Abstract
Aim: To address deficits in human resources for oral health data (HROH) in rural and remote areas in Wales, Scotland and Northern Ireland by spatially profiling and modelling the distribution pattern of dental practices according to Health Boards. Methods: National Health Service (NHS) dental practices were located and mapped against population and rural–urban classifications of Scotland, Wales and Northern Ireland, using Geographic Information System (GIS) tools. All data collected were at the smallest geographical statistical hierarchy level in each country, and population data were retrieved from the 2011 census. Results: A total of 1,695 NHS dental practices were mapped against 27 Health Board regions. In Scotland, Northern Ireland and Wales, 18.3%, 18.7% and 7.7%, respectively, of the population living in the most remote areas resided within 2.5 km of a dental practice. In each country, the Health Boards with the largest proportion of the population living more than 10 km from a dental practice were the Western Isles (Scotland), Western Health and Social Care Trust (HSCT) (Northern Ireland) and Hywel Dda University Health Board (UHB) (Wales). In each country, the highest practice-to-population (PtP) ratios were found in Forth Valley (1:7,194) (Scotland), Southern HSCT (1:5,115) (Northern Ireland) and Hywel Dda UHB (Wales) (1:7,907). Conclusion: Dental services are distributed unequally between urban and rural areas. PtP ratios coupled with GIS analysis are important tools to improve HROH distribution.
Key words: Spatial distribution, rural, oral health, distribution
INTRODUCTION
Oral health is integral to general health, our basic human right1., 2.. The lack of access to oral healthcare providers is one of the primary root causes of oral health inequity, with low access occurring particularly because of the imbalance in geographical distribution of dental practitioners3. International calls to address inequalities in healthcare distribution have been acted upon by the World Health Organization (WHO) in the dissemination of the Global Strategy on Human Resources for Health: Workforce 20304. This synthesis paper captures evidence and makes recommendations to improve the availability, accessibility, acceptability and quality of human resources for health (HRH)4. Efforts to address inequity in access to health apply directly to the dental workforce, termed human resources for oral health (HROH)5. Given that major oral disorders are amongst the top 35 causes of years of life lived with a disability around the world, it is concerning that HROH has not received the surveillance and recognition merited6.
Across the globe, the maldistribution of HROH between urban and rural areas is an established public health challenge and is a persistent problem in achieving oral health equality. Studies consistently show a greater concentration of dentists in urban areas and shortages in remote areas across the world7. In Australia, in 2013, there was a 40,000% difference in practice-to-population (PtP) ratios, which ranged from 1:52 in urban areas to 1:20,000 in rural and remote areas where the majority of suburbs are without practices8. Similarly, in New Zealand, PtP numbers in rural areas were significantly lower than in city areas9. In the USA and Australia, populations living in rural and remote areas have higher rates of dental caries, poorer access to dental care and higher prevalence of edentulism8., 10.. The rural population faces greater costs in utilizing dental care through barriers (cost of fuel, travel distance, lack of public transportation) to accessing such care; moreover, lower levels of water fluoridation (and a consequent increase in the risk of dental caries), higher poverty (resulting in a lower proportion of the population having health insurance) and higher rates of tobacco use (which has a detrimental effect on oral health) may increase the need for, and costs of, dental care11., 12.. Against this background, it is surprising that the concept of rurality is notably absent from oral health policies of English-speaking countries with sizeable rural populations, such as England and Northern Ireland, and is present in only 1% of policy documents in Wales13.
In the UK, the dental workforce has seen rapid increases in the population of registered dentists compared with general population growth, therefore greatly improving the dentist-to-population ratio. For example, from 2007 to 2017, the UK population increased by 8.23%, whilst the number of registered dentists increased by 29.8%14., 15.. Subsequently, the dentist-to-population (DtP) ratio in the UK has significantly improved within 10 years. Despite the substantial increase in the number of registered dentists, Walls & Steele observed that dentist-to-patient ratios tended to be lower in rural and remote areas where poor public transport and reduced accessibility are issues16.
The UK geographical landscape is predominantly rural (more than two-thirds of the land area is classified as rural), with an estimated 40% of the population living in these areas17. However, there is sparse research on the distribution of HROH in rural and remote areas. In Wales, Phillipps & Boulos found that the distribution of NHS dentists was not uniform, especially in rural areas where there is a shortage of HROH18. However, that research was based on regions of Welsh Local Health Boards (LHBs) which were abolished in 201319. Interestingly, research in Scotland showed that children living in rural and remote areas appeared to have better dental health (lower prevalence and severity of any caries experience) than those living in urban areas. Furthermore, children in urban areas of Scotland had greater proportions of decayed and restored teeth than children living in rural areas20. It is generally believed that in Scotland, rural areas are less deprived than urban areas but there is insufficient evidence available to determine urban–rural differences in HROH distribution20. Since the devolution of Scotland, Wales and Northern Ireland in 1998, the autonomous health systems have become increasingly distinct under the NHS family of systems19. NHS Health Boards are taking more responsibility in providing oral health care and securing access to HROH, and therefore local data are required21., 22..
Geographic Information System (GIS) is a valuable technology widely used in medical studies and has been gaining traction in dentistry. In dentistry, there is a growing standard of compelling GIS research investigating the accessibility of dentists in geographically large developed countries, such as Australia, Canada and the USA3., 5., 7., 8.. Accessibility to healthcare services is widely defined as having five dimensions: approachability; acceptability; availability and accommodation; affordability; and appropriateness23. Availability refers to the physical space or spatial accessibility to healthcare. PtP ratios and distance to the nearest provider are components of spatial accessibility that can be measured24. However, the use of GIS in analysing the spatial accessibility of HROH is relatively scarce in the UK and even more so for rural and remote areas. This current study addresses deficits in HROH distribution data in rural and remote areas in Wales, Scotland and Northern Ireland by utilizing GIS to create a spatial model and profile the distribution pattern of dental practices. The aim of this study was therefore to examine urban–rural differences in dental practice distribution in Health Boards in Wales, Scotland and Northern Ireland.
METHODS
All data were collected from 1 March to 19 June 2019 from open-access, de-identified sources. Ethics exemption was acquired from the Human Research Ethics office of the University of Western Australia.
NHS dental practice locations
The physical locations for dental practices offering General Dental Services (GDS) and Community Dental Services (CDS) were collected from the NHS dental service provider websites of Wales (https://www.nhsdirect.wales.nhs.uk), Scotland (https://www.nhsinform.scot) and Northern Ireland (http://online.hscni.net). All addresses were entered into a database and duplicate addresses were eliminated. A tailor-made software program overlaying on the free-access Microsoft maps was used to find the longitude and latitude for each dental practice (http://iroche.net/Geo2/Enter.php). All geocoded addresses were checked for accuracy. Addresses at a post code (zip code) level of accuracy were geocoded again using a free-access geocoding website (https://maps.google.com.au/maps) to resolve all dental practice addresses to a minimum accuracy of street level. Random samples of 1%–2% of geocoded data were cross-checked against personal knowledge and a web search to confirm the integrity of the data. In total, 99.3% of NHS GDS and CDS practices of Scotland, Wales and Northern Ireland were included in this study.
Population data
All population data were collected from the latest 2011 census populations collected by the National Records of Scotland (NRS)25, Northern Ireland Statistics and Research Agency (NISRA)26 and Office for National Statistics (ONS)27. All data collected were at the smallest geographical statistical hierarchy level in each country. In Wales and Scotland, population estimations for Output Areas (OA) were used and in Northern Ireland, Small Areas (SA) were used. The total number of OAs in Wales is 20,073, holding a minimum of 100 people and a maximum of 625 people. Scotland has 46,351 OAs, holding a minimum of 50 people and a maximum of 2,081 people. Northern Ireland contains 4,537 SA, holding a minimum of 98 people and a maximum of 3,075 people.
Geographical analysis
The Quantum Geographic Information System (QGIS; ver.3.6; https://www.qgis.org/en/site/) offers GIS functions that store, process and display data to perform spatial analysis28. Overlay analysis was used to overlay population data, dental practice locations, urban–rural classification data and area boundary files to determine spatial relationships. Geometric centres, called centroids, were created for each OA and SA. If a centroid was within 2.5, 5 or 10 km, it was assumed that the population of that area lived within the specified radius of the dental practice. These distances were chosen based on numerous previous publications in modelling spatial accessibility8., 9., 29., 30..
NHS Health Boards
Scotland has 14 regional NHS Boards, Wales has seven Local Health Boards (LHBs) and Northern Ireland has six Health and Social Care Trusts (HSCTs). The NHS Boards, LHBs and HSCTs of the respective countries are responsible for delivering NHS services to their areas. The latest 2014 boundaries of the Scottish NHS Boards were retrieved from the Scottish Government31. The 2016 boundaries of the LHBs in Wales were retrieved from the ONS32 and the most recent 2017 boundaries for the HSCTs were retrieved from the Department of Health of Northern Ireland33.
Rural and urban classifications
The nature of rurality and definitions are different for Scotland, Northern Ireland and Wales. The Scottish Government Urban Rural Classification (SURC) is based on (i) population and (ii) accessibility, which are based on the driving times between accessible and remote areas34. Settlements of fewer than 3,000 are classed as rural34. This study uses the eight-fold Urban–Rural Classification, the most detailed classification, in which Classes 1–5 are urban and Classes 6–8 are rural (Table 1). Northern Ireland uses Settlement Development Limits (SDLs) to define the geographical extents of settlements for rural and urban classifications35. Settlements of fewer than 5,000 are considered as rural35. The following urban–rural recommendations were utilized: Bands A–E are urban and Bands F–H are rural (Table 1)35. The 2011 Rural–Urban Classification (RUC) is used for Wales, based on ‘built-up areas’. Classes C1 and C2 are classified as urban and Classes D1 to F2 are classified as rural (Table 1)36. The population threshold for urban areas is 10,00036. The smallest available areas were each classified according to the respective classification systems; data zones (DZs) were classified for Scotland, OAs for Wales and SAs for Northern Ireland. Lookup tables were used to classify OAs from DZ classifications from Scotland.
Table 1.
Urban–rural classifications and descriptions for Wales, Northern Ireland and Scotland
| Urban–rural classifications | Urban/rural | Description |
|---|---|---|
| Wales* | ||
| City and town (Class C1) | Urban | Less than 26% living in rural settlements and hub towns |
| City and town in a sparse setting (Class C2) | Urban | At least 26% but less than 50% living in rural settlements and hub towns |
| Town and fringe (Class D1) | Rural | At least 50% but less than 80% living in rural settlements and hub towns |
| Town and fringe in a sparse setting (D2) | Rural | At least 50% but less than 80% living in rural settlements and hub towns |
| Village (Class E1) | Rural | At least 50% but less than 80% living in rural settlements and hub towns |
| Village in a sparse setting (Class E2) | Rural | At least 80% living in rural settlements and hub towns |
| Hamlets and isolated dwellings (Class F1) | Rural | At least 80% living in rural settlements and hub towns |
| Hamlets and isolated dwellings in a sparse setting (Class F2) | Rural | At least 80% living in rural settlements and hub towns |
| Northern Ireland† | ||
| Belfast (Band A) | Urban | Population of Belfast city |
| Derry city (Band B) | Urban | Population of Derry city |
| Large town (Band C) | Urban | Population above 18,000 |
| Medium town (Band D) | Urban | Population between 10,000–17,999 |
| Small town (Band E) | Urban | Population between 5,000–9,999 |
| Intermediate settlement (Band F) | Rural | Population between 2,500–4,999 |
| Village (Band G) | Rural | Population between 1,000–2,499 |
| Open countryside and small population (Band H) | Rural | Population less than 1,000 |
| Scotland‡ | ||
| Large urban areas (Class 1) | Urban | Settlements of 125,000 people and over |
| Other urban areas (Class 2) | Urban | Settlements of 10,000–124,999 people |
| Accessible small towns (Class 3) | Urban | Settlements of 3,000–9,999 people and within a 30-minute drive time of a settlement of 10,000 or more |
| Remote small towns (Class 4) | Urban | Settlements of 3,000–9,999 people, and with a drive time of over 30 minutes but ≤60 minutes to a settlement of 10,000 or more |
| Very remote small towns (Class 5) | Urban | Settlements of 3,000–9,999 people, and with a drive time of over 60 minutes to a Settlement of 10,000 or more |
| Accessible rural areas (Class 6) | Rural | Areas with a population of less than 3,000 people, and within a drive time of 30 minutes to a Settlement of 10,000 or more |
| Remote rural areas (Class 7) | Rural | Areas with a population of less than 3,000 people, and with a drive time of over 30 minutes but ≤60 minutes to a Settlement of 10,000 or more |
| Very remote rural areas (Class 8) | Rural | Areas with a population of less than 3,000 people, and with a drive time of over 60 minutes to a Settlement of 10,000 or more |
2011 Rural-Urban Classification for Wales.
Settlements and Urban-Rural Classification 2015.
Scottish Government Urban Rural Classification 2016.
Statistical analysis
All data analyses were conducted on QGIS and Microsoft Excel 2019 (ver. 16.23; https://www.microsoft.com/en-au/microsoft-365/excel). Joined data from QGIS was converted into a database for descriptive analysis in Microsoft Excel. Multiple pivot tables were used to derive descriptive measures and perform area lookups.
RESULTS
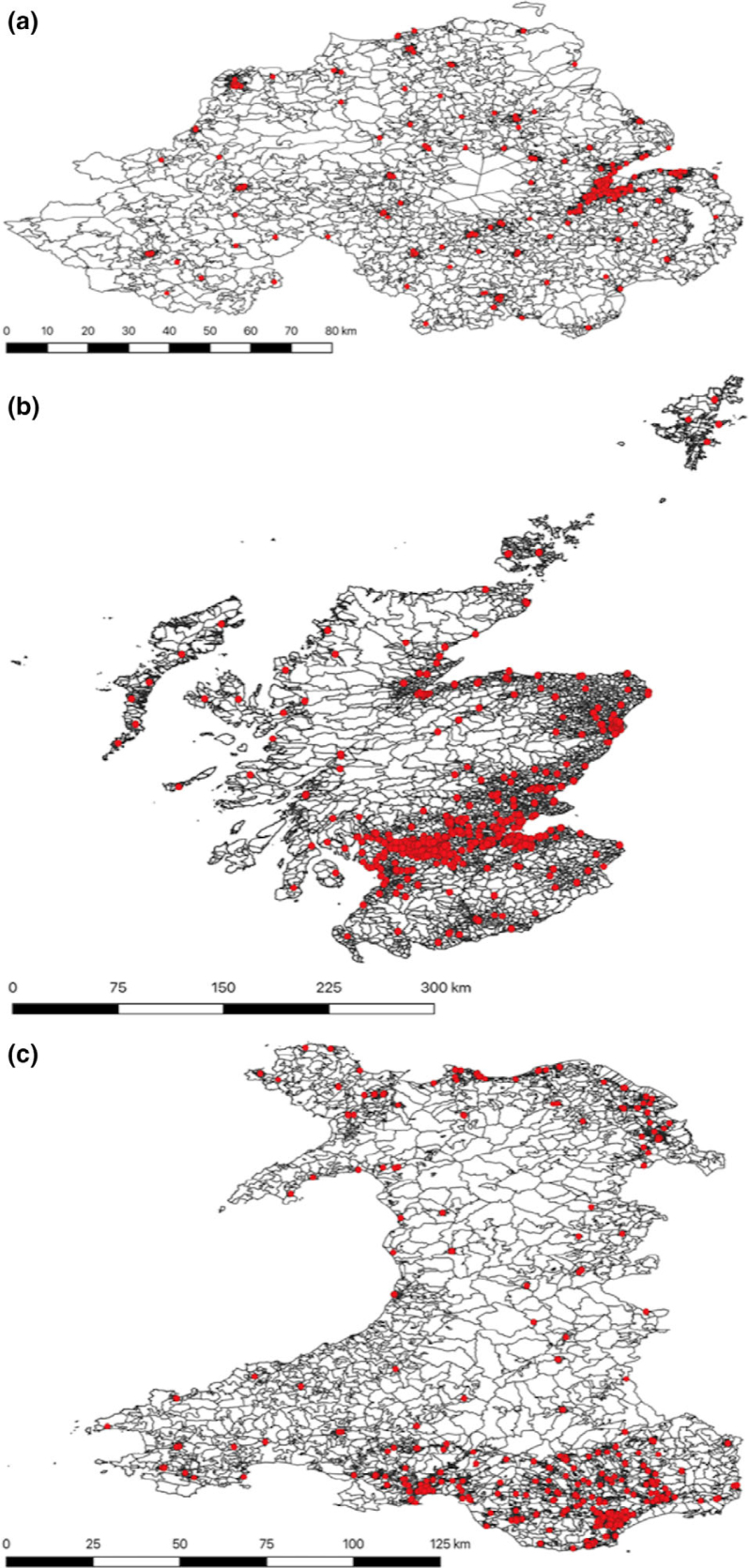
In this study, the populations of Wales (3.06 million), Scotland (5.295 million) and Northern Ireland (1.81 million) were distributed across 20,073 (20,735 km2), 46,351 (80,077 km2) and 4,537 OAs (14,130 km2), respectively. There was an average of 152 people per OA in Wales, 114 people per OA in Scotland and 399 people per OA in Northern Ireland. A total of 1,695 NHS GDS and CDS practices were distributed across a total of 70,961 OAs in Scotland, Northern Ireland and Wales (Figure 1). There were 278 dental practices in Northern Ireland, 991 in Scotland and 426 in Wales (Figure 1). Figure 1 depicts an overlay of NHS dental practices on the smallest available census areas, displaying the distribution of NHS practices in specific areas.
Figure 1.
Distribution of National Health Service (NHS) dental practices (red circles) in (a) Northern Ireland, (b) Scotland and (c) Wales.
Distance to practice according to country
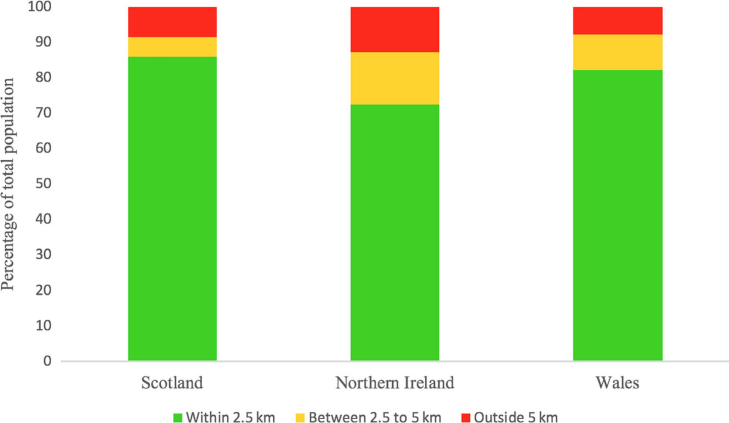
Overall, 4,549,312 (85.9%) people in Scotland, 1,313,565 (72.6%) people in Northern Ireland and 2,519,835 (82.3%) people in Wales live within 2.5 km of a dental practice; 298,698 (5.6%) people in Scotland, 267,802 (14.8%) people in Northern Ireland and 305,953 (10%) people in Wales live between 2.5 and 5 km from a dental practice; and 224,431 (8.4%) people in Scotland, 228,383 (12.6%) people in Northern Ireland and 237,668 (7.8%) people in Wales live further than 5 km from a dental practice (Figure 2).
Figure 2.
Percentage of the population living within 2.5 km, between 2.5 and 5 km and further than 5 km from a dental practice in Scotland, Northern Ireland and Wales.
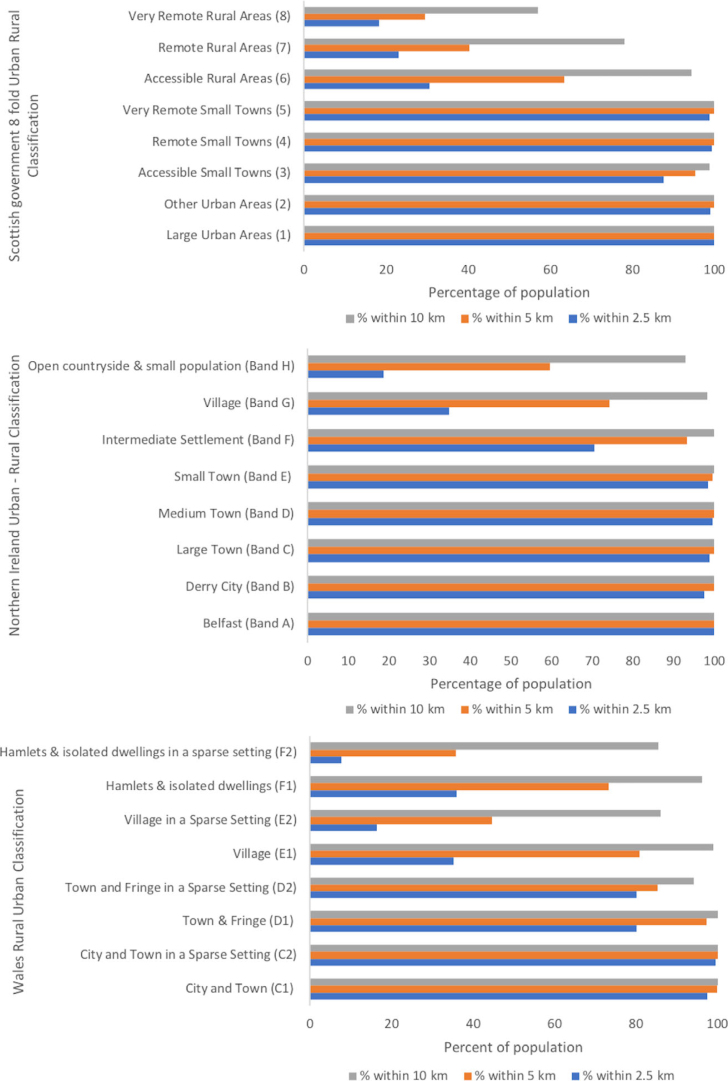
Dental practices in rural and remote areas
In Scotland, the population is unevenly distributed across the eight categories of the SURC, with 82.7% living in urban areas (Classes 1–5) and 17.3% living in rural areas (Classes 6–8) (Figure 3). All (100%) of the population living in large urban areas (Class 1) reside within 2.5 km of a dental practice. By contrast, only 18.3% of the population living in very remote rural areas (Class 8) reside within 2.5 km of a dental practice and 57% reside within 10 km of a dental practice (Figure 3). When data are converted to mean values, just under one-quarter (24%) of the rural population were found to live within 2.5 km of a dental practice compared with almost all (96.96%) of the urban population. The stark difference between Classes 6–8 (rural) and Classes 1–5 (urban) is clearly illustrated (Figure 3); a larger number of people living in urban areas have geospatial access to a practice than those in rural areas. Within the rural areas, there is an incremental decrease, from Classes 6 to 8, in the proportion of the population who live within 2.5, 5 and 10 km of a dental practice. The range of the rural population living within 2.5 km of a dental practice is 12.2% and for urban areas this is 12.4%.
Figure 3.
Percentage of the population living within 2.5, 5 and 10 km of a dental practice in urban and rural classified areas of Wales, Scotland and Northern Ireland.
In Northern Ireland, 100% of the population in Belfast city (Band A) live within 2.5 km of a dental practice compared with 18.7% and 59.5% of the population residing in open countryside and small populations (Band H) who live within 2.5 km and within 5 km, respectively, of a dental clinic (Figure 3). A marked difference can be seen in the mean proportion of rural populations (Bands F–H) (41.3%) and urban populations (Bands A–E) (98.8%) who live within 2.5 km of a dental practice. Within the rural areas, there is an incremental decrease in populations in Bands F–H who live within 2.5, 5 and 10 km of a dental practice. The range of rural populations living within 2.5 km of a dental practice is 51.7% compared with 2.5% for the range of urban populations.
In Wales, 97.4% of the population residing in an urban city and town (Class C1) live within 2.5 km of a dental practice (Figure 3). At the other end of the spectrum, only 7.7% of the population residing in Hamlets and isolated dwellings in a sparse setting (Class F2) live within 2.5 km of a dental practice (Figure 3). Interestingly, an average of 40% of the population in rural areas (Classes D1 to F2) lives within 2.5 km of a dental practice, whilst an average of 98.5% of the population in urban areas (Classes C1 and C2) lives within 2.5 km of a dental practice. The range of the rural population living within 2.5 km of a practice is 72.4% compared with 2.2% for urban areas. Villages in a sparse setting (Class E2), and Hamlets and isolated dwellings in a sparse setting (Class F2), have the lowest percentage of people living within 2.5% of a dental practice (Figure 3).
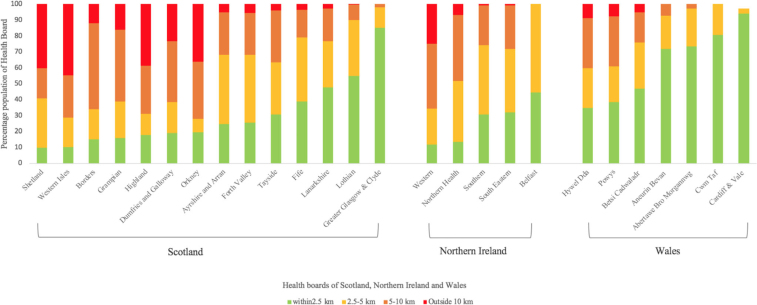
Dental practice location according to Health Board region
In Scotland, the Health Board areas with the highest percentage of the population living more than 10 km from a dental practice are the Western Isles (44.6%), Shetland (40%), Highland (38.5%) and Orkney (36.3%) (Figure 4). These areas also have the highest percentages of rural populations, at 72%, 67.6%, 47.8% and 65.3%, respectively (Table 2). It is interesting to note that in Fife, although a high proportion of the population living in rural classified areas, the majority resides within 10 km of a dental practice (96.7%).
Figure 4.
Percentage of the population living less than 2.5 km, at least 2.5 km but less than 5 km, at least 5 km but less than 10 km and further than 10 km from a dental practice within the respective Health Boards of Scotland, Northern Ireland and Wales.
Table 2.
National Health Service (NHS) practice-to-population (PtP) ratios, percentage of the population in urban and rural areas and percentage of the rural population living within 5 km of a dental practice
| Health Board area | Area (km2) | Population (n) | Dental clinic (n) | PtP ratio | %Urban | %Rural | % Rural within 5 km* |
|---|---|---|---|---|---|---|---|
| Scotland | |||||||
| Orkney | 990 | 20,731 | 6 | 3,455 | 34.7 | 65.3 | 28 |
| Highland | 32,593 | 317,793 | 85 | 3,739 | 52.2 | 47.8 | 33.9 |
| Shetland | 1,467 | 21,482 | 5 | 4,296 | 32.4 | 67.6 | 40.7 |
| Borders | 4,732 | 107,329 | 24 | 4,472 | 53.5 | 46.5 | 34 |
| Western Isles | 3,060 | 27,116 | 6 | 4,519 | 28 | 72 | 28.6 |
| Greater Glasgow & Clyde | 1,104 | 1,135,661 | 243 | 4,674 | 98.1 | 1.9 | 98.1 |
| Dumfries and Galloway | 6,426 | 150,798 | 32 | 4,712 | 54.7 | 45.3 | 38.4 |
| Lothian | 1,724 | 834,159 | 166 | 5,025 | 93.2 | 6.8 | 90.2 |
| Ayrshire and Arran | 3,369 | 373,603 | 65 | 5,748 | 81.3 | 18.6 | 68.3 |
| Tayside | 7,527 | 409,714 | 69 | 5,938 | 76.7 | 23.3 | 63.6 |
| Lanarkshire | 2,242 | 651,356 | 109 | 5,976 | 91 | 9 | 76.8 |
| Grampian | 8,736 | 568,817 | 89 | 6,391 | 71.1 | 28.9 | 38.8 |
| Fife | 1,325 | 360,380 | 51 | 7,066 | 82.5 | 17.5 | 79.4 |
| Forth Valley | 1,325 | 294,944 | 41 | 7,194 | 84 | 16 | 68.4 |
| Unknown NHS board | 21,520 | ||||||
| Northern Ireland | |||||||
| Belfast | 200 | 348,204 | 92 | 3,785 | 98.9 | 1.1 | 100 |
| Western | 4,840.9 | 249,196 | 59 | 4,224 | 54 | 46 | 34.4 |
| Northern Health | 4,355.7 | 408,330 | 88 | 4,640 | 60.1 | 39.9 | 51.6 |
| South Eastern | 1,551.2 | 346,432 | 69 | 5,021 | 63.3 | 36.7 | 71.9 |
| Southern | 3,187.6 | 358,034 | 70 | 5,115 | 46.5 | 53.6 | 74.2 |
| Unknown NHS board | 99,554 | ||||||
| Wales | |||||||
| Powys | 5,179 | 132,976 | 24 | 5,541 | 13.5 | 86.5 | 60.9 |
| Cardiff and Vale | 471 | 471,336 | 71 | 6,639 | 96.5 | 6.4 | 100 |
| Abertawe Bro Morgannwg | 1,071 | 514,056 | 77 | 6,676 | 81.6 | 18.4 | 97.3 |
| Aneurin Bevan | 1,553 | 574,785 | 82 | 7,010 | 79.9 | 20.1 | 92.9 |
| Cwm Taff | 535 | 293,212 | 38 | 7,716 | 77.4 | 22.6 | 100 |
| Betsi Cadwaladr | 6,172 | 675,325 | 86 | 7,853 | 50.8 | 49.2 | 75.8 |
| Hywel Dda | 5,781 | 379,535 | 48 | 7,907 | 36 | 64 | 51.5 |
| Unknown NHS Board | 22,231 | ||||||
Percentage of the rural population living within 5 km of an NHS dental practice.
In Northern Ireland we see that in most of the Health Boards, the majority of the population lives within 10 km of a dental practice; the exception is Western HSCT in which 24.8% of the population lives more than 10 km from a dental practice. In Belfast, 100% of the population lives within 5 km of a dental practice. Interestingly, the majority of the population in Belfast lives in urban areas (98.9%; Table 2). Southern HSCT has the highest proportion of the population who live in rural areas (53%; Table 2) but the majority of the population (99.2%) resides within 10 km of a dental practice; (Figure 4).
In Wales, 100% of the populations of Cardiff & Vale University Health Board (UHB) and CWM Taff UHB live within 5 km of a dental practice. Interestingly, Hywel Dda, Powys and Betsi Cadwaladr had the highest percentages of the population living in rural areas (64%, 86.5% and 49.2%, respectively) (Table 2), and also the lowest percentages of the population living within 2.5 km of a dental practice (59.9%, 60.9% and 75.8%, respectively) (Figure 4). There was a direct relationship between population living in rural areas and population living within 5 km of a practice, with the exception of Hywel Dda.
Association with PtP ratios
In Scotland, The Health Boards Orkney and Highland had the lowest PtP ratios, of 1:3,455 and 1:3,739, respectively (Table 2). Despite having the lowest PtP ratios compared with other Health Boards, they also had a high proportion of people living in rural areas (65.3% in Orkney and 47.8% in Highland) (Table 2). Fife and Forth Valley had the highest PtP ratios, at 1:7,066 and 1:7,194, respectively (Table 2).
In Northern Ireland, Belfast had the lowest PtP ratio, of 1:3,785, and Southern HSCT had the highest, of 1:5,515 (Table 2). Interestingly, the majority (98.1%) of the Belfast population lives in urban areas and 100% of the rural population lives within 5 km of a dental practice (Table 2). On the other hand, the Southern HSCT has the greatest rural population, at 53.6%, but also a high proportion (74.2%) of the rural population living within 5 km of a dental practice (Table 2).
In Wales, Powys teaching health board had the lowest PtP ratio, of 1:5,541, and Hywel Dda UHB had the highest PtP, of 1:7,907 (Table 2). This is quite interesting as Powys teaching health board has the highest rural population (86.5%) with 60.9% living within 5 km of a dental practice (Table 2). Overall, there was no relationship between PtP ratios and the rurality of a Health Board.
DISCUSSION
The present study found markedly lower spatial accessibility to HROH in rural and remote areas of Scotland, Wales and Northern Ireland than in urban areas. These results are no surprise as DtP ratios tend to be much lower in rural areas16. In Scotland and Northern Ireland, the percentage of the rural population living within 2.5 and 5 km of a dental practice incrementally decreased as an area was classified as more ‘rural’. In Wales, hamlets and villages in sparse settings had the lowest population living within 2.5 and 5 km of a dental practice.
In Scotland, previous geospatial analysis has shown that the population living in remote areas and Health Boards serving these areas have poorer access to critical care services than do urban areas37. Similarly, this study identified Shetland and Western Isles Health Boards have the lowest percentage of the population with access to a dental practice (Figure 4). By contrast, in Greater Glasgow & Clyde Health Board, the majority of the population live within 2.5 km of a dental practice (Figure 4). Although Orkney and Shetland Health Boards had the highest percentage of rural residents, and Shetland had a higher number of rural populations than Orkney, a larger proportion of the population in Shetland than in Orkney lived within 5 km of a dental practice (Table 2). Interestingly, although Orkney and Highland have the lowest PtP ratios, there are few rural populations in these Health Boards with a dental practice within 5 km. Previous studies have found that Dumfries & Galloway and Grampian had the lowest DtP ratios and Tayside and Greater Glasgow had the highest21. PtP ratios are complementary to the DtP ratio and are important measures of accessibility8. This study shows that Dumfries & Galloway and Grampian are no longer the Health Boards with the lowest availability of dental services. Perhaps this is because the study was conducted before legislation was passed that allowed Health Boards to take more responsibility in providing primary dental care services21. It is feasible to consider that changes in national policy, and incentives such as increasing workforce numbers, the Scottish Dental Access initiative grants and local commissioning, have improved access to dental practices in Health Boards with the lowest DtP ratios38. By integrating distance-to-provider spatial analysis with PtP ratios, we were able to detect Health Board areas in need of attention regarding rural access to HROH, which may not have been identified through the use of simple DtP ratios alone.
Wales had lower PtP ratios than either Scotland or Northern Ireland. Amongst the Health Boards of Wales, Powys had the highest PtP ratio but also the highest rural population, with over half of the rural population living within 5 km of a dental practice (Table 2). Hywel Dda had the lowest PtP ratio but also the lowest rural population living within 5 km of a dental practice (Table 2). We can infer that in Powys, the locations of practices are skewed mostly to urban areas whilst in Hywel Dda there was a general lack of dental practices relative to its population. Using this data, we are able to determine if Health Boards lack availability of dental practices overall or if practices are skewed to urban areas, leaving rural and remote areas with sparse access. For example, approximately 40% of the rural population in Powys does not have access to an HROH within 5 km despite having the highest PtP ratio. Boulos & Phillipps created ‘traffic light’ maps to profile the distribution of dentists according to Health Boards and found a shortage of NHS dentists (0.359 per 1,000 population) for the whole of Wales18. Cardiff had the greatest DtP ratio and Ceredigion had the lowest18. However, it is difficult to compare results from this study as Welsh Local Health Boards were abolished in 201319. It is notable that in Cardiff & Vale and Cwm Taff, 100% of the rural population lives within 5 km of a dental practice (Table 2).
Northern Ireland experiences some of the worst oral health inequalities in the UK39. The current oral health strategy has been rendered out of date and a new evidence-based oral health strategy has been recommended by 2021 in the Health Funding in Northern Ireland report40. This study gives some very useful insights to the distribution of HROH in urban and rural areas of Northern Ireland according to Health Boards. In Belfast, 100% of the rural population was found to live within 5 km of a dental practice. However, this can be attributable to the fact that only 1.1% of the population lived in rural areas and Belfast had the smallest area (200 km2) of all Health Boards. It is noteworthy to compare the Southern and Western Health Boards as the Southern Health Board has the highest population that lives in rural areas but also a high number of the rural population living within 5 km of a dental practice. On the other hand, the Western Health Board also had a high rural population but less than half of the rural population of the Southern Health Board lived within 5 km of a dental practice. There is sparse research in relation to spatial access to HROH in Northern Ireland. This study indicates that the Western Health Board had the greatest maldistribution of dental practices in rural and remote areas. Data analyses from this study may prove valuable for future decision makers in development of the upcoming new oral health strategy40.
PtP ratios are a valuable tool for measuring accessibility and identifying unevenness of HROH distribution8. In Australia, the PtP difference among suburbs was 40,000%, showing a gross maldistribution in dental practice distribution8. The present study found that the PtP difference among Health Boards in Scotland ranged from 3,455 to 7,194 (an estimated difference of 208%), in Northern Ireland the PtP difference among Health Boards ranged from 3,785 to 5,115 (an estimated difference of 135%) and in Wales the PtP difference among Health Boards ranged from 5,541 to 7,907 (an estimated difference of 143%). In New Zealand the PtP ratio was 1:2,713 in urban areas and 1:4,778 in rural areas; in Malaysia the total PtP ratio was 1:9,0009., 30.. The present study utilized PtP ratios as a dental workforce measure in conjunction with GIS-based spatial profiling to explore the spatial accessibility of HROH in rural and remote areas.
Oral health inequalities are not only amplified by socio-economic disparities, but also through an absence of policy and practice41. Since devolution, NHS Wales, NHS Scotland and NHS Northern Ireland became independent bodies and various health departments in the UK took independent actions in regard to improving oral health, such as changing fluoride policies, creating school-based schemes to improve oral health of children and enhancing oral health promotion22., 42.. Subsequently, it was found that the concept of rural oral health occurred most frequently in 4% of policy documents of Scotland, in 1% of policy documents of Wales and not at all in the oral health policies of Northern Ireland13. Implementation of rural oral health policies would facilitate oral health equality and therefore general health outcomes for rural communities. This study provides important analyses of the distribution of the dental workforce between urban and rural and remote areas in Scotland, Wales and Northern Ireland that can further lead policy in the respective countries.
Limitations
A limitation of this study was that we were only able to compare PtP ratios and other indicators according to Health Boards, and not according to nations, as the urban–rural classifications of Scotland, Wales and Northern Ireland differ in the nature of rurality alongside definitions of classifications34. The second limitation of this study was that the data did not reflect the proportion of GDS and CDS dentists and the number of dental health workers, such as dental therapists, hygienists and dental assistants, in each practice. In 2004, Great Britain had 20,800 dentists in GDS, 3,500 in Personal Dental Services (PDS), 1,940 in CDS, 200 in Salaried Dental Services (SDS) and 2,245 in Hospital Dental Services; just 210 practices were private only43. Practice profiling is an important issue. Further research should delineate NHS dental clinics by the type of dental services provided and further examine dental practice workforce profiles. Other limitations include the absence of data on the number of NHS dentists accepting new patients, the size of each practice, waiting times, transportation options and road networks. We were also unable to account for variations in border crossing and for patients who may attend a dental practice close to work. However, these are well-known limitations in spatial accessibility studies24.
CONCLUSION
The results of this study highlighted the disparities in spatial accessibility to HROH across Health Boards, and further identified disparities in the distribution of dental practices between urban and rural areas. Dental services are distributed unequally between urban and rural areas in Scotland, Wales and Northern Ireland. PtP ratios coupled with GIS analysis are important tools to improve HROH distribution, especially in rural and remote areas. It is evident that more research is needed on HROH to guide decision makers in ensuring oral health equity for rural communities.
Acknowledgements
This research was supported by an Australian Government Research Training Program (RTP) Scholarship.
Conflict of interest
The authors declare no conflict of interest.
REFERENCES
- 1.World Health Organisation. The right to health fact sheet no. 31; 2008. Available from: https://www.ohchr.org/documents/publications/factsheet31.pdf. Accessed 20 April 2019.
- 2.World Health Organization. The Liverpool declaration: promoting oral heath in the 21st century; 2005. Available from: https://www.who.int/oral_health/events/orh_liverpool_declaration_05.pdf?ua=1. Accessed 20 April 2019.
- 3.World Health Organisation. Increasing access to health workers in remote and rural areas through improved retention: global policy recommendations; 2010. Available from: https://apps.who.int/iris/bitstream/handle/10665/44369/9789241564014_eng.pdf?sequence=1. Accessed 20 April 2019. [PubMed]
- 4.Global Health Workforce Alliance. Synthesis paper of the thematic working groups – Health Work Force 2030 – towards a global strategy on human resources for health; 2015. Available from: https://apps.who.int/iris/bitstream/handle/10665/250368/9789241511131-eng.pdf?sequence=1. Accessed 20 April 2019.
- 5.Gallagher JE, Hutchinson L. Analysis of human resources for oral health globally: inequitable distribution. Int Dent J. 2018;68:183–189. doi: 10.1111/idj.12349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vos T, Flaxman AD, Naghavi M. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systemic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gabriel M, Cayetano MH, Galante ML, et al. A global overview of the geographical distribution of dentists: a scoping review. JDR Clin Trans Res. 2018;3:229–237. doi: 10.1177/2380084418774316. [DOI] [PubMed] [Google Scholar]
- 8.Tennant M, Kruger E, Shiyha J. Dentist-to-population and practice-to-population ratios: in a shortage environment with gross maldistribution what should rural and remote communities focus their attention on? Rural Remote Health. 2013;13:2518. [PubMed] [Google Scholar]
- 9.Kruger E, Whyman R, Tennant M. High-acuity GIS mapping of private practice dental services in New Zealand: does service match need? Int Dent J. 2012;62:95–99. doi: 10.1111/j.1875-595X.2011.00096.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vargas CM, Dye BA, Hayes KL. Oral health status of rural adults in the United States. J Am Dent Assoc. 2002;133:1672–1681. doi: 10.14219/jada.archive.2002.0120. [DOI] [PubMed] [Google Scholar]
- 11.Dodd VJ, Logan H, Brown CD, et al. Perceptions of oral health, preventive care and care-seeking behaviours among rural adolescents. J Sch Health. 2014;84:802–809. doi: 10.1111/josh.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Skillman SM, Doescher MP, Mouradian WE, et al. The challenge to delivering oral health services in rural America. J Public Health Dent. 2010;70:S49–S57. doi: 10.1111/j.1752-7325.2010.00178.x. [DOI] [PubMed] [Google Scholar]
- 13.Crocombe LA, Goldberg LR, Bell E, et al. A comparative analysis of policies addressing rural oral health in eight English-speaking OECD countries. Rural Remote Health. 2017;17:1–12. doi: 10.22605/RRH3809. [DOI] [PubMed] [Google Scholar]
- 14.Office for National Statistics. Overview of the UK population: November 2018; 2018. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/articles/overviewoftheukpopulation/november2018. Accessed 30 April 2019.
- 15.Office for National Statistics. EMP04: employment by occupation; 2018. Available from: https://www.ons.gov.uk/employmentandlabourmarket/peopleinwork/employmentandemployeetypes/datasets/employmentbyoccupationemp04. Accessed 30 April 2019.
- 16.Walls AWG, Steele JG. Geriatric oral health issues in the United Kingdom. Int Dent J. 2001;51:183–187. [PubMed] [Google Scholar]
- 17.Pateman T. Rural and urban areas: comparing lives using rural/urban classifications. Regional Trends. 2011;43:11. [Google Scholar]
- 18.Phillipps G, Boulos M. Is NHS dentistry in crisis? ‘Traffic light’ maps of dentists distribution in England and Wales. Int J Health Geogr. 2004;3:10. doi: 10.1186/1476-072X-3-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tickle M. Revolution in the provision of dental services in the UK. Community Dent Oral Epidemiol. 2012;30:110–116. doi: 10.1111/j.1600-0528.2012.00729.x. [DOI] [PubMed] [Google Scholar]
- 20.Levin KA, Davies CA, Douglas GVA, et al. Urban-rural differences in dental caries of 5-year old children in Scotland. Soc Sci Med. 2010;71:2020–2027. doi: 10.1016/j.socscimed.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Newton J, Williams A, Bower E. Access to dental services in Scotland: an analysis of dentist-population ratios. Br Dent J. 2008;204:142–143. doi: 10.1038/bdj.2007.1107. [DOI] [PubMed] [Google Scholar]
- 22.Chestnutt IG. Addressing oral health inequalities in the United Kingdom – the impact of devolution on population-based fluoride policy. Br Dent J. 2013;215:11–12. doi: 10.1038/sj.bdj.2013.626. [DOI] [PubMed] [Google Scholar]
- 23.Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. International Journal for Equity in Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. International Journal of Health Geographics. 2004;3:3. doi: 10.1186/1476-072X-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Records of Scotland. Scotland’s Census; 2018. Available from: http://www.scotlandscensus.gov.uk/census-results. Accessed 14 June 2019.
- 26.Northern Ireland Statistics and Research Agency. 2011 Census Population and Household estimates for wards and small areas for Northern Ireland; 2013. Available from: https://www.nisra.gov.uk/statistics/census/2011-census. Accessed 14 June 2019.
- 27.Office for National Statistics. 2011 Census: population and household estimate for small areas in England and Wales; 2012. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/bulletins/populationandhouseholdestimatesfortheunitedkingdom/2011-03-21. Accessed 14 June 2019.
- 28.QGIS Development Team. Introducing GIS; 2019. Available from: https://docs.qgis.org/testing/en/docs/gentle_gis_introduction/introducing_gis.html#overview. Accessed 14 June 2019.
- 29.Almado H, Kruger E, Tennant M. Application of spatial analysis technology to the planning of access to oral health care for at-risk populations in Australian capital cities. Aust J Prim Health. 2013;21:221–226. doi: 10.1071/py13141. [DOI] [PubMed] [Google Scholar]
- 30.Md Bohari NF, Kruger E, John J, et al. Analysis of dental services distribution in Malaysia: a geographic information systems – based approach. Int Dent J. 2019;69:223–229. doi: 10.1111/idj.12454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scottish Government. NHS Health Boards; 2019. Available from: https://www.spatialdata.gov.scot/geonetwork/srv/eng/catalog.search;jsessionid=60FACCB0DA9502D2F27D2A24E73E1E1C#/metadata/f12c3826-4b4b-40e6-bf4f-77b9ed01dc14. Accessed 14 June 2019.
- 32.Office for National Statistics. Local Health Boards (December 2016) cull clipped boundaries in Wales; 2016. Available from: https://data.gov.uk/dataset/35da6a3d-e0e5-476a-989c-46678df1deb3/local-health-boards-december-2016-full-clipped-boundaries-in-wales. Accessed 14 June 2019.
- 33.Department of Health. Department of health trust boundaries; 2016. Available from: https://www.opendatani.gov.uk/dataset/department-of-health-trust-boundaries. Accessed 14 June 2019.
- 34.Scottish Government. Rural and environment science and analytical services division. Scottish Government Urban Rural Classification 2016; 2018. Available from: https://www.gov.scot/publications/scottish-government-urban-rural-classification-2016/. Accessed 14 June 2019.
- 35.Northern Ireland Statistics and Research Agency. Review of the statistical classification and delineation of settlements; 2015. Available from: https://www.nisra.gov.uk/publications/settlement-2015-documentation. Accessed 14 June 2019.
- 36.Office for National statistics. The 2011 rural-urban classification for small area geographies: a user guides; 2013. Available from: https://www.ons.gov.uk/methodology/geography/geographicalproducts/ruralurbanclassifications/2011ruralurbanclassification. Accessed 14 June 2019.
- 37.Emerson P, Dodds N, Green DR, et al. Geographical access to critical care services in Scotland. J Int Care Soc. 2018;19:6–14. doi: 10.1177/1751143717714948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.The Scottish Needs assessment program. Needs assessment report on rural and remote dentistry; 2007. Available from: https://www.scotphn.net/wp-content/uploads/2015/11/SNAP_-_Remote_and_Rural_Dentistry_Mar_20071.pdf. Accessed 14 June 2019.
- 39.Mullally B. Child oral health promotion experiences in Northern Ireland. Br Dent J. 2002;192:175. doi: 10.1038/sj.bdj.4801327a. [DOI] [PubMed] [Google Scholar]
- 40.House of Commons Northern Ireland Affairs Committee. Health funding in Northern Ireland first report of session 2019; 2019. Available from: https://publications.parliament.uk/pa/cm201920/cmselect/cmniaf/300/300.pdf. Accessed 10 November 2019.
- 41.Williams DM. The research agenda on oral health inequalities: the IADR-GOHIRA initiative. Med Princ Pract. 2014;23:52–59. doi: 10.1159/000356934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jones CM. Independence and oral health: implications of the Scottish referendum. Br Dent J. 2014;217:65. doi: 10.1038/sj.bdj.2014.592. [DOI] [PubMed] [Google Scholar]
- 43.The House of Commons. Department of Health: reforming NHS dentistry thirtieth report of session 2004–05; 2005. Available from: https://publications.parliament.uk/pa/cm200405/cmselect/cmpubacc/167/167.pdf. Accessed 10 November 2019.