Abstract
Objectives: This study aimed to explore the influence of dental insurance coverage on access to preventive periodontal care. Data were extracted from the 2011, 2013 and 2015 Korean Community Health Surveys conducted by the Korea Centers for Disease Control and Prevention. Materials and methods: This study was designed as a 5-year time series analysis using secondary data. Trends in the utilisation rate of dental scaling services before and after the introduction of insurance coverage for dental scaling were evaluated, and the influence of dental insurance coverage on access to preventive periodontal care was assessed. Results: In the 4 years after 2011, the utilisation rate of scaling services increased by 12.3%. The increase in the utilisation rate from 2011 to 2015 was greater for participants ≥ 65 years old and 45–64 years old compared with those who were 19–34 or 35–44 years old. The odds ratios (ORs) for using scaling in 2011, 2013 and 2015 were 0.9, 1.1 and 1.5, respectively, for participants with healthy gingiva. For elderly participants with gingival bleeding, the utilisation rate of scaling services increased after 2015 with ORs of 0.8, 0.9 and 1.2 for 2011, 2013 and 2015, respectively. Conclusions: Insurance coverage for dental scaling positively influenced access to preventive care for periodontal disease in middle-aged and elderly individuals. In the future, the long-term contributions of dental insurance coverage to the prevalence of periodontal disease and oral health disparities should be evaluated.
Key words: Health surveys, health insurance, preventive care, preventive dentistry, periodontal disease
INTRODUCTION
Periodontal disease is a chronic condition experienced by most middle-aged and elderly individuals worldwide1., 2., and has negative effects on general health3., 4., 5.. The severity of periodontal disease increases with age, and the lack of timely prevention or treatment can result in pain, discomfort while chewing, and tooth loss, as well as impaired psychosocial functioning and economic burden1., 6.. Thus, periodontal disease is a major chronic health problem that impairs the quality of life in middle and old age7.
Dental scaling is, in some instances, considered to be a preliminary step in periodontal disease treatment and is also sometimes intended to prevent the disease. In Korea, it refers to supra-gingival scaling, which is used as a non-surgical periodontal treatment aimed at preventing periodontal disease and treating early periodontitis through the removal of plaque and calculus, as well as reducing inflammation8., 9.. Since 2013, the government of South Korea has guaranteed insurance coverage for dental scaling procedures as a part of a national health policy objective to decrease the prevalence of periodontal disease and reduce health disparities. Guaranteed health insurance is one of the factors that can improve accessibility to health services by reducing the economic burden, thereby enabling universal access to medical and dental services10. Access to health care services is need-based and can be defined in several different ways11. Accessibility is defined as the opportunity, or the convenience of consumers or communities, to use appropriate services in proportion to their needs12., 13., whereas financial accessibility is defined as the relationship between the price of services and the willingness and ability of users to pay for the services without facing unfavourable economic consequences of health-related costs14.
In the past, the benefits of health insurance in Korea were limited to severe diseases, including disability or death. Recently, however, the scope of health insurance has expanded to include common diseases and diseases that impose a considerable social burden. As a result of the insurance coverage in Korea, the cost incurred by patients for dental scaling has markedly decreased. This policy was implemented with the aim of improving economic accessibility by reducing the patient-borne cost from a previous amount of $50 to approximately $10. It covers the use of the scaling service once a year for individuals older than 19 years nationwide. Furthermore, to avail of the guaranteed services, no preconditions are required. The dentist directly receives the patient’s contribution toward the cost and the remaining amount from the insurance company15.
According to a recent report on the outcomes of this insurance policy, the number of residents who underwent dental scaling increased by 10%16. However, scaling is more common in populations with higher incomes, education and occupational status, even after the introduction of insurance coverage17., 18.. Therefore, it is difficult to conclude that the increased rate of scaling use is solely a consequence of the dental insurance policy for preventive periodontal care or a reduction in health disparities.
To determine whether health insurance effectively lowers the economic ceiling and improves accessibility to dental services, it is necessary to determine whether the service use has increased in the entire population. However, this investigation alone is insufficient; it is also necessary to verify that dental service use has increased within the population that actually requires the services. Although the utilisation has increased following implementation of the new health insurance policy, the finding that the benefits of insurance are mainly utilised by individuals with higher incomes and education levels17., 19. suggests the presence of barriers to avail the services that have not yet been eliminated by current policies. The present study considered both factors, which are increased access to dental care and access by individuals who are in actual need of this service.
In this study, the hypothesis that the insurance policy improves treatment accessibility for individuals with actual need was tested. First, the effect of introducing dental insurance on the utilisation rates for middle-aged and elderly populations was assessed. Gingival bleeding is an early sign of periodontitis and represents a major risk indicator for the onset and progression of periodontitis20., 21.; therefore, the use of the scaling services by individuals with gingival bleeding and healthy gingiva was investigated to explore whether the use was for preventive purposes.
MATERIALS AND METHODS
This study was designed as a 5-year time series analysis using secondary data. Data extracted from the 2011, 2013 and 2015 Korean Community Health Surveys (CHSs), which were conducted by the Korea Centers for Disease Control and Prevention (KCDC), were analysed.
The KCDC uses a systematic researcher education system to minimise bias during the survey. In addition, the quality of data is carefully controlled through a regional monitoring system.
Community Health Surveys provide data that can be used to plan, implement, monitor and evaluate community health promotion and disease prevention programmes. The CHS standardised questionnaire was jointly developed by the KCDC staff, a health indicator standardisation subcommittee, and health officials from 16 metropolitan cities and provinces with 253 regional sites22. The KCDC conducts quality control test–retest procedures for the CHS questionnaires23.
Interview questionnaires are prepared based on common questionnaires and protocols, for 800–1,000 subjects, in the 253 public health centre regions nationwide, and are administered for 3 months, from August to October every year. Data are collected at the same time every year to facilitate yearly comparisons between the results. The August–October interval was selected because people working in the agriculture and fishery industries are relatively less busy and can spare time for the questionnaires during this period.
The primary sample units (PSUs) were the 253 public health centres across the Republic of Korea. Data were sampled in proportion to the sampling probability for each PSU, based on the number of households and the sample size; therefore, the data are representative of the national population. First, 253 counties were sampled by probability-proportional-to-size sampling. Then, households were sampled by systematic sampling, and family members ≥ 19 years old were included. The study was undertaken after explaining the details to the participants and obtaining their written consent. In accordance with ethical guidelines, the KCDC initiated data collection after a study review and approval by the institutional review board at the KCDC (2011-05CON-04-C, 2013-06EXP-01-3C) and the Institutional Review Board for Human Research, Yonsei University Wonju Severance Christian Hospital (CR317323). The research was conducted according to the Medical Association Declaration of Helsinki (version, 2008) and its later amendments.
A total of 659,614 participants were included, comprising 228,956 participants from the 2011 survey, 228,691 from the 2013 survey, and 228,039 from the 2015 survey.
The survey was conducted using face-to-face computer-assisted personal interviews. The survey was conducted by five–six interviewers in each area, and overall approximately 1,300 interviewers were engaged in conducting the nationwide survey. The interviewers were selected and trained according to strict criteria for each public health centre. The interviewers were retrained on receiving feedback that was based on the training results from KCDC training guidelines and programmes.
To confirm the reliability of the interview results, researchers from another survey institution randomly sampled and conducted phone interviews with 10% of participants within 3 days. These results were used as quality controls for the interviewers.
The primary dependent variable was the annual percentage of participants who underwent scaling (i.e. the utilisation rate of scaling services). This variable was derived by calculating the percentage of ‘yes’ responses to the question: ‘Have you received scaling in the last 1 year?’ Here, scaling referred to the removal of plaque, calculus, nicotine and stains from tooth surfaces, and did not include whitening.
The primary independent variable was self-reported periodontal symptoms. Participants were asked ‘How is your periodontal (gum) health?’ and were instructed to select the most severe of the following options: tooth mobility, swelling, calculus, bleeding and healthy gums. This question was adapted from the Community Periodontal Index of Treatment Needs (CPITN) scale24. The scores for the CPI are as follows25: 0, healthy periodontal condition; 1, gingival bleeding; 2, calculus and bleeding; 3, shallow periodontal pockets (4–5 mm); and 4, deep periodontal pockets (≥ 6 mm).
The reason for scaling was categorised as ‘prevention’ or ‘treatment’ according to the symptoms of each participant. While ‘healthy (1)’ and ‘gingival bleeding (2)’ were considered to require prevention, ‘calculus (2),’ ‘swelling (3)’ and ‘mobility (4)’ were considered to require treatment. The validity of self-reported symptoms is comparable to clinical examinations for assessing periodontal health26. Furthermore, when large-scale data, representative of community residents, are collected, self-reported questionnaires are economical and convenient; in addition, the subjective individual symptoms are more relevant to the use of dental services compared with the diagnoses of periodontal health by a dental clinician20., 27., 28.. Accordingly, use of a self-reported questionnaire is a valid method of analysis for this present study.
To examine trends in the utilisation rate of scaling services, the mean values between each year of the survey were compared. Descriptive statistics were calculated to determine the distribution of the dependent variable according to confounding variables. To analyse the relationships between scaling and self-reported periodontal symptoms (healthy/bleeding and mobility/swelling/calculus), t-tests and one-way ANOVA were used. To determine the odds ratios (ORs) for the utilisation rates of scaling services of middle-aged and elderly participants, multivariable logistic regression analysis of the effects on the independent variable relative to the 19–34-year-old population were performed, after adjusting for factors, including sex, age, education, income and occupational status, that are known to affect dental treatment utilisation29. The precision of these factors was determined based on 95% confidence intervals (CIs). The OR graph uses unweighted values to confirm the actual range of CIs. All statistical analyses were performed using PASW statistics ver. 23.0 (SPSS, Chicago, IL, USA). The type 1 error was 0.05.
RESULTS
In the 4 years after 2011, the utilisation rate of scaling services in the study sample increased by 12.3%. The increase of 8.7% from 2013 (33.9%) to 2015 (42.6%), after the introduction of dental insurance coverage, was greater than the increase of 3.6% from 2011 (30.3%) to 2013, before the coverage (P < 0.05).
With regard to age, the increase in the utilisation rate of scaling services from 2011 to 2015 was greater for participants ≥ 65 years (19.4%) and 45–64 years (12.9%) than for those 19–34 years (9.2%) and 35–44 years (9.5%). In particular, between 2013 and 2015 there was a considerable increase of 14.7% and 8.3% for participants ≥ 65 and 45–64 years old, respectively (P < 0.05).
For participants ≥ 65 and 44–64 years old, the increase in the utilisation rate of scaling services was greater after the introduction of insurance coverage (2013–2015: 14.7% and 8.3%, respectively) compared with before insurance coverage (2011–2013: 4.7% and 4.6%, respectively; Table 1).
Table 1.
Distribution and utilisation rates of scaling services according to demographic and socioeconomic characteristics in a Korean population between 2011 and 2015
| 2011 |
2013 |
2015 |
||||
|---|---|---|---|---|---|---|
| n (%) | Scaling services utilisation rate % ± SE | n (%) | Scaling services utilisation rate % ± SE | n (%) | Scaling services utilisation rate % ± SE | |
| Total | 228,956 | 30.3 ± 0.01 | 228,619 | 33.9 ± 0.01 | 202,039 | 42.6 ± 0.01 |
| Sex | ||||||
| Men | 102,930 (49.5) | 30.1 ± 0.01 | 102,675 (49.5) | 33.9 ± 0.01 | 92,629 (49.6) | 41.9 ± 0.01 |
| Women | 126,026 (50.5) | 30.5 ± 0.01 | 125,944 (50.5) | 34.0 ± 0.01 | 109,410 (50.4) | 43.3 ± 0.01 |
| Age (years)* | ||||||
| 19–34 | 43,382 (28.4) | 31.3 ± 0.01 | 41,016 (27.4) | 34.0 ± 0.01 | 39,843 (26.3) | 40.5 ± 0.01 |
| 35–44 | 44,032 (22.5) | 34.5 ± 0.01 | 40,495 (21.4) | 37.9 ± 0.01 | 37,888 (20.3) | 44.0 ± 0.01 |
| 45–64 | 85,084 (34.9) | 33.7 ± 0.01 | 85,673 (35.9) | 38.3 ± 0.01 | 83,040 (37.1) | 46.6 ± 0.01 |
| Over 65 | 56,458 (14.2) | 13.3 ± 0.01 | 61,435 (15.3) | 18.0 ± 0.01 | 41,268 (16.3) | 32.6 ± 0.02 |
| Occupation* | ||||||
| Professional administrative | 4,704 (2.7) | 44.3 ± 0.04 | 3,629 (2.1) | 50.4 ± 0.05 | 3,655 (2.2) | 55.3 ± 0.05 |
| Expert and office worker | 37,427 (22.3) | 40.9 ± 0.01 | 39,678 (23.8) | 43.2 ± 0.01 | 40,029 (24.1) | 50.3 ± 0.01 |
| Service and sales worker | 28,525 (13.7) | 32.9 ± 0.02 | 27,979 (13.8) | 36.6 ± 0.02 | 29,013 (14.5) | 43.4 ± 0.02 |
| Agriculture, forestry, fishery | 30,410 (4.4) | 15.6 ± 0.02 | 30,692 (4.3) | 18.7 ± 0.03 | 22,533 (3.9) | 29.4 ± 0.04 |
| Technical, labour, unemployed | 40,450 (19.5) | 27.0 ± 0.01 | 40,819 (19.3) | 30.7 ± 0.01 | 38,227 (19.3) | 39.0 ± 0.01 |
| Soldier, student, housewife | 56,823 (26.3) | 28.5 ± 0.01 | 54,828 (25.4) | 32.2 ± 0.01 | 45,482 (24.1) | 41.0 ± 0.01 |
| Not employed | 30,291 (11.1) | 18.4 ± 0.01 | 30,868 (11.3) | 22.4 ± 0.01 | 22,765 (11.9) | 34.4 ± 0.02 |
| Education* | ||||||
| Elementary | 61,509 (14.5) | 12.1 ± 0.01 | 60,258 (13.6) | 15.0 ± 0.01 | 37,600 (12.6) | 26.3 ± 0.02 |
| Middle | 26,851 (9.3) | 25.0 ± 0.02 | 26,154 (8.9) | 29.0 ± 0.02 | 22,296 (8.5) | 38.2 ± 0.02 |
| High | 67,134 (31.4) | 29.9 ± 0.01 | 65,505 (30.4) | 34.1 ± 0.01 | 62,423 (30.1) | 40.7 ± 0.01 |
| College | 72,987 (44.8) | 37.6 ± 0.01 | 76,433 (47.1) | 40.3 ± 0.01 | 79,422 (48.8) | 47.5 ± 0.01 |
| Monthly income ($)* | ||||||
| under 1,000 | 47,653 (14.8) | 16.2 ± 0.01 | 45,036 (12.8) | 18.5 ± 0.01 | 33,657 (12.0) | 27.9 ± 0.02 |
| 1,001–2,000 | 37,492 (18.2) | 29.2 ± 0.01 | 34,141 (15.4) | 29.0 ± 0.01 | 33,281 (13.6) | 36.4 ± 0.02 |
| 2,001–3,000 | 33,469 (19.2) | 31.0 ± 0.01 | 32,992 (17.2) | 33.2 ± 0.01 | 39,472 (19.2) | 39.5 ± 0.01 |
| 3,001–4,000 | 19,945 (12.5) | 33.8 ± 0.02 | 21,327 (12.1) | 36.7 ± 0.02 | 35,015 (19.0) | 43.1 ± 0.01 |
| Over 4,001 | 72,831 (35.3) | 37.1 ± 0.01 | 87,316 (42.5) | 40.0 ± 0.01 | 58,561 (36.2) | 49.9 ± 0.01 |
n (%) denotes actual n (weighted %). Mean ± SE denotes weighted %.
P < 0.001.
As shown in Table 2 and Figure 1, the utilisation rate of scaling services was the highest for healthy participants (71.1%–73.5%), followed by that for those with gingival bleeding (9.9%–10.2%). Participants with tooth mobility had the lowest utilisation rate for scaling services (3.0%–3.3%).
Table 2.
Utilisation rates of scaling services (%) according to self-reported periodontal symptoms in a Korean population between 2011 and 2015
| 2011 |
2013 |
2015 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mobility | Swelling | Calculus | Bleeding | Normal | Mobility | Swelling | Calculus | Bleeding | Normal | Mobility | Swelling | Calculus | Bleeding | Normal | |
| Total | 3.0 | 9.0 | 4.3 | 10.2 | 73.5 | 3.0 | 9.0 | 4.7 | 10.0 | 73.3 | 3.3 | 9.5 | 6.2 | 9.9 | 71.1 |
| Sex* | |||||||||||||||
| Men | 3.7 | 8.0 | 5.2 | 9.9 | 73.2 | 3.5 | 8.0 | 5.9 | 9.8 | 72.8 | 4.1 | 8.0 | 7.6 | 10.0 | 70.3 |
| Women | 2.4 | 10.0 | 3.4 | 10.5 | 73.8 | 2.5 | 9.9 | 3.6 | 10.2 | 73.8 | 2.5 | 10.9 | 4.9 | 9.8 | 71.9 |
| Age (years)* | |||||||||||||||
| 19–34 | 0.6 | 6.6 | 5.2 | 12.5 | 75.1 | 0.4 | 6.7 | 5.9 | 12.9 | 74.1 | 0.7 | 7.5 | 7.4 | 12.2 | 72.2 |
| 35–44 | 2.5 | 8.8 | 5.0 | 10.7 | 73.0 | 1.8 | 9.2 | 5.5 | 10.7 | 72.8 | 2.0 | 9.2 | 7.7 | 10.8 | 70.3 |
| 45–64 | 4.8 | 10.7 | 3.5 | 8.5 | 72.7 | 4.8 | 10.1 | 4.0 | 8.1 | 73.0 | 5.0 | 10.7 | 5.4 | 8.4 | 70.5 |
| Over 65 | 6.1 | 11.2 | 1.8 | 7.7 | 73.2 | 5.8 | 10.7 | 2.2 | 7.7 | 73.6 | 6.1 | 10.5 | 2.9 | 7.3 | 73.2 |
| Occupation* | |||||||||||||||
| Professional administrative | 3.5 | 9.2 | 3.8 | 8.8 | 74.8 | 4.0 | 9.2 | 4.2 | 8.4 | 74.2 | 3.3 | 9.2 | 6.6 | 8.0 | 72.8 |
| Expert and office worker | 1.7 | 7.4 | 4.8 | 9.5 | 76.5 | 1.5 | 7.7 | 5.1 | 10.2 | 75.5 | 1.9 | 8.4 | 6.7 | 9.9 | 73.1 |
| Service and sales worker | 3.1 | 9.8 | 4.0 | 11.5 | 71.5 | 3.0 | 9.3 | 5.5 | 10.0 | 72.2 | 2.9 | 10.3 | 5.9 | 9.8 | 71.0 |
| Agriculture, forestry, fishery | 4.7 | 11.4 | 3.0 | 9.4 | 71.5 | 6.0 | 9.7 | 3.7 | 9.6 | 71.0 | 6.7 | 9.5 | 5.0 | 10.1 | 68.7 |
| Technical, labour, unemployed | 5.0 | 10.1 | 5.3 | 11.0 | 68.5 | 4.8 | 9.4 | 5.2 | 10.3 | 70.2 | 5.4 | 10.1 | 7.4 | 11.3 | 65.9 |
| Soldier, student, housewife | 2.5 | 9.4 | 3.3 | 10.4 | 74.4 | 2.6 | 9.8 | 3.7 | 9.8 | 74.1 | 2.7 | 10.0 | 4.8 | 9.4 | 73.1 |
| Not employed | 4.8 | 9.8 | 3.8 | 8.2 | 73.3 | 4.4 | 9.5 | 4.3 | 10.2 | 71.6 | 5.3 | 8.9 | 6.4 | 9.0 | 70.4 |
| Education* | |||||||||||||||
| Elementary school | 7.5 | 14.1 | 2.5 | 11.2 | 64.8 | 7.1 | 12.6 | 3.2 | 10.8 | 66.4 | 7.9 | 12.5 | 3.8 | 10.6 | 65.2 |
| Middle school | 6.2 | 12.1 | 3.2 | 11.4 | 67.2 | 6.2 | 11.3 | 3.6 | 9.8 | 69.1 | 5.6 | 11.7 | 5.0 | 10.0 | 67.6 |
| High school | 3.6 | 10.0 | 4.4 | 10.4 | 71.6 | 3.8 | 9.7 | 4.5 | 9.8 | 72.2 | 4.3 | 10.8 | 6.0 | 9.6 | 69.2 |
| College | 1.8 | 7.5 | 4.5 | 9.8 | 76.4 | 1.6 | 7.8 | 5.2 | 10.1 | 75.3 | 2.0 | 8.2 | 6.7 | 9.9 | 73.2 |
| Monthly income ($)* | |||||||||||||||
| Under 1,000 | 4.9 | 11.7 | 3.6 | 11.7 | 68.4 | 5.6 | 12.0 | 4.4 | 10.9 | 67.2 | 6.4 | 2.0 | 5.3 | 10.4 | 65.9 |
| 1,001–2,000 | 3.8 | 9.7 | 4.1 | 11.5 | 70.9 | 3.7 | 9.8 | 4.7 | 10.7 | 71.1 | 4.4 | 11.7 | 5.8 | 10.3 | 67.9 |
| 2,001–3,000 | 2.9 | 9.5 | 4.4 | 10.6 | 72.6 | 2.8 | 9.3 | 5.0 | 10.6 | 72.4 | 3.6 | 10.0 | 6.5 | 10.5 | 69.4 |
| 3,001–4,000 | 2.6 | 8.6 | 4.5 | 10.5 | 73.8 | 2.8 | 9.4 | 4.9 | 10.3 | 72.7 | 3.2 | 8.9 | 6.5 | 10.0 | 71.5 |
| Over 4,001 | 2.5 | 8.3 | 4.2 | 9.4 | 75.6 | 2.4 | 8.2 | 4.7 | 9.4 | 75.2 | 2.5 | 8.6 | 6.3 | 9.4 | 73.3 |
Utilisation rate of scaling services denotes weighted %.
P < 0.001.
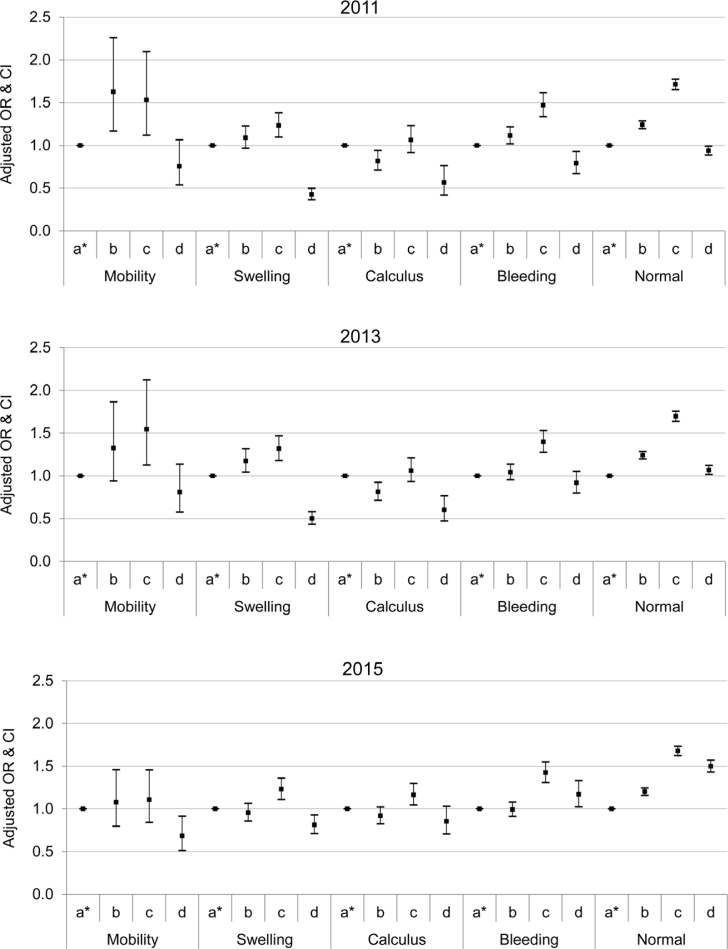
Figure 1.
Findings of the multivariable logistic regression analysis according to self-reported periodontal symptoms in a Korean population between 2011 and 2015. OR, unweighted, adjusted odds ratio (sex, age, income, education, occupation); CI, 95% confidence interval. Statistically significant based on the multivariable regression analysis. a* (ref): 19–34 years; b: 35–44 years; c: 45–64 years; d: 65+ years.
The ORs for the utilisation rate of scaling services by age category according to self-reported periodontal symptoms were calculated. The likelihood of using scaling (OR) increased for participants ≥ 65 years old in 2013 and 2015. There was no notable change for participants who were 44–64 years old (Figure 1).
The utilisation rate of scaling services for healthy participants ≥ 65 years old increased after 2013. Compared with the 19–34-year-old group, the healthy elderly group exhibited ORs of 0.9 (CI: 0.88–0.99), 1.1 (CI: 1.01–1.12) and 1.5 (CI: 1.43–1.57) for scaling utilisation in 2011, 2013 and 2015, respectively. For elderly participants with gingival bleeding, the utilisation rate of scaling services increased after 2015 with ORs of 0.8 (CI: 0.67–0.92), 0.9 (CI: 0.7–1.0) and 1.2 (CI: 1.02–1.33) for 2011, 2013 and 2015, respectively (P < 0.05).
For healthy participants 44–64 years old, the utilisation rate of scaling services was similar in 2011 (OR: 1.7, CI: 1.65–1.77), 2013 (OR: 1.7, CI: 1.63–1.75) and 2015 (OR: 1.7, CI: 1.62–1.73). Similar findings were observed for middle-aged participants with gingival bleeding [2011 (OR: 1.4, CI: 1.33–1.61), 2013 (OR: 1.4, CI: 1.27–1.53) and 2015 (OR: 1.4, CI: 1.31–1.55)].
For both elderly and middle-aged participants, there was no difference between men and women with respect to the utilisation rate of scaling services according to self-reported periodontal symptoms (P > 0.05).
DISCUSSION
This study evaluated the trends in the utilisation rate of scaling services before and after the introduction of insurance coverage for dental scaling, and assessed the influence of this access on preventive periodontal care utilisation. After the introduction of the insurance coverage, the utilisation rates of scaling services increased for the middle-aged and elderly populations, who are at higher risk for periodontal disease; according to the analyses, the utilisation rate increased considerably for elderly participants with healthy gingiva or gingival bleeding. These results are consistent with the interpretation that dental insurance contributed, at least in part, to improved accessibility to preventive periodontal care. The fact that participants with healthy gingiva or gingival bleeding exhibited increased utilisation of the service can be interpreted as overuse or the moral hazards of insurance coverage; however, if the objective of a health insurance policy is to improve accessibility to health services, then its fundamental goal has been achieved.
The use of scaling services increased during the study period. However, this may not be the result of expanding health insurance services. The prevalence of periodontal disease has been gradually increasing in Korea30. The elderly population has also increased, which may have affected the study results. Despite the implication of an increase in scaling services due to both these reasons, this study aimed to examine whether the scaling services covered by the health insurance policy were used as a preventative measure in line with its purpose, the prevention of periodontal care. The fact that patients with this symptom exhibited increased utilisation of scaling services is sufficient evidence of utilisation of the services for preventive purposes31.
In the present study, we initially examined whether the utilisation rate of scaling services increased after the implementation of dental insurance coverage. Then, with a focus on patients who should be using the service, we assessed whether the utilisation rate of services had increased for the middle-aged and elderly patients. Finally, the influence of dental insurance coverage on access to preventive periodontal care was explored. We also investigated whether scaling services were accessed more often by individuals with gingival bleeding or healthy gingiva, compared with those with more advanced symptoms. The interpretation of the results rests on the assumption that bleeding is always an early sign of periodontitis.
A subgroup analysis exploring differences in the utilisation rate of scaling services by age group and periodontal symptoms yielded that both age and periodontal symptoms were associated with differences in the utilisation rates, which had increased after the introduction of insurance coverage for scaling services. In particular, the utilisation rate of scaling services was increased for the middle-aged and elderly patients with healthy gingiva or gingival bleeding.
It was confirmed that dental insurance coverage resulted in increased use of services to prevent periodontal disease and that these services were being accessed by the individuals in need of such procedures. From 2011 to 2015, the utilisation rate of scaling services for the study cohorts ≥ 65 and 44–64 years old increased by 14.7% and 8.3%, respectively. Thus, a considerable increase in utilisation by the middle-aged and elderly groups can be considered as an encouraging result; this finding indicates that coverage yields increased access by middle-aged and elderly patients who are at higher risk for periodontal disease (Table 1).
The fact that the utilisation rate of scaling services increased more for middle-aged and elderly patients than for younger patients can be interpreted as evidence for the increasing interest in periodontal disease prevention among middle-aged and elderly patients, as well as a change in health behaviour related to periodontal disease control. However, scaling treatment in middle-aged and elderly patients can lead to further periodontal treatment, resulting in increased dental insurance expenditures. Therefore, the earlier use of scaling services by younger individuals with healthy periodontal tissue should be encouraged as a preventive health measure. Furthermore, individuals should be instructed not to overlook early symptoms, such as gingival bleeding.
The finding that insurance coverage improved access to dental services is consistent with the findings of case studies conducted outside Korea32. When insurance coverage is guaranteed, community residents with disease or symptoms can visit the hospital without experiencing a financial burden10. Moreover, due to increase in screening the cancer detection rate has increased, including detection of cancers in women33., 34., 35.. In addition, dentist visits increase when dental insurance coverage is guaranteed36., 37.; however, opposite findings have also been reported. Insurance coverage does not improve accessibility or financial protection against catastrophic expenditures. However, compared with uninsured households, insured households do have greater accessibility38.
The increase in the utilisation rates of scaling services for the middle-aged and elderly patients was expected. The prevalence of periodontal disease increases between 45 and 64 years old39., 40.; therefore, the increased utilisation rates of scaling services can be interpreted as evidence of increased interest in periodontal disease for patients in this age range41. Moreover, the increased utilisation rates of scaling services in elderly patients ≥ 65 years old can be explained by the increased utilisation of dental services by the elderly. In Korea, insurance coverage has been provided since 2012 for dental implants and denture treatment in patients ≥ 75 years old42, and was extended in 2017 to patients ≥ 65 years old, which is thought to have resulted in a gradual increase in dentist visits by elderly patients. Further evidence is provided by the fact that the OR of 0.9 for scaling services utilisation in 2011 had increased to 1.5 by 2015.
For participants with healthy gingiva or gingival bleeding, the increased utilisation rates of scaling services after the implementation of insurance coverage can be interpreted in two different ways. From a positive perspective, increased interest in periodontal disease among elderly patients may have increased the use of dental services, thereby resulting in increased accessibility to appropriate services for the individuals in need. From a negative perspective, the utilisation may have increased as a result of use by individuals with good periodontal health (who were already using dental services) for preventive care, which could represent overuse or moral hazards.
Generally, individuals with high perceived susceptibility are more interested in their health, so they more frequently use services to prevent periodontal disease43. However, participants with tooth mobility, swelling or calculus would also receive scaling treatment as a preliminary procedure before periodontal treatment. Therefore, scaling for these participants is a component of periodontal treatment rather than a preventive care measure. These individuals are more likely to show less dental treatment use compared with healthy individuals without severe periodontal symptoms for reasons that include financial burden, lack of awareness regarding disease severity and dental phobias44. The use of scaling when the periodontal tissue is still healthy or when gingivitis is relatively mild is important for preventing periodontal disease20., 31.. Accordingly, education and awareness regarding the symptoms of periodontal disease, such as bleeding, are important to increase the perceived susceptibility of middle-aged and elderly populations.
In this study, it was found that dental insurance coverage positively influenced access to preventive periodontal care in the middle-aged and elderly participants. However, verification of whether access to these services was redundant as a result of skewing toward a specific population was not possible. Therefore, it cannot be definitively concluded that dental insurance effectively contributes to improved access. Improved assessments of the effectiveness of insurance coverage could be accomplished by eliminating disparities in health care accessibility and determining equality in access, prior to discussing the effectiveness of health insurance coverage.
The present study has some limitations. First, self-reported data based on scaling services used in the previous year and current self-reported periodontal symptoms were analysed; therefore, response or interviewer bias may have been introduced45. Moreover, surveys conducted through 1:1 face-to-face interviews have a large impact on the quality of the data. It is possible that interviewer bias or common human error impacted the results, despite quality control measures.
Next, the use of cross-sectional data is a limitation. Whether symptoms developed after scaling or were present before scaling was not determined. It is also unknown whether the patient independently requested scaling or if the dentist recommended it. Moreover, the means of measurement may change over time, and parts of documents may be missing or be non-representative; these are a few of the limitations of using secondary data.
Third, the CHS data did not include a cohort sample; therefore, the follow-up results did not follow the same sample. Additionally, access to dental care, which may vary from year to year, was not considered. And, only increased utilisation of dental services and access to the required service (preventive scaling) for populations in need (middle-aged and elderly adults) was considered; therefore, it was not possible to evaluate any inequality in access to services or determine whether a service was fairly distributed. Determination in retrospect, and based on patient self-reports, whether scaling was used for prevention or treatment can also be flawed.
Finally, we did not include individuals who do not use scaling services or their reasons for the non-use; this is a major limitation of the study and cannot be easily addressed. Further research is required to address this. Moreover, it is difficult to isolate insurance coverage as the only affecting factor. However, the purpose of this study was to focus on the periodontal symptoms of the individuals using scaling services. Specifically, for individuals with complaints such as bleeding or calculus, scaling is used for the prevention of periodontal disease, while in people with complaints of periodontal symptoms, such as swelling or mobility, scaling is considered as periodontal care.
Despite these limitations, this study contributes to the literature because it used 5-year Korean CHS data, which are representative of the national population, to demonstrate that dental insurance coverage has a positive effect on access to preventive periodontal care in middle-aged and elderly adults.
CONCLUSION
A positive association of insurance coverage for dental scaling with access to preventive care for periodontal disease in middle-aged and elderly Koreans was established. Subsequent studies should evaluate the long-term contributions of dental insurance coverage to reductions in the prevalence of periodontal disease in association with preventive care and reduction in oral health disparities.
Acknowledgements
This study was supported by the KCDC Research Fund (Grant no.: Pyeongchang-gun 2016-51-0033, Wonju City 2016-51-0034, Taebaek City 2016-51-0035, Hongcheon-gun 2016-51-0022, Hoengseong-gun 2016-51-0037, Yeongwol-gun 2016-51-0036, and Jeongseon-gun 2016-51-0023).
Conflict of interest
The authors have no conflicts of interest in connection with this article.
References
- 1.Holde GE, Oscarson N, Trovik TA, et al. Periodontitis prevalence and severity in adults: A cross-sectional study in Norwegian circumpolar communities. J Periodontol. 2017;88:1012–1022. doi: 10.1902/jop.2017.170164. [DOI] [PubMed] [Google Scholar]
- 2.Tonetti MS, Jepsen S, Jin L, et al. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol. 2017;44:456–462. doi: 10.1111/jcpe.12732. [DOI] [PubMed] [Google Scholar]
- 3.Kapellas K, Maple-Brown LJ, Jamieson LM, et al. Effect of periodontal therapy on arterial structure and function among aboriginal Australians: a randomized, controlled trial. Hypertension. 2014;64:702–708. doi: 10.1161/HYPERTENSIONAHA.114.03359. [DOI] [PubMed] [Google Scholar]
- 4.Kjellstrom B, Ryden L, Klinge B, et al. Periodontal disease – important to consider in cardiovascular disease prevention. Expert Rev Cardiovasc Ther. 2016;14:987–989. doi: 10.1080/14779072.2016.1202112. [DOI] [PubMed] [Google Scholar]
- 5.Preshaw PM, Alba AL, Herrera D, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55:21–31. doi: 10.1007/s00125-011-2342-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gil-Montoya JA, de Mello AL, Barrios R, et al. Oral health in the elderly patient and its impact on general well-being: a nonsystematic review. Clin Interv Aging. 2015;10:461–467. doi: 10.2147/CIA.S54630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaziri F, Haerian A, Morowati MA, et al. Oral health-related quality of life and severity of periodontal disease. J Int Oral Health. 2016;8:440–444. [Google Scholar]
- 8.Heitz-Mayfield LJ, Trombelli L, Heitz F, et al. A systematic review of the effect of surgical debridement vs non-surgical debridement for the treatment of chronic periodontitis. J Clin Periodontol. 2002;29(Suppl 3):92–102. doi: 10.1034/j.1600-051x.29.s3.5.x. discussion 160–162. [DOI] [PubMed] [Google Scholar]
- 9.Claffey N, Polyzois I, Ziaka P. An overview of nonsurgical and surgical therapy. Periodontol 2000. 2004;36:35–44. doi: 10.1111/j.1600-0757.2004.00073.x. [DOI] [PubMed] [Google Scholar]
- 10.Philip NE, Kannan S, Sarma SP. Utilization of comprehensive health insurance scheme, Kerala: A comparative study of insured and uninsured below-poverty-line households. Asia Pac J Public Health. 2016;28:77S–85S. doi: 10.1177/1010539515602306. [DOI] [PubMed] [Google Scholar]
- 11.Campbell SM, Roland MO, Buetow SA. Defining quality of care. Soc Sci Med. 2000;51:1611–1625. doi: 10.1016/s0277-9536(00)00057-5. [DOI] [PubMed] [Google Scholar]
- 12.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peters DH, Garg A, Bloom G, et al. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- 15.Korea National Health Insurance Service. Insurance benefits: Dental scaling. Available from: https://minwon.nhis.or.kr/static/html/wbma/c/wbmac0218.html. Accessed 18 September 2018
- 16.Jang YE, Kim CB, Kim NH. Utilization of preventive dental services before and after health insurance covered dental scaling in Korea: 2009 to 2014 community health Survey. Asia Pac J Public Health. 2017;29:70–80. doi: 10.1177/1010539516684944. [DOI] [PubMed] [Google Scholar]
- 17.Park HJ, Lee JH, Park S, et al. Changes in dental care access upon health care benefit expansion to include scaling. J Periodontal Implant Sci. 2016;46:405–414. doi: 10.5051/jpis.2016.46.6.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nasseh K, Vujicic M. The impact of medicaid reform on children’s dental care utilization in Connecticut, Maryland, and Texas. Health Serv Res. 2015;50:1236–1249. doi: 10.1111/1475-6773.12265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moeller J, Quinonez C. The association between income inequality and oral health in Canada: A cross-sectional study. Int J Health Serv. 2016;46:790–809. doi: 10.1177/0020731416635078. [DOI] [PubMed] [Google Scholar]
- 20.Airila-Månsson S, Bjurshammar N, Yakob M, et al. Self-reported oral problems, compared with clinical assessment in an epidemiological study. Int J Dent Hyg. 2007;5:82–86. doi: 10.1111/j.1601-5037.2007.00231.x. [DOI] [PubMed] [Google Scholar]
- 21.Tonetti MS, Chapple IL, Jepsen S, et al. Primary and secondary prevention of periodontal and peri-implant diseases: Introduction to, and objectives of the 11th European Workshop on Periodontology consensus conference. J Clin Periodontol. 2015;42(Suppl 16):S1–S4. doi: 10.1111/jcpe.12382. [DOI] [PubMed] [Google Scholar]
- 22.Kang YW, Ko YS, Kim YJ, et al. Korea community health survey data profiles. Osong Public Health Res Perspect. 2015;6:211–217. doi: 10.1016/j.phrp.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim SJ, Han JA, Kim YH, et al. Test-retest reliability of health behavior items in the Community Health Survey in South Korea. Epidemiol Health. 2015;37:e2015045. doi: 10.4178/epih/e2015045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cutress TW, Ainamo J, Sardo-Infirri J. The community periodontal index of treatment needs (CPITN) procedure for population groups and individuals. Int Dent J. 1987;37:222–233. [PubMed] [Google Scholar]
- 25.World Health Organization . 5th edn. WHO Press; Geneva, Switzerland: 2013. Oral Health Surveys: Basic Methods; p. 127. [Google Scholar]
- 26.Page LAF, Thomson WM, Broadbent JM. Validity of self-reported periodontal questions in a New Zealand cohort. Clin Oral Investig. 2016;20:563–569. doi: 10.1007/s00784-015-1526-0. [DOI] [PubMed] [Google Scholar]
- 27.Blicher B, Joshipura K, Eke P. Validation of self-reported periodontal disease: a systematic review. J Dent Res. 2005;84:881–890. doi: 10.1177/154405910508401003. [DOI] [PubMed] [Google Scholar]
- 28.Garcia-Perez A, Borges-Yanez SA, Jimenez-Corona A, et al. Self-report of gingival problems and periodontitis in indigenous and non-indigenous populations in Chiapas, Mexico. Int Dent J. 2016;66:105–112. doi: 10.1111/idj.12213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bakeera SK, Wamala SP, Galea S, et al. Community perceptions and factors influencing utilization of health services in Uganda. Int J Equity Health. 2009;8:25. doi: 10.1186/1475-9276-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee JH, Lee JS, Choi JK, et al. National dental policies and socio-demographic factors affecting changes in the incidence of periodontal treatments in Korean: a nationwide population-based retrospective cohort study from 2002–2013. BMC Oral Health. 2016;16:118–126. doi: 10.1186/s12903-016-0310-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jepsen S, Blanco J, Buchalla W, et al. Prevention and control of dental caries and periodontal diseases at individual and population level: consensus report of group 3 of joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. 2017;44:S85–S93. doi: 10.1111/jcpe.12687. [DOI] [PubMed] [Google Scholar]
- 32.Kennedy J, Morgan S. Health care access in three nations: Canada, insured America, and uninsured America. Int J Health Serv. 2006;36:697–717. doi: 10.2190/EC30-KP22-RA84-RAL4. [DOI] [PubMed] [Google Scholar]
- 33.Smith MA, Weiss JM, Potvien A, et al. Insurance coverage for CT colonography screening: Impact on overall colorectal cancer screening rates. Radiology. 2017;284:717–724. doi: 10.1148/radiol.2017170924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bitler MP, Carpenter CS. Effects of state cervical cancer insurance mandates on pap test rates. Health Serv Res. 2017;52:156–175. doi: 10.1111/1475-6773.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peppercorn J, Houck K, Beri N, et al. Breast cancer screening utilization and understanding of current guidelines among rural US women with private insurance. Breast Cancer Res Treat. 2015;153:659–667. doi: 10.1007/s10549-015-3566-1. [DOI] [PubMed] [Google Scholar]
- 36.Teusner D, Smith V, Gnanamanickam E, et al. Examining dental expenditure and dental insurance accounting for probability of incurring expenses. Community Dent Oral Epidemiol. 2017;45:101–111. doi: 10.1111/cdoe.12264. [DOI] [PubMed] [Google Scholar]
- 37.Kreider B, Manski RJ, Moeller J, et al. The effect of dental insurance on the use of dental care for older adults: a partial identification analysis. Health Econ. 2015;24:840–858. doi: 10.1002/hec.3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bodhisane S, Pongpanich S. The impact of community based health insurance in enhancing better accessibility and lowering the chance of having financial catastrophe due to health service utilization: A case study of Savannakhet province, Laos. Int J Health Serv. 2017;47:504–518. doi: 10.1177/0020731415595609. [DOI] [PubMed] [Google Scholar]
- 39.Emrich LJ, Shlossman M, Genco RJ. Periodontal disease in non-insulin-dependent diabetes mellitus. J Periodontol. 1991;62:123–131. doi: 10.1902/jop.1991.62.2.123. [DOI] [PubMed] [Google Scholar]
- 40.Eke PI, Page RC, Wei L, et al. Update of the case definitions for population-based surveillance of periodontitis. J Periodontol. 2012;83:1449–1454. doi: 10.1902/jop.2012.110664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee HJ, Han DH. Early-life socioeconomic position and periodontal status in Korean adults. Community Dent Oral Epidemiol. 2016;44:11–23. doi: 10.1111/cdoe.12184. [DOI] [PubMed] [Google Scholar]
- 42.Korea National Health Insurance Service . National Health Insurance Service; Wonju, Korea: 2017. Benefits by subject for elderly aged over 65, dentures implant fees. Available from: http://medicare1.nhis.or.kr/hongbo/static/html/minisite/sub/bj01_3.html. Accessed 18 September 2018. [Google Scholar]
- 43.Janz NK, Becker MH. The health belief model: A decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 44.Chae S, Lee Y, Kim J, et al. Factors associated with perceived unmet dental care needs of older adults. Geriatr Gerontol Int. 2017;17:1936–1942. doi: 10.1111/ggi.12997. [DOI] [PubMed] [Google Scholar]
- 45.Peersman W, Pasteels I, Cambier D, et al. Validity of self-reported utilization of physician services: a population study. Eur J Public Health. 2014;24:91–97. doi: 10.1093/eurpub/ckt079. [DOI] [PubMed] [Google Scholar]