BACKGROUND
Dental caries has become a ubiquitous public health problem despite overwhelming evidence that it is preventable1., 2.. Petersen reported that virtually all populations are affected globally, with 60%–90% of school-going children and most adults affected by this condition1. Dental caries is a disease of the dental hard tissues characterised primarily by demineralisation following production of acid through the fermentation of carbohydrates by oral bacteria, as described in Keyes’ triad. Left untreated, caries progresses to pulpitis, a painful condition warranting emergency intervention. Conventionally, the treatment modality for caries has been through elimination of affected tooth structure and placement of direct and indirect restorations3.
An ideal restorative material should be biocompatible, resistant to fracture, demonstrate longevity, be affordable and easy to manipulate, even in a resource-strained environment4. In low- and middle-income (LMI) countries, lack of prioritisation of oral health as a result of its often morbid, but not fatal, nature, and in the face of limited resources, typically means minimal investment in the infrastructure necessary for advanced restorative treatment. In such countries, conventional caries treatment is not readily available and the ensuing alternative is extraction to provide immediate relief of symptoms; the partially dentate or completely edentulous state following tooth mortality is associated with reduced quality of life1., 2..
Dental amalgam is one of the oldest direct dental restorative materials, its use spanning more than a century. Amalgam is an alloy of a powder comprising silver, tin and copper triturated with triple distilled mercury into a soft pliable mass which is condensed into a cavity and carved, prior to setting, to a rigid solid. Dental amalgam has several advantages. It has adequate compressive strength of more than 400 MPa, is inexpensive and is easy to manipulate. It is also radiopaque and exhibits self-sealing ability as a result of corrosion products. However, its disadvantages include its metallic appearance as well as its tendency to corrode in the oral cavity, which renders it unaesthetic. Additionally, dental amalgam is brittle in tension and is not adhesive and therefore requires extensive tooth preparation to ensure mechanical retention and adequate bulk to prevent fracture.
Moreover, silver–mercury amalgam is a mercury-based product and is now scheduled to be phased down following the Minamata Convention on Mercury in 2013. The Convention is a global treaty whose agenda seeks to reduce environmental impact from mercury waste through phase-out of mercury-based products and cessation of manufacture of mercury. Although there is no proof of any adverse reactions in humans from dental amalgam, mercury is a well-known toxic substance and precaution is mandatory when handling it in the dental surgery. The looming phase-down of dental amalgam by 2020 presents a challenge to the dental profession5. Apart from its remarkable compressive strength, silver–mercury amalgam is one of the simplest to use and affordable restorative materials, making it readily accessible. The phase-down of dental amalgam is likely to hinder access to affordable restorative dental treatment in LMI countries3. Therefore, there is an urgent need to find an alternative with minimal adverse environmental impact that offers the excellent properties that characterise amalgam4.
This commentary addresses the global burden of dental caries and inequalities that exist in LMI countries, such as Kenya. It highlights the challenges of disease management, which are expected to worsen during the imminent phase-down of dental amalgam, and proposes practical and cost-effective solutions. The intent is to increase awareness by urging a paradigm shift that requires curriculum review in dental schools to promote disease prevention and further research on restorative alternatives. The articles included were accessed through a systematic search on PubMed and Google Scholar using the specified keywords. A manual search of gray literature was also performed for additional articles.
CURRENT CONCEPTS FOR MANAGING DENTAL CARIES
Restorative, or conservative, dentistry traditionally involves placement of restorations to prevent tooth loss by extraction; however, despite advances in restorative dentistry, the greatest challenge remains to find the ideal biomimetic material that can match the properties of hard dental tissues4., 6.. Navigating biocompatibility and environmental impact concerns in the quest for equivalence or superiority to established materials renders the process of biomaterial development tedious and costly. This financial burden is eventually transferred to patients, restricting access to advanced restorative treatment options.
Furthermore, prevention and minimal intervention dentistry are widely accepted concepts for the management of dental caries. Preventive dentistry programmes focussing on risk factors have proven effective in developed countries1., 2.. However, the majority of developing countries do not have preventive dentistry programmes2. This is mostly because of financial constraints in an environment where public health agendas of various stakeholders often conflict. Despite the fact that disease prevention is ultimately more economical than treatment, limited resources have led to a scenario in which oral health is largely ignored when tackling other chronic non-communicable and communicable diseases perceived to have a higher risk of mortality1., 2.. There is a lack of strategies and goodwill to invest in and implement oral health promotion and disease prevention. In Kenya, health care consumes only 8% of total Government expenditure; oral health falls under the umbrella of general health, receiving a meagre 0.0016% of overall health-care budgetary allocation.
Minimal intervention dentistry (MID) is a more recent, patient-specific treatment. It is a comprehensive longitudinal approach towards prevention through risk assessment while minimising operative intervention7. Proponents of MID suggest that ‘extension for prevention’ should be replaced by ‘prevention of extension’, arguing that the conservative goals of the former are questionable because of the surgical approach to remove diseased tissue before placement of a restoration. Preventive dentistry, atraumatic restorative treatment (ART) and adhesive dentistry are practical aspects of MID, with the ultimate goal of preventing or halting progression of disease8.
Minimising the need for intervention by arresting disease progression is cost-effective; a key advantage of approaches such as ART and silver diamine fluoride is their simplicity as well as affordability, making them practical in resource-strained settings. However, in Kenya, the dental education curriculum focusses on curative, rather than preventive, training. Often, these techniques are considered intermediary interventions until the patient can access definitive treatment. Dental amalgam is still the preferred posterior restorative material in LMI countries such as Kenya; therefore, it is anticipated that its phase-down will present challenges in oral health-care service delivery.
CHALLENGES PRESENTED BY THE MINAMATA CONVENTION REGARDING AMALGAM UTILISATION AND POSSIBLE SOLUTIONS FOR LMI COUNTRIES
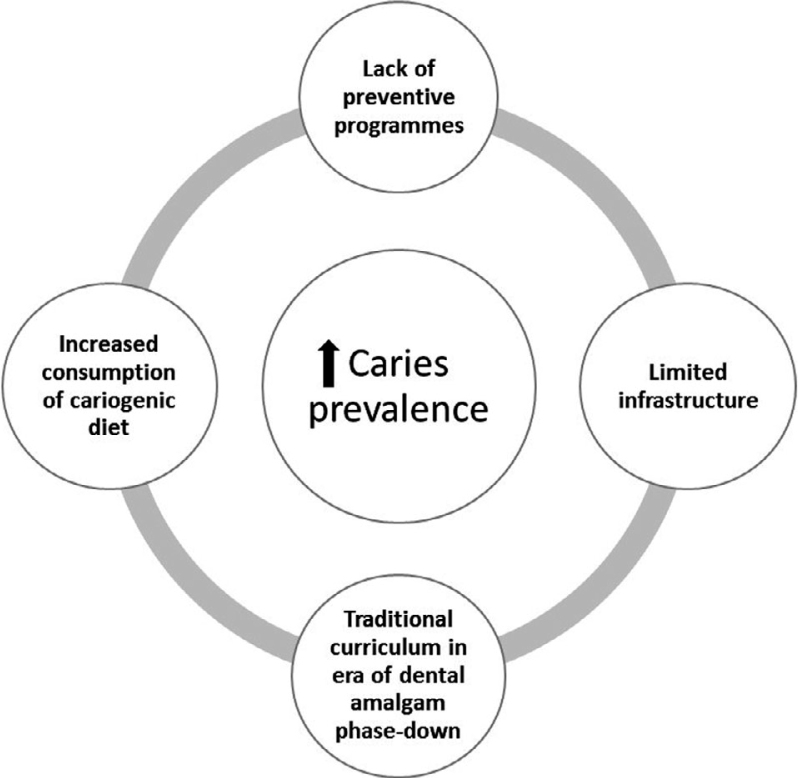
Kenya and a number of LMI countries are signatories to the Minamata Convention on Mercury5., 6.. The consequence of this policy in regard to restorative dentistry in these countries should be a matter of concern. Faced with rising caries prevalence due to a number of factors (Figure 1), they are neither economically positioned nor (in terms of infrastructure) prepared to adopt alternative materials and procedures, the majority of which require a reliable source of electricity or technology not available in these resource-poor countries4.
Figure 1.
Challenges faced by low- and middle-income (LMI) countries in addressing the burden of dental caries.
The first challenge presented by the dental amalgam phase-down is the lack of caries-prevention initiatives in LMI countries which, coupled with a corresponding rise in the prevalence of dental caries, has increased the need for restorative treatment. Economic and infrastructural limitations demand that immediate efforts should be channelled towards disease prevention. The consensus is that prevention is the best approach to address the burden of dental caries2. Data from developed countries have led to the conclusion that while the disease prevalence may remain high among adults, it is declining among children. Future generations in these countries could witness an overall significant reduction in caries prevalence as a result of preventive measures2. On the contrary, there is a rise in caries prevalence in LMI countries and suggested attributable factors include increased consumption of refined sugar as well as changing lifestyles9. Unfortunately, in these countries, implementation of preventive measures has been limited, and prevalence is likely to remain high or even increase. Therefore, stakeholders in Kenya and other LMI countries should urgently push for policy adoption and implementation of preventive oral health programmes. Where middle-level colleges exist to train auxiliary dental professionals, as is the case in Kenya, they may bolster this preventive agenda, particularly in school-based oral health programmes.
In LMI countries, rural electrification remains a challenge, impacting availability of advanced restorative treatment. Apart from the high cost of contemporary aesthetic restorative materials, as well as the established advantages of dental amalgam, this may further explain why the usage of amalgam in LMI countries far surpasses that of resin composites and resin ionomers3., 6.. Cross-sectional surveys conducted among dentists in Kenya have found that amalgam is the preferred direct posterior restorative material (50% in 2003, 76% in 2010, 49% in 2014). The Dental Amalgam Project in East Africa in 2013 also reported that dental amalgam was routinely used (91.2%) for direct restorations10. Developed countries have found alternatives in indirect restorations; however, these are impractical in developing countries because of the technical needs and associated expense3. It is proposed that simple techniques, such as ART, should be actively promoted to minimise the need for extractions. High-viscosity glass ionomer cements have been extensively examined and have been shown to survive for up to 10 years as ART restorations11. This can be performed in addition to other techniques aimed at arresting caries progression, for example, use of silver diamine fluoride12.
Most dental schools, especially those in LMI countries, still rely on traditional curricula focussed on curative management of dental caries. Resource limitations have contributed to disparities in the provision of oral health care, and oral health-care professionals are trained only to provide very basic services. Another survey in Kenya found that most dentists were aware of the Minamata Convention on Mercury, and while 57% were in favour of their country being a signatory, 43% were not. The greatest concern was that adoption of the policy might negatively impact the quality of dental training and consequently provision of oral health care as a result of increasing costs.
Nonetheless, Kenya developed a national environmental action plan in 2016 and is at an advanced stage in becoming a party to the Convention. The solid waste policy was reviewed to include a clause on best-management practice for dental amalgam waste and there has been intense lobbying by the Kenya Dental Association seeking projects to support the installation of separators and to promote recycling among dental practitioners. Advocacy for a curriculum change intended to encompass prevention, as well as emphasise innovative research to equip the dental workforce in LMI countries, is also necessary to adapt to the phase-down of amalgam.
Contemporary practice in these countries should advocate for MID. Moreover, extraction should not be regarded as treatment per se, but rather as treatment failure6. As illustrated by Banerjee13, successful minimal intervention requires a treatment plan including four elements: identify, prevent, restore and recall. The identification phase involves diagnosis using modern caries-detection techniques when available, along with caries risk assessment of the patient. Prevention involves control of disease progression by employing recognisable approaches at individual and community levels. Restoration involves tissue replacement via minimally invasive techniques and adhesive materials. Recall phase involves return visits with frequency determined by the susceptibility of the patient. Therefore, in order to prevent disease progression, which would increase the likelihood of extraction, restorations should be placed as soon as possible; the smaller the restoration, the better the prognosis. Additionally, smaller restorations may employ adhesive materials8. Such guidelines may form the basis for a standard curriculum that is easy to implement, encompassing practical aspects of MID, including prevention and simple techniques such as ART, silver diamine fluoride, fissure sealants and preventive resin infiltration while encouraging repair instead of replacement of defective restorations.
The final challenge presented by the amalgam phase-down is the need for innovative research aimed at finding alternative restorative materials that mimic enamel and dentine. Indeed, it has been stated that ‘the ideal material is no material’4. On the basis of clinical performance, the crucial factors when considering the ideal material include: resistance to fracture; ease of placement; and service life of at least 10 years. Other concerns include operator skill, available infrastructure, patient expectations, cost-effectiveness, global challenges in manufacture and supply, and environmental impact4. Infrastructure is important because it may limit the application of some materials on the basis of what is available in resource-poor settings. The ideal material should also be able to be utilised anywhere in the world without compromising standards4., 5., 6.. It will be difficult to develop a single material that can serve all restorative applications4.
We recognise that the development of biomaterials is an expensive and time-consuming process and decades may elapse before new products are commercially available. Nonetheless, the time has come for Kenya and other LMI countries to make their contribution by using locally available resources and industries to find solutions specific to local needs; locally available materials may be utilised in simple and inexpensive restorative procedures. An example of translational science is the derivation of mineral trioxide aggregate from Portland cement. A more recent approach involves alkaline-activation of naturally occurring silicate materials, such as kaolin, to produce geopolymers with potential bioactivity14. Such materials should be readily available and inexpensive, with minimal adverse environmental impact compared with dental amalgam and other mercury-based products. They may be used to reduce or arrest progression of caries, relieving symptoms, with low cost and applicable for minimally invasive techniques, such as ART.
CONCLUSIONS
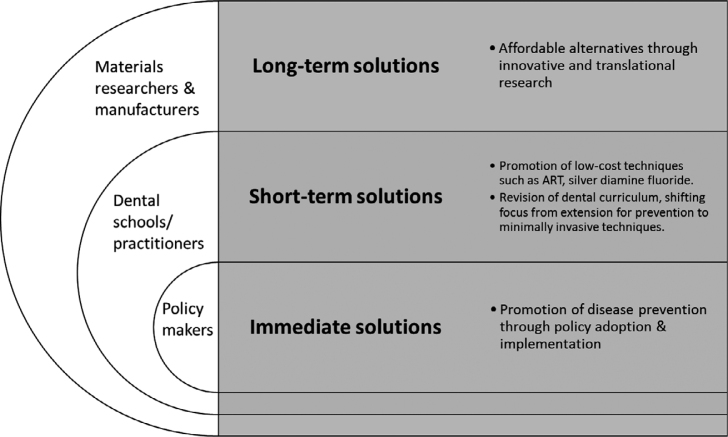
Figure 2 summarises the proposed solutions and stakeholders. The impending phase-down of dental amalgam presents a challenge to addressing the burden of dental caries in LMI countries. Development of suitable alternatives is a long-term solution. In the immediate and short-term, efforts should aim at prevention. Beyond policy, aspects of contemporary preventive dentistry, such as MID, should be incorporated in curricula of dental schools to promote practice by present-day dental workforce. The FDI Vision 2020 statement seeks to shape the future of oral healthcare by shifting focus from a curative to preventive approach15. LMI countries may find it a useful guide in seeking local and practical solutions to address challenges arising from the burden of dental caries in the face of dental amalgam phase-down.
Figure 2.
Conceptual framework model to tackle burden of caries in low- and middle-income (LMI) countries in line with the imminent phase-down of dental amalgam.
Acknowledgements
Support for this work is from the University of Nairobi, Kenya and the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Centre and the University of the Witwatersrand and funded by the Carnegie Corporation of New York (Grant No–B 8606.R02), Sida (Grant No:54100029), the DELTAS Africa Initiative (Grant No: 107768/Z/15/Z). The DELTAS Africa Initiative is an independent funding scheme of the African Academy of Sciences (AAS)’s Alliance for Accelerating Excellence in Science in Africa (AESA) and supported by the New Partnership for Africa’s Development Planning and Coordinating Agency (NEPAD Agency) with funding from the Wellcome Trust (UK) (Grant No: 107768/Z/15/Z) and the UK government. The views expressed are those of the authors.
Declaration of Competing Interests
The authors declare no competing interests.
References
- 1.Petersen PE. Challenges to improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Int Dent J. 2004;54:329–343. doi: 10.1111/j.1875-595x.2004.tb00009.x. [DOI] [PubMed] [Google Scholar]
- 2.Petersen PE. World Health Organization global policy for improvement of oral health–World Health Assembly 2007. Int Dent J. 2008;58:115–121. doi: 10.1111/j.1875-595x.2008.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 3.Petersen P, Baez R, Kwan S, et al. World Health Organization; Geneva, Switzerland: 2009. Future use of Materials for Dental Restoration; pp. 1–56. [Google Scholar]
- 4.Rekow ED, Bayne SC, Carvalho RM, et al. What constitutes an ideal dental restorative material? Adv Dent Res. 2013;25:18–23. doi: 10.1177/0022034513502206. [DOI] [PubMed] [Google Scholar]
- 5.Ferracane J, Fisher J, Eisele JL, et al. Ensuring the global availability of high-quality dental restorative materials. Adv Dent Res. 2013;25:41–45. doi: 10.1177/0022034513502208. [DOI] [PubMed] [Google Scholar]
- 6.Bayne S, Petersen PE, Piper D, et al. The challenge for innovation in direct restorative materials. Adv Dent Res. 2013;25:8–17. doi: 10.1177/0022034513506904. [DOI] [PubMed] [Google Scholar]
- 7.Wilson NH. Ouintessence; Surrey: 2007. Minimally Invasive Dentistry–The Management of Caries; pp. 72–77. [Google Scholar]
- 8.Ericson D. The concept of minimally invasive dentistry. Dent Update. 2007;34:9–18. doi: 10.12968/denu.2007.34.1.9. [DOI] [PubMed] [Google Scholar]
- 9.Macigo FG, James RM, Ogunbodede E, et al. Sugar consumption and dental caries experience in Kenya. Int Dent J. 2016;66:158–162. doi: 10.1111/idj.12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Free Communications Sessions 47–54 Saturday, August 31, 2013. Int Dent J. 2013;63:297–378. [Google Scholar]
- 11.Frencken JE, Leal SC, Navarro MF. Twenty-five-year atraumatic restorative treatment (ART) approach: a comprehensive overview. Clin Oral Investig. 2012;16:1337–1346. doi: 10.1007/s00784-012-0783-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenblatt A, Stamford T, Niederman R. Silver diamine fluoride: a caries “silver-fluoride bullet”. J Dent Res. 2009;88:116–125. doi: 10.1177/0022034508329406. [DOI] [PubMed] [Google Scholar]
- 13.Banerjee A. ‘MI’opia or 20/20 vision? Br Dent J. 2013;214:101–105. doi: 10.1038/sj.bdj.2013.105. [DOI] [PubMed] [Google Scholar]
- 14.Pangdaeng S, Sata V, Aguiar J, et al. Apatite formation on calcined kaolin–white Portland cement geopolymer. Mater Sci Eng C Mater Biol Appl. 2015;51:1–6. doi: 10.1016/j.msec.2015.02.039. [DOI] [PubMed] [Google Scholar]
- 15.Glick M, Monteiro da Silva O, Seeberger GK, et al. FDI Vision 2020: shaping the future of oral health. Int Dent J. 2012;62:278–291. doi: 10.1111/idj.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]