Abstract
Objectives: The aim of this study was to characterise the daily oral hygiene behaviours and the frequency of, and reasons for, oral health appointments, among 12-year-old adolescents in Portugal. We also investigated whether there were any associations between these behaviours and sociodemographic factors. Methods: We conducted an observational descriptive study based on 1,309 Portuguese adolescents from rural, peri-urban and urban populations. Data were drawn from the III National Prevalence Study of Oral Health Diseases. After descriptive analyses, binary logistic regression models were used. Results: In this study, 70.6% (n = 924) of adolescents reported that they brushed ‘twice a day or more’, and this behaviour was associated with all sociodemographic variables. Multivariate analysis revealed that male gender [odds ratio (OR) = 2.124; 95% confidence interval (95% CI): 1.616–2.793], rural residence (OR = 1.647; 95% CI: 1.169–2.321), peri-urban residence (OR = 1.926; 95% CI: 1.319–2.812), low level of maternal educational (OR = 2.139; 95% CI: 1.446–3.164) and father’s unemployment (OR = 1.671; 95% CI: 1.127–2.478) were associated with not brushing at least twice a day (P < 0.05). Approximately 94% (n = 1,217) of participants had already visited an oral health professional, and 74.5% (n = 860) did so in the last 12 months. Conclusion: Our results are in agreement with the literature; the oral health behaviours of 12-year-old Portuguese adolescents can be regarded as satisfactory, although there are important variations across different subpopulations. The influence of sociodemographic factors suggests that tailored strategies must be developed for specific subpopulations, at both individual and community levels.
Key words: Oral health, toothbrushing, health service accessibility, socio-economic factors, sociodemographic factors
Introduction
Oral health is part of the overall health and well-being of children1. Poor oral health affects quality of life as a result of pain or discomfort, tooth loss, implied oral functioning, missing time at school, loss of work hours and death (in the case of oral cancer)2. Detal caries (tooth decay) and periodontal disease are the two most common diseases in oral health; they share the same aetiological factor, dental plaque, but can also be influenced by specific internal and external predispositions3., 4.. When compared with other groups of diseases, oral health problems can be prevented, generally with good results5. Brushing daily, use of fluoride products, drinking fluoridated water and visiting a dental professional regularly are perhaps the most effective methods for reducing the prevalence of dental caries in children6., 7., 8., 9., 10..
Proper oral hygiene measures, correctly used in conjunction with regular professional care, potentially prevent caries and periodontal disease and help to maintain oral health11., 12.. Specifically, for 12-year-old children, it is recommended that visiting an oral health professional at least once per year is the best way to maintain good oral health13. Additionally, brushing at least twice a day is the best behaviour to achieve good oral health and oral hygiene5., 11., 14. and is recommended by professional dental associations15. The benefits of fluoride toothpaste for preventing caries in children and adolescents, when compared with placebo, are proven; a fluoride concentration of ≥1,000 ppm is recommended for children, while 1,500 ppm is recommended for adolescents16., 17., 18., 19.. It is known that oral health problems are associated with lower sociodemographic status, highlighting the influence of social determinants of health on the oral health of populations5. In the epidemiological oral health field, gender, social class, education level, income and employment are the strongest determinants of oral health outcomes20. The incidence of dental decay has been shown to be higher in children with a low sociodemographic status12. A study in Brazil found that visiting an oral health professional and brushing twice a day was less frequent among children with low sociodemographic status, and among those without family support, reinforcing the fact that social determinants influence oral health outcomes21.
In this context, this study aims to characterise oral health appointments (frequency and reasons) and daily hygiene behaviours (mainly toothbrushing but also the use of fluoride products, mouthrinses and dental floss) in 12-year-old Portuguese adolescents. This study will also investigate the associations between these behaviours and sociodemographic factors.
Methods
This article was written according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. An observational analytic study was developed based on data from the III National Prevalence Study of Oral Health Diseases (III ENPDO), by the General Directorate of Health – Portugal (DGS). III ENPDO is a cross-sectional national survey carried out between 2012 and 2013, and was conducted in full accordance with the World Medical Association Declaration of Helsinki and approved by the Ethics Committee of DGS. Written consent was obtained from the parents/guardians of all participants (12-year-old adolescents) in this study.
Our study was specifically focussed on 12-year-old adolescents who were studying in public or private schools, and who were residents of Portugal (inclusion criteria). Adolescents with some types of disabilities were automatically excluded from the study. The III ENPDO sample size for this specific age (n = 1,309) was computed based on the number of adolescents in one health region and based on the prevalence of caries (56%) found in the last national study7. The sample has a regional accuracy of 7%, ensuring a national accuracy estimate of 2.5%. This aspect (region accuracy) will be considered in statistical models. After random selection of schools, the classes were randomly selected from those in which at least 80% of students were born in 2000 or 2001. Within each class, all the students were considered. Between October 2012 and June 2013, data were collected from students of 73 private and public schools, after obtaining permission from the legal guardians. Data were collected by dentists teaching at dental schools in Portugal and by members of the Portuguese Dentists Association (OMD), assisted by dental hygienists working in the Portuguese National Health Service. A questionnaire was conducted via interview. The interviews included questions from the National Health Survey, the II National Prevalence Study of Oral Health Diseases, Eurobarometer Special Edition 330 – Report Oral Health February 2010 and the European Global Oral Health-Indicators Development Program (Health Surveillance in Europe – Oral Health Interviews Clinical Surveys: Guidelines). The interviewers had a guide document and previous training.
This questionnaire covered several dimensions, such as sociodemographic characteristics, oral hygiene behaviours and frequency and reasons for attendance at a dental appointment. The III ENPDO study defined sociodemographic profile using gender (male/female), type of local of residency (urban/peri-urban/rural), health region (North, Centre, Lisbon, Alentejo, Algarve, the Azores, RA Madeira), father’s and mother’s employment status (worker/unemployed/other) and parent’s education (less than high school/high school/college degree). Regarding the frequency and reasons for a dental appointment, participants reported if they had been to a dental appointment ever, when was the last dental appointment, how many times they had an appointment in the past 12 months and the reason for the last appointment (routine/fillings/tooth extraction/other). For the oral hygiene behaviours, variables included daily frequency of toothbrushing, use of fluoride toothpaste, frequency of daily flossing and use of other fluoride products (such as pills or mouthrinses).
In agreement with the literature, and based on the data collected, the major variables were computed. For toothbrushing and oral health appointment frequencies, several variables were computed. The variable ‘When was the last dental appointment’ was categorised into ‘potentially adequate’ (the last appointment was in the last 12 months) and ‘potentially inadequate’ (the last appointment was prior to the last 12 months). The variable ‘How many times do you brush your teeth per day?’ was categorised into ‘potentially adequate’ (‘brushing twice or more per day’) and ‘potentially inadequate’ (‘brushing once or less per day’).
After descriptive analyses, correlations were analysed: the chi-square test was used for categorical data and Fisher’s exact test was used for quantitative data (if assumptions were met). In some cases, low category frequencies were observed; however, it was decided not to aggregate categories because the results lose interpretability (in such cases, the corresponding results are flagged with P* and they must only be seen as exploratory results) and should be tested in future studies with higher frequencies.
The influence of the sociodemographic variables on both the presence of inappropriate toothbrushing frequency and on not visiting the dentist in the last 12 months were assessed using binary logistic regressions, based on the Enter method (using all selected variables). Crude and adjusted (for sex, if statistically significant) odds ratios (ORs) and respective confidence intervals (CIs) are presented.
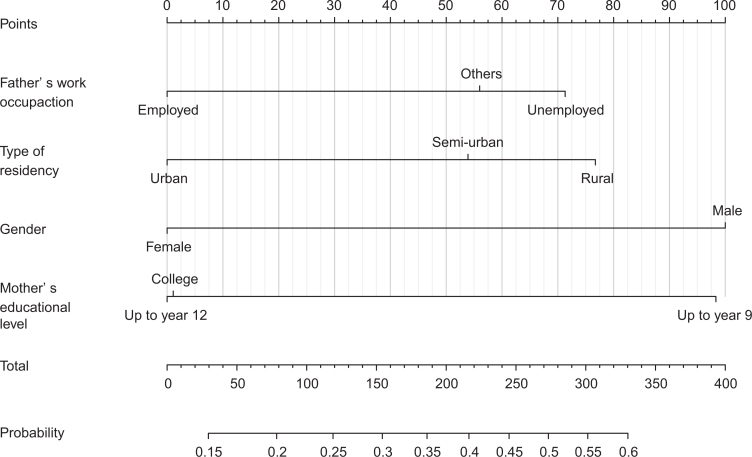
A final multivariate model was developed, using the forward likelihood method, and its validity, quality of fit and predictive capacity were assessed using the Hosmer–Lemeshow test, the Nagelkerke correlation coefficient, the area under the receiver operating curve (ROC), and specificity and sensitivity. The variable reflecting health region was incorporated to consider the effect of the sampling design. This final model was also presented through a nomogram, a very user-friendly and intuitive tool that can be widely used to identify potential cases22. The nomogram is a graphical approach, based on a set of scales, one for each variable in the model. The score for each variable is obtained by drawing a straight edge across the known values on the scales, and the sum of scores is linked with the correspondent probability. In order to clarify its application, an example is presented in Figure 1.
Figure 1.
Nomogram for inadequate brushing (less than twice a day).
For the statistical analyses we used R and SPSS software (v.20.9; SPSS Inc., Chicago, IL, USA) and adopted a statistical significance level of 5%.
Results
This study was based on a sample of 1,309 students (from the III ENPDO study) who were 12 years of age; 45.4% (n = 594) were male and the majority 51.6% (n = 676) lived in urban areas. Regarding mother’s educational level, 47.8% (n = 555) had less than high school, 33% (n = 383) had graduated from high school and 19.2% (n = 224) had a college degree. Of the mothers, 74.5% (n = 968) were working, 9.2% (n = 119) were housewives and 14.9% (n = 193) were unemployed (Table 1). Regarding father’s educational level, 58.2% (n = 644) had less than high school, 26.3% (n = 291) had graduated from high school and 15.5% (n = 172) had a college degree. Of the fathers, 12% (n = 153) were unemployed and 84.8% (n = 1,077) were working.
Table 1.
Descriptive statistics of the sociodemographic variables analysed in this study
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Gender (n = 1,309) | ||
| Male | 594 | 45.4 |
| Female | 715 | 54.6 |
| Health region (n = 1,309) | ||
| North | 192 | 14.7 |
| Centre | 192 | 14.7 |
| Lisbon | 192 | 14.7 |
| Alentejo | 184 | 14.1 |
| Algarve | 184 | 14.1 |
| Azores | 183 | 13.9 |
| Madeira | 182 | 13.8 |
| Type of residency (n = 1,309) | ||
| Rural area | 262 | 20.0 |
| Peri-urban area | 371 | 28.4 |
| Urban area | 676 | 51.6 |
| Mother’s educational level (n = 1,162) | ||
| Less than high school | 555 | 47.8 |
| High school | 383 | 33.0 |
| College degree | 224 | 19.2 |
| Father’s educational level (n = 1,107) | ||
| Less than high school | 644 | 58.2 |
| High school | 291 | 26.3 |
| College degree | 172 | 15.5 |
| Mother’s employment status (n = 1,299) | ||
| Worker | 968 | 74.5 |
| Unemployed | 193 | 14.9 |
| Domestic | 119 | 9.2 |
| Other | 19 | 1.4 |
| Father’s employment status (n = 1,271) | ||
| Worker | 1,077 | 84.8 |
| Unemployed | 153 | 12.0 |
| Other | 41 | 3.2 |
| Have you ever gone to an oral health appointment? (n = 1,292) | ||
| Yes | 1,217 | 94.2 |
| No | 75 | 5.8 |
| When was the last time that you went to a dental appointment? (n = 1,155) | ||
| Less than 1 year | 860 | 74.5 |
| More than 1 year and less than 2 years | 212 | 18.4 |
| More than 2 years and less than 5 years | 74 | 6.4 |
| More than 5 years | 9 | 0.7 |
| Frequency of toothbrushing (n = 1,309) | ||
| 1 or less times per week | 37 | 2.7 |
| 1 or more times per week | 87 | 6.6 |
| 1 time per day | 261 | 19.9 |
| 2 or more times per day | 924 | 70.6 |
| Use of fluoride toothpaste (n = 929) | ||
| Yes | 890 | 95.8 |
| No | 39 | 4.2 |
| Use more types of fluoride products (n = 1,233) | ||
| Pills and mouthrinse | 1 | 0.1 |
| Mouthrinse | 390 | 31.6 |
| Others | 5 | 0.4 |
| No | 837 | 67.9 |
| Use of dental floss (n = 1,300) | ||
| 1 or more times a day | 71 | 5.5 |
| Sometimes weekly | 182 | 14.0 |
| Sometimes monthly | 154 | 11.8 |
| Never | 893 | 68.7 |
The majority of participants (94.2%; 1,217) had attended a dental appointment at least once, with 74.5% (860/1,155, considering the existence of 62 missing values) reporting that they attended a dental appointment in the past 12 months. In this study, 18.4% (n = 212) of participants reported that their last visit to a dental professional was 1–2 years ago, 6.4% (n = 74) reported that their last visit was 2–5 years ago and 0.7% (n = 9) reported that their last dental appointment was more than 5 years ago.
Table 2 shows frequencies of visits to an oral health professional (number of participants = 1,155), considering more or less than 12 months as a cut-off.
Table 2.
Frequency of visits to an oral health professional in the last 12 months and crude odds ratio (OR) for don’t visit an oral health professional in the last 12 months
| Variable | % Last dental appointment more than 12 months | % Last dental appointment in last 12 months | Crude OR |
|---|---|---|---|
| Gender | |||
| Male | 141 (26.8) | 385 (73.2) | 1.130 (0.867–1.472) |
| Female* | 154 (24.5) | 475 (75.5) | |
| Health region | |||
| Lisbon* | 38 (20.9) | 144 (79.1) | |
| North | 38 (21.9) | 136 (78.2) | 0.704 (0.432–1.146) |
| Centre | 48 (27.3) | 128 (72.7) | 0.745 (0.457–1.215) |
| Alentejo | 35 (21.3) | 129 (78.7) | 0.724 (0.439–1.192) |
| Algarve | 37 (20.7) | 142 (79.3) | 0.695 (0.425–1.135) |
| Azores | 54 (43.2) | 71 (56.8) | 2.028 (1.249–3.294) |
| Madeira | 45 (29.0) | 110 (71) | 1.091 (0.675–1.763) |
| Type of residency | |||
| Rural area | 76 (32.5) | 158 (67.5) | 1.601 (1.148–2.233) |
| Peri-urban area | 79 (25.1) | 236 (74.9) | 1.114 (0.811–1.530) |
| Urban area* | 140 (23.1) | 466 (79.6) | |
| Mother’s educational level | |||
| Less than high school | 138 (29) | 338 (71) | 1.837 (1.227–2.750) |
| High school | 84 (23.4) | 275 (76.6) | 1.375 (0.896–2.109) |
| College degree* | 38 (18.2) | 171 (81.1) | |
| Father’s educational level | |||
| Less than high school | 160 (28.6) | 400 (71.4) | 1.733 (1.119–2.684) |
| High school | 60 (21.8) | 215 (78.2) | 1.209 (0.741–1.973) |
| College degree* | 30 (18.8) | 130 (81.3) | |
| Mother’s employment status | |||
| Worker* | 200 (23) | 668 (71) | |
| Unemployed | 40 (23.7) | 129 (76.3) | 1.036 (0.720–1.527) |
| Domestic | 42 (45.2) | 51 (54.8) | 2.751 (1.775–4.262) |
| Other | 9 (51.9) | 8 (47.1) | 3.757 (1.431–9.866) |
| Father’s employment status | |||
| Worker* | 239 (24.5) | 735 (75.5) | |
| Unemployed | 24 (28.1) | 87 (71.9) | 1.202 (0.788–1.834) |
| Other | 12 (36.4) | 21 (36.4) | 1.757 (0.852–3.625) |
*Reference class.
Statistical significant results are highlighted in bold.
Participants who lived in predominantly rural areas reported fewer visits to an oral health professional than those who lived in urban areas (OR = 1.601). Adolescents with parents with who had not completed high school were found to have a higher risk of not attending a dental appointment in the last 12 months compared with adolescents who had a father (OR = 1.733) or mother (OR = 1.873) with a college degree.
The major reasons cited for attendance at a dental appointment were routine check-ups (39.2%; n = 513), fillings (28.9%; n = 378) and tooth extraction (13.5%; n = 177) (each participant was allowed to choose more than one reason, and a total of 1,310 reasons were identified). Parents’ employment, mothers’ education and health region were significantly associated with attending a dental appointment in the last 12 months (P < 0.05). Attending an appointment with an oral health professional in the last 12 months was not statistically associated with any other variables, neither in the adjusted models nor in the final model.
In our sample, 70.6% (n = 924) of adolescents brushed their teeth twice a day or more, while 19.0% (n = 261) reported that they brushed only once a day. A fluoride toothpaste was used by 95.8% (n = 890) of the participants. Use of a mouthrinse with fluoride was reported by 31.6% (n = 390) participants. Only 5.5% (n = 71) participants reported that they flossed daily; 68.7% (n = 893) did not floss at all (Table 1). Table 3 presents the frequency of toothbrushing and the crude, adjusted and final-model ORs for brushing once or less a day relative to the sociodemographic variables.
Table 3.
Frequency of brushing, and crude, adjusted and final model odds ratios (ORs) for brushing once a day or less
| Variable | % Brushing less than twice a day | % Brushing at least twice a day | Crude OR | Adjusted OR* | Final Model OR (Forward LR) |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 217 (36.5) | 377 (63.5) | 1.874 (1.474–2.383) | 2.124 (1.616–2.793) | |
| Female† | 168 (23.5) | 547 (76.5) | |||
| Health region | |||||
| Lisbon† | 61 (32.8) | 131 (68.4) | |||
| North | 56 (29.2) | 136 (70.8) | 1.050 (0.682–1.616) | 1.044 (0.674–1.615) | 0.931 (0.564–1.536) |
| Centre | 59 (30.7) | 133 (69.3) | 0.928 (0.600–1.437) | 0.936 (0.602–1.457) | 0.750 (0.445–1.265) |
| Alentejo | 54 (29.3) | 130 (70.7) | 0.936 (0.602–1.456) | 0.888 (0.568–1.388) | 0.668 (0.386–1.158) |
| Algarve | 41 (22.3) | 143 (77.7) | 0.646 (0.407–1.027) | 0.606 (0.379–0.968) | 0.634 (0.369–1.090) |
| Azores | 52 (28.4) | 131 (71.6) | 0.895 (0.574–1.395) | 0.828 (0.528–1.299) | 0.497 (0.287–0.861) |
| Madeira | 62 (34.1) | 120 (65.9) | 1.165 (0.755–1.797) | 1.143 (0.737–1.772) | 0.787 (0.465–1.332) |
| Type of residency | |||||
| Rural area | 99 (37.8) | 163 (62.2) | 1.896 (1.397–2.574) | 1.953 (1.434–2.661) | 1.647 (1.169–2.321) |
| Peri-urban area | 122 (32.9) | 249 (67.1) | 1.530 (1.155–2.022) | 1.518 (1.145–2.012) | 1.926 (1.319–2.812) |
| Urban area† | 164 (24.3) | 512 (75.7) | |||
| Mother’s educational level | |||||
| Less than high school | 206 (37.1) | 349 (62.9) | 2.284 (1.582–3.297) | 2.395 (1.615–3.474) | 2.139 (1.7446–3.164) |
| High school | 81 (21.1) | 302 (78.9) | 1.038 (0.691–1.558) | 1.054 (0.699–1.590) | 1.032 (0.677–1.575) |
| College degree† | 46 (20.5) | 178 (79.5) | |||
| Father’s educational level | |||||
| Less than high school | 223 (34.6) | 421 (65.4) | 2.724 (1.761–4.213) | 2.795 (1.800–4.314) | |
| High school | 63 (21.6) | 228 (78.4) | 1.421 (0.869–2.323) | 1.391 (0.847–2.284) | |
| College degree† | 28 (16.3) | 144 (83.7) | |||
| Mother’s employment status | |||||
| Worker† | 264 (27.3) | 704 (72.7) | |||
| Unemployed | 68 (35.2) | 125 (64.8) | 1.451 (1.046–2.013) | 1.462 (1.050–2.037) | |
| Domestic | 45 (37.8) | 74 (62.2) | 1.622 (1.091–2.411) | 1.650 (1.105–2.466) | |
| Other | 3 (15.8) | 16 (84.2) | 0.500 (0.145–1.730) | 0.488 (0.140–1.704) | |
| Father’s employment status | |||||
| Worker† | 285 (26.6) | 792 (73.5) | |||
| Unemployed | 66 (43.1) | 87 (56.9) | 2.108 (1.489–2.984) | 2.194 (1.542–3.121) | 1.671 (1.127–2.478) |
| Others | 17 (41.5) | 24 (58.5) | 1.968 (1.042–3.718) | 2.102 (1.103–4.006) | 1.520 (0.689–3.350) |
*Adjusted by gender; †Reference class; LR - Likelihood ratio.
Statistical significant results are highlighted in bold.
Education level of the parents had a direct effect on the frequency of daily toothbrushing and flossing (P < 0.05). Furthermore, all the sociodemographic variables were significantly associated with the frequency of toothbrushing (P < 0.05). Boys had worse oral habits (brushing less than twice a day) compared with girls (OR = 1.874). Those who lived in rural areas were more likely to brush less than twice a day compared with those who lived in urban areas (OR = 1.896). Adolescents with parents who had not completed high school had a higher risk of inadequate toothbrushing compared with adolescents whose parents had a college degree (OR = 2.284 for mothers and OR = 2.724 for fathers). Parents’ employment status was also related to toothbrushing; having a mother (OR = 1.451) or father (OR = 2.108) who is unemployed was associated with a lower frequency of toothbrushing than having parents who are working. After adjusting the ORs for gender, some differences remained, as shown in Table 3. As expected, region was not statistically significant but was included to control for the sampling design characteristics.
In the final model, gender, type of residency area, mother’s education and father’s employment status were significantly associated with brushing less than twice a day. This model was considered mathematically valid but with a relatively weak predictive capacity (Hosmer–Lemeshow = 0.832 and Nagelkerke R Square = 0.109). The area under the ROC curve was 0.675 (95% CI = 0.641–0.710) with a specificity and sensitivity of 64% (cut-off = 0.277).
Figure 1 shows the nomogram corresponding to the final model, highlighting the characteristics most associated with inadequate toothbrushing, namely gender, type of residency area, mother’s education and father’s employment status.
To exemplify how a nomogram can be used as a user-friendly tool for detecting cases of inadequate toothbrushing, a specific case can be illustrative. For example, an adolescent who has an unemployed father (68 points – identified with a straight vertical line drawn from the horizontal line of the ‘father’s employment status’ toward the horizontal line of the ‘score’), is male (99 points – similar base using ‘gender’ line), living in the Azores (0 points), in an urban area (0 points) and has a mother who did not complete high school (100 points) has a total score of 267 (sum of scores – ‘total points’). This value corresponds to a 40% probability of toothbrushing less than twice a day, as identified by drawing a straight vertical axis from ‘total points’ towards the line ‘probability’. Finally, using the cut-off value of 0.26 (parameterised in the model), this adolescent would be identified as a possible case of inadequate toothbrushing.
This intuitive representation depicts the weight of variables (segment lengths) in inadequate toothbrushing and identifies the categories that promote the event (corresponding to higher points), and vice versa (= 0 points).
Discussion
Adolescence is a period of adopting new practices, values, attitudes and behaviours, along with increased autonomy, which allows adolescents to take part in several situations that might be risky and that can affect general and oral health. Additionally, it is a stage when teens do not always appreciate help from adults, in spite of the strong influence of the family in oral health issues23., 24..
Of the 1,309 participants in this study, we found that 94.2% (n = 1,217) had attended a dental appointment at least once in their life, with 74.5% (860/1,155, considering 62 missing values) reporting attendance in the last 12 months. This value is lower than reported in the previous national survey of oral health7, which found that 85% of participants had attended a dental appointment in the last 12 months. This decrease can potentially be explained by the economic and social crisis that has taken place in Portugal in the last few years. The Spanish national health survey found that 62.5% of children 10–12 years of age attended an oral health appointment in the last 12 months25. In another study, the same authors found that 88.2% of children 6–12 years of age attended an oral health appointment in the last 12 months26.
Seeing an oral health professional regularly is a preventive strategy; one study showed that children, 9–12 years of age, who did not go to an oral professional at least once in the previous 12 months were 1.6 times more likely to have oral health problems compared with those who did attend an appointment with an oral health professional 27. In the present study, when focussing on participants to identify the last time that they went to a dental appointment (n = 1,155), we found that 18.4% (n = 212) had their last visit to an oral health professional 1–2 years prior to the start of the study, 6.4% (n = 74) saw an oral health professional 2–5 years prior to the start of the study and 0.7% (n = 9) saw an oral health professional more than 5 years ago. In Poland, 71% of participants, 6–12 years of age, had seen a dentist in the last 12 months, 20% between 1 and 2 years ago, 3% more than 2 years ago and 8% had never visited a dentist28. In our study we found a lower percentage of participants who had not seen an oral health professional (5.8%; n = 75), when compared with countries such as Brazil, considering students with similar ages (year 7, 15.2%29). In the current study, male gender was associated with a higher risk of not regularly attending dental appointments, compared with female gender (OR = 1.130). However, this finding was not statistically significant (P > 0.05). In our study, 75.5% (n = 475) of girls reported visiting an oral health professional in the last 12 months, compared with 73.2% (n = 385) of boys; this tendency has been observed in other studies29. In our study, similar findings were also observed regarding frequency of toothbrushing. In terms of location of residency, participants who lived in rural areas had a higher risk (OR = 1.601) of not visiting an oral health professional compared with those who lived in urban areas. In most European countries, geographical proximity to dental clinics is one of the determinants for attending a dental appointment30.
It has been shown that children whose parents have a higher level of education see an oral health professional at least a year31, which indicates that parent’s health literacy is a protective factor for children’s health32. In our study we found that children with a mother (OR = 1.837) or father (OR = 1.733) who had not completed high school had a higher probability of not seeing an oral health professional at least once a year compared with those children whose parents had a college degree. We also found that the major reason for visiting oral health professionals was for ‘preventive reasons’ 39.2% (n = 513), and this was associated with all the demographic variables in the study, except for mother’s education level. The other reasons reported for visiting an oral health professional included ‘fillings and treatment’ 28.9% (n = 378) and ‘tooth extraction’ 13.5% (n = 177). In 2005, the reasons for going to an oral health professional were the same, but more participants reported seeing an oral health professional for ‘preventive reasons’ (56%)7.
Regarding oral hygiene habits, 70.6% (n = 924) of participants reported that they brush ‘two or more times a day’; this is a higher percentage than that of the last national study, in which 67% of participants reported that they brush at least twice a day7. The Health Behaviour in School-Aged Children survey (2010), among the Portuguese population (n = 5,012), reported that 67.4% of children brushed their teeth one or more times a day; among students in the sixth grade (i.e. 12 years old), this was 62.6%, with girls claiming to brush more often than boys (74.3% vs. 59.7%)33. Our study showed that girls brush twice a day more often than boys (76.5% vs. 63.5%) and other authors34 found the same tendency in Italy (54% of boys and 74% of girls), Greece (41% of boys and 56% of girls) and Spain (43% of boys and 60% of girls). We also found that boys were statistically more likely than girls not to brush correctly (OR = 1.874). Many studies suggest that girls have better oral hygiene habits than boys24., 29., 34., 35., 36., 37., 38., 39..
In the current study, 75.7% (n = 512) of those who lived in urban areas brushed at least twice a day, which is a higher proportion than those who lived in peri-urban (67.1%; n = 249) or rural (62.2%; n = 163) areas. After multivariate analysis, we found that living in rural (OR = 1.647) and peri-urban (OR = 1.926) areas is a risk factor for not brushing at least twice a day compared with those who live in urban areas. This is consistent with the findings of another Portuguese study, in which the rates of brushing twice a day were 61.1%, 34% and 43.4%, for urban, peri-urban and rural areas, respectively40.
Oral hygiene is influenced by sociodemographic factors; mother’s education level and type of residency are among the major influences40. A low level of maternal education is associated with poor oral hygiene routines and a higher risk for not brushing properly, compared with mothers with higher educational levels (OR = 2.284). In our study, the higher the mother’s educational level, the higher the percentage of participants who reported brushing correctly; 62.9% (n = 349) of participants whose mother had not completed high school reported brushing properly compared with 78.9% (n = 302) for those whose mother had completed high school and 79.5% (n = 178) for those whose mother had a college degree. The same relationship has been found in many other studies28., 41., 42.. Mother’s education level seems to have a stronger influence on children’s health than father’s education level26. However, father’s employment status is important for oral health; we found that adolescents with unemployed parents had a higher risk of not brushing twice a day (OR = 2.108) compared with adolescents who had working parents (43.1% and 26.6%, respectively, P < 0.001). These findings are in agreement with the literature which suggests that father’s occupation influences oral hygiene habits34.
The major limitation of this study is the use of ‘self-report’ data. Self-report data can be affected by social desirability and memory bias43.
Conclusions
Our study found that oral hygiene habits and visits to an oral health professional by Portuguese 12-year-old subjects were consistent with the literature on this subject. The oral health behaviours of Portuguese adolescents seem to be similar to those of teens in other European countries, although there were still some concerns (about one-third of participants did not brush their teeth at least twice a day, and about one-quarter had not visited a dentist in the past year).
We conclude that social health determinants have a major impact on oral health habits, suggesting that future approaches in oral health should always include not only the clinical symptoms and needs but also a holistic perspective of the patient. These findings point to the huge policy relevance of this issue and suggest that future approaches should be specific to some subpopulations and must also include the parents. Schools, health centres and the community should work together to build effective long-term strategies that focus on those most at risk, such as children from low socioeconomic backgrounds. Future studies in public oral health should focus on all social health determinants and their relationship to attitudes and behaviours in oral health.
Acknowledgements
The authors would like to thank the General Directorate of Health (Portugal) for providing access to the data. Additionally, the authors gratefully acknowledge the Portugese Chief Dental Officer, Dr Rui Calado, and his team for their support.
Funding
No funding to declare.
Competing interests
The authors declare that they have no competing interest.
References
- 1.Villalobos-Rodelo JJ, Medina-Soli C, Molina-Frechero N, et al. Dental caries in schoolchildren aged 6–12 years in Navolato, Sinaloa, México: experience, prevalence, severity and treatment needs. Biomedica. 2006;26:224–233. [PubMed] [Google Scholar]
- 2.Petersen PE, Kwan S. Equity, social health determinants and public health programmes – the case of oral health. Community Dent Oral Epidemiol. 2011;39:481–487. doi: 10.1111/j.1600-0528.2011.00623.x. [DOI] [PubMed] [Google Scholar]
- 3.Petersen PE, Bourgeois D, Ogawa H, et al. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83:661–669. [PMC free article] [PubMed] [Google Scholar]
- 4.Deljo E, Babbacic R, Meskovic B, et al. Impact of continuous education about oral hygiene on the changes of CPI-index for 12–15-year-old schoolchildren. Acta Inform Med. 2011;19:220–223. doi: 10.5455/aim.2011.19.220-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petersen PE. OMS; Geneva: 2003. The World Oral Health Report. [Google Scholar]
- 6.Bader J. Risk-based recall intervals recommended. Evid Based Dent. 2005;6:2–4. doi: 10.1038/sj.ebd.6400305. [DOI] [PubMed] [Google Scholar]
- 7.Lisboa; 2008. DGS – Saúde Oral – Estudo Nacional de Prevalência das Doenças Orais. [Google Scholar]
- 8.European Academy of Pediatric Dentistry Guidelines on the use of fluoride in children : an EAPD policy document. Eur Arch Paediatr Dent. 2009;10:129–135. doi: 10.1007/BF03262673. [DOI] [PubMed] [Google Scholar]
- 9.Riley P, Worthington HV, Clarkson JE, et al. Recall intervals for oral health in primary care patients. Cochrane Database Syst Rev. 2013;12(12):CD004346. doi: 10.1002/14651858.CD004346.pub4. [DOI] [PubMed] [Google Scholar]
- 10.American Academy of Pediatric Dentistry. Policy on use of fluoride. Reference Manual 2014 38(6): 16/17. Available from www.aapd.org/media/Policies_Guidelines/P_FluorideUse1.pdf. Accessed 28 February 2017.
- 11.Choo A, Delac DM, Messer LB. Oral hygiene measures and promotion: review and considerations. Aust Dent J. 2001;46:166–173. doi: 10.1111/j.1834-7819.2001.tb00277.x. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Pediatric Dentsistry. The state of the little teeth report; 2014. Available from: www.aapd.org/assets/1/7/State_of_Little_Teeth_Final.pdf. Accessed 28 February 2017.
- 13.NICE. Dental recall – recall interval between routine dental examinations; 2004. [PubMed]
- 14.Sjogren K, Birkhed D, Rangmar B. Effect of a modified toothpaste technique on approximal caries in preschool children. Caries Res. 1995;29:435–441. doi: 10.1159/000262111. [DOI] [PubMed] [Google Scholar]
- 15.Cunha-Cruz J, Milgrom P, Shirtcliff RM, et al. “Everybody brush!”: protocol for a parallel-group randomized controlled trial of a family-focused primary prevention program with distribution of oral hygiene products and education to increase frequency of tooth brushing. JMIR Res Protoc. 2015;4:e58. doi: 10.2196/resprot.4485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chestnutt IG, Schafer F, Jacobson AP, et al. The influence of toothbrushing frequency and post-brushing rinsing on caries experience in a caries clinical trial. Community Dent Oral Health Epidemiol. 1998;26:406–411. doi: 10.1111/j.1600-0528.1998.tb01979.x. [DOI] [PubMed] [Google Scholar]
- 17.Marinho VC, Higgings JP, Logan S, et al. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and dolescents. Cochrane Database Syst Rev. 2003;4(4):CD002782. doi: 10.1002/14651858.CD002782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van-Louvern C, Ketley CE, Cochran JA, et al. Fluoride ingestion from toothpaste: fluoride recovered from the toothbrush, the expectorate and the after-brush rinses. Commun Dent Oral Epidemiol. 2004;32(suppl):54–61. doi: 10.1111/j.1600-0528.2004.00140.x. [DOI] [PubMed] [Google Scholar]
- 19.Walsh T, Worthington HV, Glenny AM, et al. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2010;1(1):CD007868. doi: 10.1002/14651858.CD007868.pub2. [DOI] [PubMed] [Google Scholar]
- 20.Blas E, Kurup S. World Health Organization; Geneva: 2010. Equity, Social Determinants and Public Health Programmes; pp. 1–29. [Google Scholar]
- 21.Davoglio RS, Abegg C, Aerts RGC. Factors related to the use of dental services among adolescents from Gravataí, RS, Brazil, in 2005. Rev Bras Epidemiol. 2013;16:546–554. doi: 10.1590/S1415-790X2013000200028. [DOI] [PubMed] [Google Scholar]
- 22.Iasonos A, Schrag D, Ganesh RV, et al. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26:1364–1370. doi: 10.1200/JCO.2007.12.9791. [DOI] [PubMed] [Google Scholar]
- 23.Freire M, Sheiham A, Bino YA. Hábitos de higiene bucal e fatores sociodemográficos em adolescentes. Rev Bras Epidemiol. 2007;10:606–614. [Google Scholar]
- 24.Vettore MV, Moysés SJ, Sardinha LMV, et al. Sociodemographic status, toothbrushing frequency, and health-related behaviors in adolescents: an analysis using the PeNSE database. Cad Saude Pública. 2012;28:s101–s113. doi: 10.1590/s0102-311x2012001300011. [DOI] [PubMed] [Google Scholar]
- 25.Lapresa LB, Barbero BS. Análisis multinivel del uso de servicios de salud bucodental por población infanto-juvenil. Gac Sanit. 2011;25:91–96. doi: 10.1016/j.gaceta.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 26.Lapresa LB, Barbero BS, Arizaleta HL. Prevalencia de hábitos bucodentales saludables en la población infanto-juvenil residente en España. An Pediatr (Barc) 2012;76:140–147. doi: 10.1016/j.anpedi.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 27.Dominguez-Rojas V, Astasio-Arbiza P, Ortega-Molina P, et al. Analysis of several risks factors involved in dental caries through multiple logistic regression. Int Dent J. 1993;43:149–156. [PubMed] [Google Scholar]
- 28.Wierzbicka M, Petersen PE, Szatko F, et al. Changing oral health status and oral health behaviour of schoolchildren in Poland. Community Dent Health. 2002;19:243–250. [PubMed] [Google Scholar]
- 29.Freddo SL, Aerts DR, Abegg C, et al. Hábitos de higiene bucal e utilização de serviços odontológicos em escolares de uma cidade da Região Sul do Brasil. Cad Saúde Pública. 2008;24:1991–2000. doi: 10.1590/s0102-311x2008000900005. [DOI] [PubMed] [Google Scholar]
- 30.Pinilla J, González B. Exploring changes in dental workforce, dental care utilisation and dental caries levels in Europe, 1990–2004. Int Dent J. 2009;59:87–95. [PubMed] [Google Scholar]
- 31.Petersen PE, Jiang H, Peng B, et al. Oral and general health behaviours among Chinese urban adolescents. Commun Dent Oral Epidemiol. 2008;36:76–84. doi: 10.1111/j.1600-0528.2007.00375.x. [DOI] [PubMed] [Google Scholar]
- 32.Savage MF, Lee JY, Kotch JB, et al. Early preventive dental visits: effects on subsequent utilization and costs. Pediatrics. 2004;114:e418–e423. doi: 10.1542/peds.2003-0469-F. [DOI] [PubMed] [Google Scholar]
- 33.Matos MG, Simões C, Tomé G, et al. 1st ed. Centro de Malária e Outras Doenças Tropicais/IHMT/UNL; Lisboa: 2012. A Saúde dos Adolescentes Portugueses: Relatório do Estudo HBSC 2010; pp. 1–175. ISBN 9789899584952. [Google Scholar]
- 34.Maes L, Vereecken C, Vanobbergen J, et al. Tooth brushing and social characteristics of families in 32 countries. Int Dent J. 2006;56:159–167. doi: 10.1111/j.1875-595x.2006.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 35.CAHRU . Child and Adolescent Health Research Unit (CAHRU); Edinburgh: 2008. Inequalities in Young People’s Health Key Findings from the Health Behaviour in School-aged Children (HBSC) 2005/2006 Survey; pp. 1–5. [Google Scholar]
- 36.Kanli A, Kanbur NO, Dural S, et al. Effects of oral health behaviors and sociodemographic factors on a group of Turkish adolescents. Quintessence Int. 2007;38:26–32. [PubMed] [Google Scholar]
- 37.Levin KA, Currie C. Inequalities in toothbrushing among adolescents in Scotland 1998–2006. Health Educ Res. 2008;24:87–97. doi: 10.1093/her/cym096. [DOI] [PubMed] [Google Scholar]
- 38.Sakalauskien≐ Z, Vehkalahti MM, Murtomaa H, et al. Factors related to gender differences in toothbrushing among Lithuanian middle-aged university employees. Medicina (Kaunas) 2011;47:180–186. [PubMed] [Google Scholar]
- 39.Sakki TK, Knuuttila ML, Anttila SS. Lifestyle, gender and occupational status as determinants of dental health behavior. J Clin Periodontol. 1998;25:566–570. doi: 10.1111/j.1600-051x.1998.tb02489.x. [DOI] [PubMed] [Google Scholar]
- 40.de Almeida CM, Petersen PE, André SJ, et al. Changing oral health status of 6- and 12-year-old schoolchildren in Portugal. Community Dent Health. 2003;20:211–216. [PubMed] [Google Scholar]
- 41.Smyth E, Caamaño F, Fernández-Riveiro P. Oral health knowledge, attitudes and practice in 12-year-old schoolchildren. Med Oral Patol Oral Cir Bucal. 2007;12:614–620. [PubMed] [Google Scholar]
- 42.Nourijelyani K, Yekaninejad MS, Eshraghian MR, et al. The influence of mothers’ lifestyle and health behavior on their children: an exploration for oral health. Iran Red Crescent Med J. 2014;16:1–8. doi: 10.5812/ircmj.16051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonita R, Beaglehole R, Kjellström T. © World Health Organization; Geneva: 2006. Basic Epidemiology. [Google Scholar]