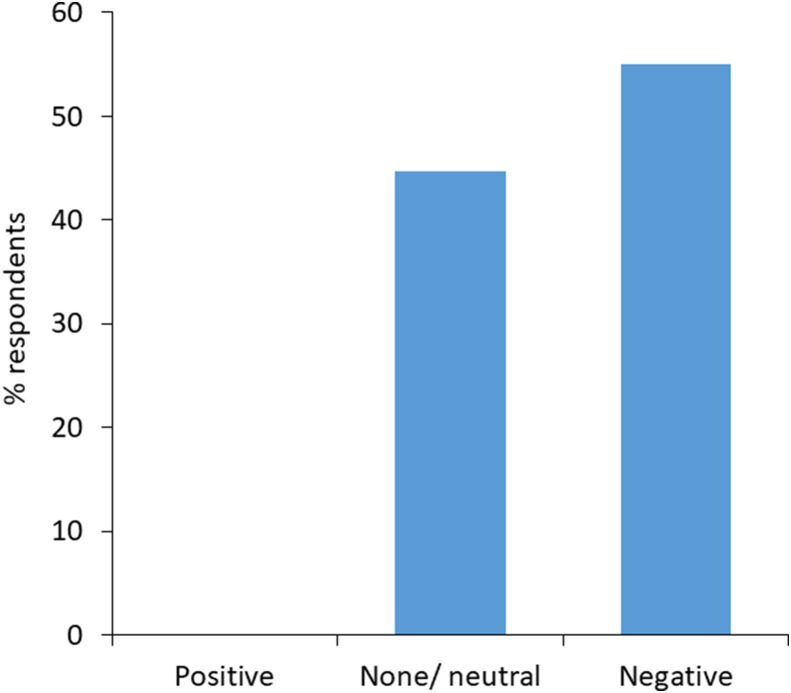
Before being asked in detail about the effects of the pandemic on their core or higher training experience, respondents were asked about the overall impact of the pandemic on their breast training as a whole, whatever their stage (Fig 2 ). Excluding 11 participants who selected “Not Applicable (I was not scheduled to be on a breast rotation at any point during the COVID-19 pandemic)”, 55% of respondents (32/58) felt that the pandemic had a negative effect on their breast training, and 45% (26/58) felt it had no impact. No respondents felt it had a positive impact.
Figure 2.
Overall impact of the pandemic on trainees' breast training as a whole, whatever their stage (n=58).
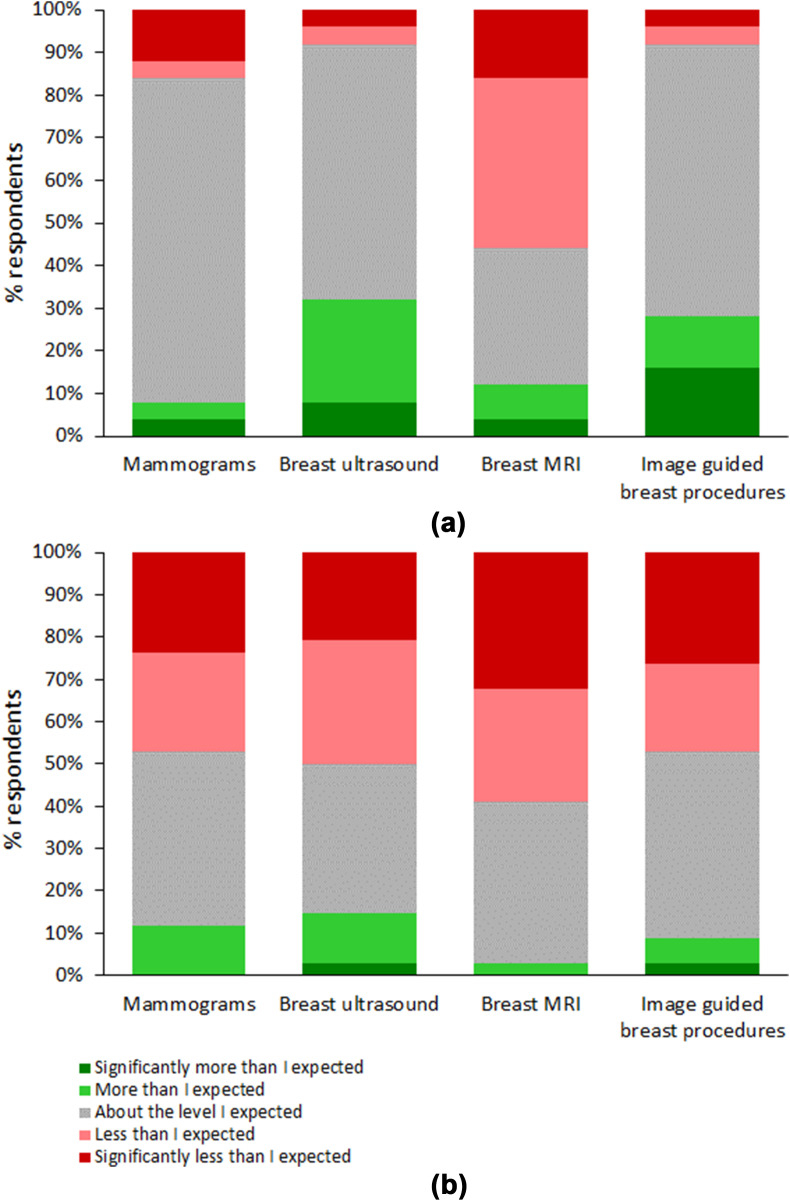
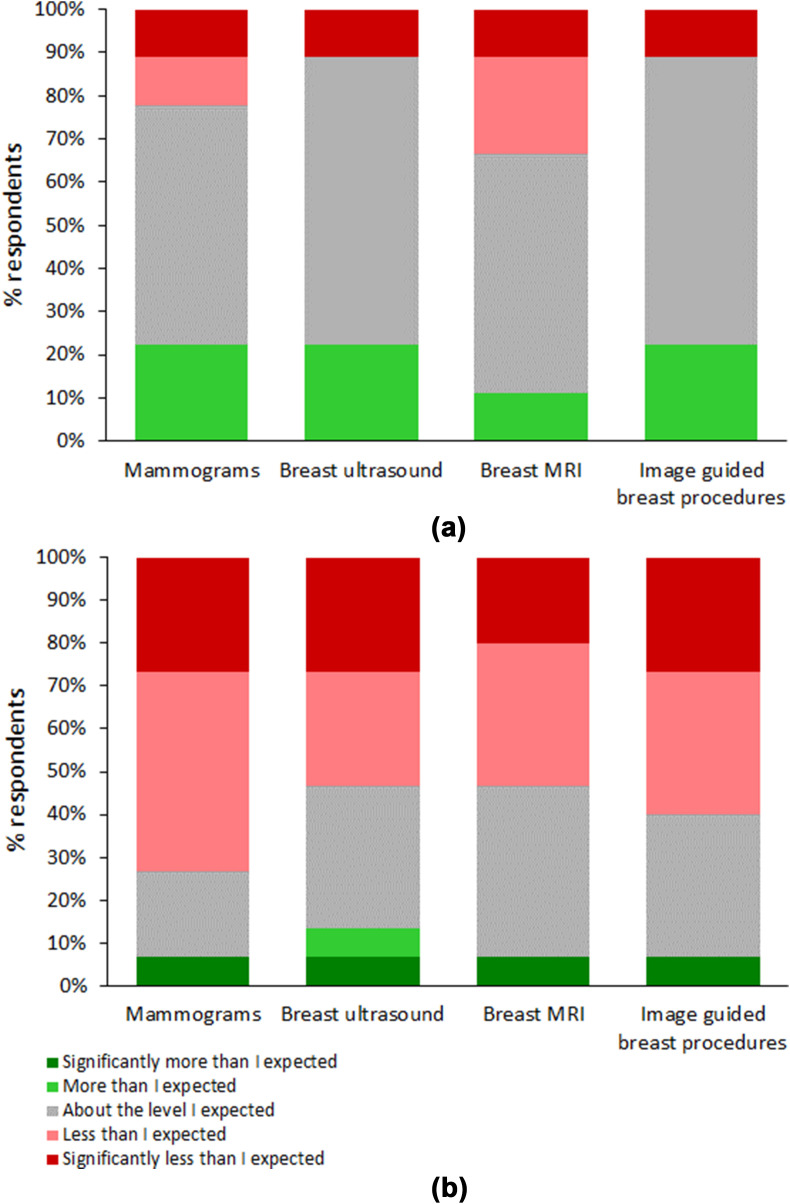
Respondents who had completed a core or higher breast rotation at any point were asked to rate their perceived exposure to four key breast imaging methods during their placements: mammography, ultrasound, magnetic resonance imaging (MRI), and image-guided breast procedures. The results are separated according to whether the rotation was at core (Fig 3 ) or higher level (Fig 4 ) and whether trainees completed their rotations before (Figure 3, Figure 4a) or during the pandemic (Figure 3, Figure 4b). For respondents completing core rotations during the pandemic, a greater proportion felt that their exposure to mammography, ultrasound, and image-guided breast procedures, was less than or significantly less than expected compared to when core rotations were completed before the pandemic (Fig 3). Overall a greater proportion of trainees reported their exposure to breast MRI was less than or significantly less than expected when compared to the other imaging methods, and this did not seem to change whether the rotation was done before or during the pandemic (Fig 3). For those doing higher breast training, a greater proportion of respondents doing their rotations during the pandemic felt that exposure to all four techniques was less or significantly less than expected compared to when rotations were done before the pandemic (Fig 4).
Figure 3.
Trainees' experiences of exposure to four key breast imaging techniques during their core breast rotations. (a) When core breast rotations were completed before the pandemic (n=25). (b) When core breast rotations were completed during the pandemic (n=34).
Figure 4.
Higher trainees' experiences of exposure to four key breast imaging methods during their breast rotations. (a) When higher breast rotations were completed before the pandemic (n=9). (b) When higher breast rotations were completed during the pandemic (n=15).
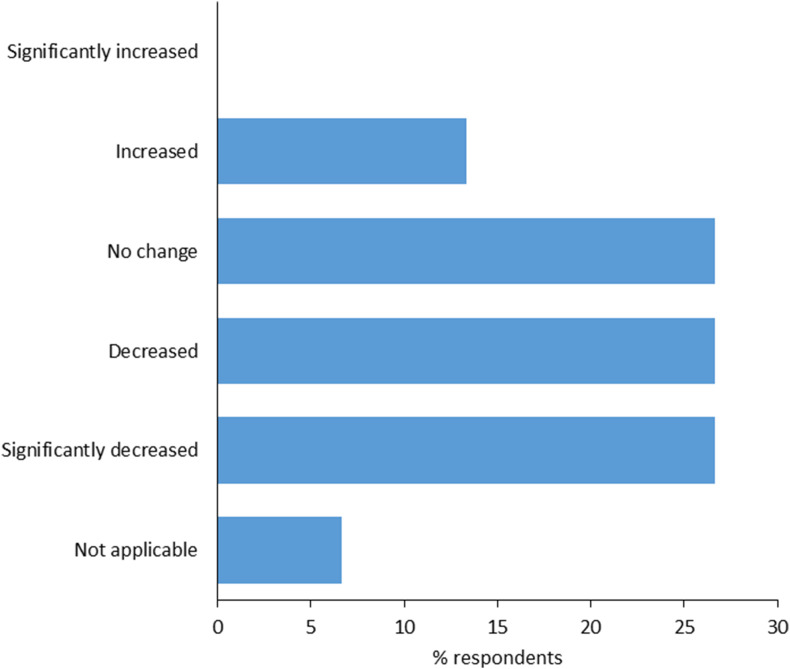
Of the 15 respondents who were on a higher breast rotation during the pandemic, 27% (4/15) felt their workload was unchanged compared to before the pandemic, 27% felt it decreased, and a further 27% felt it significantly decreased (Fig 5 ). Two respondents (13%) reported their workload increased, while none reported it has significantly increased. One respondent selected “Not Applicable”.
Figure 5.
Higher breast trainees' workload during the pandemic compared to before it (n=15).
Of all respondents who were on either a core or higher breast rotation during the pandemic, 47% (21/45) reported that breast multidisciplinary team (MDT) meetings continued as normal, 11% reported face-to-face meetings continued but were less frequent, 31% reported that face-to-face meetings stopped altogether, and 11% were unsure (data not shown). Eighty-two per cent (37/45) reported that there were opportunities for remote access to the MDT meetings, 4% reported there were no remote access opportunities, and 13% were unsure (data not shown). Of the same respondents completing either a core or higher breast rotation during the pandemic, 47% (21/45) reported that alternative non-face-to-face teaching methods were in place, such as Microsoft Teams, Star Leaf, or Zoom. Twenty-four per cent (11/45) reported there were no alternative teaching methods, 4% (2/45) were unsure, and 24% (11/45) gave no response (data not shown).
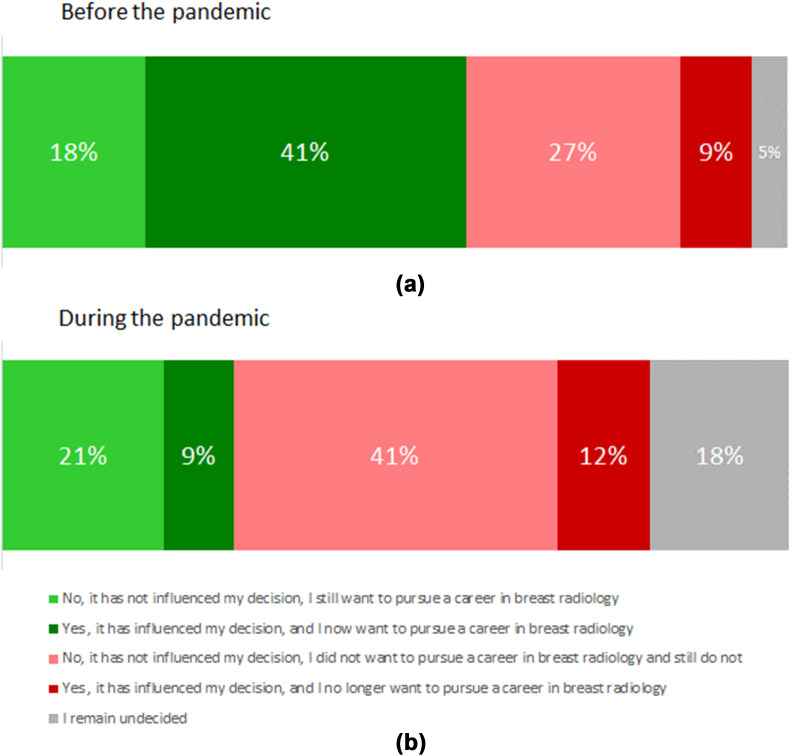
Impact on likelihood of pursuing a career in breast radiology
Core trainees were asked if their rotation before or during the pandemic impacted their decision to pursue a career in breast radiology (Fig 6 ). Of those who did their core rotation before the pandemic, 18% went into the rotation intending to pursue higher breast radiology, and their core rotation experience did not alter this decision; this proportion was similar for trainees completing their core rotation during the pandemic, increasing marginally to 21%, suggesting that any difference in core training experience during the pandemic compared to before it did not greatly influence career choice on those already planning on pursuing higher breast training. In contrast, whereas 41% of respondents who did their core rotation before the pandemic felt their core rotation experience positively changed their decision to now want to pursue breast radiology, this figure was just 9% in those who completed their core rotation during the pandemic. This 4.6-fold difference indicates that a significant opportunity to recruit trainees to breast radiology was lost because of the different experiences of core breast training during the pandemic compared to before it. This is also reflected in the finding that the proportion of respondents who had no intention of pursuing a career in breast radiology prior to their core rotation, and whose core rotation experience did not affect this decision, increased from 27 to 41% when their rotation took place during pandemic compared to before it, again suggesting that the core rotation experience has the potential to positively change trainees' minds about breast radiology, even when they previously had no intention of pursuing it, and that trainees' different experiences during the pandemic compared to before it, have to some extent negated this.
Figure 6.
Impact of completing a core rotation (a) before or (b) after the pandemic on likelihood of pursuing higher breast radiology training.
The proportion of trainees who wanted to pursue higher breast radiology training before their core rotation but changed their mind against it based on their core training experience was similar when the core rotation was completed before compared to during the pandemic, if anything showing a marginal increase from 9% to 12%. Just 5% of respondents who did their core breast rotation prior to the pandemic were undecided about their career choice upon completion of the rotation, compared to 18% who did their rotation during the pandemic, again indicating the potential for a positive core training experience to cement trainees' decisions (Fig 6).
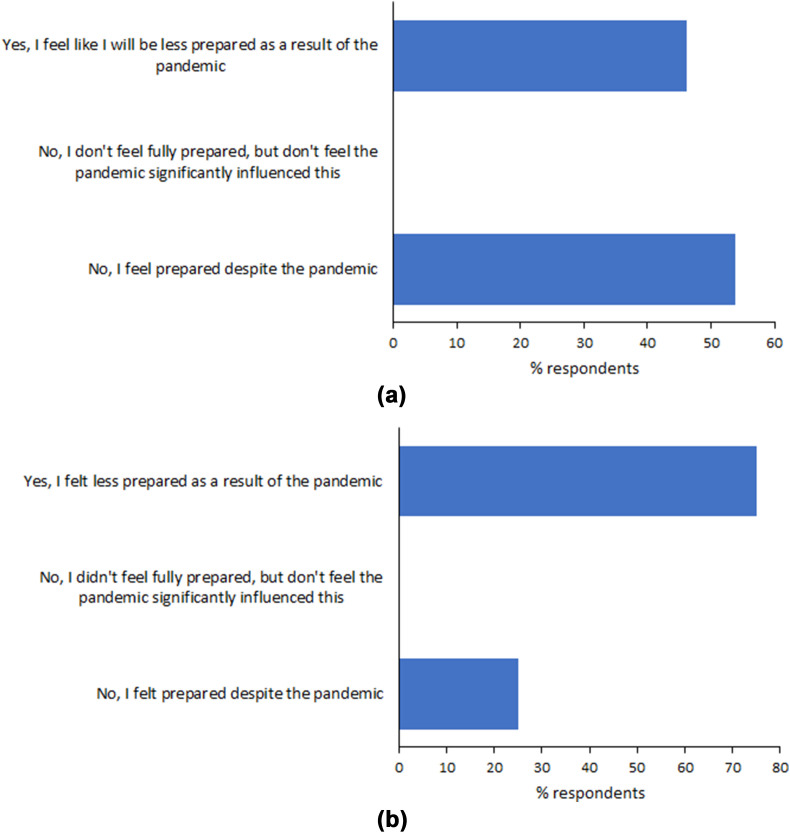
Impact on preparedness for becoming a consultant breast radiologist
Of 13 respondents currently higher breast training, six respondents (46%) felt they will be less prepared for becoming a consultant because of the COVID-19 pandemic, and seven (54%) felt they will be prepared despite the pandemic (Fig 7 a). Of the four consultant breast radiologists in their first year post-CCT, three respondents (75%) felt they were less prepared for becoming a consultant as a result of the pandemic, and one (25%) felt prepared despite the pandemic (Fig 7b).
Figure 7.
Impact of the pandemic on the perceived preparedness to become a consultant breast radiologist. (a) Higher breast radiology trainees (n=13). (b) Consultant breast radiologists in their first year post CCT (n=4).
Positive outcomes of COVID-19 pandemic on training and things that could have been done differently
In relation to breast radiology education, respondents were asked to provide details of any positive outcomes resulting from the pandemic, summarised in Table 2 . Notably, though perhaps unsurprisingly, the most common themes centred around the increased use/availability of online resources such as webinars, online teaching/educational material, online/remote MDTs, and virtual conferences.
Table 2.
Responses to the question: “Looking back to the beginning of the pandemic and thinking about your breast radiology education, has there been anything positive to come out of the pandemic experience, e.g., on-demand webinars, increased time to access educational resources, etc.?”
| Positive |
| Webinars (12) |
| Increased online teaching/educational material (12) |
| Online MDTs (6) |
| Audit/QIP opportunities increased (2) |
| More time (to be able to access resources) (3) |
| Virtual conferences (4) |
| Less commuting/travelling between sites (as a result of/allowing increased remote working/online resources) (2) |
| “More simulated biopsy experience, as less availability to practice on real patients” (1) |
| Negative |
| “No”/“none” (i.e. nothing positive to result from the pandemic) (9) |
| “Increased workload and had to home school children so no additional time to access educational resources” (1) |
| Mixed |
| “Remote courses definitely made them more accessible but it is not the same having all our teaching delivered virtually” (1) |
| “Unsure” (1) |
Common themes have been grouped. Verbatim responses are given in quotation marks. The number of comments per grouped theme/comment is given in parenthesis. Comments were received from 38 respondents; note that in some cases respondents made more than one comment and these have been counted separately.
In terms of what was felt could have been done differently, there was again emphasis placed on the use of online/remote facilities, such as more webinars, live online teaching, educational resources, remote MDM opportunities, and better home reporting capabilities, as well as being allocated more time to access these (Table 3 ). There were acknowledgements of less hands-on and case-based clinical exposure, with comments around needing more MRI, missed opportunities for reporting mammograms because of suspension of the screening programme, and there were suggestions for better opportunities for simulated biopsy practice. One respondent commented they had not had a core breast rotation during ST1 or ST2 (although they stated that they felt this was not necessarily as a result of the pandemic), and felt this was a missed opportunity for learning, and that they felt disadvantaged as a result. They also felt uninformed regarding the possibility of pursuing breast radiology as a career choice because they had not had any clinical experience to help them make that decision. There were also 13 respondents who felt that nothing could be done differently, with six respondents providing supporting comments, two acknowledging that it would have been hard doing things differently given the situation, and the others providing positive comments on the experiences they did have.
Table 3.
Responses to the question: “Again, looking back to the beginning of the pandemic and thinking about your breast radiology education, what do you think could have been done differently to support your breast education?”
| Things that could have been done differently |
| More webinars (2) |
| “National higher breast trainee webinars would also have been of value.” |
| More online (live) teaching sessions/case-based reviews (3) |
| More online educational resources (e.g. bank of mammograms) (1) |
| More effort into (in-person) teaching to help get the most out of the placement (1) |
| Better access to home workstations/reporting facilities (e.g. for mammography) (1) |
| More/better opportunities for simulated biopsy practice (2) |
| Remote access to the MDM (1) |
| Dedicated time to allow for viewing of webinars and completion of eLfH modules. (1) |
| “Needed clinical exposure. Could have had core breast radiology catch-up programmes nationally?” (1) |
| Other comments |
| Missed out on breast MRI (2) |
| “If the normal rota was not disrupted it would have given more time for attending webinars and using other resources. Also stopping screening significantly reduced mammo reading numbers.” (1) |
| Not had a core breast rotation at ST1 or 2, though not necessarily as a result of the pandemic, so have missed an educational opportunity and any opportunity to experience breast radiology before making career choice (1) |
| “Not sure” (2) |
| No |
| “No” (13) |
| Specific comments: “I was as well supported as I could be” |
| “With such little time to prepare I think it would have been difficult” |
| “Happy with training during pandemic” |
| “Nothing could be done. The trainees were redeployed to the wards” |
| “None, I had a near normal core breast rotation.” |
| “Nothing. It was great.” |
Common themes have been grouped. Verbatim responses are given in quotation marks. The number of comments per grouped theme/comment is given in parenthesis. Comments were received from 28 respondents; note that in some cases respondents made more than one comment and these have been counted separately.
Discussion
Like other specialty training areas, clinical radiology training been negatively impacted by the COVID-19 pandemic. Specifically, this survey demonstrates the effect on breast radiology training, with over half of the respondents confirming that the pandemic has had a negative impact on their breast training, whatever their stage. This appears to be the culmination of several factors.
Just over a quarter of all trainees in the dataset were redeployed to other areas at some point, a similar proportion to that found in a survey of radiology trainees within the Severn Deanery, where 24% of trainees had been redeployed.3 In the present dataset, 38% of the regions had at least one respondent redeployed, which is lower than that found in a survey of JRF representatives, where 76% of training programmes had redeployed trainees.4 The difference in values is likely to reflect the fact that the JRF survey was an overarching representation of whether any trainees in the respective training programmes had been redeployed, whereas the current survey reflects a snapshot of individual experiences, and, with only limited responses from each region, it is likely that the proportion of training regions in which trainees were redeployed is underrepresented. The present survey also pooled training programmes (e.g., from London and from Scotland) into a smaller number of regions, which may have affected the proportions; however, if anything this would have been expected to increase the apparent proportion of training regions in which trainees were redeployed.
What was not explored, as this was beyond the scope of this study, is where trainees were deployed to, for how long, and whether this was personal choice. Of the respondents across all training groups that were redeployed, 78% (14/18) were core trainees (representing 42% of all core trainee respondents; 14/33), and 22% (4/18) were higher trainees. What was also not explore was the proportion of the breast rotation that was missed by those who were redeployed, which would have been helpful in assessing the extent to which redeployment had a direct impact on breast training. Nevertheless, it is clear from those who did complete breast rotations during the COVID-19 crisis that the pandemic has had an overall negative impact on their training experience, with trainees overall gaining less than expected exposure to the key breast imaging techniques compared to those completing their rotations before the pandemic. This applied to both core and higher rotations. Interestingly, trainees' exposure to breast MRI in core rotations was overall less than expected whether the rotation was completed before or during the pandemic, which is perhaps something to be considered when delivering core rotations in the future.
The perceived negative impact of the pandemic on breast training also translated into trainees' confidence regarding becoming a consultant. Three of the four consultants in their first year felt less prepared as a result of the pandemic, and 46% of current higher trainees will also be less prepared for becoming a consultant.
Maintaining high quality training is critical in ensuring that trainees gaining their CCT feel well prepared for becoming consultants entering a chronically pressurised radiology workforce. The disruptions caused by the pandemic have therefore necessitated a change in the way training is delivered. One advantage in clinical radiology compared to many other specialties is that it is very amenable to the use of electronic learning resources,6 which can be used as an effective way to develop knowledge base7 and may offer opportunities to simulate clinical work. This, combined with the potential for remote reporting of real-life clinical imaging (where facilities are in place to allow this), can help mitigate some of the learning barriers encountered by reduced face-to-face contact as a result of COVID-19 measures. In the current survey, this was consistently raised as one of the positive outcomes from the pandemic, with increased use of webinars, online teaching/educational material, and remote MDT meetings all identified as valuable training resources. This supports the JRF survey funding,4 and is something that will no doubt continue to be used in the post-pandemic future. For breast radiology in particular, the National Breast Imaging Academy (NBIA) has recently set up an extensive, comprehensive e-learning platform, which provides online materials for remote learning in all aspects of breast imaging aimed at radiologists and other healthcare professionals at all stages of their learning.8
Despite this, because a significant proportion of the clinical work in breast radiology involves patient contact and the development of practical skills, remote resources, while hugely valuable, can only provide some of the learning opportunities needed to develop competencies in the specialty. Even the non-patient-facing reporting components of breast radiology, such as screen reading, may have to be done on-site depending on access to the NHS Breast Screening Service software and the requirement for strict reporting conditions, meaning that remote reporting options become very limited. This is likely to have been compounded further by the temporary suspension of the NHS Breast Screening Programme during the pandemic, something one respondent did comment on. Thus it is possible, although difficult to substantiate, that the disruption in breast training may not have been as well compensated for by remote learning as in some other areas.
One other key observation was the negative impact the pandemic has had on attracting core trainees to higher breast radiology, with those completing core breast rotations during the pandemic less likely to pursue higher training in breast radiology compared to those completing core rotations before the pandemic. For those embarking on their core breast training who had already decided on pursuing a career in breast radiology, the pandemic did not seem to change their opinion, but for trainees not previously considering a pursuing higher breast training, the timing of their core rotation made a big difference to their decision, with 4.6-fold more respondents changing their career decision towards pursuing breast radiology when their core rotation took place before the pandemic compared to when they did the rotation during the pandemic. Similarly, looking at things from a different viewpoint, the proportion of trainees who stated they had no intention of pursuing breast radiology prior to their core rotation and still did not want to pursue it after completing it increased 1.5-fold when their rotation took place during pandemic (41%) compared to before it (27%), again suggesting that trainees' core breast rotation experience has the potential to positively influence career decisions towards breast radiology. The notion of trainees' core rotation experience influencing their decision to pursue higher breast training was also addressed in a previous survey of UK radiology trainees, where 17% of respondents had said their core rotation positively changed their mind to pursue breast radiology when they had not previously considered it.9 In fact having had a “positive experience during [their] core rotation” was one of the top reasons why trainees pursuing higher breast training had chosen to do so, second only to having a “good level of patient contact” and being “interested in the subject”.9
As COVID-19 restrictions have eased and normal clinical services and specialty training have begun to resume, many of the negative effects of the pandemic will hopefully have been temporary; however, it should not be assumed that resumption of normal specialty training will alone be enough to restore interest in pursuing higher breast training. The findings of this survey highlight a significant window of opportunity to develop trainees' interest in pursuing higher breast training by providing a positive core training experience, something as trainers we have the power to influence.
Recruitment into breast radiology continues to present a critical workforce issue. Consultant breast radiologists were the most in-demand of all specialist interest areas in 2020,5 consistent with previous RCR census reports in recent years, with minimal growth in the number of consultants over the past 5 years (1% on average compared to 4% on average for the whole consultant radiology workforce) and a vacancy rate in 2020 of 8%. Furthermore, 24% of consultant breast radiologists are due to retire within 5 years, which is greater than the clinical radiology consultant average of 19%, with the census stating that “The shortage of breast CR [clinical radiology] consultants is highly likely to rise further over the next 5 years unless mitigating action is taken”.5 The year-on-year increase in demand for clinical breast services will only compound this problem. It is therefore more important than ever that trainees are given a positive experience during their breast rotations and given opportunities and encouragement to consider breast radiology as a potential career choice.
As with any survey, sample size and type are potential limiting factors. The response rate of 69 eligible participants represents just 4% of UK radiology trainees at the time the survey was conducted (information obtained by direct communication with the RCR on 21 March 2022); however, every reasonable effort was made to ensure that the survey was distributed to trainees across the country, and there was at least one respondent from every training region, accepting the limitation that the London and Scottish regions were respectively pooled. Achieving a good response rate is challenging at the best of times; not only does it rely on effective distribution, but at a time when trainees are busy with their own commitments, time-pressured, and may well be suffering from “survey overload”, completion of yet another survey may have been seen as an onerous task.
Conflict of interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Advisory Editor for Clinical Radiology – S Lowes, Y Graham, N Sharma, I Lyburn.
Acknowledgements
The authors thank the British Society of Radiology Executive Committee for supporting the study, as well as the specialty trainees and consultants who completed the survey.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.crad.2022.07.005.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Blumenthal D., Fowler E.J., Abrams M., et al. Covid-19 — implications for the health care system. N Engl J Med. 2020;383(15):1483–1488. doi: 10.1056/NEJMsb2021088. [DOI] [PubMed] [Google Scholar]
- 2.GMC National training survey. 2020. https://www.gmc-uk.org/-/media/documents/nts-results-2020–-summary-report_pdf-84371830.pdf Available at: [DOI] [PMC free article] [PubMed]
- 3.Veerasuri S., Vekeria M., Davies S.E., et al. Impact of COVID-19 on UK radiology training: a questionnaire study. Clin Radiol. 2020;75(11) doi: 10.1016/j.crad.2020.07.022. 877.e7-877.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fossey S., Ather S., Davies S., et al. Impact of COVID-19 on radiology training: royal College of radiologists Junior radiologists Forum national survey. Clin Radiol. 2021;76(7) doi: 10.1016/j.crad.2021.03.013. 549.e9-549.e15. [DOI] [PubMed] [Google Scholar]
- 5.Royal College of Radiologists UK workforce census. 2020. https://www.rcr.ac.uk/system/files/publication/field_publication_files/clinical-radiology-uk-workforce-census-2020-report.pdf Report. Available at:
- 6.Pervez A., McCurdie F., Poon D. The pursuit of radiology training in times of a pandemic. BJR Open. 2020;2(1):20200039. doi: 10.1259/bjro.20200039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Upadhyay N., Wadkin J.C.R. Can training in diagnostic radiology be moved online during the COVID-19 pandemic? UK trainee perceptions of the Radiology-Integrated Training Initiative (R-ITI) e-learning platform. Clin Radiol. 2021;76(11):854–860. doi: 10.1016/j.crad.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Breast Imaging Academy Academy Online e-learning programme. https://www.e-lfh.org.uk/programmes/national-breast-imaging-academy/
- 9.Lowes S., Bydder M., Sinnatamby R. A national survey exploring UK trainees’ perceptions, core training experience, and decisions to pursue advanced training in breast radiology. Clin Radiol. 2017;72(11):991.e1–991.e13. doi: 10.1016/j.crad.2017.06.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.