Abstract
Objectives: To analyse prescription of antibodies in emergency dental service according to antibiotic type, working diagnosis, patient visit time and patient demographic characteristics. Additionally, prescription practices among individual dentists were analysed. Methods: The data in this retrospective cohort study were collected from electronic medical records and analyzed using descriptive statistics. Statistical analyses were conducted using the chi-square test and the Z-test with post-hoc Bonferroni adjustment (α =0.05). Results: The study covered 20,879 patient visits during a 1.5-year period (from 1 June 2015 to 1 December 2016). Antibiotics were prescribed in 10,188 (48.8%) visits. In 6,202 (29.7%) visits, no dental treatment was performed and only an antibiotic was prescribed. The antibiotics most frequently prescribed were from the penicillin group and also contained clavulanic acid (70.5%); the second most frequently prescribed antibiotic was clindamycin (15.0%). The most common diagnoses for which an antibiotic was prescribed were acute apical abscess, pericoronitis and retained root; for these diagnoses, an antibiotic was prescribed in 79.8%, 64.3% and 63.3% of visits, respectively. Prescription of an antibiotic was significantly more frequent during Sundays and holidays (55.6% of visits) than during working days (33.2% of visits). Prescription of an antibiotic increased from the age of 1 towards the age of 75 and decreased thereafter. Female dentists prescribed antibiotics slightly but significantly (P < 0.001) more frequently than male dentists (50.8% and 46.8% of visits, respectively). High heterogeneity was observed among dentists regarding their criteria for prescribing antibiotics; individual dentists prescribed antibiotics in 15.0%–72.1% of the total number of visits. Conclusion: Multiple possible issues in the prescription of antibiotics were observed, ranging from administration for inappropriate indications to noncritical and excessive prescription.
Key words: Antibiotics, dentistry, antibiotic resistance, emergency dental service, acute odontogenic infections
INTRODUCTION
The development of antibiotic resistance poses a major threat to global public health1 and, by 2050, might lead to 10 million deaths per year worldwide from infections caused by antibiotic-resistant strains of bacteria.2 A 2016 USA survey estimated that of the total number of antibiotics prescribed, about 10% are given by dentists, suggesting their significant contribution to the issue of antibiotic resistance.3
To our knowledge, there is only one questionnaire-based study on the practice of antibiotic prescription by dentists in Croatia.4 This study reported that the antibiotics most commonly prescribed were of the penicillin group (73% of all antibiotics), and the most common indication for antibiotic prescription was a periapical or periodontal abscess (44% of all indications).
There are several studies on antibiotic prescription in dentistry from other parts of the world, which were also primarily based on self-reported data collected from dental practitioners using a questionnaire.5., 6., 7., 8. Salako et al.9 examined 200 dentists in Kuwait and found that that 90% would prescribe antibiotics for systemic involvement, while 55% would prescribe antibiotics for localised fluctuant swelling without systemic involvement. The preferred antibiotic in this study was amoxicillin (prescribed by 87% of dentists). A cross-sectional study from Belgium recorded antibiotic prescription during a 2-week period.7 Antibiotics were prescribed in 4.2% (1,033 out of 24,421) of patient visits. Broad-spectrum antibiotics (amoxicillin, amoxicillin + clavulanic acid and clindamycin) were those most commonly prescribed, representing 82% of all prescriptions. Generally, the literature reports suggest that antibiotic prescription may be inappropriate in many cases and that administration of such prescriptions has increased over time.4., 7., 10., 11., 12., 13.
Retrospective studies on antibiotic prescription in emergency dental service based on data from medical records are scarce.14., 15. A study of emergency dental clinics in Cheshire, UK, reported that 74% of patients received antibiotics without any surgical intervention.15 The most common reason for visiting an emergency dental office was acute pain, and the most commonly prescribed antibiotic was amoxicillin (72%).
The emergency dental service in the city of Zagreb is part of the public health service of primary dental care. It is organised in three dedicated dental offices, which provide acute pain relief on working days (Monday–Saturday), overnight (from 22.00 to 06.00 hours) on working days and for the entire 24-hour period from midnight on Saturday to midnight on Sunday and public holidays.16 The catchment of the emergency dental service in Zagreb is about 800,000. Dental treatment in emergency dental offices differs from that offered in regular dental offices, with the former being limited to providing simple and quick procedures, such as abscess incision or pulp extirpation, and the patient is referred to the regular dental service for all other types of treatment.
The aim of this study was to analyse antibiotic prescription in emergency dental services in the city of Zagreb according to several factors: type of antibiotic; working diagnosis; patient visit time; patient demographic characteristics; and prescription patterns of individual dentists.
METHODS
The study was conducted in full accordance with the World Medical Association Declaration of Helsinki and was approved by the Ethics Committee of the Community Health Center ‘Zagreb – Center’ (No. 2016/072-30/16-01/004) and the Ethics Committee of the Zagreb University School of Dental Medicine (No. 05-PA-15-3/2017). As the data were collected retrospectively from the computer database, no informed consent from patients was requested. All potentially identifying information was deleted immediately after acquiring the data.
The data were collected from electronic medical records in the period 1 June 2015– 1 December 2016 and entered into a computer database. The 1.5-year period was chosen in order to achieve the target sample size of about 20,000. All patients who attended the emergency dental service were included. The following variables were collected: time of patient’s arrival; patient age and gender; the name of the dentist who treated the patient; working diagnosis; dental procedure performed; and antibiotics prescribed. Working diagnoses were based on the assessment of the dentist in the emergency dental office who admitted the patient. Time of patient arrival was categorised by rounding up or down to the nearest hour.
In the data analysis, a new variable, denoted ‘frequency of antibiotic prescription’, was introduced, which was defined as the number of visits in which an antibiotic was prescribed divided by the total number of visits, for various levels of other factors.
Data were summarised by descriptive statistics, and proportions among different levels of categorical variables were compared using the chi-square test and the Z-test with Bonferroni correction. The association between workload and frequency of antibiotic prescription was explored using a linear regression model and Pearson correlation analysis. Statistical analysis was performed using SPSS 20 (IBM, Armonk, NY, USA) at a level of significance set at 0.05.
RESULTS
A total of 20,879 patient visits were recorded. The summary of patient characteristics is presented in Table 1. Antibiotics were prescribed in 10,188 cases, representing 48.8% of visits.
Table 1.
Summary of patient characteristics
| Characteristic | n | % |
|---|---|---|
| Age (years) | ||
| 1–10 | 1,768 | 8.5 |
| 11–20 | 1,870 | 9.0 |
| 21–30 | 5,245 | 25.1 |
| 31–40 | 4,324 | 20.7 |
| 41–50 | 3,268 | 15.7 |
| 51–60 | 2,251 | 10.8 |
| 61–70 | 1,295 | 6.2 |
| 71–80 | 618 | 3.0 |
| 81–90 | 226 | 1.1 |
| 91–100 | 14 | 0.1 |
| Gender | ||
| Male | 10,958 | 52.5 |
| Female | 9,921 | 47.5 |
| Diagnosis | ||
| Periapical periodontitis | 5,924 | 28.4 |
| Acute apical abscess | 4,565 | 21.9 |
| Pulpitis | 4,280 | 20.5 |
| Other | 1,829 | 8.8 |
| Retained root | 1,113 | 5.3 |
| Periodontitis | 944 | 4.5 |
| Caries | 816 | 3.9 |
| Pulpal necrosis | 689 | 3.3 |
| Pericoronitis | 406 | 1.9 |
| Gingivitis | 313 | 1.5 |
| Antibiotic prescribed | ||
| No antibiotic | 10,691 | 51.2 |
| Penicillin + clavulanic acid | 7,186 | 34.4 |
| Clindamycin | 1,322 | 6.3 |
| Metronidazole + penicillin | 735 | 3.5 |
| Metronidazole | 504 | 2.4 |
| Metronidazole + clindamycin | 207 | 1.0 |
| Cephalosporin | 110 | 0.5 |
| Penicillin | 50 | 0.2 |
| Penicillin + metronidazole | 35 | 0.2 |
| Penicillin + clindamycin | 27 | 0.1 |
| Other | 12 | 0.1 |
| Visit on | ||
| Working days | 13,552 | 35.1 |
| Sundays/holidays | 7,327 | 64.9 |
The most commonly prescribed antibiotics were of the penicillin group containing clavulanic acid (70.5%), followed by clindamycin (15.0%), metronidazole + penicillin (7.2%) and metronidazole alone (4.9%). Less common antibiotics included sulfonamides, tetracyclines, cephalosporins and macrolides.
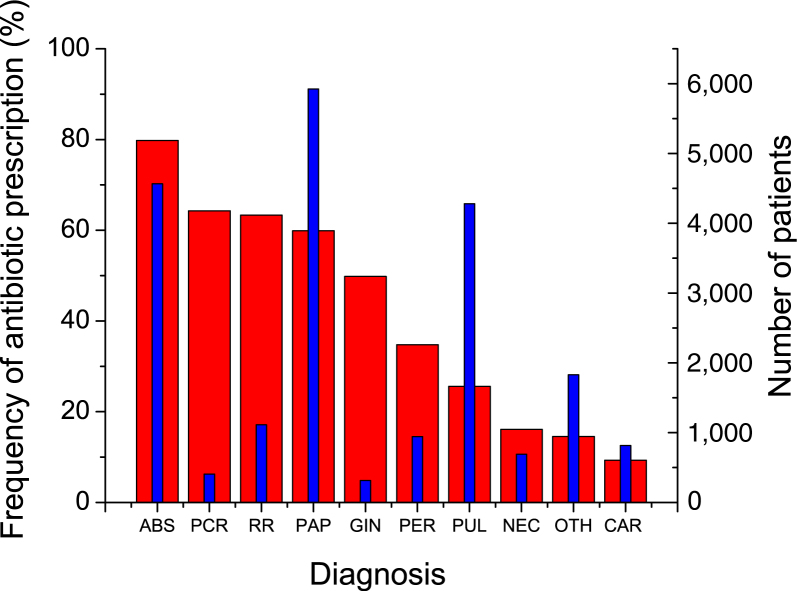
Figure 1 plots the frequency of antibiotic prescription for separate diagnoses, as well as the number of patients with a particular diagnosis. The most frequent diagnoses were periapical periodontitis, acute apical abscess and pulpitis, together representing 70.7% of all diagnoses. The frequency of antibiotic prescription was highest for acute apical abscess (79.8%), pericoronitis (64.3%) and retained root (63.3%). It is interesting to note that antibiotics were rather frequently prescribed for pulpitis (25.6%) and caries (9.3%), conditions for which they are ineffective.
Figure 1.
Frequency of antibiotic prescribed for an individual diagnosis (thick red bars) and number of patients (thin blue bars) with an individual diagnosis. ABS, acute apical abscess; CAR, caries; GIN, gingivitis; NEC, pulpal necrosis; OTH, other; PAP, periapical periodontitis; PCR, pericoronitis; PER, periodontitis; PUL, pulpitis; RR, retained root.
The frequency of antibiotic prescription was significantly higher (P < 0.001) over Sundays/holidays (55.6%) than during working days (36.2%). To compare the workload of emergency dental offices, the number of visits was divided by the number of working hours. The workload measure thus obtained (i.e. the average number of visits per hour) for Sundays/holidays was 3.3 visits per hour, nearly double that obtained for working days (1.7 visits per hour).
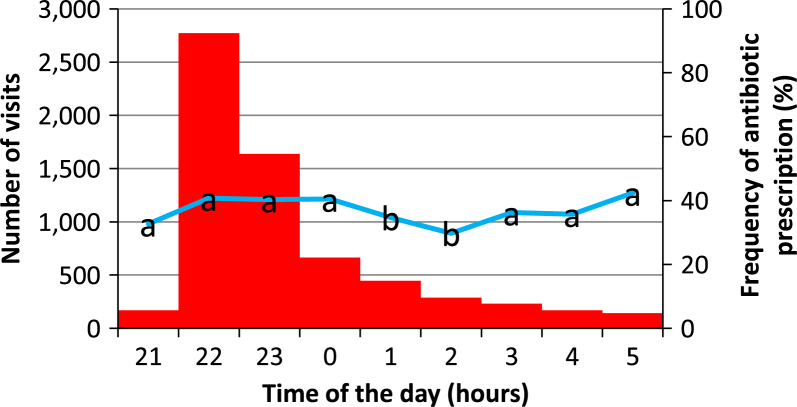
The distribution of patient visits throughout a working day (Monday to Saturday) shows marked inhomogeneity, with the peak value at 22.00 hours (Figure 2). After that, the number of visits declined gradually towards the morning. However, the frequency of antibiotic prescription was statistically similar when compared hour-by-hour, except for 01.00–02.00 hours, when it was significantly lower compared with other times of day.
Figure 2.
Analysis of the number of visits (red bars) and the frequency of antibiotic prescription (blue line) during working days. The same letters denote statistically homogeneous groups.
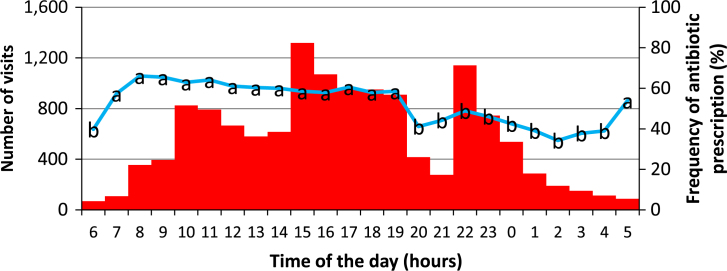
The distribution of patient visits over Sundays/holidays shows three peaks at 10.00, 15.00 and 22.00 hours. Visits were least frequent in the period between 02.00 and 07.00 hours (Figure 3). The frequency of antibiotic prescription was highest at 08.00 hours and exhibited a trend of decline towards 02.00 hours. The statistical analysis revealed two homogeneous groups – the first with a higher frequency of antibiotic prescription (55.4%–66.1%) in the period from 07.00 to 19.00 hours, and the second with a lower frequency of antibiotic prescription (34.2%–48.9%) in the period from 20.00 to 04.00 hours. For Sundays/holidays, Pearson correlation analysis revealed a significant moderate correlation (P = 0.014, R = 0.46) between the number of visits per hour and the frequency of antibiotic prescription. By contrast, no correlation was identified for working days.
Figure 3.
Analysis of number of visits (red bars) and the frequency of antibiotic prescription (blue line) during Sundays/holidays. The same letters denote statistically homogeneous groups.
As the distribution of diagnoses over the day may have had an effect on antibiotic prescription, the distribution of individual diagnoses throughout the day was assessed. The statistical analysis showed that all the diagnoses were homogeneously distributed in an hour-by-hour comparison, except for the diagnosis acute apical abscess, which showed a higher frequency in the morning (07.00–11.00 hours) during Sundays/holidays and a decreasing trend over the rest of the day.
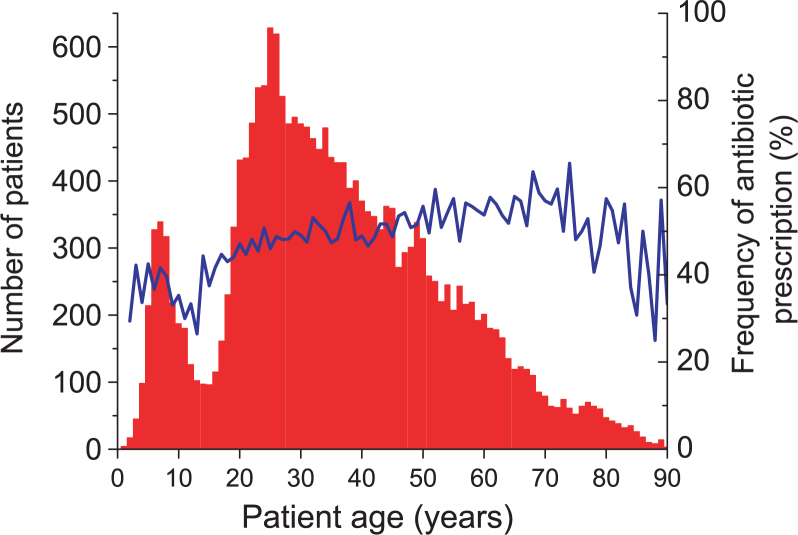
A bimodal distribution of patient age, with peak values at 7 and 25 years, was observed (Figure 4). The frequency of antibiotic prescription rose from 1 to 75 years (29.4%–65.6%, respectively), and decreased thereafter. A sharp decline in the frequency of antibiotic prescription around the age of 13 is concurrent with the decline in patient number around this age.
Figure 4.
Distribution of patients according to age (red bars) and the frequency of antibiotic prescription (blue line).
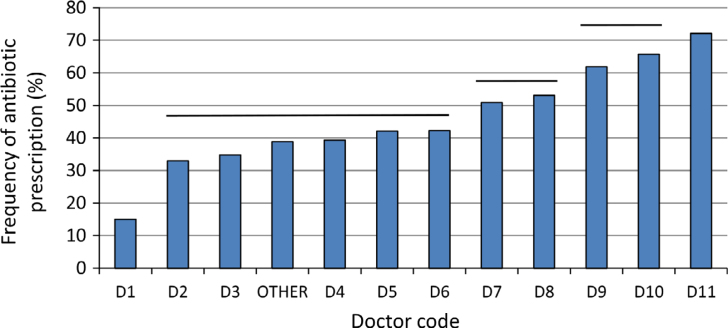
The frequency of antibiotic prescription was compared among 11 dentists who were permanently employed, while an additional 10 dentists who worked temporarily and treated a small number of patients (altogether <2%) were grouped in the category ‘other’ (Figure 5). Although the frequency of antibiotic prescription differed vastly among dentists, ranging between 15.0% and 72.1%, the preference for particular antibiotic types was similar among dentists: antibiotics of the penicillin group were those most commonly prescribed (65.3%–80.3% of all antibiotics) followed by clindamycin (6.9%–20.6%).
Figure 5.
Frequency of antibiotic prescription among individual dentists. Horizontal lines above bars denote statistically homogeneous groups.
The frequency of antibiotic prescription was statistically similar (P = 0.77) between male and female patients. However, the gender of dentists significantly influenced antibiotic prescription, with female dentists prescribing significantly more (P < 0.001) antibiotics than male dentists (in 50.8% and 46.8% of the total number of visits, respectively).
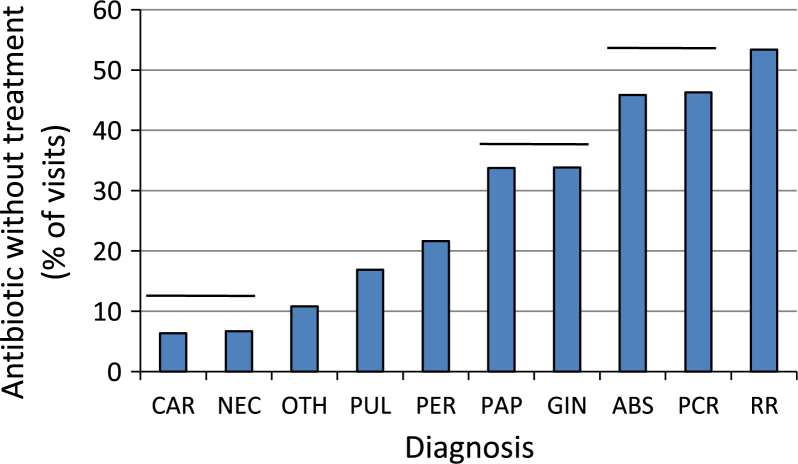
In 6,202 visits, no dental treatment was performed and only an antibiotic was prescribed. This number represents 29.7% of the total number of visits (20,879) and 60.9% of the total number of visits in which an antibiotic was prescribed (10,188). The practice of prescribing an antibiotic without performing any dental treatment was observed for all 11 dentists, with a wide variation in frequency among individual dentists (18.3%–44.6%). The frequency of antibiotic prescription with no treatment varied widely among diagnoses, ranging from 6.4% to 53.4% of the total number of visits (Figure 6).
Figure 6.
Percentage of visits in which an antibiotic was prescribed without any dental treatment being performed. ABS, acute apical abscess; CAR, caries; GIN, gingivitis; NEC, pulpal necrosis; OTH, other; PAP, periapical periodontitis; PCR, pericoronitis; PER, periodontitis; PUL, pulpitis; RR, retained root. Horizontal lines above bars denote statistically homogeneous groups.
DISCUSSION
This is the first large-scale study on antibiotic prescription in emergency dental service in Croatia which analysed 20,879 patient visits over a period of 1.5 years. A high frequency of antibiotic prescription (in 48.8% of all visits) was observed. Various factors were shown to affect the frequency of antibiotic prescription, such as day of the week, time of day, age of patient and even gender of the dentist.
The antibiotics most frequently prescribed are from the penicillin group and were given in combination with clavulanic acid. The preference of prescribing broad-spectrum antibiotics from the penicillin group (particularly amoxicillin) in our study was similar to that in the emergency dental service in the UK (70.5% and 72.0% of the total number of prescribed antibiotics, respectively).15 A similar practice of prescribing broad-spectrum penicillin was reported for dentists in Turkey, with amoxicillin being the antibiotic most commonly prescribed (67.8%).17 By contrast, the antibiotic prescription practice of Norwegian dentists is more conservative and narrow spectrum pencillin is preferred.11 The predominance of the penicillin group among the antibiotics prescribed in emergency dental service could be explained by the fact that acute odontogenic infections are usually characterised by abscess formation, which is caused primarily by strict anaerobes. Therefore, in most cases, the antibiotic is determined empirically without performing the time-consuming antibiogram, which is not feasible in emergency dental services.18 It should be noted that penicillins were predominantly prescribed in conjunction with clavulanic acid, while the prescription of penicillin only was negligible (Table 1). However, the combination of penicillin and clavulanic acid is considered unnecessary for treatment of odontogenic infection according to Scottish and UK guidelines19., 20. as there is no evidence of their superior effectiveness but presents an increased risk of Clostridium difficile infection. A Croatian study which analysed self-reported data on antibiotic prescription among 110 dentists found that both general practitioners and specialists also preferred the combination of penicillin and clavulanic acid.4
The second most frequently prescribed antibiotic was clindamycin. Indications for clindamycin use in dentistry are a medically proven allergy to penicillin or previously unsuccessful therapy with penicillin.21 Considering that the prevalence of penicillin allergy is about 10% in the general population, the ratio of clindamycin in the total number of prescribed antibiotics is expected to be similar.22 However, the observed ratio of clindamycin was somewhat higher (15.0%), which could be attributed to uncertainty about possible penicillin allergy because of difficulties in obtaining a detailed medical history in the emergency dental setting. Therefore, an alternative antibiotic (clindamycin) may have been chosen to avoid potential complications. The frequency of clindamycin prescriptions reported in our study is similar to that of Belgian dentists (13.9%) but lower than that of Turkish dentists (26.8%).7., 23.
Acute apical abscess was the leading diagnosis for which antibiotics were prescribed (79.8%, Figure 1). Comparatively, a cross-sectional study from the UK reported that general dental practitioners prescribed antibiotics for acute apical abscess with no systematic involvement (14.4%), with systematic involvement (9.8%) and chronic apical abscess (13.8%).24 A Cochrane review on systemic antibiotic administration in the therapy of periapical lesions identified only two representative studies, which were considered of low quality; thus, it was concluded that there is insufficient evidence to determine the effectiveness of systemic antibiotics in the treatment of acute apical abscess.25 It is interesting to note that antibiotics were also prescribed for pulpitis in 25.6% of cases (Figure 1). In comparison, Spanish oral surgeons and Belgian dentists prescribed antibiotics for pulpitis in 31.5% and 4.3% of cases, respectively.7., 26. A Cochrane review on antibiotic use for irreversible pulpitis stated that there is insufficient evidence to determine the effectiveness of antibiotics for pain reduction and also recommended that antibiotics should not be used as a substitute for immediate pulpectomy.27
As prescription of antibiotic was considerably more frequent during Sundays/holidays (55.6%) than working days (36.2%), it was investigated whether the number of patient visits per hour affected the frequency of antibiotic prescription. It was hypothesised that the higher workload of emergency dental offices at certain times of day (Figures 2 and 3) might affect frequency of antibiotic prescription. During working days, the frequency of antibiotic prescription was rather stable and ranged between 29.8% and 42.4%, despite the enormous difference in workload: nearly 25 times more patients per hour at the beginning of the shift than at the end of the shift (Figure 2). The number of patients per hour also appears to have had no influence on the frequency of antibiotic prescription during Sundays/holidays: although there were three ‘peak times’ for patient visits (Figure 3), none seems to have exerted an impact on the frequency of antibiotic prescription, which gradually decreased throughout the day. However, the moderate positive Pearson correlation identified for Sundays/holidays (R = 0.46) suggests that a higher workload of emergency dental offices was associated with increased prescription of antibiotics.
The distribution of individual diagnoses throughout the day was evaluated, as this may be the underlying cause of the trends in the frequency of antibiotic prescription shown in Figures 2 and 3. Therefore, the frequencies of each diagnosis were calculated on an hourly basis and compared throughout the day to check whether there are any patterns in the occurrence of any particular diagnosis as a function of time. All of the diagnoses were found to be equally distributed (occurring in statistically similar frequencies at all times of the day), except the diagnosis acute apical abscess on Sundays/holidays, which was significantly more frequent in the morning (07.00–11.00 hours) and gradually became less frequent towards the end of the day. Because acute apical abscess was the second most frequent diagnosis (21.9% of all diagnoses) and the first diagnosis by the frequency of antibiotic prescription (Figure 2), it is possible that the decreasing frequency of this diagnosis towards the end of the day is reflected in the antibiotic prescription pattern shown in Figure 3.
A possible explanation for the higher frequency of antibiotic prescription during Sundays/holidays than on working days could be prescription termed ‘just in case’, which was described in the literature as an empirical prescription of antibiotics in cases with no definitive indication, but rather with the aim of preventing possible complications.28 Another explanation for the higher frequency of prescriptions during Sundays/holidays could be the higher average workload of emergency dental offices (3.3 visits per hour, compared with 1.7 visits per hour during working days). The lack of time may mean that dentists in emergency dental offices are unable to perform adequate diagnostic tests and therapeutic procedures, leading them to prescribe antibiotics as the first line of treatment.15 Similar reasons for antibiotic prescription were also observed in a UK study of emergency dental service, in which a large number of patients were seen during working time.15
Patient’s request or patient’s expectation for antibiotics and lack of patient’s cooperation are additional reasons, identified in the literature, for potentially inappropriate or excessive prescription of antibiotics.24., 29. These factors may be more pronounced during Sundays/holidays because of longer waiting periods before treatment in general dental offices.
The frequency of antibiotic prescription increased from the age of 1, peaked at the age of 75 and decreased thereafter (Figure 4). As it is not possible to claim that increasing patient age is accompanied by a higher frequency of indications for antibiotic therapy, it could only be speculated that the observed increase in antibiotic prescription with age is a result of dentists’ subjective judgment that older patients should be ‘covered’ with antibiotics because of the higher prevalence of chronic diseases in older age.30 By contrast, the decreasing frequency of antibiotic prescription after the age of 75 could be attributed to the higher use of a large number of different medications, which is common among elderly subjects, and could lead to more conservative and critical prescription of antibiotics. It is interesting to note a decline in the frequency of antibiotic prescription in patients around the age of 13. A possible explanation is the presence of a young permanent dentition, which did not have sufficient time to develop severe odontogenic infections that would require an emergency intervention followed by the prescription of antibiotics. This explanation is supported by the distribution of visits according to patient age in Figure 4, showing the lowest frequency of visits to emergency dental offices around the age of 13.
A consensus regarding the types of antibiotics prescribed was observed among dentists; however, high variability was noted in the frequency of antibiotic prescription among dentists (Figure 5). Assuming that the severity of clinical cases was averaged among all dentists because of the large sample size, the fact that the frequency of antibiotic prescription among dentists varied in the range of 15.0%–72.1% indicates an enormous difference in subjective criteria for prescribing antibiotics. This could be explained by the lack of national guidelines for antibiotic use in dentistry and differences in education and work experience. In any case, these data highlight the notable disagreement among dentists regarding the need to use antibiotics in acute odontogenic infections.
The frequency of antibiotic prescription was similar between male and female patients. No gender differences in antibiotic prescription were found in British Columbia,10 whereas general dentists in the USA prescribed antibiotics more frequently for female patients than for male patients (8.5% and 6.9% respectively).12 By contrast, dentists from Kosovo prescribed antibiotics slightly more often for male patients (52%) than for female patients (48%).31
The gender of the dentist slightly, but significantly, influenced the prescription of antibiotics: female dentists prescribed antibiotics more frequently (in 50.8% of visits) than male dentists (46.8%). By contrast, Germack et al.3 found no difference in prescribing between male and female dentists. The data collected in our study are not sufficient to explain this gender difference but they point to the fact that antibiotic prescription is influenced by many, as yet unclarified, factors.
The finding that in 29.7% of the total number of visits only antibiotic was prescribed without performing any dental treatment suggests that antibiotics were very often considered as the first (and only) line of treatment. This finding is even more concerning considering that in more than the half (60.9%) of visits in which an antibiotic was prescribed, no additional dental treatment was performed. This indicates a very noncritical approach to the use of antibiotics, which are indicated for dental infection only when the signs of systemic spread of infection – fever, malaise, lymphadenopathy, cellulitis, progressive diffuse swelling and trismus – are present, as well as in cases of medically compromised patients.32 Although systemic antibiotic therapy should never be administered without local dental treatment, our data suggest that it was a very common practice.33 Figure 6 shows that antibiotics were occasionally prescribed without dental treatment, even for benign diagnoses (e.g. caries, in 6.4% of visits). More concerning is the fact that the highest frequencies of this practice were identified for rather severe diagnoses, namely acute apical abscess and pericoronitis (45.8% and 46.3% of visits, respectively).
While the inferences of this study are backed up by the large sample size, the focus on emergency dental care precludes generalisability of the findings presented to other types of dental care. Patients attending emergency dental offices differ from these encountered in a scheduled dental care setting primarily by their acute diagnoses and the lack of medical history available to the emergency dentist. Additionally, emergency dental patients tend to have poorer oral health and are generally less health conscious than the general population. Thus, emergency dentistry can be regarded as the least conservative setting for antibiotic prescription, whereas general and specialist dental offices would presumably have a more appropriate approach.
To summarise, the findings of this study indicate multiple possible issues in antibiotic prescription in Croatian emergency dental service, ranging from administration of antibiotics for inappropriate indications to noncritical and excessive prescription. Further studies encompassing general and specialist dental practices in Croatia are recommended in order to obtain a comprehensive insight into antibiotic prescription patterns. The issue of antibiotic over-prescription should be given more attention in dental school curricula, as well as in continuing education courses.
Acknowledgements
We would like to thank the software company MCS (Zagreb, Croatia) for help with the export of data from electronic medical records. The preliminary version of this study received the first prize for the best student research work sponsored by the School of Dental Medicine, University of Zagreb and Colgate. Part of this study was presented at the 2017 CED-IADR/NOF Congress in Vienna and received the first prize at the Robert Frank junior competition. This study received no external funding.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Aminoshariae A, Kulild JC. Evidence-based recommendations for antibiotic usage to treat endodontic infections and pain: a systematic review of randomized controlled trials. J Am Dent Assoc. 2016;147:186–191. doi: 10.1016/j.adaj.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 2.De Kraker MEA, Stewardson AJ, Harbarth S. Will 10 million people die a year due to antimicrobial resistance by 2050? PLoS Med. 2016;13:e1002184. doi: 10.1371/journal.pmed.1002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Germack M, Sedgley CM, Sabbah W, et al. Antibiotic use in 2016 by members of the american association of endodontists: report of a national survey. J Endod. 2017;43:1615–1622. doi: 10.1016/j.joen.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Perić M, Perković I, Romić M, et al. The pattern of antibiotic prescribing by dental practitioners in Zagreb, Croatia. Cent Eur J Public Health. 2015;23:107–113. doi: 10.21101/cejph.a3981. [DOI] [PubMed] [Google Scholar]
- 5.Jaunay T, Sambrook P, Goss A. Antibiotic prescribing practices by South Australian general dental practitioners. Aust Dent J. 2000;45:179–186. doi: 10.1111/j.1834-7819.2000.tb00554.x. [DOI] [PubMed] [Google Scholar]
- 6.Palmer NA, Pealing R, Ireland RS, et al. A study of therapeutic antibiotic prescribing in National Health Service general dental practice in England. Br Dent J. 2000;188:554–558. doi: 10.1038/sj.bdj.4800538. [DOI] [PubMed] [Google Scholar]
- 7.Mainjot A, D’Hoore W, Vanheusden A, et al. Antibiotic prescribing in dental practice in Belgium. Int Endod J. 2009;42:1112–1117. doi: 10.1111/j.1365-2591.2009.01642.x. [DOI] [PubMed] [Google Scholar]
- 8.Al-Haroni M, Skaug N. Knowledge of prescribing antimicrobials among Yemeni general dentists. Acta Odontol Scand. 2006;64:274–280. doi: 10.1080/00016350600672829. [DOI] [PubMed] [Google Scholar]
- 9.Salako NO, Rotimi VO, Adib SM, et al. Pattern of antibiotic prescription in the management of oral diseases among dentists in Kuwait. J Dent. 2004;32:503–509. doi: 10.1016/j.jdent.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Marra F, George D, Chong M, et al. Antibiotic prescribing by dentists has increased: Why? J Am Dent Assoc. 2016;147:320–327. doi: 10.1016/j.adaj.2015.12.014. [DOI] [PubMed] [Google Scholar]
- 11.Demirbas F, Gjermo PE, Preus HR. Antibiotic prescribing practices among Norwegian dentists. Acta Odontol Scand. 2006;64:355–359. doi: 10.1080/00016350600844394. [DOI] [PubMed] [Google Scholar]
- 12.Roberts RM, Bartoces M, Thompson SE, et al. Antibiotic prescribing by general dentists in the United States, 2013. J Am Dent Assoc. 2017;148:172–178.e171. doi: 10.1016/j.adaj.2016.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okunseri C, Zheng C, Steinmetz CN, et al. Trends and racial/ethnic disparities in antibiotic prescribing practices of dentists in the United States. J Public Health Dent. 2018;78:109–117. doi: 10.1111/jphd.12245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cachovan G, Phark JH, Schon G, et al. Odontogenic infections: an 8-year epidemiologic analysis in a dental emergency outpatient care unit. Acta Odontol Scand. 2013;71:518–524. doi: 10.3109/00016357.2012.696694. [DOI] [PubMed] [Google Scholar]
- 15.Dailey YM, Martin MV. Are antibiotics being used appropriately for emergency dental treatment? Br Dent J. 2001;191:391–393. doi: 10.1038/sj.bdj.4801190. [DOI] [PubMed] [Google Scholar]
- 16.Klaić B, Bratolić V, Šostar Z, et al. Organization of the emergency dental service in the city of Zagreb and Zagreb County. Acta Stomatol Croat. 2003;37:341–342. [Google Scholar]
- 17.Koyuncuoglu CZ, Aydin M, Kirmizi NI, et al. Rational use of medicine in dentistry: do dentists prescribe antibiotics in appropriate indications? Eur J Clin Pharmacol. 2017;73:1027–1032. doi: 10.1007/s00228-017-2258-7. [DOI] [PubMed] [Google Scholar]
- 18.Matijević S, Lazić Z, Kuljić-Kapulica N, et al. Empirical antimicrobial therapy of acute dentoalveolar abscess. Vojnosanit Pregl. 2009;66:544–550. doi: 10.2298/vsp0907544m. [DOI] [PubMed] [Google Scholar]
- 19.Scottish Dental Clinical Effectiveness Programme. Drug Prescribing for Dentistry - Dental Clinical Guidance, 3rd ed; 2016. Available from: www.sdcep.org.uk/
- 20.Palmer N, editor. Antimicrobial Prescribing for General Dental Practitioners. Faculty of General Dental Practice (UK); Wales, UK: 2016. Available from: www.fgdp.org.uk/ [Google Scholar]
- 21.Addy LD, Martin MV. Clindamycin and dentistry. Br Dent J. 2005;199:23–26. doi: 10.1038/sj.bdj.4812535. [DOI] [PubMed] [Google Scholar]
- 22.Albin S, Agarwal S. Prevalence and characteristics of reported penicillin allergy in an urban outpatient adult population. Allergy Asthma Proc. 2014;35:489–494. doi: 10.2500/aap.2014.35.3791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaptan RF, Haznedaroglu F, Basturk FB, et al. Treatment approaches and antibiotic use for emergency dental treatment in Turkey. Ther Clin Risk Manag. 2013;9:443–449. doi: 10.2147/TCRM.S52009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cope AL, Francis NA, Wood F, et al. Antibiotic prescribing in UK general dental practice: a cross-sectional study. Community Dent Oral Epidemiol. 2016;44:145–153. doi: 10.1111/cdoe.12199. [DOI] [PubMed] [Google Scholar]
- 25.Cope A, Francis N, Wood F et al. Systemic antibiotics for symptomatic apical periodontitis and acute apical abscess in adults. Cochrane Database Syst Rev 2014: CD010136. [DOI] [PubMed]
- 26.Segura-Egea JJ, Velasco-Ortega E, Torres-Lagares D, et al. Pattern of antibiotic prescription in the management of endodontic infections amongst Spanish oral surgeons. Int Endod J. 2010;43:342–350. doi: 10.1111/j.1365-2591.2010.01691.x. [DOI] [PubMed] [Google Scholar]
- 27.Agnihotry A, Fedorowicz Z, van Zuuren EJ et al. Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev 2016: CD004969. [DOI] [PubMed]
- 28.Poveda Roda R, Bagan JV, Sanchis Bielsa JM, et al. Antibiotic use in dental practice. A review. Med Oral Patol Oral Cir Bucal. 2007;12:E186–E192. [PubMed] [Google Scholar]
- 29.Chate RA, White S, Hale LR, et al. The impact of clinical audit on antibiotic prescribing in general dental practice. Br Dent J. 2006;201:635–641. doi: 10.1038/sj.bdj.4814261. [DOI] [PubMed] [Google Scholar]
- 30.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 31.Haliti N, Krasniqi S, Begzati A, et al. Antibiotic prescription patterns in primary dental health care in Kosovo. Fam Med Prim Care Rev. 2017;19:128–133. [Google Scholar]
- 32.Siqueira JF, Jr, Rocas IN. Microbiology and treatment of acute apical abscesses. Clin Microbiol Rev. 2013;26:255–273. doi: 10.1128/CMR.00082-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramu C, Padmanabhan TV. Indications of antibiotic prophylaxis in dental practice–Review. Asian Pac J Trop Biomed. 2012;2:749–754. doi: 10.1016/S2221-1691(12)60222-6. [DOI] [PMC free article] [PubMed] [Google Scholar]