Abstract
Introduction: A relationship between masticatory function and cognition has been reported. It is proposed that mastication changes the blood flow stimulating the perfusion/oxygenation of the brain. This literature review analysed the relation between mastication as a protective factor of the cognitive decline and the changes produced at brain level in adults associated with the brain blood flow. Materials and methods: A systematic review was performed according to the ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses’ (PRISMA) criteria in PubMed/MEDLINE, Web of Science, Scopus and Embase. Primary studies were included with no limit on the publication date, conducted on humans, and that established a relation between mastication, brain blood flow and cognitive functions in adult patients. Results: Nine clinical descriptive studies were selected and qualitatively analysed. The collected data suggest the greatest brain areas activated during mastication were the frontotemporal cortex, the caudate nucleus and the thalamus, revealing a positive correlation between chewing intensity and perfusion of the principal trigeminal nucleus. The increase in cerebral blood flow was measured by a local vasodilator effect resulting in increased neuronal metabolism in the region linked to learning and memory. In addition, partially edentulous participants had a marked prefrontal deactivation when they chewed without a prosthesis and presented a decrease in masticatory activity. Conclusion: Masticatory function may act as a protective factor in those patients with cognition impairment and neurodegenerative diseases, suggesting some mechanisms among which is the increase of cerebral blood flow.
Key words: Masticatory function, chewing, neurodegenerative disease, cerebral blood flow, cognition
INTRODUCTION
During the past few years, a relationship between mastication and cognitive function has been reported1. This association has been generally defined as ‘brain-stomatognathic axis’ and might be due to mastication as a physiological process that consists of a complex movement by a neuronal network that involves several areas of the brain, including the prefrontal cortex (PFC)2., 3..
Some authors suppose that mastication changes the blood flow of the internal carotid artery, stimulating the oxygenation and perfusion of the brain3., 4., 5., 6.. In addition, there is evidence that mastication increases the cortical blood flow of the somatosensory area, motor area, insular cortex, thalamus and cerebellum, and in pyramidal cells of the hippocampus7., 8..
Studies conducted in animals have established that a dysfunction in rat molars leads to a progressive loss of memory and learning capacity9., 10., revealing deficits that may play an important role in cognitive decline. To date, few studies have established the association between mastication and cognitive impairment. Nevertheless, cognitive decline and masticatory dysfunction should be carefully interpreted2.
Descriptive studies have shown that people with difficulty chewing also present with lower cognitive function and greater cognitive impairment, whereas activation of cerebral blood flow has a positive effect on a wide range of cognitive functions11. Tooth loss has also been described as a possible risk factor for developing neurodegenerative diseases such as Alzheimer’s disease (AD) or dementia in older adults12., 13., and it is estimated that the prevalence of these diseases will be about 131.5 million people by 205014. Dementia has also been associated with chronic periodontal disease. It is estimated that this periodontal condition may provide a peripheral source for pro-inflammatory cytokines and as a final consequence tooth loss. However, this relationship must be analysed carefully because tooth loss may be caused by a multitude of reasons besides periodontal15.
In this same context, it was reported that oral rehabilitation with a dental prosthesis may have a preventive effect on the cognitive and neurological deterioration of this population16.
The aim of this review is to analyse the available evidence that supports the relation between the masticatory function as a protective factor for cognitive decline and the changes produced at brain level, with special attention on the increase of brain blood flow.
MATERIALS AND METHODS
Literature search
A qualitative systematic review of literature was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria17. The following databases were used: PubMed/MEDLINE, Web of Science, Scopus and Embase; and the following keywords were used: mastication, masticatory, chewing, ‘brain oxygenation’, ‘cerebral blood flow’, ‘cognition’, ‘cognitive memory’, ‘cognitive function’, ‘neurodegenerative disease’ and ‘Alzheimer’s disease’. The keywords were combined with conjunctions OR and AND. The search was conducted between March and April, 2018. In addition, a manual search was made of the literature by reviewing the references in the articles found in the electronic search.
Eligibility criteria
This review included primary studies in humans (cross-sectional, retrospective or prospective, cohort, case–controls or clinical trials) that established a relationship among masticatory function, changes at the cerebral cortex level and cognitive functions in adults. Full-text articles with no limits on the publication date, written in English or Spanish, were also included for analysis. Systematic literature reviews, letters to the editor and case series or reports were excluded.
Article selection and data extraction
Two independent reviewers analysed articles obtained in the systematic search process by reviewing the titles and abstracts. Articles that fulfilled the eligibility criteria were analysed in full text to confirm their relevance. A third reviewer resolved any discrepancy during the article review process. The following information was collected from the full-text articles comprising the final selection: author(s), publication year, country, design of study, sample sizes, sex and ages of subjects. The primary evaluated outcome was increased cerebral blood flow, increased brain perfusion/oxygenation and cognitive decline by the Mini-Mental State Exam (MMSE).
Evaluation of article quality
The risk of bias in the articles included in this review was assessed according to the study verification checklist of the ‘Cohort of the Critical Appraisal Skills Programme’ (CASP)18. This list was modified for its application in cross-sectional studies, following the methodology of Tada and Miura (2017)11; for example, question 2, ‘Was the cohort recruited in an acceptable way?’ was changed to ‘Was the sample recruited in an acceptable way?’ Questions about participant follow-up were excluded due to the study and design. For each study, the strength and weakness were calculated based on relevant elements in the verification checklist, and assigned a qualification of ‘low’, ‘moderate’ or ‘high’.
RESULTS
Study selection
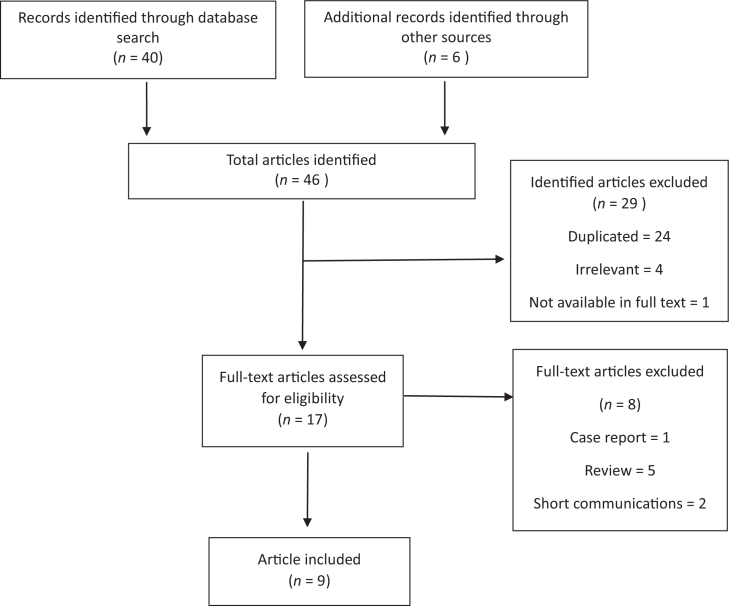
The article search and selection process is summarised in Figure 1. The total number of articles found in the used databases was 40. Six additional articles were included after the manual search. After the initial reading by title and abstract, 29 articles were ruled out, of which 24 were duplicates, four bore no relation to the study subject and one was not available in full text. Of all the articles available for evaluation (17 in total), eight were excluded, of which five were literature reviews, two were short communications and one was a case report. Finally, in this review nine articles were included that corresponded to descriptive studies.
Figure 1.
Flow chart of the qualitative systematic review.
Characteristics of the studies
All articles selected were ‘cross-sectional studies’, two of them analysed cerebral blood flow by magnetic resonance imaging (Table 1). Viggiano et al.6 quantified blood perfusion from the principal trigeminal nucleus after a mastication exercise, whereas Momose et al.7 evaluated the changes in regional cerebral blood flow during mastication. The latter also used positron emission tomography to measure brain activity. Other articles used methodologies such as bilateral transcranial Doppler ultrasound4 and xenon-enhanced computed tomography19.
Table 1.
Summary of studies on mastication and cerebral blood flow
| Reference | Study sample | Mastication | Outcome | Results |
|---|---|---|---|---|
| Momose et al.7 | 12 individuals (18–40 years, Japan) | Chew gum | Increased regional cerebral blood flow | Positive association in the primary sensorimotor areas increased by 25%–28% |
| Sesay et al.19 | 7 individuals (24–57 years, Japan) | Chew gum | Increased regional cerebral blood flow | Positive association between mastication and cerebral blood flow |
| Hasegawa et al.4 | 12 individuals (mean age, 26.6 ± 3.5 years, Japan) | Gum chewing, clenching and tooth tapping | Human jaw movement increased cerebral blood flow | The patterns and intensity of muscle contraction during jaw movements increased cerebral blood flow |
| Viggiano et al.6 | 18 individuals (19–28 years, Italy) | Chew gum on one side of the mouth | Increased blood perfusion of the principal trigeminal nucleus | Mastication exercise caused a perfusion increase within the principal trigeminal nucleus but not in the dorsolateral midbrain |
Two articles evaluated the association between mastication and cerebral oxygenation (Table 2). By using a magnetic resonance image, Onozuka et al.1., 20. examined the association between neuronal activity and chewing gum in various age groups. Other authors, such as Yokoyama et al.3, using near-infrared spectroscopy, pointed out the relation between mastication and cerebral oxygenation, just as Kamiya et al.12 reported the effects of dental prostheses on the activity of the PFC during mastication.
Table 2.
Summary of studies on mastication and brain perfusion/oxygenation
| Reference | Study sample | Mastication | Outcome | Results |
|---|---|---|---|---|
| Onozuka et al.20 | 17 individuals (20–31 years, Japan) | Chew gum (G-type and X-type) | Increase in brain neuronal activities related to gum hardness | Chewing causes regional increases in brain neuronal activities related to biting force |
| Onozuka et al.1 | 32 individuals (19–73 years) divided into three groups | Chew gum | Changes in brain regional activity | Bilateral increase in blood oxygenation level dependent on the sensorimotor cortex, cerebellum, thalamus, supplementary motor area and insula |
| Campos et al.21 | 16 individuals (76.7 ± 6.3 years) with mild AD 16 age and gender-matched healthy controls (75.23 ± 4.4 years) |
Optical chewable test | MMSE | Mild AD patients had decreased masticatory performance and MMSE compared with controls, and it was suggesting a lower stimulation in brain areas related to memory |
| Kamiya et al.12 | 12 individuals (mean age = 63.1 ± 6.1 years, Japan) | Chew gum, tooth loss and wearing dentures | Improved prefrontal activity | Prefrontal activation during chewing with a denture may prevent prefrontal depression induced by tooth loss in elderly edentulous patients |
| Yokoyama et al.3 | 11 individuals (mean age = 20.9 ± 0.9 years, Japan) | Chew gum at differing rates: 30, 70, and 110 rpm | Oxygenation of the PFC | Increased PFC oxygenation during faster mastication compared with normal and slower mastication conditions |
AD, Alzheimer’s disease; MMSE, Mini-Mental State Exam; PFC, prefrontal cortex.
Campos et al.21 by using the MMSE assessed the relation among chewing function in elderly individuals with AD with cognitive status.
Quality of the studies
According to the results obtained by the CASP (Table 3), the strengths of the studies analysed included the focus of the study subjects, the recruitment of the participants, and the measurement of exposure and results to minimise bias. The weaknesses found in most of the studies were the identification of confounding factors for study design and analysis. In summary, only three studies identified and considered factors such as the composition and hardness of the gum for the trial, the side of preference during mastication, the number of functional teeth in the mouth, and ages of the participants. With respect to the quality of the studies, three were described as high and five as moderate.
Table 3.
Risk assessment of bias in the articles
| 1 | 2 | 3 | 4 | 5a | 5b | 6 | 7 | 8 | Quality assessment | |
|---|---|---|---|---|---|---|---|---|---|---|
| Momose et al.7 | + | + | + | + | − | − | + | + | + | Moderate |
| Sesay et al.19 | + | + | + | + | − | − | + | + | + | Moderate |
| Onozuka et al.20 | + | + | + | + | + | + | + | + | + | High |
| Onozuka et al.1 | + | + | + | + | + | + | + | + | + | High |
| Hasegawa et al.4 | + | + | + | + | − | − | + | + | + | Moderate |
| Viggiano et al.6 | + | + | + | + | − | − | + | + | + | Moderate |
| Kamiya et al.12 | + | + | + | + | − | − | + | + | + | Moderate |
| Yokoyama et al.3 | + | + | + | + | + | + | + | + | + | High |
1 Did the study address a clearly focused issue? 2 Were the subjects recruited in an acceptable way? 3 Was the exposure accurately measured to minimise bias? 4 Was the outcome accurately measured to minimise bias? 5a Have the authors identified all important confounding factors? 5b Have they taken account of the confounding factors in the design and/or analysis? 6 Do you believe the results? 7 Can the results be applied to the local population? 8 Do the results of this study fit with other available evidence?
Impact of mastication and the increase of cerebral blood flow
The results indicate that four articles show an association between mastication and the increase in regional cerebral blood flow4., 6., 7., 19..
These articles indicate that the increase in cerebral blood flow as measured by a local vasodilator factor (such as the increase in partial carbon dioxide CO2 pressure or the reduction in partial pressure of O2) resulting from an increase in neuronal metabolism7 in the region of the primary sensorimotor cortices, supplementary motor areas, the insula, the corpus striatum and the cerebellum. These regions are linked to learning and memory, so an increase in oxygen concentration would be essential to carrying out these processes7., 22.. According to the study by Tada and Miura, the zones with the greatest activation during mastication were the frontotemporal cortex, the caudate nucleus and the thalamus, where an increase of over 15% in regional cerebral blood flow was recorded19. Moreover, it was previously found that there is a correlation between chewing intensity and blood perfusion in the principal trigeminal nucleus; the authors maintain that an increase in cerebral blood flow increases neuronal activity in the trigeminal nucleus6.
Impact of mastication on brain activity (perfusion) and oxygenation
From another perspective, the relation between mastication and the activation of different parts of the brain has also been studied. The effect of masticatory frequency and oxygenation on the PFC has been observed, with an increase in oxygenation being recorded at a mastication frequency of 110 rpm3. Moreover, Onozuka et al.1., 20. observed a significant bilateral increase in cerebral oxygenation in all subjects, in areas such as the sensorimotor cortex, supplementary motor area, thalamus, cerebellum and insula1., 20.. The study by Kamiya et al.11 found that partially edentulous participants had a marked prefrontal deactivation when they chewed without a prosthesis and presented a decrease in masticatory activity. Finally, Campos et al.21 mentioned that chewing may stimulate brain areas related to memory, especially the hippocampus and, according to his results, participants with AD show a decrease in MMSE and values of masticatory performance compared with control subjects.
DISCUSSION
The present systematic review of the literature was carried out with the aim of qualitatively assessing and evaluating existing clinical evidence on the correlation between decreased masticatory function and cognitive decline. All the articles selected demonstrated a correlation between the decline of both factors; however, due to the great disparity in methodologies, it is still not clear what the most probable mechanisms associated with this correlation would be.
Early experiments on animals suggest that mastication can alter the neuronal metabolism and provision of regional cerebral blood, activating some areas of the cerebral cortex23., 24., 25.. There is evidence of the impact that mastication has on cerebral activation; descriptive studies in humans demonstrate6., 7., 19. different areas of activation, such as the primary sensorimotor cortex, supplementary motor area, insula, corpus striatum, thalamus and cerebellum, the activity of which increases as a result of mastication. It is estimated that these areas receive information from oral structures (lips, tongue, oral mucosa, teeth, jaw); hence, they could be considered the masticatory centre26. Other authors have also confirmed the relation between mastication and the increase in bilateral cerebral blood flow in the frontal and parietal inferior lobes27.
Suzuki et al.28 demonstrated that chewing moderately hard food leads to an increase in cerebral blood flow through flow changes that occur from the common carotid artery and the internal carotid artery. These results are complemented by Onozuka et al.20 who reported that chewing gum with differing degrees of hardness significantly increases brain activity; later, in 2003, they also reported that some regional increases in neuronal activity in the brain may be age-dependent1, and were one of the first studies to analyse these variables. A high level of blood oxygen was reported in some cerebral regions, such as the PFC and hippocampus, and is needed for processes such as learning and memory, which also relates to the status of mastication and cognitive processing3.
Evidence from animal studies demonstrated that a decrease in masticatory function, either by extraction or reduction in the height of molars with a long-term soft diet, may be associated with reduction in learning and memory24., 25., 29., 30., 31., 32., and changes in occlusal function appear to be related to morphological alterations in animal models. Epidemiological studies also highlight the correlation between tooth loss and the worsening of dementia in older adults, and it has been reported that chewing efficiency with a dental prosthesis decreases by 30–40%4., 33., 34.. For example, Campos et al.21 discovered a correlation between masticatory function and cognitive decline in mild AD, partially edentulous subjects, compared with a control group. However, limited evidence links these variables and cerebral blood flow during mastication, but some results show a significant activation of the PFC when participants used a dental prosthesis, and it is proposed that rehabilitation may be effective in prevention of neurodegenerative diseases.
As mentioned, it has been proposed that mastication could be a protective factor against neurodegenerative diseases35, because different studies support the hypothesis that those with a greater number of teeth have a lower rate of dementia and therefore less cognitive impairment11., 21., 36., 37.. Due to the number of studies that have examined changes in cerebral blood flow, this mechanism should be considered to help explain this relationship.
According to the results of this review, the confounding factors are the hardness of the chewing gum, the side of preference during mastication, the number of functional teeth in the mouth and age of the participants. Only the study of Kamiya et al.12 related mastication to tooth loss and regional cerebral activation, revealing that the activation occurs mainly with the use of a dental prosthesis; besides, it is important to emphasise that both mastication and cerebral activation were objectively evaluated using validated methods but did not take into account the confounding factors. Otherwise, this descriptive study was performed on healthy subjects, with no intervention in masticatory function and in a small sample. Thus, a greater number of participants are needed to assess the importance of all variables. Activation of cerebral activity was found to increase significantly in the dorsal PFC during chewing while wearing a dental prosthesis, compared with controls without dentures5., 12., although experimental studies in animal models suggested that other cerebral zones are activated during mastication, not only the PFC29., 30., 31., 32.. Furthermore, according to the study by Kamiya et al.,12 prefrontal activation is not related to age, because little difference was found between elderly participants wearing dentures during mastication and young healthy controls. Thus, it has been suggested that a compensatory mechanism allows the response to increasing masticatory cognitive demand, activating the same prefrontal region12. Nevertheless, with the available evidence, it is estimated that early dental rehabilitation can contribute not only to chewing comfort and oral quality of life in aged people, but also with the prevention of cognitive deficiencies in adults.
CONCLUSIONS
The data analysed in this systematic review suggested that masticatory function may act as a protective factor in those patients with cognition impairment and neurodegenerative diseases, suggesting the importance of cerebral blood flow; also it is dependent on the intensity of this function and the number of functional teeth in the mouth. However, further investigation is needed to correlate the effect of tooth loss on cerebral activation as it relates to memory and learning. To do this, intervention studies are suggested.
Conflict of interest
The authors declare no conflict of interest.
Source of funding
The authors did not receive any funding to undertake this study.
References
- 1.Onozuka M, Fujita M, Watanabe K, et al. Age-related changes in brain regional activity during chewing: a functional magnetic resonance imaging study. J Dent Res. 2003;82:657–660. doi: 10.1177/154405910308200817. [DOI] [PubMed] [Google Scholar]
- 2.Lin C. Revisiting the link between cognitive decline and masticatory dysfunction. BMC Geriatr. 2018;18:5. doi: 10.1186/s12877-017-0693-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yokoyama T, Sato M, Natsui S, et al. Effect of gum chewing frequency on oxygenation of the prefrontal cortex. Percept Mot Skills. 2016;124:58–71. doi: 10.1177/0031512516683074. [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa Y, Ono T, Hori K, et al. Influence of human jaw movement on cerebral blood flow. J Dent Res. 2007;86:64–68. doi: 10.1177/154405910708600110. [DOI] [PubMed] [Google Scholar]
- 5.Narita N, Kamiya K, Yamamura K, et al. Chewing-related prefrontal cortex activation while wearing partial denture prosthesis: pilot study. J Prosthodont Res. 2009;53:126–135. doi: 10.1016/j.jpor.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Viggiano A, Manara R, Conforti R, et al. Mastication induces long-term increases in blood perfusion of the trigeminal principal nucleus. Neuroscience. 2015;311:75–80. doi: 10.1016/j.neuroscience.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 7.Momose T, Nishikawa J, Watanabe T, et al. Effect of mastication on regional cerebral blood flow in humans examined by positron-emission tomography with 15O-labelled water and magnetic resonance imaging. Arch Oral Biol. 1997;42:57–61. doi: 10.1016/s0003-9969(96)00081-7. [DOI] [PubMed] [Google Scholar]
- 8.Stratulat I, Cuciureanu D, Eva L, Rad R., Dr No. 99 cerebral blood flow in patients with central nervous pathologies associated with an adequate edentation treatment. PM&R. 2014;6:S115. [Google Scholar]
- 9.Yamamoto T, Hirayama A. Effects of soft-diet feeding on synaptic density in the hippocampus and parietal cortex of senescence-accelerated mice. Brain Res. 2001;902:255–263. doi: 10.1016/s0006-8993(01)02410-6. [DOI] [PubMed] [Google Scholar]
- 10.Terasawa H, Hirai T, Ninomiya T, et al. Influence of tooth-loss and concomitant masticatory alterations on cholinergic neurons in rats: immunohistochemical and biochemical studies. Neurosci Res. 2002;43:373–379. doi: 10.1016/s0168-0102(02)00063-9. [DOI] [PubMed] [Google Scholar]
- 11.Tada A, Miura H. Association between mastication and cognitive status: a systematic review. Arch Gerontol Geriatr. 2017;70:44–53. doi: 10.1016/j.archger.2016.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Kamiya K, Narita N, Iwaki S. Improved prefrontal activity and chewing performance as function of wearing denture in partially edentulous elderly individuals: functional near-infrared spectroscopy study. PLoS ONE. 2016;11:e0158070. doi: 10.1371/journal.pone.0158070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weijenberg R, Scherder E, Lobbezoo F. Mastication for the mind—the relationship between mastication and cognition in ageing and dementia. Neurosci Biobehav Rev. 2011;35:483–497. doi: 10.1016/j.neubiorev.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Alzheimer’s Disease International . Alzheimer’s Disease International; London: 2015. World Alzheimer Report 2015. [Google Scholar]
- 15.Tonsekar P, Jiang S, Yue G. Periodontal disease, tooth loss and dementia: is there a link? A systematic review. Gerodontology. 2017;34:151–163. doi: 10.1111/ger.12261. [DOI] [PubMed] [Google Scholar]
- 16.Ribeiro G, Campos C, Rodrigues Garcia R. Influence of a removable prosthesis on oral health-related quality of life and mastication in elders with Parkinson disease. J Prosthet Dent. 2017;118:637–642. doi: 10.1016/j.prosdent.2016.12.018. [DOI] [PubMed] [Google Scholar]
- 17.Hutton B, Catalá-López F, Moher D. La extensión de la declaración PRISMA para revisiones sistemáticas que incorporan metaanálisis en red: PRISMA-NMA. Med Clín. 2016;147:262–266. doi: 10.1016/j.medcli.2016.02.025. [DOI] [PubMed] [Google Scholar]
- 18.Gray M, Brice R, Moore S et al. CASP Checklists – CASP – Critical Appraisal Skills Programme (Internet). CASP – Critical Appraisal Skills Programme; 2018. Available from: https://casp-uk.net/casp-tools-checklists/. Accessed 22 June 2018
- 19.Sesay M, Tanaka A, Ueno Y, et al. Assessment of regional cerebral blood flow by xenon-enhanced computed tomography during mastication in humans. Keio J Med. 2000;49:125–128. [PubMed] [Google Scholar]
- 20.Onozuka M, Fujita M, Watanabe K, et al. Mapping brain region activity during chewing: a functional magnetic resonance imaging study. J Dent Res. 2002;81:743–746. doi: 10.1177/0810743. [DOI] [PubMed] [Google Scholar]
- 21.Campos C, Ribeiro G, Costa J, et al. Correlation of cognitive and masticatory function in Alzheimer’s disease. Clin Oral Invest. 2016;21:573–578. doi: 10.1007/s00784-016-1923-z. [DOI] [PubMed] [Google Scholar]
- 22.Senda M, Ishiyama N, Ishii K, et al. Changes in regional cerebral blood flow during mastication in young and old normal subjects measured with positron emission tomography. J Masticat Health Soc. 1992;2:49–54. [Google Scholar]
- 23.Funakoshi M, Kawamura S, Fujiwara H, et al. In: Mechanobiological Research on the Masticatory System. Kubota K, editor. VEB Verlag ftir Medizin und Biologie; Berlin: 1989. Effects of mastication on postnatal development of brain; pp. 162–167. [Google Scholar]
- 24.Onozuka M, Watanabe K, Mirbod SM, et al. Reduced mastication stimulates impairment of spatial memory and degeneration of hippocampal neurons in aged SAMP8 mice. Brain Res. 1999;826:148–153. doi: 10.1016/s0006-8993(99)01255-x. [DOI] [PubMed] [Google Scholar]
- 25.Kawahata M, Ono Y, Ohno A, et al. Loss of molars early in life develops behavioral lateralization and impairs hippocampus-dependent recognition memory. BMC Neurosci. 2014;15:1–8. doi: 10.1186/1471-2202-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakamura Y, Katakura N. Generation of masticatory rhythm in the brainstem. Neurosci Res. 1995;23:1–19. [PubMed] [Google Scholar]
- 27.Watanabe I, Ishiyama N, Senda M. Cerebral blood flow during mastication measures with positron emission tomography. Geriatric Dent. 1992;6:148–150. [Google Scholar]
- 28.Suzuki M, Ishiyama I, Takiguchi T, et al. Effects of gum hardness on the response of common carotid blood flow volume, oxygen uptake, heart rate and blood pressure to gum-chewing. J Mastica Health Sci. 1994;4:9–20. [Google Scholar]
- 29.Mori D, Katayama T, Miyake H, et al. Occlusal disharmony leads to learning deficits associated with decreased cellular proliferation in the hippocampal dentate gyrus of SAMP8 mice. Neurosci Lett. 2013;534:228–232. doi: 10.1016/j.neulet.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Kubo KY, Yamada Y, Iinuma M, et al. Occlusal disharmony induces spatial memory impairment and hippocampal neuron degeneration via stress in SAMP8 mice. Neurosci Lett. 2007;414:188–191. doi: 10.1016/j.neulet.2006.12.020. [DOI] [PubMed] [Google Scholar]
- 31.Onishi M, Iinuma M, Tamura Y, et al. Learning deficits and suppression of the cell proliferation in the hippocampal dentate gyrus of offspring are attenuated by maternal chewing during prenatal stress. Neurosci Lett. 2014;560:77–80. doi: 10.1016/j.neulet.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 32.Kato T, Usami T, Noda Y, et al. The effect of the loss of molar teeth on spatial memory and acetylcholine release from the parietal cortex in aged rats. Behav Brain Res. 1997;83:239–342. doi: 10.1016/s0166-4328(97)86078-0. [DOI] [PubMed] [Google Scholar]
- 33.Hansson P, Sunnegårdh-Grönberg K, Bergdahl J, et al. Relationship between natural teeth and memory in a healthy elderly population. Eur J Oral Sci. 2013;121:333–340. doi: 10.1111/eos.12060. [DOI] [PubMed] [Google Scholar]
- 34.Lexomboon D, Trulsson M, Wårdh I, et al. Chewing ability and tooth loss: association with cognitive impairment in an elderly population study. J Am Geriatr Soc. 2012;60:1951–1956. doi: 10.1111/j.1532-5415.2012.04154.x. [DOI] [PubMed] [Google Scholar]
- 35.Chen H, Iinuma M, Onozuka M, et al. Chewing maintains hippocampus-dependent cognitive function. Int J Med Sci. 2015;12:502–509. doi: 10.7150/ijms.11911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Okamoto N. Effect of occlusal support by implant prostheses on brain function. J Prosthodont Res. 2011;55:206–213. doi: 10.1016/j.jpor.2011.01.003. [DOI] [PubMed] [Google Scholar]
- 37.Oh B, Han D, Han K, et al. Association between residual teeth number in later life and incidence of dementia: a systematic review and meta-analysis. BMC Geriatr. 2018;18:1–9. doi: 10.1186/s12877-018-0729-z. [DOI] [PMC free article] [PubMed] [Google Scholar]