Abstract
Objectives:
To examine how the COVID-19 pandemic affected driving and health outcomes in older adults.
Methods:
We compared Advancing Understanding of Transportation Options (AUTO) study participants enrolled before (December 2019 to March 2020) vs. during the pandemic (May 2020 to June 2021). Participants were English-speaking, licensed drivers (≥70 years) who drove weekly and had a primary care provider at a study site and ≥1 medical condition potentially associated with driving cessation. We used baseline self-reported measures on mobility and health.
Results:
Compared to those enrolled pre-COVID-19 (n=61), more participants enrolled during COVID-19 (n=240) reported driving reductions (26% versus 70%, p<0.001) and more often for personal preference (vs. medical/emotional reasons). While mean social isolation was higher during than pre-COVID-19, self-reported depression, stress, and overall health PROMIS scores did not differ significantly.
Discussion:
Our findings highlight the resiliency of some older adults and have implications for mitigating the negative effects of driving cessation.
Keywords: Driving, COVID-19, Well-Being
INTRODUCTION
Social isolation has long been identified as a risk factor for poor mental and physical health outcomes in older adults (Courtin & Knapp, 2017). Driving reduction or cessation has also been linked to depression and other poor health outcomes (Chihuri et al., 2016), in part because of decreased mobility and engagement in community activities, but also due to the emotional ties between driving and independence (Betz et al., 2016). Early in the COVID-19 pandemic, the negative effects of stay-at-home orders and social distancing were identified as a potential problem for older adults, with calls for close monitoring and innovative interventions (Hwang et al., 2020; Roy et al., 2020; Sepúlveda-Loyola et al., 2020; Wu, 2020). Prior studies have found older adults did feel isolated or more stressed after the pandemic began (D’cruz & Banerjee, 2020; Piette et al., 2020; Wu, 2020), albeit at lower rates than other age groups (Losada-Baltar et al., 2021; Vahia et al., 2020).
COVID-19 pandemic restrictions led to a general reduction in drivers on the road, especially in the earlier stage when stay-at-home orders were in place. Recent studies showed that older driver’s experiences and attitudes around driving changed during the pandemic; one large cohort study found reduced number of days driven and shorter distance of trips taken during the early pandemic (January to April, 2020) compared to pre-pandemic (Roe et al., 2021). Analyses of traffic crashes and fatalities across all ages found decreases during COVID-19 as compared to before (Katrakazas et al., 2021), with a greater proportional reduction among older drivers (Wegman & Katrakazas, 2021). Studies of older adults in multiple counties showed a restriction of life-space mobility during the pandemic (Rantanen et al., 2020; Saraiva et al., 2021). Other work has examined the pandemic (and related isolation) on mental and physical health among older adults; one study found mental health levels were unchanged (van Tilburg et al., 2021), while a meta-analysis found mental and physical health were negatively impacted from COVID-19’s social distancing requirements (Sepúlveda-Loyola et al., 2020). To date, there has been less attention to how pandemic-related changes in older driver behavior may have influenced health outcomes.
The Advancing Understanding of Transportation Options (AUTO) study is an ongoing randomized trial testing a decision aid to support decisions about changes in driving habits of older adults. The study began prior to the pandemic and completed enrollment of older drivers in June 2021. In this analysis, we use baseline data from the enrolled drivers in the trial to identify self-reported changes in mobility and wellness. We hypothesized that the pandemic – whether through official stay-at-home orders or fear about getting sick – led to decreased driving, and that subsequent decreased mobility, along with pandemic-related stressors, led to poorer mental health.
METHODS
Study Population
Participants were enrolled in the AUTO study, a randomized trial of older drivers and simultaneously enrolled study partners (family member or friend) with longitudinal follow-up at 6, 12, 18 and 24 months. As described elsewhere in detail (Betz et al., 2021), eligible participants were adults aged ≥70 years who spoke English, drove at least once a week with a valid license, had a primary care provider affiliated with one of the study sites (San Diego, California; Denver, Colorado; Indianapolis, Indiana), and had at least one medical condition known to be associated with impaired driving safety or increased likelihood of driving cessation. Study staff identified potentially eligible individuals from primary care clinic rosters and then contacted them via letter and telephone. Telephone calls screened for additional eligibility criteria, including a 5-minute Montreal Cognitive Assessment (Wong et al., 2015) score of ≥21 to exclude participants with moderate to severe dementia. The trial preferentially enrolled individuals who identified a study partner for dyad participation until at least 67 dyads per site had been enrolled; after that, older adults could enroll by themselves. Study recruitment began in December 2019 and continued through June 2021; there was a pause in recruitment from March 12 to May 18, 2020 as the staff adjusted study protocols for remote enrollment and inclusion of COVID-19-related measures. Participants will have continued follow-up at pre-determined intervals for 24 months (Betz et al., 2021); the current analysis includes only baseline data from older drivers (referred to hereafter as “participants”), not study partners. All participants provided informed consent, and the study was approved by the institutional review boards of University of California San Diego, University of Colorado, and Indiana University. The trial is registered with clinicaltrials.gov (Clinical Trials.gov Identifier NCT04141891).
Study Measures
As part of the baseline questionnaire, all participants (regardless of intervention group) answered questionnaires about their demographics, driving patterns, use of alternative transportation, and physical and emotional health. Participants who reported reducing driving in the past 6 months were also asked the types of and reasons for reduction. For overall recent mobility and function, participants completed the Life-Space Assessment instrument (Baker et al., 2003). Total scores range from 0 (bedbound) to 120 (travel out of town every day without assistance) (Stalvey et al., 1999), and scores of ≤60 have been associated with lower social participation and higher mortality (Phillips et al., 2015).
Health-related PROMIS scales included Social Isolation, Depression, Emotional Support, and Global Health. All PROMIS scores are analyzed as standardized T-scores with higher scores indicating higher levels of isolation, depression, support, or overall health (HealthMeasures, 2020). For any given PROMIS domain, a score of 50 represents the average for a reference population. The 4-item Perceived Stress Scale (Cohen et al., 1983) measured general stress (scale: 0–16, with 16 indicating highest stress). Questions from the CoRonavIruS Health Impact Survey (CRISIS V0.1) Adult Self-Report Baseline Current Form (Bromet et al., 2020) were added in May 2020, along with COVID-19-related response options for questions about driving reduction.
Analysis
For this descriptive analysis, we included each participant’s responses from the baseline questionnaire (point of enrollment). We categorized time periods for analysis based on the COVID-19 pandemic: pre- (December 2019 through March 2020) and during (May 2020 to June 2021). We compared participant responses between time periods with two-sample t tests for continuous variables and Fisher’s exact tests for categorical variables, due to small sample sizes in some cells. We also used Fisher’s exact tests to calculate unadjusted odds ratios (OR) with 95% confidence intervals (95%CI). We graphed study measures (e.g. Life-Space score) pre- and during COVID-19 using locally weighted least squares regression (LOESS) to allow for different trends in the two time periods and for exploration of non-linear trends over time. For some variables with smaller sample sizes pre-COVID-19, only mean levels with standard errors were plotted, since LOESS curves achieve a more optimal visual fit for large, densely sampled data. To determine whether mean levels of study measures differed significantly pre- and during COVID-19, we used linear mixed models that included a random intercept for site. Statistical analyses were performed using R version 4.0.5 (Vienna, Austria). For free-text responses, quotes were reviewed independently by at least two study team members to categorize them into emergent themes, with subsequent discussion with the full study team and adjudication of any disagreements.
RESULTS
Over the study period, 301 older drivers were enrolled (~100 at each site). The sample was predominantly non-Hispanic white adults, with a near-even split between men and women; ages ranged from 70 to 92 years (Table 1). Nearly half of participants had completed post-graduate education and the majority were married or partnered and lived with someone in a private home (not assisted living). Based on residence ZIP code, 98% of participants lived in urban, 1.7% in suburban, and 0.3% in rural areas (USDA ERS - Rural-Urban Commuting Area Codes, 2020). Demographics of participants enrolled between pre- (n=61) or during (n=240) COVID-19 were generally similar. However, the racial distribution changed significantly, from 87% non-Hispanic white pre-COVID-19 to 98% during COVID-19.
Table 1.
Participant characteristics (N=301)
| n or mean | % or SD | |
|---|---|---|
| Age (years) | 77.1 | 5.1 |
| Female | 154 | 51.2 |
| Race | ||
| White | 283 | 95.3 |
| Black or African American | 6 | 2.0 |
| Asian | 3 | 1.0 |
| American Indian or Alaska Native | 0 | 0 |
| Native Hawaiian or Other Pacific Islander | 0 | 0 |
| Other/≥1 race | 5 | 1.7 |
| Hispanic ethnicity | 3 | 1.0 |
| Highest grade completed | ||
| ≤ High school graduate | 27 | 9.0 |
| Some college / vocational/ tech | 65 | 21.6 |
| College graduate | 69 | 22.9 |
| Any post-graduate work (masters, doctorate) | 140 | 46.5 |
| Employment status | ||
| Employed full time | 17 | 5.6 |
| Employed part time | 28 | 9.3 |
| No paid employment | 7 | 2.3 |
| Retired | 249 | 82.7 |
| Current marital status | ||
| Married / Partnered | 188 | 62.7 |
| Widowed / Divorced / Never married | 112 | 37.3 |
| Currently livesa | ||
| Alone | 99 | 33.1 |
| With a spouse or partner | 181 | 60.5 |
| With a friend / children / other family members | 26 | 8.7 |
| Lives in | ||
| Private home or apartment | 277 | 92.0 |
| Assisted living facility / retirement community / senior community | 24 | 8.0 |
Participants may select >1 option, so percentages do not sum to 100%. SD: standard deviation.
Driving and mobility
Before COVID-19, 26% (n=16/61) of participants reported having reduced their driving in the past six months; this rose to 70% (n=167/239) during COVID-19; p<0.001). Among those who had reduced their driving, the most commonly reported types of reductions were number of trips taken or miles driven per week, followed by days per week and trip distance (Figure 1a). Before COVID-19, drivers who had reduced driving most commonly said they had done so for medical or emotional reasons (Figure 1b). However, during COVID-19, over time, increasing proportions of those reporting reductions said they had done so because of their own desire to go out less, while declining proportions reported reductions due to official COVID-19 orders (Figure 1b; Supplementary Figure 1). When asked about driving destinations in the past 3 months, fewer older adults had driven to distant towns during COVID-19 than pre-COVID-19 (45% versus 60.7%; p=0.032; OR 0.53, 95%CI 0.29–0.98) or outside of their state (10.4% versus 26.2%; p = 0.003; OR 0.33, 95% CI 0.15–0.71). During COVID-19, 31.4% of drivers said the pandemic had changed the way they think about driving.
Figure 1. Types of (A) and reasons (B) for driving reduction in the past 6 months, among those reporting reductions (n=16 pre-COVID; n=167 during COVID-19).
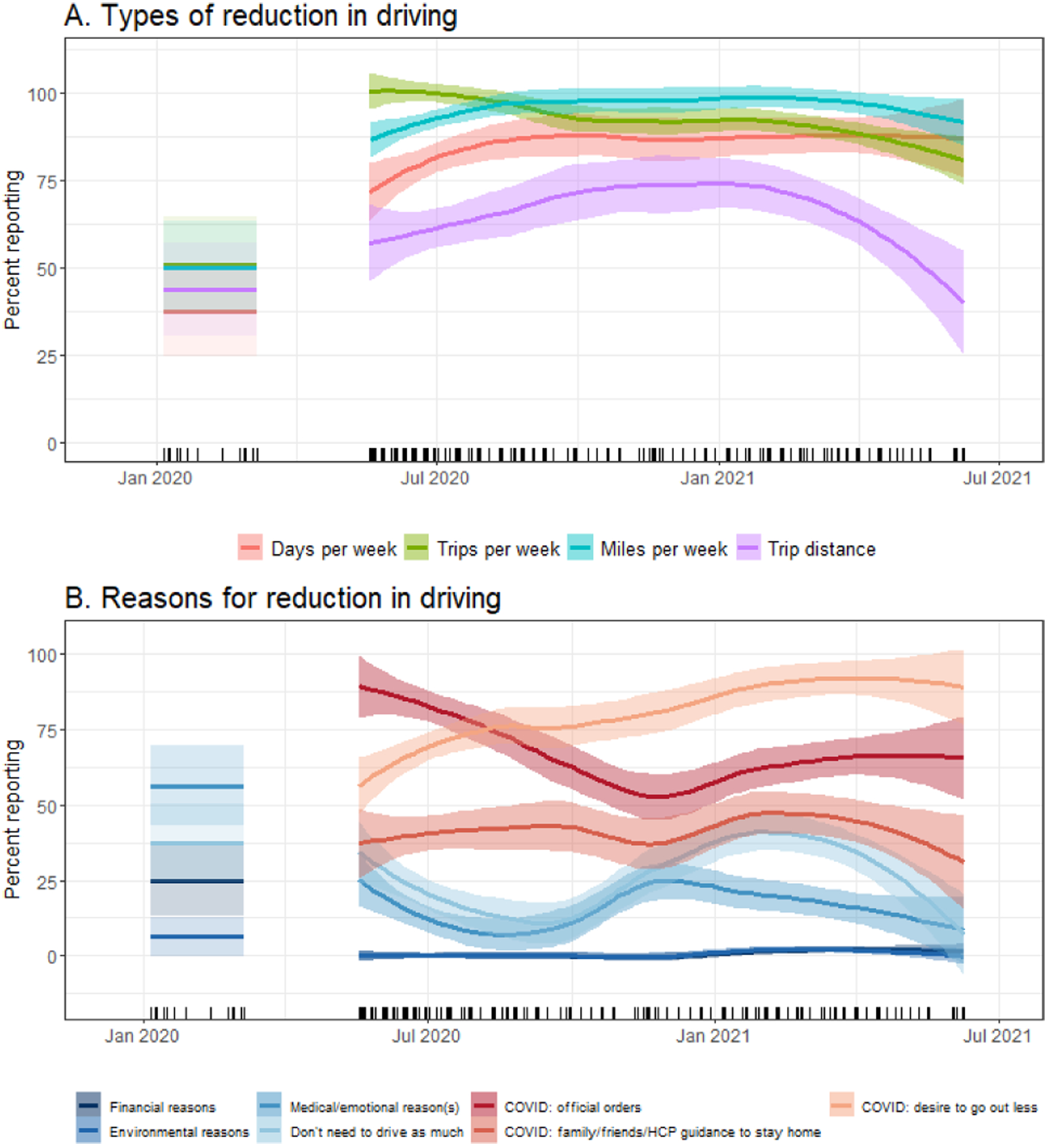
Lines represent percent reporting ± standard error. Multiple responses allowed. COVID-19-related reasons were added after the COVID-19 pandemic began.
The most common form of alternative (non-driving) transportation was rides with friends or family; 86% of participants pre-COVID-19 and 82% of those enrolled during COVID-19 reported having gotten a ride within the past three months. However, reported use of public and other transportation within the past three months changed significantly during COVID-19, with marked declines early in the pandemic (Figure 2). Pre-COVID-19, 32.8% of drivers said during past 3 months they’d used rideshare services like Lyft or Uber, where only 7.9% of drivers said they’d used them in the past 3 months over the entire COVID-19 period (p < 0.001). Notably, use of rideshare services reached a low in January 2021 but has made the sharpest recovery, to about half of its pre-COVID-19 level, with local train/subway use also increasing. Mean Life-Space scores declined after the start of COVID-19 (pre: 85.1, SD 20.8; during: 73.7, SD 18.7; p<0.001), rising again in 2021 (Figure 3a).
Figure 2. Use of alternative transportation in the past 3 months (n=16 pre-COVID; n=167 during COVID-19).
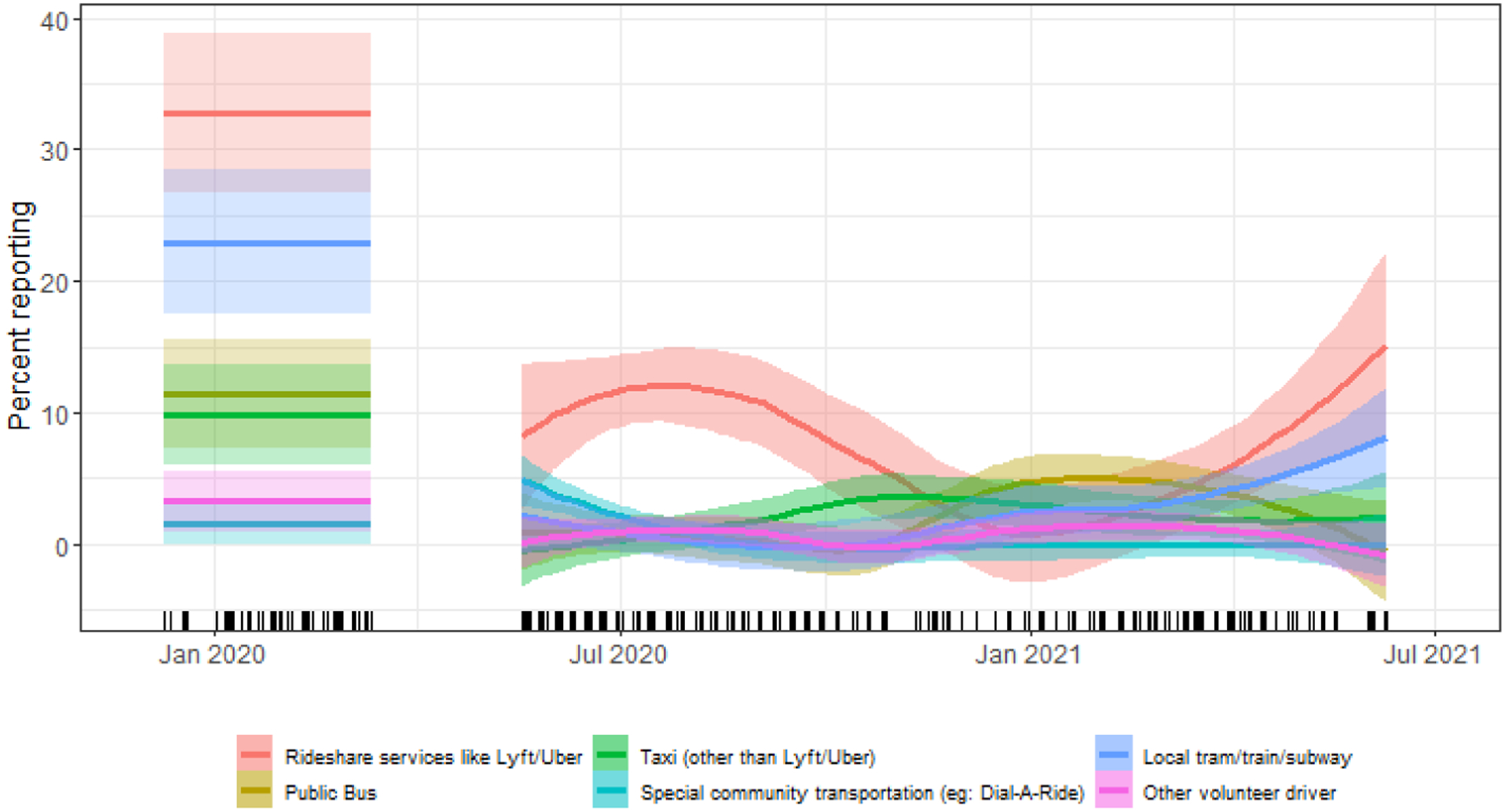
Lines represent percent reporting ± standard error
Figure 3. Participant scores over time (n=16 pre-COVID; n=167 during COVID-19).
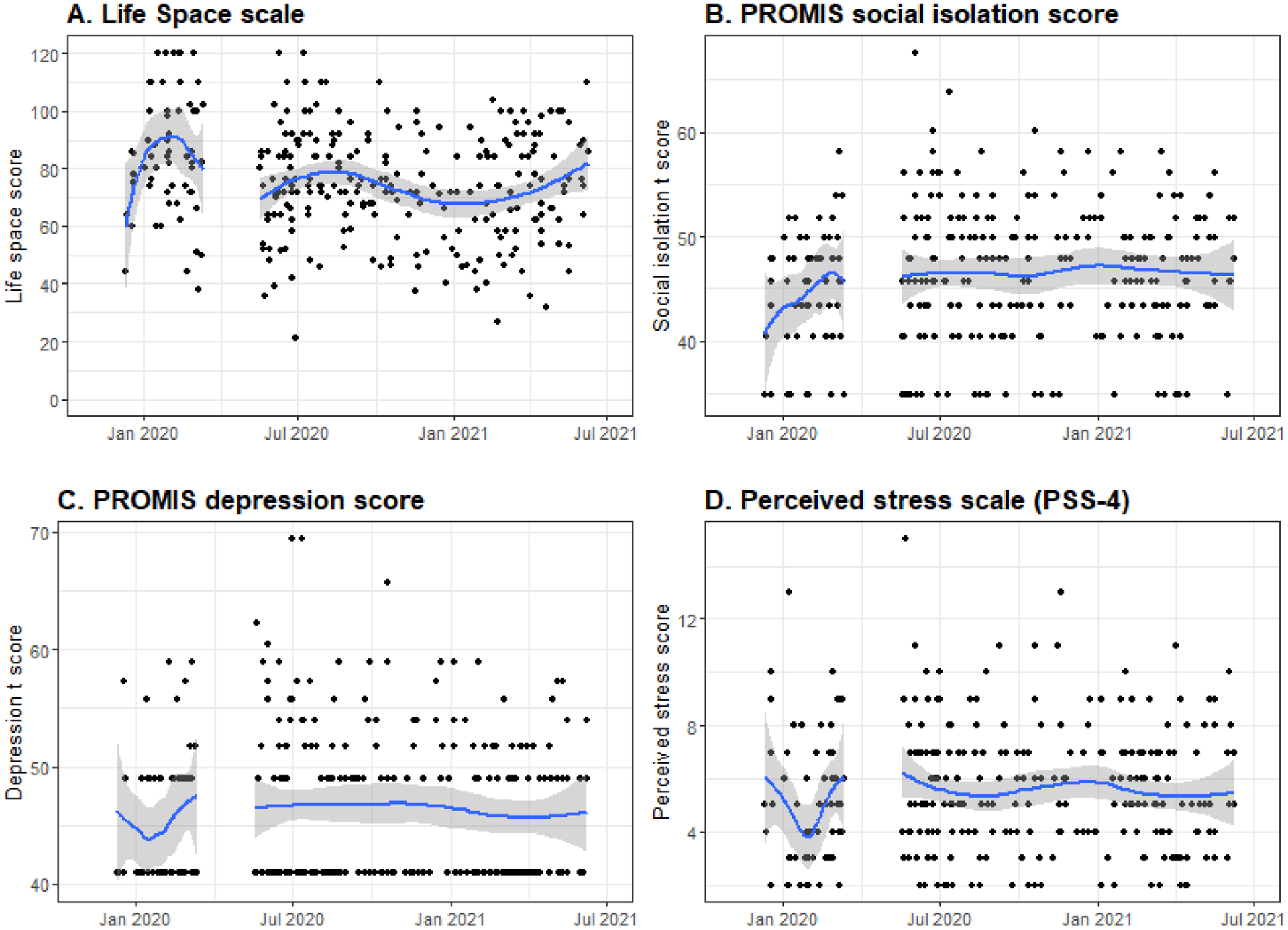
Lines represent scale score, with 95% confidence intervals. All PROMIS scores are analyzed as standardized T-scores.
Health and well-being
Mean self-reported emotional support remained slightly higher than reference population averages throughout the study (pre-COVID-19 PROMIS t-score: 55.3, SD 6.5; during-COVID-19: 55.3, SD 6.9; p=0.950). Mean social isolation was higher during COVID-19 (t-score: 46.6, SD 6.4) as compared to pre-COVID-19 (44.8; SD 5.8; p<0.05; Figure 3b). However, mean self-reported depression changed little between pre- and during COVID-19, remaining slightly lower than reference population averages over time (Figure 3c; pre-COVID-19: 45.5, SD 5.8; during-COVID-19: 46.4, SD 6.5; p=0.315).
Reported global health also did not change significantly over time; mean t-scores remained average for PROMIS subscales of both physical (pre-COVID-19: 50.7, SD 7.5; during-COVID-19: 49.4, SD 7.6; p=0.263) and mental (pre-COVID-19: 53.8, SD 6.8; during-COVID-19: 53.0, SD 6.5) health. Mean perceived stress scores remained moderate and stable over time (Figure 3d; pre-COVID-19: 5.0 [scale: 0–16], SD 2.5; during COVID-19: 5.5, SD 2.4; p=0.396), although 36.3% of those enrolled during COVID-19 said that restrictions on leaving home had been at least moderately stressful.
Effects of COVID-19
Among those enrolled during COVID-19 (n=240), 46.7% said the pandemic had changed their views on driving. Many reported being more thoughtful about whether each trip was necessary and realizing how much they could do without driving, like getting groceries delivered (Table 2). While a few reported driving less because of their fear of COVID-19-exposure if they were in a crash, one participant said he and his wife were taking longer drives as a way to escape boredom at home.
Table 2.
Illustrative open-ended responses from participants about COVID-19-related experiences, by question posed and general theme of response
| HOW THE PANDEMIC CHANGED VIEWS ON DRIVING | ||
|---|---|---|
| More concerned about driving | “If i get into an accident this would increase my exposure [to COVID-19]. So I drive less now to avoid exposure.” | |
| “I don’t make unnecessary trips; I plan out my driving and make sure I don’t go to places where I don’t need to be (in order to be safe)” | ||
| Before COVID-19, both she and her husband would use UBER, but now they are very hesitant to do that. | ||
| Doesn’t make unnecessary trips where she could expose self. Worries about car breaking down leading to exposure. Feels especially vulnerable due to underlying conditions. | ||
| “Have lost confidence in my driving since driving less now” | ||
| Less concerned about not driving, or driving more | “Made me realize that I can get along driving less” | |
| Realizes she can do without driving so much. Less traffic. Found that she drove more than she needed to [pre-COVID-19]. Other ways to get what she needs | ||
| “My son has come weekly to [help with] my grocery shopping. “This made me less fearful about losing my ability to drive later on. I have less need to go places. I am really comfortable just being on my property” | ||
| “We (my wife and I) take more trips to get away from the house” | ||
| HOW THE PANDEMIC HAS PERSONALLY AFFECTED PARTICIPANTS | ||
| Increased isolation or fear | Feels total restriction on life, mentally felt as a total restriction. Doing such few things already and having even those things taken away makes her sad. | |
| “I miss not having people over for dinner and hugging my grandkids” | ||
| “It closes in on you. You don’t feel safe unless you are in your bubble. It puts stress on going anywhere. I think a lot more every time I go anywhere.” | ||
| Found that after not seeing people for a while that she forgot some names of some people. Made a conscious effort to rebuild relationships and be more social now that things are opening. | ||
| “I’m hesitant to interact with neighbors since I don’t know if they are practicing safe measures with the virus.” | ||
| “I have a daughter in law who’s pregnant who is concerned. I [am] concerned for my family getting [COVID-19].” | ||
| Effects on daily life | “Library being closed has been a major disruption. I broke my arm when the stay at home order began but was afraid to go to the hospital because of fear of the virus and not wanting to [overload] the system” (said she finally went 3 weeks later) | |
| “Needs are being met and feel fortunate but feel very restricted in every other way” | ||
| Difficult visiting husband in hospital while he was dying and coronavirus restrictions, now delayed in having funeral for him; Overall health better (weight loss, healthy eating); Miss social interactions - phone and zoom aren’t sufficient for doctor visits or fitness classes | ||
| Decline in physical strength because not able to work out and go to the gym to lift weights. Feel relieved to be vaccinated and able to do some things again. | ||
| “Life is easier since I don’t go out as much.” (She has to carry around an oxygen tank wherever she goes) | ||
| HOW THE PANDEMIC LED TO POSITIVE CHANGES IN LIFE | ||
| New modes of communication | “Talk on the phone more. Learned how to Zoom call. I am in communication with people more now by increasing alternative methods of talking.” | |
| “I am in contact with more out of town friends now. I communicate with people more now.” | ||
| “Virtual doctor visits are great! I’m impressed with how well we were able to adjust and adapt to new normal” | ||
| Improved health and lifestyle | “more time alone with husband, fewer demands from other people, more time to meditate, calmer life” | |
| Improved cleanliness; hands, surfaces- more sanitary; wearing masks has prevented other colds | ||
| “It has brought our family closer together. We check on each other more often. I have a lot of grandchildren and I worry about them.” | ||
| Better eating habits - more home cooked meals - lost 15 pounds; more contact w others by phone - who wouldn’t have otherwise spoke with | ||
| “The kids have been forced to spend more time with parents. There has been a lot of working together. My children show concern for me. I have seen a lot of respect towards me. “ | ||
| “I am more considerate; I am more aware and understanding of others; I no longer believe everything I read” | ||
| “We order our groceries for pickup which makes it easier. We’ll continue to do this after the pandemic.” | ||
When asked about COVID-19-related events within the past two weeks, few participants reported suspected or confirmed infections in themselves (3.3%) or family members (10.5%), while 21.3% reported family members being in quarantine (with or without COVID-19 symptoms) and 14.2% said family members had lost jobs or had reduced ability to earn money. Nearly one fifth (18.8%) said that, within the past two weeks, COVID-19-related changes had created financial problems for them or their family, and 10.4% were at least slightly worried about the stability of their living situation. The majority of participants had only a little (37.6%) or no difficulty (50.6%) following COVID-19-related social distancing.
Among those enrolled during COVID-19, a minority of participants said the COVID-19 pandemic had at least moderately influenced their physical (25.4%) or emotional (21.3%) health within the past two weeks. More participants, when asked about their concerns in the past two weeks, were at least moderately worried about friends or family being infected with COVID-19 (49.4%) than being infected themselves (30.1%; p<0.001); this difference in concern for others versus self was smaller for participants enrolled during the first two weeks of the COVID-19 period (53.8% versus 46.2%) than those enrolled in the last two weeks of the COVID-19 period (42.9% versus 14.3%). The majority (94.9%) had not delayed or avoided seeking care for possible medical emergencies within the past two weeks, but 53.0% had cancelled important routine things like healthcare appointments. Participants noted COVID-19-related disruptions in exercise activities (42.3%), medical care for chronic illness (12.6%), physical therapy (9.6%), and psychotherapy (2.5%), along with volunteer programs (29.3%) and recreational activities (41.8%).
When asked about relationships with others in the past two weeks, most said the quality of relationships with family members (71.3%) or friends (68.4%) had not changed, with fewer saying relationships had worsened (9.6% family; 20.0% friends). Half (51.3%) of those enrolled during COVID-19 said they had had less contact with people outside their home as compared to pre-COVID-19.
When asked how else the COVID-19 pandemic had personally affected them, 78.3% (n=188) of participants provided free-text responses. Many expressed a general sense of restriction, along with sadness at not being able to see family in-person, concern about their families’ health, and frustration at disruptions in activities like going to the gym or library (Table 2). Yet many participants (39.1%) thought the COVID-19 crisis in their area had led to at least some positive changes in their life, predominantly more frequent communication with friends and family, including through video services. Some participants said they had enjoyed a slower pace of life or new hobbies, several reported realizing that they can do without driving as much, and one noted feeling less fearful about losing her ability to drive in the future, after finding that she could meet her needs without driving.
DISCUSSION
In this large, multi-state study of older drivers, there were changes between those enrolled before versus during the COVID-19 pandemic in driving, including in amounts driven and perceptions about or desire to drive. Drivers enrolled during the pandemic also reported higher levels of social isolation. Driving cessation has previously been associated with increases in depression and poor health outcomes (Chihuri et al., 2016; Curl et al., 2013; Edwards et al., 2009; Freeman et al., 2006; Ragland et al., 2005), and participants in this study reported fears about infection in family or themselves. Yet – in this largely White and well-educated, community-dwelling sample of older adults – there were not significant increases in depression or stress. The majority of participants reported little stress from or difficulty following COVID-19-related restrictions, which may help explain our study findings.
The effects of COVID-19 on both mobility and health outcomes likely differ in other populations. For example, a mixed-methods study conducted between April and June of 2020 (during the shelter-in-place COVID-19 order) found 40% of community-dwelling older adults in San Francisco were socially isolated; notably, its participants were older and frailer than the generally healthy, community-dwelling older adults in ours (Kotwal et al., 2021). Other work has found that younger adults, women, and those with lower income were most affected by the COVID-19 pandemic (Ettman et al., 2020; Pieh et al., 2020). One explanation may be that retired older adults (82% in our sample) suffered less from the economic impacts of COVID-19-related closures and job loss, although nearly one fifth of participants noted COVID-19-related financial issues for them or their families.
Our study findings have implications for general approaches to supporting older adults through the process of driving retirement. COVID-19 and restrictions to travel or human contact have led to growth of alternative options for routine needs, including telemedicine (Gorenko et al., 2021; Kotwal et al., 2021). Multiple participants spoke of becoming familiar with – and excited about - things like video conferences for connecting with family and friends, or delivery services for groceries. Services and programs like these have the potential to help older adults stay connected and meet their daily needs after driving cessation (Batsis et al., 2021; Van Orden et al., 2021).
Although our study found no significant increase in depression or stress in those during versus before COVID-19, participants did report experiencing stress and fear related to COVID-19. Reported social isolation was higher in those enrolled during COVID-19, but participant comments displayed a range of coping techniques. Other studies have also suggested high resiliency in older adults in their response to COVID-19 stressors (Klaiber et al., 2020; Vahia et al., 2020). Some of these strategies, like delivery services, may only be available to individuals with financial resources. Other strategies, like reminders to connect with family or friends; future work to understand, and encourage, emotional resiliency is important for older and younger adult populations.
A key limitation to consider in interpreting these data is that the sample was predominantly white and well-educated, especially those who enrolled during the pandemic. COVID-19 mortality in the United States has been higher in communities of color due to numerous factors, including systemic discrimination, unequal healthcare access, higher occupational exposure, socioeconomic disparities, and other social determinants of health (CDC, 2020; Webb Hooper et al., 2020). Thus, experiences may be very different in these communities and in populations with lower socioeconomic status, such as those who faced financial pressures from lost jobs, or who worked in essential jobs or industries requiring them to continue working in person through the pandemic. This analysis presents only a single time point of data per individual; hence, it describes average differences between those enrolled before versus during the early and peak COVID-19 pandemic in the United States. Those who chose to enroll during COVID-19 differed from those enrolled before COVID-19 by race and ethnicity, but there may have been other unmeasured differences as well. In addition, no participants were enrolled during the first two months (March to May, 2020) of the pandemic, when stress may have been higher. Other temporal factors besides COVID-19 – such as political tensions and social unrest – may have also affected older adult stress and well-being but were not assessed in this study. In the future, longitudinal analyses of within-individual changes may add nuance to our understanding of these issues. Another limitation is that drivers were recruited from urban and suburban areas in three states, so results may not generalize to other areas. In particular, older drivers in rural areas – without access to alternative transportation or certain services– have traditionally had different experiences and attitudes around driving (Huseth-Zosel et al., 2016; Johnson, 2002), and their views are not reflected in this analysis. The study relied on self-reported outcomes, raising concerns about social-desirability or recall biases. Finally, the study enrolled older adults who could identify a family or friend to enroll as a study partner, so this sample may have had less social isolation and more emotional support at baseline than the general population of older adults.
Despite these limitations, this large study of community-dwelling older drivers provides useful new information, including that those enrolled during the COVID-19 pandemic reported more reductions in driving, and for different reasons, than those enrolled before the pandemic. However, in this sample of predominantly educated, white participants, there was little or no difference in isolation and mental and physical health before vs. during the pandemic. The study has implications for supporting older adults through driving cessation to mitigate negative health outcomes and promote resiliency.
Supplementary Material
Sponsor’s Role:
This study was funded by the National Institutes of Health (R01 AG059613; CTSA UL1 TR002535). The sponsor had no role in study design, methods, subject recruitment, data collection or analysis, or preparation of the manuscript.
Footnotes
Conflict of Interest: The authors report no conflicts of interest
Human Subjects: The study was approved by the institutional review boards of University of California San Diego, University of Colorado (19-0059), and Indiana University. The AUTO trial is registered with clinicaltrials.gov (Clinical Trials.gov Identifier NCT04141891). Prior to COVID, participants provided written, in-person consent; during COVID, participants provided verbal consent by telephone (with IRB approval of this protocol).
REFERENCES
- Baker PS, Bodner EV, & Allman RM (2003). Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc, 51(11), 1610–1614. [DOI] [PubMed] [Google Scholar]
- Batsis JA, Daniel K, Eckstrom E, Goldlist K, Kusz H, Lane D, Loewenthal J, Coll PP, & Friedman SM (2021). Promoting Healthy Aging During COVID-19. Journal of the American Geriatrics Society, 69(3), 572–580. 10.1111/jgs.17035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, Omeragic F, Meador L, DiGuiseppi CG, Fowler NR, Han SD, Hill L, Johnson RL, Knoepke CE, Matlock DD, Moran R, & AUTO Research Team. (2021). The Advancing Understanding of Transportation Options (AUTO) study: Design and methods of a multi-center study of decision aid for older drivers. Injury Epidemiology, 8(1), 23. 10.1186/s40621-021-00310-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, Scott K, Jones J, & DiGuiseppi C (2016). “Are you still driving?” Meta-synthesis of older adults’ preferences for communication with healthcare providers about driving. Traffic Inj Prev, 17(4), 367–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromet E, Colcombe S, Geogiadis K, Klein D, & Salum G (2020). The CoRonavIruS Health Impact Survey (CRISIS): Adult Self-Report Baseline Current Form. https://www.nlm.nih.gov/dr2/CRISIS_Adult_Self-Report_Baseline_Current_Form_V0.3.pdf [Google Scholar]
- CDC. (2020, February 11). COVID-19: Health Equity Considerations and Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html [Google Scholar]
- Chihuri S, Mielenz TJ, DiMaggio CJ, Betz ME, DiGuiseppi C, Jones VC, & Li G (2016). Driving cessation and health outcomes in older adults. J Am Geriatr Soc, 64(2), 332–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. J Health Soc Behav, 24(4), 385–396. [PubMed] [Google Scholar]
- Courtin E, & Knapp M (2017). Social isolation, loneliness and health in old age: A scoping review. Health & Social Care in the Community, 25(3), 799–812. 10.1111/hsc.12311 [DOI] [PubMed] [Google Scholar]
- Curl AL, Stowe JD, Cooney TM, & Proulx CM (2013). Giving Up the Keys: How Driving Cessation Affects Engagement in Later Life. The Gerontologist. 10.1093/geront/gnt037 [DOI] [PubMed] [Google Scholar]
- D’cruz M, & Banerjee D (2020). ‘An invisible human rights crisis’: The marginalization of older adults during the COVID-19 pandemic – An advocacy review. Psychiatry Research, 292, 113369. 10.1016/j.psychres.2020.113369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards JD, Perkins M, Ross LA, & Reynolds SL (2009). Driving status and three-year mortality among community-dwelling older adults. J Gerontol A Biol Sci Med Sci, 64(2), 300–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, & Galea S (2020). Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Network Open, 3(9), e2019686. 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman EE, Gange SJ, Munoz B, & West SK (2006). Driving status and risk of entry into long-term care in older adults. Am J Public Health, 96(7), 1254–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorenko JA, Moran C, Flynn M, Dobson K, & Konnert C (2021). Social Isolation and Psychological Distress Among Older Adults Related to COVID-19: A Narrative Review of Remotely-Delivered Interventions and Recommendations. Journal of Applied Gerontology, 40(1), 3–13. 10.1177/0733464820958550 [DOI] [PubMed] [Google Scholar]
- HealthMeasures. (2020). PROMIS Adult Measures. http://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis/list-of-adult-measures
- Huseth-Zosel AL, Sanders G, O’Connor M, Fuller-Iglesias H, & Langley L (2016). Health Care Provider Mobility Counseling Provision to Older Adults: A Rural/Urban Comparison. J Community Health, 41(1), 1–10. 10.1007/s10900-015-0055-8 [DOI] [PubMed] [Google Scholar]
- Hwang T-J, Rabheru K, Peisah C, Reichman W, & Ikeda M (2020). Loneliness and social isolation during the COVID-19 pandemic. International Psychogeriatrics, 32(10), 1217–1220. 10.1017/S1041610220000988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE (2002). Why rural elders drive against advice. J Community Health Nurs, 19(4), 237–244. 10.1207/S15327655JCHN1904_04 [DOI] [PubMed] [Google Scholar]
- Katrakazas C, Michelaraki E, Sekadakis M, Ziakopoulos A, Kontaxi A, & Yannis G (2021). Identifying the impact of the COVID-19 pandemic on driving behavior using naturalistic driving data and time series forecasting. Journal of Safety Research, 78, 189–202. 10.1016/j.jsr.2021.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klaiber P, Wen JH, DeLongis A, & Sin NL (2020). The ups and downs of daily life during COVID-19: Age differences in affect, stress, and positive events. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, gbaa096. 10.1093/geronb/gbaa096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotwal AA, Holt-Lunstad J, Newmark RL, Cenzer I, Smith AK, Covinsky KE, Escueta DP, Lee JM, & Perissinotto CM (2021). Social Isolation and Loneliness Among San Francisco Bay Area Older Adults During the COVID-19 Shelter-in-Place Orders. Journal of the American Geriatrics Society, 69(1), 20–29. 10.1111/jgs.16865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada-Baltar A, Martínez-Huertas JÁ, Jiménez-Gonzalo L, Pedroso-Chaparro MDS, Gallego-Alberto L, Fernandes-Pires J, & Márquez-González M (2021). Longitudinal correlates of loneliness and psychological distress during the lockdown situation due to COVID-19. Effects of age and self-perceptions of aging. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, gbab012. 10.1093/geronb/gbab012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips J, Dal Grande E, Ritchie C, Abernethy AP, & Currow DC (2015). A population-based cross-sectional study that defined normative population data for the Life-Space Mobility Assessment-composite score. J Pain Symptom Manage, 49(5), 885–893. 10.1016/j.jpainsymman.2014.09.010 [DOI] [PubMed] [Google Scholar]
- Pieh C, Budimir S, & Probst T (2020). The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. Journal of Psychosomatic Research, 136, 110186. 10.1016/j.jpsychores.2020.110186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette J, Solway E, Singer D, Kirch M, Kullgren J, & Malani P (2020). Loneliness Among Older Adults Before and During the COVID-19 Pandemic. University of Michigan National Poll on Healthy Aging. https://www.healthyagingpoll.org/reports-more/report/loneliness-among-older-adults-and-during-covid-19-pandemic [Google Scholar]
- Ragland DR, Satariano WA, & MacLeod KE (2005). Driving cessation and increased depressive symptoms. J Gerontol A Biol Sci Med Sci, 60(3), 399–403. [DOI] [PubMed] [Google Scholar]
- Rantanen T, Eronen J, Kauppinen M, Kokko K, Sanaslahti S, Kajan N, & Portegijs E (2020). Life-Space Mobility and Active Aging as Factors Underlying Quality of Life among Older People before and during COVID-19 Lock-down in Finland—A Longitudinal Study. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 10.1093/gerona/glaa274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roe CM, Rosnick CB, Colletta A, & Babulal GM (2021). Reaction to a Pandemic: Social Distancing and Driving Among Older Adults During COVID-19. Journal of Applied Gerontology, 40(3), 263–267. 10.1177/0733464820966516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy J, Jain R, Golamari R, Vunnam R, & Sahu N (2020). COVID-19 in the geriatric population. International Journal of Geriatric Psychiatry, 35(12), 1437–1441. 10.1002/gps.5389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saraiva MD, Apolinario D, Avelino-Silva TJ, de Assis Moura Tavares C, Gattás-Vernaglia IF, Marques Fernandes C Rabelo LM, Tavares Fernandes Yamaguti S, Karnakis T, Kalil-Filho R, Jacob-Filho W, & Romero Aliberti MJ (2021). The Impact of Frailty on the Relationship between Life-Space Mobility and Quality of Life in Older Adults during the COVID-19 Pandemic. The Journal of Nutrition, Health & Aging, 25(4), 440–447. 10.1007/s12603-020-1532-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P, Ganz F, Torralba R, Oliveira DV, & Rodríguez-Mañas L (2020). Impact of Social Isolation Due to COVID-19 on Health in Older People: Mental and Physical Effects and Recommendations. The Journal of Nutrition, Health & Aging, 24(9), 938–947. 10.1007/s12603-020-1469-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stalvey BT, Owsley C, Sloane ME, & Ball K (1999). The Life Space Questionnaire: A measure of the extent of mobility of older adults. Journal of Applied Gerontology, 18(4), 460–478. [Google Scholar]
- USDA ERS - Rural-Urban Commuting Area Codes. (2020). https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/
- Vahia IV, Jeste DV, & Reynolds CF III. (2020). Older Adults and the Mental Health Effects of COVID-19. JAMA, 324(22), 2253–2254. 10.1001/jama.2020.21753 [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Bower E, Lutz J, Silva C, Gallegos AM, Podgorski CA, Santos EJ, & Conwell Y (2021). Strategies to Promote Social Connections Among Older Adults During “Social Distancing” Restrictions. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 29(8), 816–827. 10.1016/j.jagp.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Tilburg TG, Steinmetz S, Stolte E, van der Roest H, & de Vries DH (2021). Loneliness and Mental Health During the COVID-19 Pandemic: A Study Among Dutch Older Adults. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 76(7), e249–e255. 10.1093/geronb/gbaa111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb Hooper M, Nápoles AM, & Pérez-Stable EJ (2020). COVID-19 and Racial/Ethnic Disparities. JAMA, 323(24), 2466–2467. 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wegman F, & Katrakazas C (2021). Did the COVID-19 pandemic influence traffic fatalities in 2020? A presentation of first findings. IATSS Research, 45(4), 469–484. 10.1016/j.iatssr.2021.11.005 [DOI] [Google Scholar]
- Wong A, Nyenhuis D, Black SE, Law LS, Lo ES, Kwan PW, Au L, Chan AY, Wong LK, Nasreddine Z, & Mok V (2015). Montreal Cognitive Assessment 5-minute protocol is a brief, valid, reliable, and feasible cognitive screen for telephone administration. Stroke, 46(4), 1059–1064. 10.1161/STROKEAHA.114.007253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu B (2020). Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Global Health Research and Policy, 5, 27. 10.1186/s41256-020-00154-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


