Abstract
Background: The recognition of work stressors and their links to sociodemographic characteristics, health behaviours and coping strategies is important for enhancing the working conditions of dentists. Aim: The aim of our study was to identify and rank work stressors in dentists from Cluj-Napoca, Romania, and to investigate their potential links to sociodemographic characteristics, health behaviours and coping strategies. Study design: A questionnaire based on the Work Stress Inventory for Dentists (WSID) was delivered to a cross-sectional sample of 250 dentists working in six neighborhoods across Cluj-Napoca, Romania, as well as at the local Faculty of Dentistry. We collected and analysed information on sociodemographic characteristics, work stressors, health behaviours and coping strategies. Results: Time and scheduling pressure, concerns about the future and pay-related work stressors were found to rank highest among the categories of work stressors investigated. Higher work stress was significantly linked to higher workloads, lower job satisfaction, poorer eating and exercise habits, higher work pain and discomfort, lower perceived health and less sleep. Job satisfaction was the single best predictor variable of work stress scores. The most frequently used coping strategy to deal with work stress was resting and taking breaks. Only one-quarter of respondents used active coping strategies. Conclusion: Our findings suggest that work stress is linked to a number of detrimental attitudes in dentists and that there is room for dentists to make lifestyle improvements.
Key words: Professional work stress, dentist, health behaviour, coping strategy
Introduction
Stress is a manifestation appearing when environmental demands tax or exceed the adaptive capacity of an organism, thus leading to psychological or biological changes1., 2.. Immediate stress may produce temporary disturbances of cognition, emotion and behaviour that can adversely affect the person’s well-being. Continuous long-term stress, however, may lead to physiological changes that exacerbate, or even cause, disease; a person can become predisposed to illnesses affecting various bodily systems, including the immune, central nervous, gastrointestinal, endocrine and genitourinary systems, as well as the skin, muscle and connective tissue1. Evidence suggests that chronic stress may be linked to poorer health practices, accelerated disease progression, greater symptom reporting, more frequent health-service utilisation and increased mortality3.
Work stress in dentistry has been examined for over four decades now, beginning with studies such as that of Howard et al.4, in 1976, which highlighted that work stress was linked to the physical and psychological well-being of dentists. Indeed, research has claimed that dentists are at the top of the chart for stressful professions, with academics and physicians referring to dentistry as being an ‘impossible’ profession, in terms of balancing working life, family life and having time to oneself5. Aside from this, dentists face numerous daily workplace challenges, such as working in uncomfortable positions, high noise levels, defective equipment, variability of treatment outcomes, financial matters, legal hazards, handling of difficult patients, coordination of staff members, time and scheduling pressures, administrative responsibilities, periods of prolonged concentration and social isolation6., 7., 8.. Such work stressors may disrupt the physical and mental well-being of dentists, progressively leading to outcomes such as burnout, the development of anxiety and depression and, at times, even to suicidal thoughts6., 8.. Such major and potentially lethal consequences of exposure to prolonged work stress explain the importance of using efficient methods to cope with daily work stress.
Stress-coping strategies can be divided into two broad categories: approach-oriented strategies and avoidance-oriented strategies. An approach-oriented strategy, or active strategy, refers to dealing with problems or confronting them in a direct manner. It requires an active attempt to resolve the stressor that is causing the problem. Conversely, an avoidance-oriented strategy implies dealing with problems indirectly, by avoiding active confrontation with the stressor and thereby reducing emotional tension associated with the stressor causing the problem9., 10..
In the late 1980s, Cooper et al.11 proposed that accurate diagnosis of the nature of work stressors in dentistry was a requisite for attempting to minimise work stress, maximise job satisfaction and improve the general well-being of dentists. With this intention, they developed a Work Stress Inventory for Dentists (WSID), which allowed them to investigate the relationship between some of the possible sources of work stress and both job satisfaction and mental ill-health. Since then, a number of studies have employed modified versions of the WSID in questionnaires, in order to examine suspected links between work stress and factors relating to various sociodemographic characteristics, health behaviours and coping strategies of dentists12., 13., 14., 15..
These studies have been able to suggest links between work stress and factors of the aforementioned categories. A recent systematic review of factors contributing to burnout in dentists and dental students suggests that younger age, male gender, personality types, high job-strain and long working hours may play important roles16.
In the current study, we aimed to identify and rank work stressors, as well as to investigate their relationship to sociodemographic characteristics, health behaviours and coping strategies, in dentists practising in Cluj-Napoca, Romania.
Therefore, our study assessed whether sufficient evidence exists to reject the null hypotheses that sociodemographic characteristics, health behaviours and coping strategies did not influence the level of work stress in dentists from Cluj-Napoca, Romania.
Materials and Methods
Between the beginning of April and the end of July 2014, a questionnaire based on the WSID was personally delivered to a cross-sectional sample of 250 dentists working in six neighborhoods across Cluj-Napoca, Romania.
The computed sample size necessary to achieve a test power of 1−β = 0.95, assuming a medium effect size of d = 0.6, was 148 respondents. The 250 questionnaires distributed exceeded this computed sample size by almost 70%, in order to compensate for a possibly low response rate.
Dental offices in six neighborhoods of Cluj-Napoca, Romania, were randomly selected from a complete listing provided by the Public Health Registry of Cluj County. Other dental offices that were situated on the way to the randomly selected offices were also visited to deliver the questionnaire. In addition, questionnaires were distributed to teaching staff working at the Faculty of Dentistry of the Iuliu Hatieganu University of Medicine and Pharmacy, who also practised part-time in private dental offices situated in Cluj-Napoca.
Inclusion criteria for survey participation consisted of being a dentist registered with the Romanian College of Dentists and practising either full-time or part-time as a resident, specialist or consultant. Exclusion criteria were defined as not practising within the city of Cluj-Napoca, being on leave of absence, not wishing to complete the questionnaire or not adequately completing at least 80% of the questionnaire (i.e. any missing answer in the Professional Stress part of the questionnaire or more than 12 missing answers in the Socio-demographic and Daily Habits parts of the questionnaire).
In line with the 2013 revision of the World Medical Association (WMA) Declaration of Helsinki, upon receiving the questionnaires, all potential survey participants were provided with a written letter of introduction and information about the aims and methods of the study, clearly stating that their individual responses were to be used for research while being kept anonymous and confidential. As part of the informed consent process of every potential survey participant, supplementary information was provided verbally whenever needed, in order to ensure that all information was well understood. The agreement to complete and return the anonymous questionnaire was regarded as proper informed consent to participate in this study.
A complete ethical review procedure for this study was waived by the Research Ethics Committee of the Iuliu Hatieganu University of Medicine and Pharmacy because the study was classified as minimal-risk research, using an anonymous survey of public behaviour, with a very low risk of causing emotional or physical stress to study participants, and not placing research subjects at risk of legal liability or damage to their financial standing, employability or reputation. No traceable personal data were collected or stored as part of this survey.
Measures
Information about the sociodemographic background, work stressors, health behaviours and coping strategies of respondents was collected using a questionnaire containing 64 questions, divided into three main parts: Socio-demographic Data (16 questions); Professional Stress (30 questions); and Daily Habits (18 questions).
Sociodemographic data included age, gender, relationship status, children, university affiliation, number of workplaces, number of work days and work hours per week, number of vacation weeks per year and job satisfaction.
A modified version of the WSID was used that adhered more closely to the local working conditions of dentists. A total of 30 work stress items was used. These items were divided into seven broad categories: time and scheduling pressures (four items); pay-related stress (four items); staff and technical problems (four items); problems with patients (four items); concerns about the future (four items); nature of work (six items); and personal dissatisfaction (four items).
Respondents were asked to rate each stressor by frequency with which it was usually experienced. A six-point Likert-type scale, ranging from ‘never’ to ‘always’ causing stress, was used to quantify stressors. All statements indicating the presence of stress were scored on an increasing scale from 0 (never feeling stressed) to 5 (always feeling stressed). Each respondent was assigned a total stress score corresponding to the sum of all 30 items.
Questions relating to health behaviour focussed on frequency and length of physical exercise, eating habits, smoking, drinking, physical pain or discomfort at work, sleeping habits, weight, height, medications taken over the past month, perceived health and measures to improve health.
Coping strategies used to deal with stress were also quantified using a six-point Likert-type scale. Active coping strategies to deal with stress were defined as changing the work environment, active changes in the relationship with patients, employees or colleagues and consulting a stress specialist.
Data analysis
Data were handled using complete case analysis because data were rarely missing (0.6% of all questionnaire items) after having excluded four inadequately completed questionnaires.
The reliability of the modified WSID questionnaire has been investigated using Cronbach’s Alpha. Sampling adequacy for factor analysis was confirmed using the Kaiser–Meyer–Okin (KMO) measure, and factor analysis was performed for the seven work stress categories investigated using the modified WSID questionnaire.
Sociodemographic characteristics, health behaviours and stress coping strategies were described and summarised using descriptive statistics: mean, median, standard deviation (SD), standard error (SE), absolute and relative frequencies, as well as 95% confidence intervals. Confidence intervals were corrected for a finite population of not more than 700 dentists, with a sex distribution of 37% male and 63% female, estimated to be active in Cluj-Napoca, Romania, based on data published by the Romanian College of Dentists17.
Work stress scores were calculated using two computational methods. The first approach was mean oriented, summing the scores for each stress item and then dividing this sum by the number of responses. The second method was frequency oriented; Likert scores of 4 or 5, corresponding to ‘very often causing stress’ and ‘always causing stress’, were assigned scores of 1, and Likert scores of <4 were assigned a score of 0. The top ranking work stressors were considered to be those appearing in the top 10 for both computational approaches.
Using histograms, descriptive statistics and a Kolmogorov–Smirnov normality test, the distribution of these overall work stress scores was first investigated and confirmed to stem from a normally distributed population.
Overall work stress scores were compared based on sociodemographic characteristics, health behaviours, as well as stress coping strategies, using t-tests. Bartlett’s test for inequality of variances was used in order to determine if a t-test should assume equal or unequal variances. Further on, individual work stress categories of time and scheduling pressures, pay-related stress, worries about the future and personal dissatisfaction were also compared based on sociodemographic characteristics, health behaviours and stress coping strategies.
In order to perform these comparisons, sociodemographic characteristics and health-related behaviours were dichotomised based on threshold values chosen in accordance with similar studies11., 12., 13., 14., 15., 18., 19., 20. and other relevant literature16., 21..
Hypotheses regarding categorical variables (e.g. differences in coping strategies based on gender) were investigated using chi-square tests.
Statistical significance was set at α = 0.05, with a Bonferroni correction down to α = 0.0025 for multiple comparisons involving the same stress scores grouped by up to 20 predictors.
Simple linear regression models were used to identify the best single predictors of scores corresponding to each work stress category investigated. To identify the best predictors of overall stress scores, a multivariate analysis adjusted for age was performed. Stress score variance that could be explained by the investigated predictors was computed and expressed as an r2 value.
Sample size and power calculations were performed using G*Power 3.1.9 (Heinrich Heine University, Düsseldorf, Germany).
Data analysis was performed using Microsoft Excel (Microsoft, Redmond, WA, USA), EpiInfo 7 (Centers for Disease Control and Prevention, Atlanta, GA, USA) and PSPP 0.10.2 (GNU Project, Free Software Foundation, Boston, MA, USA).
Results
After excluding four inadequately completed questionnaires, the survey yielded a response rate of 46.4%. This allowed us to analyse 116 questionnaires, thereby achieving a test power of 89% for comparisons between groups of equal size and always higher than 80% for comparisons involving groups of unequal size.
The reliability of the modified WSID questionnaire was confirmed by Cronbach’s Alpha (α = 0.842). Sampling adequacy for factor analysis was confirmed by a KMO value of 0.733. Factor analysis of the modified WSID questionnaire confirmed good loading of questionnaire items, corresponding to the seven categories of work stress investigated (time and scheduling pressures, pay-related stress, staff and technical problems, problems with patients, concerns about the future, nature of work and personal dissatisfaction).
Descriptive characteristics of the study sample
Sociodemographic descriptors
Age and gender
Ten percent of the responding dentists were older than 40 years of age and 45% were between 26 and 30 years of age. Female respondents accounted for 65.5% (n = 76) of the study sample, while male respondents accounted for 34.5% (n = 40).
Workplace type, number of workplaces, work days and work hours
Among the responding dentists, 57.76% (n = 67) worked only in private offices, while 42.24% (n = 49) worked both in private offices and as teaching staff at the Cluj-Napoca University of Medicine and Pharmacy.
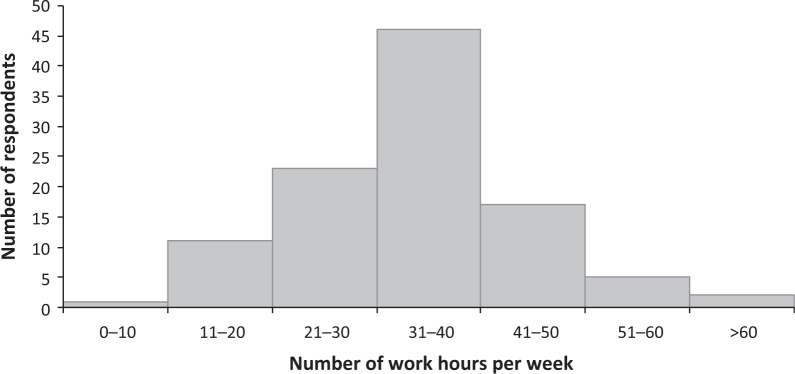
Over 70% of the responding dentists worked in more than one workplace: 34% worked in two workplaces; 31% worked in three workplaces; and 6% worked in more than three workplaces. The majority of dentists (60%) had a 5-day work week. Approximately 40% of the respondents worked between 31 and 40 hours a week, 20% between 21 and 30 hours per week, and 15% between 41 and 50 hours per week (Figure 1).
Figure 1.
Distribution of work hours per week indicated by respondents.
Job satisfaction
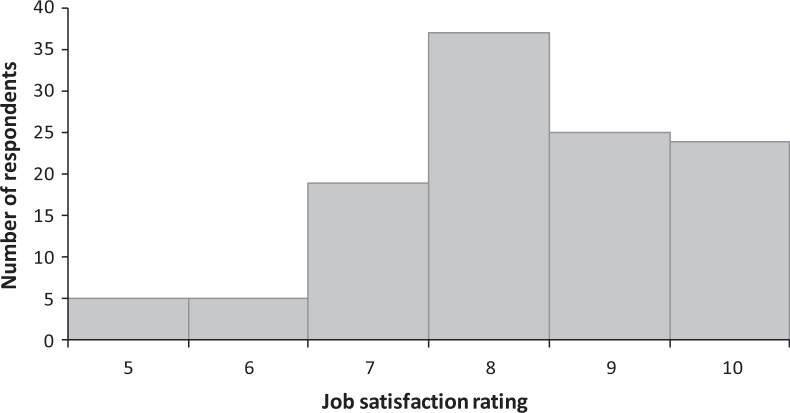
Over two-thirds of dentists rated their job satisfaction with scores of ≥8 out of 10 (Figure 2).
Figure 2.
Job satisfaction indicated by respondents on a scale from 1 to 10.
Work stressors
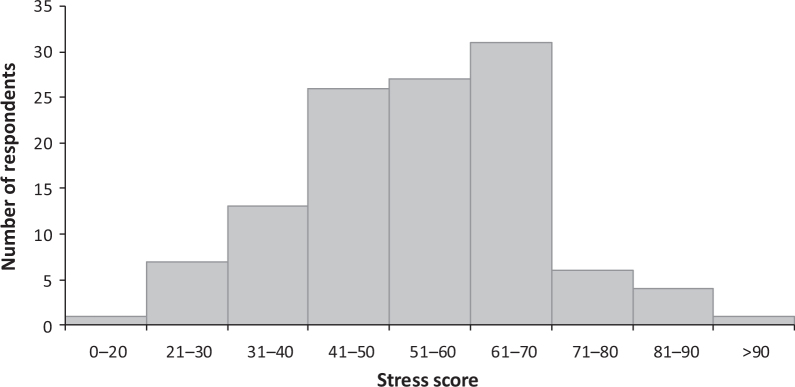
Overall stress scores fluctuated widely among dentists, ranging from < 20 to > 90 (Figure 3). The scores followed a fairly normal distribution, with a mean stress score of 54, a median stress score of 55, SE = 1.39, skewness = −0.063 and kurtosis = 0.289. The top ranking stressors using the two different computational approaches are presented in Table 1.
Figure 3.
Overall stress score distribution in the study sample.
Table 1.
Ranking of the investigated work stressors based on the ranking methods presented
| First method (mean oriented) | Rank | Second method (frequency oriented) |
|---|---|---|
| Long working hours | 1 | Tired after work |
| Tired after work | 2 | Worry about the future direction of my career |
| Worry about the future direction of my career | 3 | High work expenses |
| High work expenses | 4 | Long periods of concentration without breaks |
| Long periods of concentration without breaks | 5 | Long working hours |
| Work under time pressure | 6 | Insufficient income for desired lifestyle |
| Insufficient income for desired lifestyle | 7 | Work under time pressure |
| Insufficient time for family and friends | 8 | Insufficient time for family and friends |
| Treating difficult patients | 9 | Worry about whether will live well at retirement |
| Patients cancel appointments | 10 | Strong competition with other dentists |
| Strong competition with other dentists | 11 | Delays with work schedule |
| Worry about whether will live well at retirement | 12 | Treating difficult patients |
| Delays with work schedule | 13 | Possible viral infection |
| Possible viral infection | 14 | Fear of malpraxis |
| Defective equipment and materials | 15 | Conflict between medical ethics and profit |
| Fear of malpraxis | 16 | Defective equipment and materials |
| Fear of mistakes in medical practice | 17 | Believe another career would have been better |
| Unsatisfactory collaboration with dental technicians | 18 | Patients cancel appointments |
| Fear of emergency in the office | 19 | Fear of emergency in the office |
| Unsatisfied with auxiliary help | 20 | Unsatisfied with auxiliary help |
| Patients do not pay on time | 21 | Patients do not pay on time |
| Not capable of meeting my professional goals | 22 | Not capable of meeting my professional goals |
| Conflict between medical ethics and profit | 23 | Fear of mistakes in medical practice |
| Feel that patients do not appreciate my work | 24 | Unsatisfactory collaboration with dental technicians |
| Work is repetitive and monotonous | 25 | Work is repetitive and monotonous |
| Believe another career would have been better | 26 | Cause unwanted pain to patients |
| Cause unwanted pain to patients | 27 | Feel isolated in daily work |
| Unpleasant collaboration with patients | 28 | Feel that patients do not appreciate my work |
| Feel isolated in daily work | 29 | Unpleasant collaboration with patients |
| Problems communicating with other dentists | 30 | Problems communicating with other dentists |
Health behaviours
Physical exercise
About one-third (34%) of respondents exercised one to two times a week and about a quarter (26%) exercised three to four times a week for more than 15 minutes. Approximately half (49%) of the respondents exercised between 30 minutes and 1 hour, and over one-quarter (27%) exercised between 1 and 2 hours during each exercise session. The vast majority of dentists (72%) participated in seasonal sports.
Eating behaviours
With regard to eating habits, slightly over one-third of dentists ate breakfast every morning, two-fifths rarely or never snacked between meals and nearly three-quarters usually or always ate homemade food. Just over half of the dentists questioned believed that their diet was well-balanced most of the time or always.
Smoking and alcohol consumption
The majority of dentists were non-smokers (66%), while 16% and 18% were occasional and inherent smokers, respectively. Consumption of alcohol was low; around 80% of dentists consumed alcohol once a month or less. Per drinking event, the quantity of alcohol consumed was less than 2 units for 53% of respondents and 2–5 units for 39% of respondents. Very few dentists (8%) admitted drinking more than 5 units of alcohol per drinking event.
Sleeping habits
Three-quarters of dentists slept for fewer than 8 hours per night, 39% slept for 7 hours and 25% slept for 6 hours. The mean number of sleep hours per night was 6.8 among the dentists sampled.
Physical pain or discomfort
Half of the dentists reported having no symptoms of pain or discomfort at work. Minor problems, which did not prevent dentists from performing their activities at work, were reported by 41% of respondents. The remaining 9% experienced forms of work pain and discomfort that stopped them from performing certain activities.
Body mass index
Sixty-eight percent of the dentists investigated had a body mass index (BMI) in the normal range (BMI = 18.5–24.9). One-quarter were overweight (BMI = 25–29.9), 4% were obese (BMI >30) and 4% were underweight (BMI <18.5). A significantly higher proportion of female dentists (87%) had BMI values in the normal range (BMI = 18.5–24.9) compared with male dentists (44%), (P < 0.001; chi-square test).
Medications
About half of the respondents had taken analgesic and anti-inflammatory medication in the last month. Vitamins were used by 30%, while 2–9% took other medications. Only about one-quarter of dentists had taken no medication at all in the last month.
Perceived health
Many dentists perceived their health as being very good (37%) or good (45%). A smaller percentage of dentists perceived their health as being excellent (9%), satisfactory (8%) or poor (1%).
Health improvement measures
Over half of the dentists believed that more physical exercise (57%), better nutrition (54%) and more relaxation time (52%) would improve their health. Other factors perceived as measures to improve health were: more sleep (46%); respecting meal times (45%); weight loss (38%); better stress control (33%); less smoking (14%); and less alcohol consumption (3%).
Coping strategies
Almost 90% of dentists claimed to adopt resting and taking breaks as a major coping strategy against work stress. In second place was socialising, while close together, in third and fourth places, were having hobbies and playing sports. Just one-quarter of dentists used active coping strategies to deal with work stress and only a few smoked or drank alcohol (Table 2).
Table 2.
Coping strategies for reducing work stress in the study sample
| Rank | Coping strategy | Frequency | ||
|---|---|---|---|---|
| Overall | Male | Female | ||
| 1 | Resting and taking breaks | 87 (81–93) | 80 (68–92) | 91 (85–97) |
| 2 | Interactions with people | 64 (56–72) | 55 (40–70) | 68 (58–78) |
| 3 | Hobbies | 59 (51–67) | 63 (49–77) | 58 (48–68) |
| 4 | Sports | 59 (51–67) | 65 (51–79) | 55 (45–65)* |
| 5 | Forgetting about work | 41 (33–49) | 40 (26–54) | 42 (32–52) |
| 6 | Spending money, shopping | 31 (23–39) | 15 (5–25) | 39 (29–49)** |
| 7 | Active coping strategies | 25 (18–32) | 18 (7–29) | 29 (20–38) |
| 8 | Eating | 14 (8–20) | 8 (0–16) | 17 (9–25) |
| 9 | Smoking | 9 (4–14) | 13 (3–23) | 8 (2–14) |
| 10 | Alcohol | 3 (2–6) | 3 (0–8) | 3 (0–6) |
Values are given as % (95% CI). *P = 0.01; **P = 0.007 (chi-square test).
Analysis of factors connected to work stress
Significantly increased overall stress scores were found to be linked to the factors listed in Table 3.
Table 3.
Overall stress score differences based on demographic and health-related characteristics
| Lower stress scores | Higher stress scores | t-test P-value |
|---|---|---|
| ≤2 workplaces | >2 workplaces | 0.017 |
| ≤30 hours of work/week | >30 hours of work/week | 0.05 |
| ≥8 job satisfaction | <8 job satisfaction | <0.001** |
| Seasonal sports | No seasonal sports | 0.028 |
| Usually or always eats cooked food | Half the time or less eats cooked food | 0.007 |
| Usually or always a well-balanced nutrition | Half the time or less a well-balanced nutrition | 0.001** |
| Consumes alcohol ≥3–4 times/week | Consumes alcohol <3–4 times/week | 0.026 |
| No work pain or discomfort | Work pain or discomfort | 0.005 |
| ≥8 hours of sleep/night | <8 hours of sleep/night | 0.002** |
| Very good or excellent perceived health | Satisfactory, poor perceived health | 0.001** |
Significant at Bonferroni corrected level (P < 0.0025).
Physical exercise was a factor which almost achieved uncorrected statistical significance (P = 0.059). The overall stress scores of subjects who exercised, for a minimum of one or two times a week, for at least 30 minutes to 1 hour, tended to be lower compared with those of dentists who exercised less (exercising for intervals shorter than 30 minutes or exercising rarely to never).
Higher time and scheduling pressure stress was linked to working in more than two workplaces (P = 0.002), working >5 days per week (P = 0.009), working >30 hours per week (P < 0.001), sleeping <8 hours per night (P = 0.008), eating homemade food for only half of meals or less (P < 0.001) and having a self-perceived unbalanced nutrition (P < 0.001). Dentists who also taught at the University exhibited higher time and scheduling pressure types of stress compared with dentists who only practised in dental offices (P = 0.03), but overall stress scores (P = 0.54) and job satisfaction scores (P = 0.5) were comparable between these two categories.
Regarding pay-related stress, significantly higher scores were associated with <2 weeks of vacation per year (P < 0.001) and job satisfaction scores of ≤8 (P = 0.003). Having or not having children did not reach statistical significance but exhibited a tendency towards uncorrected statistical significance (P = 0.069) in connection to pay-related stress.
Dentists with job satisfaction scores of <8 and those sleeping <8 hours per night exhibited significantly higher worries about future stress (P = 0.01 and P = 0.001, respectively).
Personal dissatisfaction stress was more prominent among male dentists compared with female dentists (P = 0.02). Personal dissatisfaction stress was particularly associated with work under time pressure (P < 0.001), long working hours (P = 0.003), long periods of concentration without taking breaks (P < 0.001), often to always feeling tired after work (P = 0.001), as well as with a self-perceived unbalanced nutrition (P = 0.005) and sleeping <8 hours per night (P = 0.001).
Coping strategies associated with reduced work stress
Eating (P = 0.030), resting and taking breaks (P = 0.037), as well as spending money and shopping (P = 0.041) were linked to lower overall stress scores.
More female than male dentists acknowledged shopping as a means for coping with stress (P = 0.007), while participating in sport was a stress-coping method preferred by male dentists (P = 0.01). No other significant differences were found between genders regarding the frequency of different coping strategies. Stress-coping methods were also similar between dentists who taught at the University compared with dentists who only practised in dental offices.
Association of BMI and perceived health
Dentists who rated their health as very good or excellent showed significantly lower BMI values (P < 0.001) compared with those who rated it as good, satisfactory or poor.
Predictors of work stress
The best single predictor of overall work stress, in a simple linear regression, was job satisfaction (r = 0.43, r2 = 0.18, P < 0.001). It also best predicted ‘pay-related’ (r = 0.34, r2 = 0.12, P < 0.001) and ‘worries about the future’ types of work stress (r = 0.28, r2 = 0.08, P = 0.003). For ‘time and scheduling pressure’ work stress, the best single predictor was the number of work hours per week (r = 0.52, r2 = 0.27, P < 0.001), while work under time pressure best predicted ‘personal dissatisfaction’ work stress (r = 0.46, r2 = 0.21, P < 0.001).
In multivariate analysis adjusted for age, the best multiple linear regression predictors of overall stress scores were job satisfaction (P < 0.001), the frequency and duration of physical exercise (P = 0.011), balanced nutrition (P = 0.014), work pain or discomfort (P = 0.037) and the number of workplaces (P = 0.038), with a multiple r = 0.62 and an adjusted r2 = 0.34.
Discussion
Our study demonstrated that work stress was significantly linked to a number of sociodemographic characteristics, health behaviours and coping strategies.
The main univariate findings of our study suggested that reduced overall work stress may be especially linked to high job satisfaction, sufficient sleep, balanced nutrition and regular physical exercise. These characteristics also reflected in excellent or very good self-perceived health.
In simple linear regressions, 18% of overall work stress variation was explained by job satisfaction, which also accounted for 12% of ‘pay-related’ stress and 8% of ‘worries about the future’ type of stress. ‘Time and scheduling pressure’ stress was best predicted by the number of work hours per week, at 27% of its variation. Working under time pressure predicted 21% of the variation in ‘personal dissatisfaction’ type stress.
Our age-adjusted multivariate analysis predicted 34% of overall stress variation based on job satisfaction, frequency and duration of physical exercise, nutrition balance, work pain or discomfort, and the number of workplaces.
Study strengths and limitations
The proportion of female (65.5%; n = 76) to male (34.5%; n = 40) respondents in our study closely mirrored the distribution of 63% female and 37% male dentists estimated to be active in Cluj-Napoca, Romania, based on data published by the Romanian College of Dentists17.
Nearly 60% of our survey respondents included dentists who only worked in private offices in Cluj-Napoca, while the remaining respondents were University teaching staff who also practised part-time in private dental offices. After consulting University statistics and official census data published by the Romanian College of Dentists17, we estimated the proportion of dentists who taught at the Dental School in Cluj-Napoca while also practising in private dental offices to be around 20% of all dentists practising in Cluj-Napoca (140 teaching staff, among approximately 700 practising dentists in Cluj-Napoca). Owing to a higher response rate in teaching dentists compared with dentists who worked only in private practices, the final proportion of dentists who also taught at the Cluj-Napoca Dental School (42.24%) exceeded the above estimate of their proportion among dentists practicing in Cluj-Napoca. This may have led to an overestimation of certain types of work-related stress in our sample. Time and scheduling type work stress, for instance, was found to be significantly higher in teaching dentists compared with dentists who only practised in private dental offices.
The fact that the resulting sample was predominantly young was probably because young dentists were more receptive to completing the questionnaire. Thus, the results of our study pertain mostly to dentists under the age of 40 and should be interpreted with caution for older age-groups.
Survey response rates have been reported to vary between 51.5% and 71.4% in health surveys of different lengths mailed per post22. Consequently, we tried to compensate for an estimated response rate of 60% by personally distributing (rather than mailing per post) almost 70% more questionnaires than the computed sample size. Despite these precautions, the main limitation of our study was its low response rate, of only 46.4%. This decreased our intended test power (0.95), but succeeded in ensuring test powers of > 0.8 in all planned comparisons.
Another limitation of our study, inherent to all questionnaire surveys, was its potential for information bias. A possibly lower reporting of socially undesirable factors, such as alcohol consumption or smoking, may have led to an underestimation of the frequency of such health-related behaviours. Conversely, it is also conceivable that an overly enthusiastic reporting of socially desirable behaviours, such as working numerous hours per week, undertaking physical exercise or having a balanced diet, may possibly have led to an overestimation of the frequency of such behaviours. Despite our questionnaires being completed and returned anonymously, an under- or over-reporting of certain health-related and stress-coping behaviours cannot be excluded, possibly leading to the above-mentioned effects on both the estimated frequencies of such behaviours and on their influence on work stress scores quantified through the WSID part of the questionnaire.
Comparison with previous findings
The facts that dentists do not perform adequate physical exercise on a daily basis, and that frequency of exercise rather than length of exercise was an issue, has been previously underlined about dentists in the UK by Kay and Lowe18, who reported that only 17% of dentists exercised daily. Our study found the frequency of physical activity to be even lower. With respect to the duration of exercise, our findings were almost identical to those found by Kay and Lowe18. Only 10% of dentists in our study exercised daily, and just 36% of respondents exercised three to four times per week or more. Compared with the study of Myers and Myers12, our population of dentists had poorer eating habits; just 36% of respondents ate breakfast daily (which was half of what Myers and Myers12 reported) and triple the amount of dentists in our study snacked between meals (61%). Interestingly, although our sample of dentists displayed poorer physical activity and eating habits, their BMI values were in healthier ranges compared with dentists in the UK12., 18.. Our study found that a greater proportion of female (87%) than male (44%) dentists had normal BMIs, thus reaffirming the claim of Kay and Lowe18 that female dentists have healthier BMIs.
Alcohol consumption among dentists in Romania was lower than among dentists in the UK. The majority of dentists from Cluj-Napoca, Romania (79%) drank alcohol only once a month or less, while 90% of dentists in the UK consumed alcohol regularly12. However, in our sample, four times as many dentists smoked compared with those in the study of Kay and Lowe18 and twice as many compared with those reported by Myers and Myers12. Nevertheless, cultural differences between the UK and Romania are likely to support different patterns of social acceptance regarding these behaviours, possibly accounting for parts of these rather important differences in reporting drinking and smoking.
It has been reported that dentists frequently worked with their back in an awkward position and thus experienced several types of work-related pain and discomfort18. Our study found that half of the respondents were free of pain and discomfort, which is higher than in other studies: Kay and Lowe18 found that 42% of dentists were free from pain and discomfort, while Myers and Myers12 reported that 37% were free from pain and discomfort. However, the lower occurrence of pain and discomfort in our study may also be attributed to the young age of dentists who responded to our survey. Still, it is worrying to learn that half of the dentists in our sample were already experiencing problems, which may worsen in later life, especially if ergonomic working positions are not properly adopted.
Only 46% of dentists included in our study rated their health as being excellent or very good, which is considerably lower than in the study of Kay and Lowe18 (67%). This may explain why over 90% of dentists in our study planned to take measures to improve their health; the top ranking measures included increased physical exercise (57%), better nutrition (54%) and more time to relax (52%). Although more respondents were satisfied with their health status in the investigation of Kay and Lowe18, still 90% planned to take action in order to improve their health, with the top-ranked measures being more exercise (58%), losing weight (42%) and improving eating habits (32%). Thus, two out of the top three measures intended to improve health were common between dentists in the UK and those in Romania. Another similarity between the results found by our study and those found by Kay and Lowe18 was that around one-third of dentists desired to have better control over work stress.
In a large survey performed by O’Shea et al.23 on nearly 1,000 American dentists attending an annual meeting of the American Dental Association, the top-ranking stressors included falling behind schedule, striving for technical perfection, causing pain or anxiety in patients, cancelled or late appointments and lack of cooperation from patients in the chair. In our stressor rankings, we found most of the work stressors to be part of the categories of time and scheduling pressures, followed by concerns about the future and related to pay. Among four studies to which we can readily compare our top five ranking work stressors, three12., 13., 14. found problems with patients and all four12., 13., 14., 15. found time and scheduling pressures as primary work stress categories. Although the top five work stressors in the investigation by Pouradeli et al.15 of Iranian dentists were not identical to those in our study, all stressors fitted into the same three categories as those found in our study: time and scheduling pressures; concerns about the future; and pay-related. It is noteworthy to mention that all five studies, ours included, had the category of time and scheduling pressures in common; this suggests that time and scheduling pressure stress may be ubiquitous to dentistry.
Our data analysis suggested that work stress was linked to increased workload, specifically to the number of work hours and workplaces. Previous findings, such as those of Myers and Myers12 in the UK, Ayers et al.13 in New Zealand and Pouradeli et al.15 in Iran, also reported that higher workload was associated with greater stress scores. A high level of significance (P < 0.001) was found between work stress and job satisfaction: respondents with higher stress levels had significantly lower job satisfaction scores. This is in line with the studies of Cooper et al.11 and Myers and Myers12, who also reported an inverse relationship between work stress and job satisfaction.
In the Netherlands, Gorter et al.24 reported dentists with a high burnout risk having health complaints and unhealthy behaviours, such as low levels of physical exercise, increased alcohol consumption and unhealthy diets, to a greater extent than dentists with a low burnout risk. In our study, work stress was also confirmed to be significantly associated with poorer health practices. Lower stress scores were detected in respondents who practised seasonal sports, as well as in those who ate homemade food and frequently maintained a well-balanced nutrition. To a slight degree, (P = 0.059), our study tended to confirm Myers and Myers’12 claim that lower physical exercise was linked to higher stress scores. Moreover, variables reflecting good health, such as the absence of work pain and discomfort, better perceived health and more sleep, were linked to lower stress scores. Myers and Myers12 also found that less sleep was associated with more work stress, but found no significant relationship between work pain or discomfort and work stress. In contrast to Myers and Myers12, we found that regular alcohol usage (≥3–4 times/week) could be related to lower stress levels. However, it is worth noting that only eight of the 116 dentists responding to our survey were part of this group. Therefore, although an uncorrected statistical significance level was reached (P = 0.026), accounting for how much alcohol was consumed on every occasion, studying a larger sample and testing a single hypothesis would be needed in order to suggest such a link. Finally, in contrast to other studies, we were unable to confirm that having children12, age14., 15., 16. or gender14., 15., 16., 19. was linked to higher work stress.
The most common coping strategies used to deal with work stress by dentists included in our study (see Table 2) were the same as in the study of Pouradeli et al.15, although in a different sequence. Ayers et al.13 reported interactions with people as being the most frequent coping strategy, while it only ranked second in our study. Smoking and alcohol were not commonly used coping strategies to deal with work stress, this being similar to the findings of Pouradeli et al.15 in dentists from Iran. In contrast, Ayers et al.13 reported that around one-quarter of respondents used alcohol to relieve stress, while Myers and Myers12 noted higher alcohol usage among respondents with higher stress scores. Once again, cultural diversity, leading to different levels of social acceptance and therefore reporting of this type of coping behaviour, may be partly responsible for these observed differences. Our study also found differences between male and female coping strategies, which is in accordance with the findings of Ayers et al.13, in dentists from New Zealand. Taking part in sports was preferred especially by male dentists, while going shopping was a coping strategy more often preferred by female dentists included in our study. Overall, just one-quarter of respondents in our study used active coping strategies to reduce stress (e.g. changing their work environment or consulting specialists for help). This low use of active coping strategies is consistent with previous literature13., 20., 25. confirming the need to promote the benefits26., 27. of active stress coping strategies for dentists across the globe.
Conclusions
Most dentists in our study exhibited elements of a sedentary lifestyle and poor eating habits. Moderate self-perceived health scores and an expressed desire to take measures to improve health indicated that many dentists seemed to be conscious of their unhealthy habits but did not take a proactive stance towards making improvements in their daily habits. The fact that half of the dentists surveyed took analgesics and that the same proportion experienced work pain and discomfort, despite the fact that 90% were <40 years of age, emphasises a strong need to consider more ergonomic working postures. Work stress was linked to higher workloads, lower job satisfaction, poorer eating and exercise habits, higher work pain and discomfort, lower perceived health and less sleep. Job satisfaction was identified to be the single best predictor of work stress scores. Active stress coping strategies were used by a relatively low proportion of respondents.
Acknowledgement
There was no funding for this study.
Conflicts of interest
The authors declare that they have no conflicts of interest.
References
- 1.McCance KL, Huether SE, Brashers VL, et al. Mosby; St. Louis, MO: 2010. Pathophysiology: The Biologic Basis for Disease in Adults and Children. [Google Scholar]
- 2.Cohen S, Kessler RC, Gordon LU. Oxford University Press; New York, NY: 1995. Measuring Stress: A Guide for Health and Social Scientists. [Google Scholar]
- 3.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 4.Howard JH, Cunningham DA, Rechnitzer PA, et al. Stress in the job and career of a dentist. J Am Dent Assoc. 1976;93:630–636. doi: 10.14219/jada.archive.1976.0194. [DOI] [PubMed] [Google Scholar]
- 5.Gerschman JA, Burrows GD. Stress and distress in dentistry. Stress Med. 1998;14:213–217. [Google Scholar]
- 6.Sancho FM, Ruiz CN. Risk of suicide amongst dentists: myth or reality? Int Dent J. 2010;60:411–418. [PubMed] [Google Scholar]
- 7.Agrawal N, Gupta ND, Bey A, et al. Occupational hazards in modern dentistry: a review. Int J Med Health Res. 2014;1:1–9. [Google Scholar]
- 8.Perez-Padron M, Bernabé E, Gomez-Santos G, et al. Healthy mind and body in a healthy work environment. Int Dent J. 2010;60:395–398. [PubMed] [Google Scholar]
- 9.Roth S, Cohen LJ. Approach, avoidance, and coping with stress. Am Psychol. 1986;41:813–819. doi: 10.1037//0003-066x.41.7.813. [DOI] [PubMed] [Google Scholar]
- 10.Soderstrom M, Dolbier C, Leiferman J, et al. The relationship of hardiness, coping strategies, and perceived stress to symptoms of illness. J Behav Med. 2000;23:311–328. doi: 10.1023/a:1005514310142. [DOI] [PubMed] [Google Scholar]
- 11.Cooper CL, Watts J, Baglioni AJ, et al. Occupational stress amongst general practice dentists. J Occup Psychol. 1988;61:163–174. [Google Scholar]
- 12.Myers HL, Myers LB. ‘It’s difficult being a dentist’: stress and health in the general dental practitioner. Br Dent J. 2004;197:89–93. doi: 10.1038/sj.bdj.4811476. [DOI] [PubMed] [Google Scholar]
- 13.Ayers KM, Thomson WM, Newton JT, et al. Job stressors of New Zealand dentists and their coping strategies. Occup Med (Lond) 2008;58:275–281. doi: 10.1093/occmed/kqn014. [DOI] [PubMed] [Google Scholar]
- 14.Jamjoom HM. Stress among dentists in Jeddah, Saudi Arabia. Saudi Dent J. 2008;20:88–95. [Google Scholar]
- 15.Pouradeli S, Shahravan A, Eskandarizdeh A, et al. Occupational stress and coping behaviours among dentists in Kerman, Iran. Sultan Qaboos Univ Med J. 2016;16:e341–e346. doi: 10.18295/squmj.2016.16.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh P, Aulak DS, Mangat SS, et al. Systematic review: factors contributing to burnout in dentistry. Occup Med (Lond) 2016;66:27–31. doi: 10.1093/occmed/kqv119. [DOI] [PubMed] [Google Scholar]
- 17.Campian RS. Statistics regarding the number of members and dental offices in Cluj County [online]. Romanian College of Dental Medics/Surgeons Cluj; 2011. Available from: http://cmdcluj.ro/date/RAPORT_2010_Site.pdf. Accessed 27 May 2017.
- 18.Kay EJ, Lowe JC. A survey of stress levels, self-perceived health and health-related behaviours of UK dental practitioners in 2005. Br Dent J. 2008;204:622–623. doi: 10.1038/sj.bdj.2008.490. [DOI] [PubMed] [Google Scholar]
- 19.Rogers C, Malone KM. Stress in Irish dentists: developing effective coping strategies. J Ir Dent Assoc. 2009;55:304–307. [PubMed] [Google Scholar]
- 20.Newton JT. Stress in dental practice: a qualitative comparison of dentists working within the NHS and those working within an independent capitation scheme. Br Dent J. 1996;180:329–334. doi: 10.1038/sj.bdj.4809080. [DOI] [PubMed] [Google Scholar]
- 21.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166:1689–1692. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 22.Jepson C, Asch DA, Hershey JC, et al. In a mailed physician survey, questionnaire length had a threshold effect on response rate. J Clin Epidemiol. 2005;58:103–105. doi: 10.1016/j.jclinepi.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 23.O’Shea RM, Corah NL, Ayer WA. Sources of dentists’ stress. J Am Dent Assoc. 1984;109:48–51. doi: 10.14219/jada.archive.1984.0282. [DOI] [PubMed] [Google Scholar]
- 24.Gorter RC, Eijkman MA, Hoogstraten J. Burnout and health among Dutch dentists. Eur J Oral Sci. 2000;108:261–267. doi: 10.1034/j.1600-0722.2000.108004261.x. [DOI] [PubMed] [Google Scholar]
- 25.Alexander RE. Stress-related suicide by dentists and other healthcare workers. Fact or folklore? J Am Dent Assoc. 2001;132:786–794. doi: 10.14219/jada.archive.2001.0278. [DOI] [PubMed] [Google Scholar]
- 26.Bretherton R, Chapman HR, Chipchase S. A study to explore specific stressors and coping strategies in primary dental care practice. Br Dent J. 2016;220:471–478. doi: 10.1038/sj.bdj.2016.334. [DOI] [PubMed] [Google Scholar]
- 27.Van der Klink JJ, Blonk RW, Schene AH, et al. The benefits of interventions for work-related stress. Am J Public Health. 2001;91:270–276. doi: 10.2105/ajph.91.2.270. [DOI] [PMC free article] [PubMed] [Google Scholar]