Abstract
Objectives: Brazil is one of the largest countries in the world, in terms of geography and population. Most Brazilians reside in the south and south-eastern regions, with notable numbers in the regions’ megacities, such as São Paulo city. Healthcare provision in such a complex environment is difficult. Thus, a clear understanding of the distribution – or rather, the maldistribution – of these services is fundamental for optimising the allocation of human and financial resources to areas of greatest privation. The present study aimed to determine the distribution of primary dental clinics in São Paulo city. Methods: A total of 4,101 primary dental clinics in São Paulo city were identified and geocoded. Clinic locations were integrated with the city’s 19,128 constituent census tracts – each containing sociodemographic data for the 11,252,204 residents – using Geographic Information Systems (GIS). Results: Approximately two-thirds (64.8%) of the population resided within 0.5 km of a primary dental clinic, and a further 23.9% were within 1 km. Populations more than 1 km out were typically characterised as sociodemographically disadvantaged. Primary dental clinics were also more sparsely distributed in the city’s peripheral census tracts than central census tracts. Conclusion: Primary dental clinics are maldistributed in São Paulo city, with disadvantaged populations having less spatial access than their advantaged counterparts.
Key words: Dentistry, oral health, public dental health, spatial access
Introduction
The United Nations Sustainable Development Goals of 2015, as it relates to health, emphasises the need to address health inequalities in all countries. Health inequalities are defined as differences in health determinants and outcomes between individuals or groups1. Socioeconomically disadvantaged groups and certain demographic groups (including children and ethnic minorities) often suffer a greater burden of diseases – a phenomenon well established in both developing and developed nations2., 3., 4., 5..
Health inequalities can be attributed to barriers that inhibit the access to healthcare1., 6., 7.. Much is known about the role of financial and cultural barriers. For example, disadvantaged populations – with limited knowledge and limited funds – often present lower utilisation rates8., 9., 10..
In contrast, very little is known about how other barriers affect access, such as geographic distance8., 9.. Recent advances to geospatial tools, such as Geographic Information Systems (GIS), have allowed for such knowledge deficits to be addressed11., 12., 13.. At present, most applications of GIS have been conducted in the context of urban–rural comparisons for hospital and specialty services14.
Much less is known about the role of distance on primary care utilisation, especially within urban conglomerations where the majority of the world’s population resides8. Moreover, primary care is the most important form of healthcare for addressing health inequalities, because it is relatively inexpensive, easily delivered and most effective in large-scale disease prevention8. In Brazil, free primary dental care coexists with traditional private services15.
Building on past studies that have investigated the role of geographic distance on the spatial accessibility of dental care, the present research aimed in determine the distribution of fixed primary dental clinics in São Paulo city, Brazil. We tested the hypothesis that clinics are maldistributed across the city.
Materials and methods
Ethics
The study used de-identified data from online open-source databases. As such, no ethics approval was required.
Population census
São Paulo city – as defined by the Instituto Brasileiro de Geografia e Estatística (IBGE) – was divided into 120 districts, and sub-divided into 19,128 census tracts (including non-residential tracts), the smallest units for census data collection. Administrative boundaries for all tracts were provided by the IBGE (http://downloads.ibge.gov.br/downloads_geociencias.htm). Population data for each tract were retrieved from the 2010 Population Census, which surveyed 67.6 million households in 5,565 municipalities. All datasets were available on the IBGE repository (http://downloads.ibge.gov.br/downloads_estatisticas.htm).
The sociodemographic variables of interest included income, education, age and race. The income variable was presented by the average monthly nominal household income for each tract. Education was based on literacy rates calculated for those older than 14 years – the minimum age for admission to employment. The age variable divided the population into three groups: children (0–14 years), adults (15–64 years) and elderly (65+ years). The race variable included those who self-identified as being ‘black’, ‘brown’, ‘yellow’ or ‘indigenous’ (herein collectively referred to as ‘ethnic minorities’).
Primary dental clinics
Addresses for all primary dental clinics in São Paulo city were obtained from Brasil Páginas Amarelas (Yellow Pages) (http://www.brasilpaginasamarelas.com.br). Duplicates and specialists were identified if their names and/or addresses indicated as such, and subsequently excluded. The confirmatory sample of 4,101 primary dental clinics were then converted into geographic coordinates using the Google Maps API (https://www.google.com/maps/) via a locally developed access tool. Coordinates with accuracy values less than street-level accuracy were manually geocoded using Google Maps.
Geographic mapping
All subsequent geographic mapping was conducted on Quantum Geographic Information Systems (QGIS) (version 2.16.0 - Nødebo, QGIS Development Team, GNU General Public License), using the World Geodetic System 1984 (WGS 84) standard of coordinate referencing. Census data were joined to their corresponding census tracts. Coordinates for the dental clinics were then imported, and analysed.
Statistical analyses
Descriptive statistical analyses – including practice-to-population ratios – were conducted using Microsoft Excel (version 2016, Microsoft, Redmond, WA, USA). These methods were consistent with past papers resting upon descriptive statistics alone16., 17..
Results
In 2010, São Paulo city consisted of 11,252,204 residents, distributed across 120 districts and 19,128 census tracts. Residential tracts presented varying geographic areas and population sizes that ranged from 1 to 3,252, and averaged 613 people per tract. A total of 4,101 fixed primary dental clinics were identified within São Paulo city.
Two-thirds of São Paulo residents were located within 0.5 km of at least one primary dental clinic; one-quarter were located between 0.5 km and 1 km; and only 11.4% were more than 1 km out (Figure 1, Table 1). Those within 0.5 km presented higher average monthly household incomes and lower illiteracy rates, with lower proportions of children and ethnic minorities, and higher proportions of elderly, than those further out (Table 1).
Figure 1.
Distribution of fixed primary dental clinics in São Paulo city, Brazil. Clinics (grey dots) are presented against the city centre, Praça da Sé (black cross). High resolution inset shows districts (thick grey lines) and census tracts (thin grey lines) overlayed with clinics that have 0.5 km and 1 km buffers (green).
Table 1.
Sociodemographic profile of populations living at various distances from primary dental clinics in São Paulo city, Brazil
| Distance to practice (km) | Population (n (%)) | Average monthly nominal household income (US$) | Illiteracy (%) | Children (0–14 years) (%) | Elderly (65+ years) (%) | Ethnic minorities (%) |
|---|---|---|---|---|---|---|
| 0–0.5 | 7,287,677 (64.8) | 1,552 | 2.4 | 17.6 | 10.4 | 31.6 |
| 0.5–1 | 2,684,634 (23.9) | 882 | 4.4 | 23.6 | 5.7 | 47.1 |
| 1+ | 1,279,893 (11.4) | 615 | 5.6 | 26.4 | 4.2 | 54.0 |
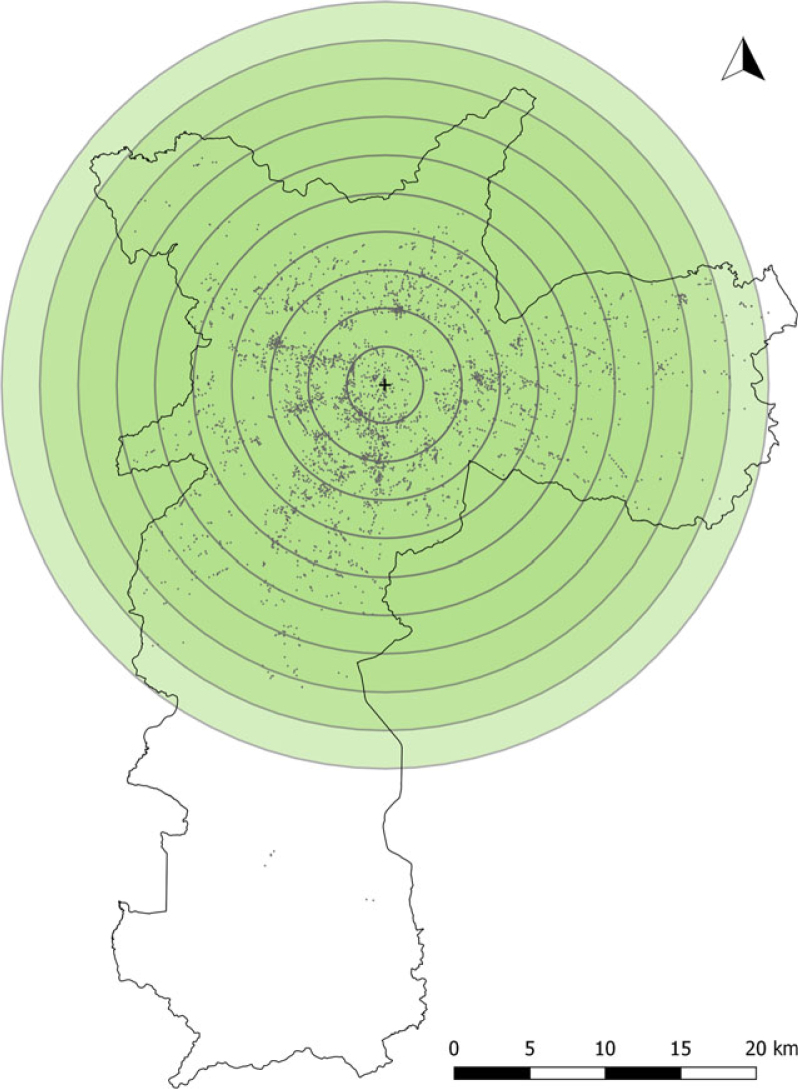
The city presented an overall practice-to-population ratio of 1:2,744 – or one primary dental clinic per 2,744 people. More than a quarter of clinics were located within 5 km of the city centre, and more than three-quarters were within 10 km. Almost all clinics were accounted for at 20 km, and only nine clinics were located more than 25 km from the city centre (Figure 2, Table 2). In comparison, less than one-tenth of the population were located within 5 km of the city centre, and one-third were within 10 km. Approximately 82.9% of people were accounted for at 20 km, and only 2.6% of the population were located more than 25 km out (Figure 2, Table 2).
Figure 2.
Distribution of fixed primary dental clinics in São Paulo city, Brazil. Clinics (grey dots) are presented against buffers (green) of increasing radii of 2.5 km out from the city centre, Praça da Sé (black cross).
Table 2.
Practice-to-population ratios of fixed primary dental clinics at various distances out from the city centre (Praça da Sé) in São Paulo city, Brazil
| Distance from city centre (km) | Population (n (%)) | Practices (n (%)) | Practice-to-population ratio (1:n) |
|---|---|---|---|
| 0–2.5 | 375,548 (3.3) | 373 (9.1) | 1,007 |
| 2.5–5 | 619,815 (5.5) | 795 (19.4) | 780 |
| 5–7.5 | 1,278,769 (11.4) | 1,227 (29.9) | 1,042 |
| 7.5–10 | 1,536,261 (13.7) | 761 (18.6) | 2,019 |
| 10–12.5 | 1,652,447 (14.7) | 402 (9.8) | 4,111 |
| 12.5–15 | 1,524,410 (13.5) | 211 (5.1) | 7,225 |
| 15–17.5 | 1,151,817 (10.2) | 138 (3.4) | 8,347 |
| 17.5–20 | 1,193,170 (10.6) | 107 (2.6) | 11,151 |
| 20–22.5 | 903,944 (8.0) | 61 (1.5) | 14,819 |
| 22.5–25 | 728,634 (6.5) | 17 (0.4) | 42,861 |
| 25+ | 287,389 (2.6) | 9 (0.2) | 31,932 |
| Total* | 11,252,204 (100.0) | 4,101 (100.0) | 2,744 |
Totals may not add due to rounding.
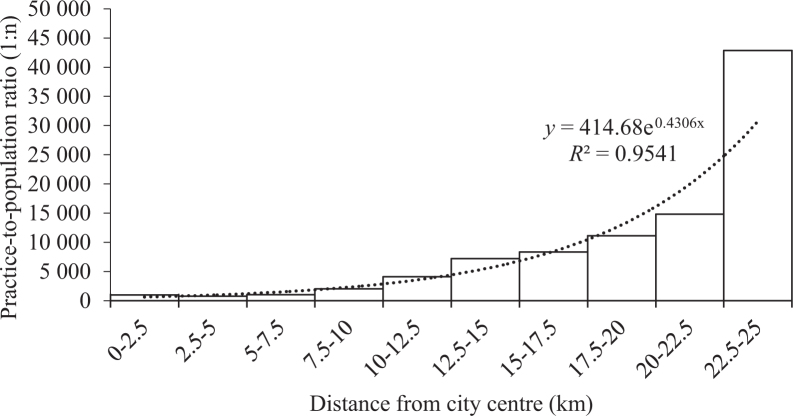
Practice-to-population ratios were lowest at the 2.5–5 km catchment (1:780) – marginally greater than the first 2.5 km catchment (1:1,007). Ratios increased exponentially with increasing distances out from the city centre (y = 414.68e0.4306x), up until the 22.5–25 km catchment (1:42,861) (Table 2, Figure 3). The greatest change in density occurred between the 20 and 22.5 km catchment (1:14,819) and the 22.5–25 km catchment (1:42,861), which presented a tripling in paucity. Clinics located more than 25 km out presented a smaller ratio (1:31,932) (Table 2, Figure 3).
Figure 3.
Practice-to-population ratios of fixed primary dental clinics at various distances out from the city centre (Praça da Sé) in São Paulo city, Brazil. Ratios for census tracts located more than 25 km out from the city centre were excluded.
Discussion
The present research aimed to determine the spatial distribution of fixed primary dental clinics in São Paulo city, testing the hypothesis that clinics are maldistributed across the city. The study found that two-thirds of the population live within 0.5 km of at least one clinic – a testament to how densely built and densely populated the city is. The close proximity of all clinics (with respect to population distribution) has never been observed in the literature; this is not surprising, seeing as São Paulo city is the first megacity to be studied this way. However, tracts located further away from the clinics were typically characterised as sociodemographically disadvantaged, evidence for the maldistribution of clinics.
The city presented an overall practice-to-population ratio of 1:2,744. Hence, each clinic should be responsible for 2,744 people ceteris paribus – like that observed in Australia, New Zealand and the USA16., 18., 19.. However, the geospatial models confirm that this is not the case. Clinics within 10 km of the city centre presented practice-to-population ratios well below the overall average. In contrast, peripheral clinics presented higher ratios and thus, are responsible for a larger population than those more centrally located. In other words, peripheral tracts have a greater sparsity of clinics, as consistent with the hypothesis that clinics are maldistributed.
The degree of sparsity was found to increase with increasing distance – reflected in the exponential change in ratios. The most peripheral tracts presented a sparsity of provision of 40 times that of the most central tracts. Similar methods have only been applied to Auckland, New Zealand, which presented a doubling in paucity between those within 2.5 km of the centre (1:1,300) and those 12.5 km out (1:2,700)20. Hence, the degree of maldistribution is greater in São Paulo city than in Auckland.
One dilemma faced by studies regarding spatial accessibility is determining optimum practice-to-population ratios21. For example, the ratios presented by Auckland could be considered a case of oversupply, and that the ratios in São Paulo city are sufficient to meet population demands. Regardless, the present findings – together with previous studies – raise some key questions: what level of maldistribution is society willing to accept, and what density of practices in central tracts is considered a case of oversupply21?
Answers to these questions are complex and likely impossible, given the number of factors affecting health, disease, demand and utilisation. For example, patients often seek treatments outside of their immediate vicinity22. In many instances, interactions with healthcare are organised around other priorities, such as work or school, and care is obtained nearby14. In São Paulo city, employment opportunities are largely concentrated around the historical centre, which contains a high concentration of clinics13., 23..
Understanding the spatial distribution – or rather, the maldistribution – of these services is fundamental for optimising the allocation of human and financial resources to areas of the greatest privation13., 24.. The present geospatial models provide a rapid shortlisting of potential sites for future improvements, which provides an effective method for evidence-based policymaking17., 25.. Policy solutions for underserved sites range from simple advertising for private practices, to private practice incentivisation schemes, to full government-funded schemes25. Another strategy could involve the deployment of mobile dental units to deprived areas15.
Note that measuring accessibility in terms of distance poses some inherent limitations. The present study used discrete arbitrary units – specifically census tracts and buffers – and straight-line distances to represent utilisation patterns, which do not consider where patients are seeking treatment14. For a more accurate picture of access, future studies should explore the role of continuous space on utilisation patterns16. Possible disaggregated zonal approaches include Global Positioning Systems (GPS), remote sensing, aerial photography and simulation-based approaches26.
Practice-to-population ratios also present some inherent limitations – principally that they are insensitive to the complexity of dental workforce planning. Ratios fail to consider the many variables governing the productive capacity of healthcare systems – such as operating hours and the number of practitioners – in addition to the cultural, social and economic drivers19., 27.. Dentist-to-population ratios could substantiate some of these questions in future assessments27.
Future research should also consider distinguishing between public and private services, which would serve to better inform the workforce planning process18., 28., 29.. Subsequent studies should also consider mapping primary dental clinics against the distribution of specialists, the supply of fluoridated water and the burden of oral diseases, for a clearer assessment of the inequity of access13., 25..
In closing, the present findings are confirmatory of the proposed hypothesis that primary dental clinics are maldistributed across São Paulo city. This study is the first of its kind to be conducted in São Paulo city – and South America at large – and the only study to be conducted on a megacity to date.
Acknowledgements
None.
Funding
None.
Conflict of Interest
None.
References
- 1.Alonge O, Peters DH. Utility and limitations of measures of health inequities: a theoretical perspective. Global Health Act. 2015;8:27591–27599. doi: 10.3402/gha.v8.27591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Q. 2005;83:1–28. [PubMed] [Google Scholar]
- 3.Gwatkin DR. Health inequalities and the health of the poor: what do we know? What can we do? Bull World Health Organ. 2000;78:3–18. [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen PE, Bourgeois D, Ogawa H, et al. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661–668. [PMC free article] [PubMed] [Google Scholar]
- 5.Peres MA, Barbato PR, Reis SCGB, et al. Tooth loss in Brazil: analysis of the 2010 Brazilian oral health survey. Rev Saude Publica. 2010;2014:78–89. doi: 10.1590/s0034-8910.2013047004226. [DOI] [PubMed] [Google Scholar]
- 6.Blane D. Disease aetiology and materialist explanations of socioeconomic mortality differentials. Eur J Public Health. 1997;7:385–391. [Google Scholar]
- 7.Sisson KL. Theoretical explanations for social inequalities in oral health. Community Dent Oral Epidemiol. 2007;35:81–88. doi: 10.1111/j.1600-0528.2007.00354.x. [DOI] [PubMed] [Google Scholar]
- 8.Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. Int J Health Geogr. 2004;3:3–15. doi: 10.1186/1476-072X-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Tudor Hart J. The inverse care law. Lancet (London, England) 1971;1:405–412. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 11.Carvalho MS, Souza-Santos R. Analysis of spatial data in public health: methods, problems, and perspectives. Cadernos de Saúde Pública. 2005;21:361–378. doi: 10.1590/s0102-311x2005000200003. [DOI] [PubMed] [Google Scholar]
- 12.Graham AJ, Atkinson PM, Danson FM. Spatial analysis for epidemiology. Acta Trop. 2004;91:219–225. doi: 10.1016/j.actatropica.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 13.Pereira SM, Ambrosano GMB, Cortellazzi KL, et al. Geographic Information Systems (GIS) in assessing dental health. Int J Environ Res Public Health. 2010;7:2423–2436. doi: 10.3390/ijerph7052423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higgs G. The role of GIS for health utilization studies: literature review. Health Serv Outcomes Res Methodol. 2009;9:84–99. [Google Scholar]
- 15.Pucca GA, Gabriel M, de Araujo ME, et al. Ten years of a national oral health policy in Brazil: innovation, boldness, and numerous challenges. J Dent Res. 2015;94:1333–1337. doi: 10.1177/0022034515599979. [DOI] [PubMed] [Google Scholar]
- 16.Almado H, Kruger E, Tennant M. Application of spatial analysis technology to the planning of access to oral health care for at-risk populations in Australian capital cities. Aust J Prim Health. 2013;21:221–226. doi: 10.1071/py13141. [DOI] [PubMed] [Google Scholar]
- 17.Rocha CM, Kruger E, McGuire S, et al. Role of public transport in accessibility to emergency dental care in Melbourne, Australia. Aust J Prim Health. 2013;21:227–232. doi: 10.1071/py13102. [DOI] [PubMed] [Google Scholar]
- 18.Kruger E, Whyman R, Tennant M. High-acuity GIS mapping of private practice dental services in New Zealand: does service match need? Int Dent J. 2012;62:95–99. doi: 10.1111/j.1875-595X.2011.00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kurcz R, Kruger E, Tennant M. Using GIS to analyse dental practice distribution in Indiana, USA. Community Dent Health. 2013;30:155–160. [PubMed] [Google Scholar]
- 20.Kruger E, Whyman R, Tennant M. High acuity GIS comparison of dentist and doctor surgery locations in Auckland, New Zealand. Community Dent Health. 2013;30:83–87. [PubMed] [Google Scholar]
- 21.Tennant M, Kruger E. Turning Australia into a ‘flat-land’: what are the implications for workforce supply of addressing the disparity in rural–city dentist distribution? Int Dent J. 2014;64:29–33. doi: 10.1111/idj.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tennant M, Kruger E. A national audit of Australian dental practice distribution: do all Australians get a fair deal? Int Dent J. 2013;63:177–182. doi: 10.1111/idj.12027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zandonade P, Moretti R. O padrao de mobilidade de Sao Paulo e o pressuposto de desigualdade. EURE. 2012;113:77–97. [Google Scholar]
- 24.Antunes JLF, Frazão P, Narvai PC, et al. Spatial analysis to identify differentials in dental needs by area-based measures. Community Dent Oral Epidemiol. 2002;30:133–142. doi: 10.1034/j.1600-0528.2002.300207.x. [DOI] [PubMed] [Google Scholar]
- 25.Shiikha Y, Kruger E, Tennant M. Rural and remote dental services shortages: filling the gaps through geo-spatial analysis evidence-based targeting. Health Inf Manage J. 2015;44:39–44. doi: 10.1177/183335831504400305. [DOI] [PubMed] [Google Scholar]
- 26.Wiehe SE, Carroll AE, Liu GC, et al. Using GPS-enabled cell phones to track the travel patterns of adolescents. Int J Health Geogr. 2008;7:22–32. doi: 10.1186/1476-072X-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tennant M, Kruger E, Shiyha J. Dentist-to-population and practice-to-population ratios: in a shortage environment with gross mal-distribution what should rural and remote communities focus their attention on? Rural Remote Health. 2013;13:2518–2524. [PubMed] [Google Scholar]
- 28.Kruger E, Tennant M, George R. Application of geographic information systems to the analysis of private dental practices distribution in Western Australia. Rural Remote Health. 2011;11:1736–1744. [PubMed] [Google Scholar]
- 29.Antunes JLF, Narvai PC. Políticas de saúde bucal no Brasil e seu impacto sobre as desigualdades em saúde. Rev Saude Publica. 2010;44:360–365. [Google Scholar]