Abstract
Objectives
Numerous case reports have referred to new onset or flare of SLE after SARS-CoV-2 messenger RNA (mRNA) vaccines. Several observational studies showed that the short-term flare rate of SLE after SARS-CoV-2 vaccination is low. However, well-controlled clinical surveys are unavailable and the medium-term impact of the SARS-CoV-2 mRNA vaccines against the flare of SLE is uncertain. Therefore, we aimed to analyse the association between vaccination and medium-term subjective and objective disease activities of SLE and flares using matched pair methods.
Methods
Altogether, 150 patients with SLE from the Kyoto Lupus Cohort were included. Patients who received two doses of the SARS-CoV-2 mRNA vaccines were 1:1 matched with unvaccinated patients based on the first vaccination date. The outcome measures were the SLE Disease Activity Index-2000 (SLEDAI-2K), the Japanese version of the SLE Symptom Checklist Questionnaire (SSC-J) and the Safety of Estrogens in Lupus Erythematosus National Assessment-SLEDAI flare index at 30, 60 and 90 days after vaccination.
Results
SLEDAI-2K levels were not significantly different in vaccinated and unvaccinated patients with SLE at 30, 60 and 90 days after the second vaccination (adjusted estimate (95% CI): 30 days: −0.46 (−1.48 to 0.56), p=0.39; 60 days: 0.38 (−0.64 to 1.40), p=0.47; 90 days: 0.40 (−0.54 to 1.34), p=0.41). Similar results were observed in the SSC-J score (adjusted estimate (95% CI), 30 days: 0.05 (−1.46 to 1.56), p=0.95; 60 days: −0.63 (−2.08 to 0.82), p=0.40; 90 days: 0.27 (−1.04 to 1.58), p=0.69) and flare index (adjusted OR (95% CI), 30 days: 0.81 (0.36 to 1.85), p=0.62; 60 days: 1.13 (0.50 to 2.54), p=0.77; 90 days: 0.85 (0.32 to 2.26), p=0.74).
Conclusion
SARS-CoV-2 vaccination did not significantly influence the medium-term subjective and objective disease activities or flares of SLE until 90 days after the second vaccination.
Keywords: lupus erythematosus, systemic; vaccination; COVID-19
WHAT IS ALREADY KNOWN ON THIS TOPIC
The flare rate of SLE after SARS-CoV-2 messenger RNA (mRNA) vaccination is reported to be approximately 10%, but the evaluation was mostly based on interviews or questionnaires.
The exact impact on flares is unknown because no studies have included matched SLE patients who were not vaccinated.
There have been reports related to the short-term relapse rate of the SARS-CoV-2 mRNA vaccine, but its medium-term to long-term impact is unknown.
WHAT THIS STUDY ADDS
Using matched pair methods, SARS-CoV-2 mRNA vaccination was found not to influence the medium-term subjective and objective disease activities or flares compared with those of the SARS-CoV-2 mRNA vaccinated and unvaccinated control groups.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The SARS-CoV-2 mRNA vaccine may be safe for patients with SLE with medium-term disease activity and flares.
The results of this study reassure patients with SLE who have not yet received the vaccine.
Introduction
Recently, the frequency of adverse reactions in autoimmune inflammatory rheumatic disease after vaccination has been similar to that in healthy subjects,1–3 and the autoimmune inflammatory rheumatic disease relapse rate is low.1 2 4 However, most of these studies focused on rheumatoid arthritis and did not examine flares in patients with SLE. Regarding the relationship between SLE and the SARS-CoV-2 vaccine, numerous case reports of new-onset or flare after vaccination suggest that vaccination might worsen SLE.5–7 Type I interferonopathy, the primary pathogenesis of SLE, is also triggered by the SARS-CoV-2 vaccination, which causes the onset or flare of SLE.8
A few observational studies have reported that the relapse rate of SLE after vaccination is low.9–11 However, there are several problems, such as the inadequate evaluation of SLE disease activities based on non-validated questionnaires and patient self-reports; the difficulty in distinguishing between adverse reactions and SLE disease activities in a short period after vaccination and the inability to establish a strict control group. Hence, the influence of vaccination on disease activity in patients with SLE is not thoroughly understood.
In the present matched-pair study, we investigated the medium-term impact of vaccination on disease activity in patients with SLE using physicians’ objective assessment of disease activity, laboratory tests and a validated questionnaire.
Methods
Inclusion criteria
All patients with SLE who fulfilled the following inclusion criteria were included in the study:
Patients in the Kyoto Lupus Cohort,12 who visited Kyoto University Hospital and who had a minimum of two visits between 1 January 2021 and 1 December 2021 (considering the vaccination situation in Japan).
Patients with the 1997 American College of Rheumatology13 or the 2012 Systemic Lupus, as well as those who met the International Collaborating Clinics classification criteria.14
Patients whose disease activity was measured.
The sample size was not estimated.
Matching methods
The first vaccination date during two doses of vaccination was defined as the index date. The patients with SLE who had completed their second vaccination were grouped as vaccinated patients. Among patients with SLE, every vaccinated patient was matched to one unvaccinated patient whose disease activities were assessed on the same index date as that with replacement, which consists of selecting one match for each control and returning the matched controls to the pool of observations. Patients who did not match were excluded.
Disease activities
Disease activities were assessed before the first vaccination and after the second vaccination using the SLE Disease Activity Index-2000 (SLEDAI-2K) as an objective parameter15; the Japanese version of the SLE Symptom Checklist Questionnaire (SSC-J) as a subjective parameter and12 physician-visual analogue scale (Ph-VAS), patient-VAS (Pt-VAS) and laboratory data. The flare of SLE was evaluated using the Safety of Estrogens in Lupus Erythematosus National Assessment (SELENA)-SLEDAI flare index.16 Disease activities up to 3 months before the index date were defined as baseline.
Outcomes
Primary outcomes
The primary outcome was SLEDAI-2K scores at 30 days after the second vaccination.
Secondary outcomes
The secondary outcomes were as follows:
SLEDAI-2K scores at 60 and 90 days after the second vaccination.
SSC-J scores at 30, 60 and 90 days after the second vaccination.
SELENA-SLEDAI flare index at 30, 60 and 90 days after the second vaccination.
Ph-VAS and Pt-VAS scores at 30, 60 and 90 days after the second vaccination.
SLEDAI-2K arthritis categories and SSC-J arthralgia at 30 days after the second vaccination.
Serological activities at 30 days after the second vaccination, including white blood cell count (×103/μL), platelet count (×103/μL), C3 (mg/dL), C4 (mg/dL), CH50 (CH50/mL), anti-DNA antibody titre (IU/mL) and urine protein-to-creatinine (P/C) ratio (g/gCre).
SLEDAI-2K and SSC-J scores at 30, 60 and 90 days after the second vaccination in patients with high disease activity (SLEDAI-2K>10).
Missing value
The missing values were adjusted using the simple imputation method to assign the mean of the values preceding and following the missing value.
Statistical analysis
The χ2 and Wilcoxon rank-sum tests were used for categorical and continuous variables, respectively. Linear and logistic mixed-effect models were used to calculate estimates, ORs and 95% CIs. JMP software V.14, R software V.3.4.1 and GraphPad Prism V.9.3.1 were used for analysis or drawing figures. The level of statistical significance was set at p<0.05.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
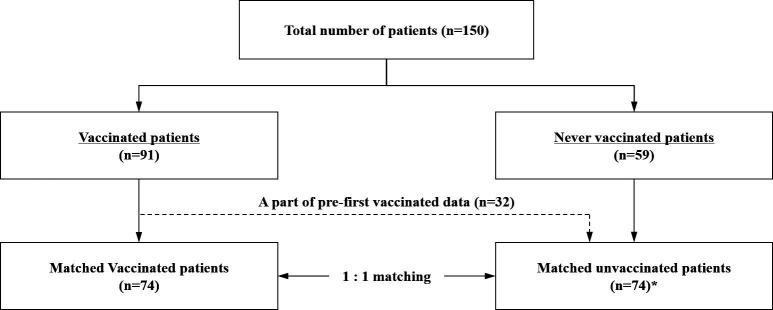
Of the 150 patients who fulfilled the inclusion criteria, 74 vaccinated and 74 unvaccinated patients were selected based on the 1:1 match on the index date. The prefirst vaccination data of 32 patients in the vaccinated group were registered in the unvaccinated group (figure 1).
Figure 1.
Flow chart of patients included in the present study. Altogether, 150 patients with SLE were included. The patients were divided into two groups: the vaccinated group (n=91) and the never-vaccinated group (n=59). The prefirst vaccination data of the 32 patients in the vaccinated group was registered in the unvaccinated group. Then, we selected 74 vaccinated and 74 unvaccinated patients by 1:1 matching with replacement. *‘Matched unvaccinated patients’ referred to 42 never-vaccinated patients and 32 patients in the vaccinated group before their first vaccination.
Table 1 shows the characteristics of the patients in the vaccinated and unvaccinated groups. There were no significant differences in patients’ characteristics, including age, sex, disease duration and medications, between the two groups. The baseline serological disease activity and disease activity scores did not differ. In the vaccinated group, 16 out of 74 (21%) patients had high disease activity (SLEDAI-2K>10).
Table 1.
Patient characteristics of the vaccinated and unvaccinated groups
| Vaccinated | Unvaccinated | P value | |
| Number, n | 74 | 74 | – |
| Female, n (%) | 71 (96) | 73 (99) | 0.62 |
| Age, years, mean (SD) | 50 (14) | 44 (14) | 0.11 |
| Disease duration, years | 19.5 (10.75, 27.5) | 17 (8.75, 25.25) | 0.45 |
| Body mass index | 20.8 (18.8, 22.5) | 19.8 (19.4, 21.98) | 0.65 |
| Complications | |||
| Lupus nephritis, n (%) | 37 (50.0) | 41 (55.4) | 0.62 |
| Antiphospholipid antibody syndrome, n (%) | 7 (9.5) | 3 (4.1) | 0.33 |
| Comorbidity | |||
| Rheumatoid arthritis, n (%) | 6 (8.1) | 4 (5.4) | 0.75 |
| Sjögren’s syndrome, n (%) | 6 (8.1) | 9 (12.2) | 0.59 |
| Mixed connective tissue disease, n (%) | 3 (4.1) | 2 (2.7) | 1.00 |
| Systemic sclerosis, n (%) | 3 (4.1) | 7 (9.5) | 0.33 |
| Treatment | |||
| Glucocorticoid, n (%) | 64 (89.9) | 69 (93.2) | 0.28 |
| Prednisolone dose (mg) | 5 (3, 8) | 6 (4, 8) | 0.19 |
| Hydroxychloroquine, n (%) | 27 (36.5) | 28 (37.8) | 1.00 |
| Immunosuppressant or biologics, n (%) | 52 (70.3) | 54 (73.0) | 0.86 |
| Tacrolimus, n (%) | 26 (35.1) | 30 (40.5) | 0.61 |
| Azathioprine, n (%) | 11 (14.9) | 9 (12.2) | 0.81 |
| Mycophenolate mofetil, n (%) | 10 (13.5) | 15 (20.3) | 0.38 |
| Methotrexate, n (%) | 6 (8.1) | 7 (9.5) | 1.00 |
| Mizoribine, n (%) | 6 (8.1) | 7 (9.5) | 1.00 |
| Ciclosporin A, n (%) | 4 (5.4) | 4 (5.4) | 1.00 |
| Belimumab, n (%) | 9 (12.2) | 14 (18.9) | 0.36 |
| Serological disease activity | |||
| Anti-DNA antibody (IU/mL) | 5 (2.25, 14.5) | 7 (4, 11) | 0.56 |
| C3 (mg/dL) | 82.9 (71.8, 94.3) | 88.9 (71.7, 102.5) | 0.35 |
| CH50 (CH50/mL) | 41 (35, 46.3) | 41 (36, 46.3) | 0.46 |
| Disease activity score | |||
| SLEDAI-2K score | 6 (2, 10) | 6 (4, 12) | 0.60 |
| Disease activity | |||
| None (SLEDAI-2K: 0), n (%) | 14 (18.9) | 6 (8.1) | 0.09 |
| Low (SLEDAI-2K: 1–5), n (%) | 18 (24.3) | 30 (40.5) | 0.053 |
| Moderate (SLEDAI-2K: 6–10), n (%) | 26 (35.1) | 19 (25.7) | 0.28 |
| High (SLEDAI-2K: 11–19), n (%) | 13 (17.6) | 14 (18.9) | 1.00 |
| Very high (SLEDAI-2K: <19), n (%) | 3 (4.1) | 5 (6.8) | 0.72 |
| SSC-J score | 29 (11, 49) | 35 (10, 53) | 0.77 |
| Physician VAS (mm) | 17 (7.5, 33.25) | 20 (9.75, 33) | 0.67 |
| Patient VAS (mm) | 45.5 (22, 59) | 54 (29, 67.5) | 0.06 |
| SARS-CoV-2 vaccination | |||
| BNT162b2 (Pfizer/BioNTech), n (%) | 65 (88) | – | – |
| mRNA-1273 (Moderna), n (%) | 9 (12) | – | – |
| COVID-19 infection | 0 (0.0) | 0 (0.0) | – |
All glucocorticoids were converted to equivalent prednisolone doses. The χ2 and Wilcoxon rank-sum tests were used for categorical and continuous variables, respectively. Continuous variables are expressed as IQRs.
mRNA, messenger RNA; SLEDAI-2K, SLE Disease Activity Index-2000; SSC-J, Japanese version of the SLE Symptom Checklist Questionnaire; VAS, visual analogue scale.
Primary outcome
The quantitative changes in SLEDAI-2K scores from the prefirst vaccination baseline to 30 days after the second vaccination were not significantly different between the vaccinated and unvaccinated groups (ΔSLEDAI-2K (mean±SD): vaccinated vs unvaccinated group (−0.3±4.6) vs (0.2±5.5), p=0.93, respectively) (figure 2A). The slope graph of SLEDAI-2K scores between the two time points was similar (online supplemental figure 1A, B). The linear mixed-effects models showed no significant difference in SLEDAI-2K scores 30 days after the second vaccination between the groups (estimate (95% CI) −0.53 (−1.22 to 0.16), p=0.13) (table 2). A similar result was obtained after adjusting for age, sex, SLEDAI-2K at baseline, and immunosuppressive drug or biological agent use (adjusted estimate (95% CI) −0.46 (−1.48 to 0.56), p=0.39).
Figure 2.
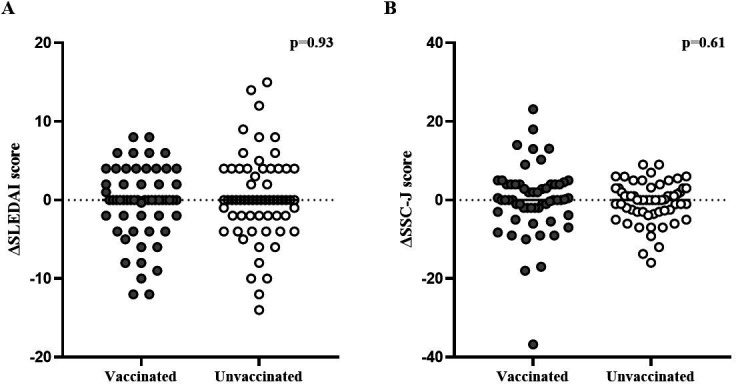
Quantitative change in the SLEDAI-2K and SSC-J scores in the vaccinated and unvaccinated groups at 30 days after the second vaccination. (A) ΔSLEDAI-2K, (B) ΔSSC-J. Analysed by using the Wilcoxon rank-sum test (ΔSLEDAI-2K (mean±SD): vaccinated group vs unvaccinated group, −0.3±4.6 vs 0.2±5.5 (p=0.93); ΔSSC-J (mean±SD): vaccinated group vs unvaccinated group, 0.04±8.85 vs −0.49±5.06 (p=0.61)). SLEDAI-2K, SLE Disease Activity Index-2000; SSC-J, Japanese version of the SLE Symptom Checklist Questionnaire. The value of statistical significance was set at p<0.05.
Table 2.
Estimates in a linear mixed-effects model of vaccination effects for SLEDAI-2K and SSC-J score
| Unadjusted | Adjusted | |||
| Estimate (95% CI) | P value | Estimate (95% CI) | P value | |
| 30 days (15–61 days) | ||||
| SLEDAI-2K | −0.53 (−1.22 to 0.16) | 0.13 | −0.46 (−1.48 to 0.56) | 0.39 |
| SSC-J | 0.21 (−0.32 to 0.74) | 0.75 | 0.05 (−1.46 to 1.56) | 0.95 |
| 60 days (28–120 days) | ||||
| SLEDAI-2K | 0.29 (−0.51 to 1.09) | 0.49 | 0.38 (−0.64 to 1.40) | 0.47 |
| SSC-J | −1.13 (−2.50 to 0.24) | 0.07 | −0.63 (−2.08 to 0.82) | 0.40 |
| 90 days (56–189 days) | ||||
| SLEDAI-2K | 0.48 (−0.44 to 1.40) | 0.31 | 0.40 (−0.54 to 1.34) | 0.41 |
| SSC-J | 0.09 (−1.20 to 1.38) | 0.89 | 0.27 (−1.04 to 1.58) | 0.69 |
Mixed-effects models were used to evaluate SLEDAI-2K and SSC-J scores between the groups at 30 days after the second vaccination. Adjustment variables: age, sex, SLEDAI-2K and SSC-J scores at baseline, and use of immunosuppressive drugs or biological agents. The missing values were adjusted using the simple imputation method to assign the mean of the values preceding and following the missing value ((SSC-J score at 30 days) n=2).
SLEDAI-2K, SLE Disease Activity Index-2000; SSC-J, Japanese version of the SLE Symptom Checklist Questionnaire.
lupus-2022-000727supp001.pdf (580.1KB, pdf)
Secondary outcomes
The linear mixed-effects model showed no significant difference between the vaccinated and unvaccinated groups in the SLEDAI-2K scores at 60 and 90 days after the second vaccination (adjusted estimate (95% CI), 60 days: 0.38 (−0.64 to 1.40), p=0.47; 90 days: 0.40 (−0.54 to 1.34), p=0.41) (table 2).
The change in SSC-J scores from prefirst vaccination baseline to 30 days after the second vaccination was not significantly different between the two groups (ΔSSC-J (mean±SD): vaccinated vs unvaccinated group (0.04±8.85) vs (−0.49±5.06), p=0.61, respectively) (figure 2B). The slope graph of SSC-J scores between the two time points was similar (online supplemental figure 1C, D). The mixed-effects models, adjusted for age, sex, baseline SSC-J score and immunosuppressive drug or biological agent use, did not show significant variation in the SSC-J score after the vaccination (adjusted estimate (95% CI), 30 days: 0.05 (−1.46 to 1.56), p=0.95; 60 days: −0.63 (−2.08 to 0.82), p=0.40; 90 days: 0.27 (−1.04 to 1.58), p=0.69) (table 2).
The rate of SLE flares 30 days after the second vaccination was 20.3% (mild or moderate, 20.3% (n=15/74); severe, 0.0% (n=0/74)) and 23.3% (mild or moderate, 20.3% (n=15/74); severe, 4.1% (n=3/74)) in the vaccinated and unvaccinated groups, respectively. The flare rates at 60 and 90 days are similar in the two groups (online supplemental table 1). The linear mixed-effects model, adjusted for age, sex and immunosuppressive drug or biological agent use, showed no significant association between the vaccination and flares at 30, 60 and 90 days after the second vaccination (adjusted OR (95% CI), 30 days: 0.81 (0.36 to 1.85), p=0.62; 60 days: 1.13 (0.50 to 2.54), p=0.77; 90 days: 0.85 (0.32 to 2.26), p=0.74) (table 3).
Table 3.
Estimated OR and 95% CI for the association between vaccination and flares at 30, 60 and 90 days after the second vaccination
| Unadjusted | Adjusted | |||
| OR (95% CI) | P value | OR (95% CI) | P value | |
| 30 days | 0.85 (0.38 to 1.91) | 0.70 | 0.81 (0.36 to 1.85) | 0.62 |
| 60 days | 1.10 (0.50 to 2.41) | 0.81 | 1.13 (0.50 to 2.54) | 0.77 |
| 90 days | 0.76 (0.29 to 1.97) | 0.57 | 0.85 (0.32 to 2.26) | 0.74 |
Adjustment variables included age, sex and the use of immunosuppressive drugs or biological agents.
The subanalyses showed that the categories of ‘arthritis’ in SLEDAI-2K and ‘arthralgia’, the subjective symptoms evaluated in SSC-J, were not associated with vaccination. The scores at 30 days after the second vaccination were (adjusted OR (95% CI) (arthritis (SLEDAI-2K)): 0.88 (0.20 to 3.85), p=0.87; (arthralgia (SSC-J)): 1.92 (0.70 to 5.29), p=0.20) (online supplemental table 3).
The Ph-VAS scale at 30, 60 and 90 days and Pt-VAS scale at 30 and 60 days were similar in both the groups; however, the Pt-VAS scale at 90 days was significantly lower in the vaccinated group (adjusted estimate (95% CI) −3.43 (−6.49 to −0.37) mm, p=0.03) (online supplemental table 4).
Serological disease activity indices showed no clinically significant differences at 30 days after vaccination; however, platelet count was lower by 1.6×103/μL (95% CI −2.64 to −0.56), p=0.003) and C3 was higher by 1.1 mg/dL (95% CI −0.02 to 2.22, p=0.05) in the vaccinated group compared with that in the unvaccinated group. The other parameters were not significantly different between the two groups (online supplemental table 5).
The linear mixed-effects model adjusting for age, sex, SLEDAI-2K at baseline and immunosuppressive drug or biological agent use, showed no significant differences in SLEDAI-2K or SSC-J scores after the second vaccination between vaccinated and unvaccinated groups in patients with high disease activity (SLEDAI-2K: adjusted estimate (95% CI), 30 days: −0.95 (−3.13 to 1.23), p=0.40; 60 days: 0.50 (−2.32 to 3.32), p=0.73; 90 days: 1.22 (−1.31 to 3.75), p=0.35; SSC-J: adjusted estimate (95% CI), 30 days: 0.74 (−1.63 to 3.11), p=0.55; 60 days: −0.61 (−3.06 to 1.84), p=0.63; 90 days: −0.81 (−4.28 to 2.66), p=0.65).
Discussion
Our study subjectively and objectively evaluated the medium-term influence of SARS-CoV-2 mRNA vaccination on SLE disease activities by comparing the vaccinated group with the unvaccinated group. There were no significant differences between the two groups in subjective or objective disease activities or flares until 90 days after the second vaccination. Previous reports have shown that musculoskeletal symptoms are the most common symptoms of short-term flare after vaccination.10 In the present study, a subanalysis of musculoskeletal symptoms among SLEDAI-2K and SSC-J items, including arthritis and joint pain, showed no significant difference between the vaccinated and unvaccinated groups. In our study, 21% of patients in the vaccinated group had high disease activity before vaccination. However, there was no significant difference in disease activity at 30, 60 and 90 days after the second vaccination between vaccinated and unvaccinated patients. In general, disease activity in autoimmune inflammatory rheumatic diseases prior to vaccination should be controlled. The results of this study, in which prevaccination disease activity did not affect postvaccination disease activity, suggest that vaccination may be acceptable in urgent cases such as COVID-19, regardless of prevaccination disease activity. However, caution is needed for interpretation because the sample size was small.
Regarding the SARS-CoV-2 vaccine, data are adequate regarding its usefulness to policymakers, clinicians and patients in preventing infection, but not adequate regarding its side effects. Despite the benefits of the SARS-CoV-2 vaccinations, 28.2% of patients with SLE tend to hesitate in receiving them,17 the primary reason being a flare of SLE due to vaccination (56%).18 Our results will help alleviate patient concerns.
Previous studies showed 3%–10.6% short-term flare rates after vaccination within 7 days.9–11 However, the assessments of disease activities were based on interviews or questionnaires, and the evaluation periods were short—not enough to distinguish SLE flares from reactions to vaccines. One study reported that the flare rate evaluated using SLEDAI was 11.4%.19 However, the observation period was short (an average of 23.6 days) and did not establish appropriate controls. Our study has several strengths. First, we used the SLEDAI-2K as an objective measure and the SSC-J score as a validated subjective measure. Second, we compared vaccinated and unvaccinated patients with SLE. Unlike the adverse reactions to vaccines, it is crucial to compare the two groups to assess the effect of vaccines on disease activity. Third, the vaccinated and unvaccinated patients were matched on the first vaccination date. Thus, more precise assessments of the changes in disease activity can be obtained. Finally, we evaluated disease activity in the present study for up to 3 months after the second vaccination.
Our study had several limitations. First, data were unavailable for all patients, as in previous studies. Second, the Kyoto Lupus Cohort contained many patients who had already received the vaccine. Therefore, we included prevaccination data of vaccinated patients in the unvaccinated group. Furthermore, the observation period was limited to 3 months. Since booster vaccination has already been started in Japan, further extended observation periods are challenging.
In this study, the prescription rate of hydroxychloroquine (HCQ) was 37 %, which is less frequent than that in the USA and Europe, and this might have influenced SLE disease activity. There are two reasons for the low prescription rate of HCQ in Japan. First, HCQ was approved by the Ministry of Health, Labour and Welfare in Japan only recently, in 2015. Second, HCQ exerts a higher risk of retinopathy, a side effect of HCQ, in Asians, including the Japanese.20
In conclusion, we observed that medium-term disease activities or flares of SLE did not worsen with the SARS-CoV-2 vaccination, which supports its use in patients with SLE. Further studies are needed to evaluate the long-term impact of vaccines over several years.
Footnotes
Contributors: The study was designed, directed and coordinated by TY, the principal investigator. HT and AO are the co-investigators and in charge of the study conducted at all stages. All the coauthors recruited participants into the study and evaluated patients’ prevaccination and postvaccination activity measures. TY, HT and AO wrote the article, which was critically reviewed by all coauthors. TY, HT, and AO are authors responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by the Ethics Committee of Kyoto University Graduate School and Faculty of Medicine (R145). Written informed consent was obtained from all the patients.
References
- 1.Furer V, Eviatar T, Zisman D, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis 2021;80:1330–8. 10.1136/annrheumdis-2021-220647 [DOI] [PubMed] [Google Scholar]
- 2.Geisen UM, Berner DK, Tran F, et al. Immunogenicity and safety of anti-SARS-CoV-2 mRNA vaccines in patients with chronic inflammatory conditions and immunosuppressive therapy in a monocentric cohort. Ann Rheum Dis 2021;80:1306–11. 10.1136/annrheumdis-2021-220272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Simon D, Tascilar K, Fagni F, et al. SARS-CoV-2 vaccination responses in untreated, conventionally treated and anticytokine-treated patients with immune-mediated inflammatory diseases. Ann Rheum Dis 2021;80:1312–6. 10.1136/annrheumdis-2021-220461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connolly CM, Ruddy JA, Boyarsky BJ, et al. Disease flare and Reactogenicity in patients with rheumatic and musculoskeletal diseases following two-dose SARS-CoV-2 messenger RNA vaccination. Arthritis Rheumatol 2022;74:28–32. 10.1002/art.41924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tuschen K, Bräsen JH, Schmitz J, et al. Relapse of class V lupus nephritis after vaccination with COVID-19 mRNA vaccine. Kidney Int 2021;100:941–4. 10.1016/j.kint.2021.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zavala-Miranda MF, González-Ibarra SG, Pérez-Arias AA, et al. New-Onset systemic lupus erythematosus beginning as class V lupus nephritis after COVID-19 vaccination. Kidney Int 2021;100:1340–1. 10.1016/j.kint.2021.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nune A, Iyengar KP, Ish P, et al. The emergence of new-onset SLE following SARS-CoV-2 vaccination. QJM 2021;114:739–40. 10.1093/qjmed/hcab229 [DOI] [PubMed] [Google Scholar]
- 8.Teijaro JR, Farber DL. COVID-19 vaccines: modes of immune activation and future challenges. Nat Rev Immunol 2021;21:195–7. 10.1038/s41577-021-00526-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Felten R, Kawka L, Dubois M, et al. Tolerance of COVID-19 vaccination in patients with systemic lupus erythematosus: the International VACOLUP study. Lancet Rheumatol 2021;3:e613–5. 10.1016/S2665-9913(21)00221-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barbhaiya M, Levine JM, Bykerk VP, et al. Systemic rheumatic disease flares after SARS-CoV-2 vaccination among rheumatology outpatients in New York City. Ann Rheum Dis 2021;80:1352–4. 10.1136/annrheumdis-2021-220732 [DOI] [PubMed] [Google Scholar]
- 11.Fan Y, Geng Y, Wang Y, et al. Safety and disease flare of autoimmune inflammatory rheumatic diseases: a large real-world survey on inactivated COVID-19 vaccines. Ann Rheum Dis 2022;81:443–5. 10.1136/annrheumdis-2021-221736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doi H, Ohmura K, Tabuchi Y, et al. Validation and verification of the Japanese version of the systemic lupus erythematosus symptom checklist for patient quality of life. Lupus 2021;30:1108–15. 10.1177/09612033211005026 [DOI] [PubMed] [Google Scholar]
- 13.Hochberg MC. Updating the American College of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997;40:40. 10.1002/art.1780400928 [DOI] [PubMed] [Google Scholar]
- 14.Petri M, Orbai A-M, Alarcón GS, et al. Derivation and validation of the systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 2012;64:2677–86. 10.1002/art.34473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol 2002;29:288–91. [PubMed] [Google Scholar]
- 16.Petri M, Kim MY, Kalunian KC, et al. Combined oral contraceptives in women with systemic lupus erythematosus. N Engl J Med 2005;353:2550–8. 10.1056/NEJMoa051135 [DOI] [PubMed] [Google Scholar]
- 17.Felten R, Dubois M, Ugarte-Gil MF, et al. Vaccination against COVID-19: expectations and concerns of patients with autoimmune and rheumatic diseases. Lancet Rheumatol 2021;3:e243–5. 10.1016/S2665-9913(21)00039-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ramirez GA, Argolini LM, Bellocchi C, et al. Impact of the COVID-19 pandemic in patients with systemic lupus erythematosus throughout one year. Clin Immunol 2021;231:108845. 10.1016/j.clim.2021.108845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Izmirly PM, Kim MY, Samanovic M, et al. Evaluation of immune response and disease status in systemic lupus erythematosus patients following SARS-CoV-2 vaccination. Arthritis Rheumatol 2022;74:284–94. 10.1002/art.41937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melles RB, Marmor MF. Pericentral retinopathy and racial differences in hydroxychloroquine toxicity. Ophthalmology 2015;122:110–6. 10.1016/j.ophtha.2014.07.018 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
lupus-2022-000727supp001.pdf (580.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.