Abstract
Introduction: This article describes the features that should be considered when describing, purchasing and using a light-curing unit (LCU). Methods: The International System of Units (S.I.) terms of radiant power or radiant flux (mW), spectral radiant power (mW/nm), radiant exitance or tip irradiance (mW/cm2), and the irradiance received at the surface (also in mW/cm2) are used to describe the output from LCU. The concept of using an irradiance beam profile to map the radiant exposure (J/cm2) from the LCU is introduced. Results: Even small changes in the active tip diameter of the LCU will have a large effect on the radiant exitance. The emission spectra and the effects of distance on the irradiance delivered are not the same from all LCUs. The beam profile images show that using a single averaged irradiance value to describe the LCU can be very misleading. Some LCUs have ‘hot spots’ of high radiant exitance that far exceed the current ISO 10650 standard. Such inhomogeneity may cure the resin unevenly and may also be dangerous to soft tissues. Recommendations are made that will help the dentist when purchasing and then safely using the LCU. Conclusions: Dental manufacturers should report the radiant power from their LCU, the spectral radiant power, information about the compatibility of the emission spectrum from the LCU with the photoinitiators used, the active optical tip diameter, the radiant exitance, the effect of distance from the tip on the irradiance delivered, and the irradiance beam profile from the LCU.
Key words: Dental curing lights, light measurement techniques, beam profiling, fibre optic spectrometer, resin-based composites, light and optics terminology, radiant exposure
INTRODUCTION
The FDI World Dental Federation represents over one million dentists, most of whom will own and use a dental light-curing unit (LCU). This LCU and how it is used will affect the physical properties, biocompatibility and the clinical success of light-cured dental polymer systems (resin-based composites, adhesives, orthodontic resins, luting agents, sealants, etc.) that are used in the dental office1., 2., 3.. Of note, globally, there exists a large discrepancy between how long resin composite restorations are reported to last in well-controlled clinical trials4., 5., and how long they last when placed in most dental offices6., 7., 8., 9.. Although the reasons for these discrepancies in the long-term success of restorations are multifactorial, the general lack of understanding about the differences between LCUs, how to describe the output from the LCU, and how to use the LCU in everyday dentistry10., 11., 12., 13., 14., 15., 16., 17., 18., 19. may very well be contributing factors. Due to this lack of knowledge and information about the LCU and the consequences of inadequate light curing, the dentist may not use the LCU correctly, and they may purchase an inexpensive device from the Internet, thinking that all LCUs emit similar blue light and will have equivalent efficacy. This can result in the dentist unknowingly delivering less overall energy or the wrong wavelengths of light to photocure the resin in the mouth in comparison to the energy delivered in the vast majority of laboratory studies and in well-controlled clinical trials. After reading this article, the reader will know what to look for when purchasing and using a curing light. They will understand reasons why there can be considerable differences between LCUs, and why reliance upon a single reported irradiance value can be misleading.
Light-curing units
Small, battery-operated and energy-efficient light-emitting diode (LED) curing lights dominate the market10., 14., 18., 20.. The LCUs in Figure 1 offer different features but, unfortunately, the cost of the unit and a ‘high’ irradiance value greater than 1,000 mW/cm2 are the two main factors upon which many clinicians base their decision when purchasing a new LCU. However, there are considerable differences in the light output from almost all currently available LCUs that cannot be adequately described by an irradiance value alone21. Because most dentists were never taught what to look for when purchasing their next LCU, or how to use the LCU correctly, a meeting attended by over 50 key opinion leaders and manufacturers was held in 2014. At the conclusion, a consensus was achieved on what the clinician should look for when purchasing and using a new curing light22., 23., 24.. These recommendations are freely available to download22., 23..
Figure 1.
An assortment of light-emitting diode (LED) curing lights. Note the range of shapes and sizes.
Curing lights are medical devices
In most countries, dental LCUs are classified as medical devices, and it behooves the dentist to ensure that any medical device they use has been ‘cleared’ or ‘approved’ for use on patients25., 26., 27.. Indicators that a curing light should not be used on patients, or that the safety of the electrical components in the LCU and its charger, has not been verified, would be the lack of appropriate certification labels, poorly worded instructions for use, the lack of contact information should any harm or malfunction occur, or that the device is not listed as being cleared or approved on the regulatory authority database.
Describing the light-curing unit
Most manufacturers and researchers alike do not describe the light output from the LCUs in a consistent manner21., 28.. This has led to the unintentional dissemination of misinformation about the light sources21, or about the photo-curing requirements of light-cured dental polymer systems28., 29., 30.. Because the output from the LCU, the radiant exposure, and the wavelengths (nm) of light received by the light-cured dental polymer systems used in the vast majority of studies have often not been adequately reported28, clinical decisions based on the results and conclusions from these studies may not be valid.
To ensure that all parties are describing the light from the LCU using the same terms, the International System of Units (S.I.) should be used by manufacturers, researchers and clinicians alike (Table 1). While the current ISO 10650 standard31 provides much useful and important information, it is based on the assumption that the light output is homogeneously distributed across the light tip. This is not the case in many dental LCUs21., 32., 33., 34., 35., 36., 37.. In the standard31, the total radiant power (mW) is measured from the LCU and then divided by the optical cross-sectional area of the light guide/light-emitting tip to produce a single averaged radiant exitance value in mW/cm2. This radiant exitance at the light tip is the same as the irradiance (also in mW/cm2) at the light tip. The standard31 also requires that the radiant exitance in the 380–515 nm wavelength region should not be greater than 4,000 mW/cm2.
Table 1.
Glossary of S.I. radiometric terms used to describe the output from dental light curing units (LCUs)21., 29.
| Term | Unit commonly used in dentistry | Symbol | Explanation |
|---|---|---|---|
| Radiant energy | Joule | J | This is the energy emitted from the LCU |
| Radiant power (or radiant flux) | Watt | W or J/second | This is the energy per unit of time emitted from the LCU |
| Radiant exposure | Joule per square centimetre | J/cm2 | This is the energy received from the LCU per unit area |
| Radiant exitance, tip irradiance, or radiant emittance | milliWatts per square centimetre | mW/cm2 | This is the radiant power from a defined unit area. The radiant exitance is the same as the tip irradiance from the LCU at zero distance |
| Irradiance (incident irradiance) | milliWatts per square centimetre | mW/cm2 | This is the radiant power received by a unit area. It reflects an average value received over a defined area. |
| Emission spectrum | nanometres | Nm | These are the wavelengths of the light emitted from the LCU |
| Spectral radiant power | milliWatts per nanometre | mW/nm | This is the radiant power at a specific nm wavelength delivered from the LCU |
| Spectral irradiance | milliWatts per square centimetre per nanometre | mW/ cm2/nm | This is the irradiance received by a defined area at each nm of light emitted from the LCU |
Relationship between radiant power (radiant flux), active light-emitting area and radiant exitance (tip irradiance)
The use of budget priced LCUs that have often been purchased over the Internet is becoming popular16. Many of these budget LCUs appear to be equivalent to higher cost LCUs from quality manufacturers because these budget lights often claim similar radiant exitance (irradiance) values. However, the light output from these budget lights is often unstable and sometimes declines rapidly as the battery discharges38., 39., 40., 41.. In addition, most budget LCUs have only a small 6- or 7-mm diameter ‘active’ light tip from where useful light is emitted, whereas most lights from quality manufacturers have a 9–11+ mm active tip diameter42., 43.. Because the active area is calculated from the cross-sectional area, πr2, any reduction in the active tip diameter from where light is emitted will have a substantial effect on the tip area and the radiant exitance. For example, if the active tip diameter is reduced from 10 to 7 mm, the area from where light is emitted is halved from 78.6 mm2 to 38.5 mm2. This will double the radiant exitance. Consequently, without increasing the radiant power output from the LCU, a manufacturer can increase the radiant exitance (irradiance) by reducing the tip area. For this reason, comparing LCUs using the radiant exitance (tip irradiance) value alone without also knowing the radiant power from the LCU and the active optical tip diameter or the active tip area should be avoided21.
Effect of distance from the light tip
As the distance from the light tip increases, the irradiance received declines2., 44., 45., 46.. The effect of distance is not the same for all LCUs. This reduction in the irradiance received does not follow the ‘inverse-square law’ because the light from most LCUs is a somewhat focused beam of light. Some LCUs emit a well-collimated beam of light and, for others, the beam spreads out rapidly. Thus, manufacturers should report the radiant exitance not only at the light tip, (tip irradiance), but also the irradiance delivered at clinically relevant distances up to 10 mm away.
Emission spectrum
Dentists can now purchase light-cured resin systems that use a variety of alternative photoinitiators in addition to or as replacements for camphorquinone (CQ), and they can also buy LCUs that emit different emission spectra of light1., 2., 21.. The CQ initiator that is used in almost all dental resins is most efficiently activated by blue light at 468 nm. However, CQ is yellow, and some manufacturers use several other photoinitiators that are less yellow and are more efficient than CQ. These initiators are usually most sensitive to ultraviolet or violet light between 380 and 410 nm1., 2., 47., 48..
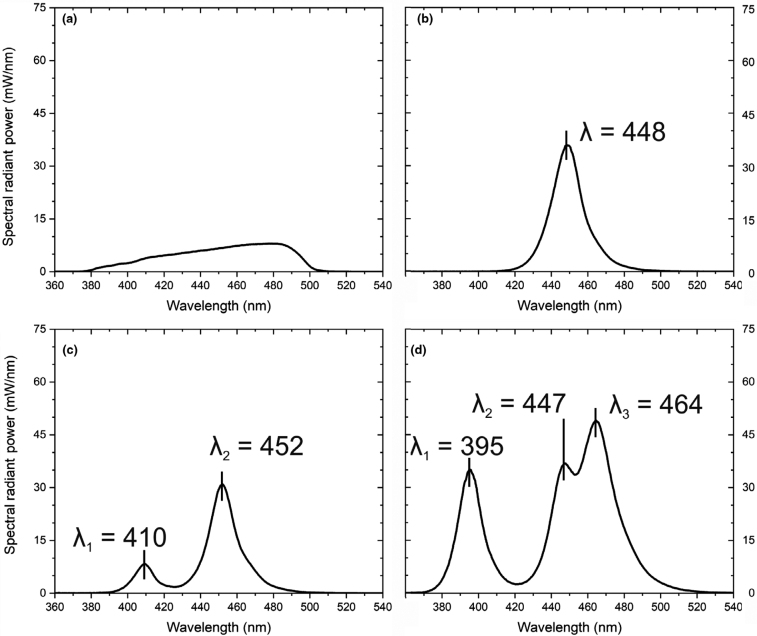
In contrast to quartz-tungsten-halogen (QTH) curing lights that emitted a broad spectrum of both violet and blue light (Figure 2a), the LED emitter used in many contemporary LCUs can only produce light over a limited spectral range (Figure 2b). Thus, single-peak LED curing lights that deliver very little light below 420 nm are not ideal LCUs to activate the initiators that require violet light1., 2., 21.. However, the differences between the resin-based products or between LCUs are not readily apparent to the purchaser because all LCUs will activate the CQ initiator that is used in almost all resin-based products and the top surface of the resin will feel hard. Consequently, the dentist may not realise that their LCU does not deliver light below 420 nm and thus cannot activate the additional photoinitiators.
Figure 2.
Emission spectra (nm) from (a) a quartz-tungsten-halogen (QTH), (b) a single-peak light-emitting diode (LED), (c) a dual-peak, and (d) a multi-peak LED curing light. To the human observer, the light-curing units (LCUs) will appear to emit similar ‘blue’ light.
To better activate these alternative photoinitiators, some LED curing lights (Figure 2c,d) now include additional LED emitters that produce additional light in the violet range of wavelengths2., 20., 21., 32., 36.. Figure 2(c,d) illustrates that the number and location of these violet and blue light emission peaks can vary between manufacturers, as does the relative contribution of each wavelength peak to the total radiant power output from the LCU. However, unless the LCU is carefully designed, the addition of several different wavelength LED emitters in the LCU can negatively affect the total amount of blue light present and the overall uniformity of the emitted light beam. This will then change the spectral irradiance received across the resin surface, which may then produce an uneven polymerisation within the RBC2., 21., 32., 36., 49., 50..
Light beam irradiance uniformity
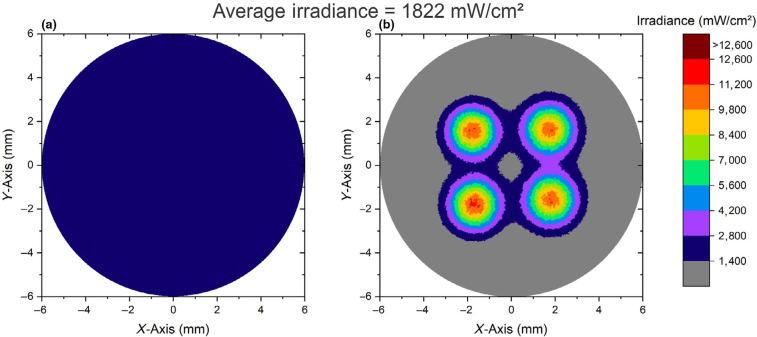
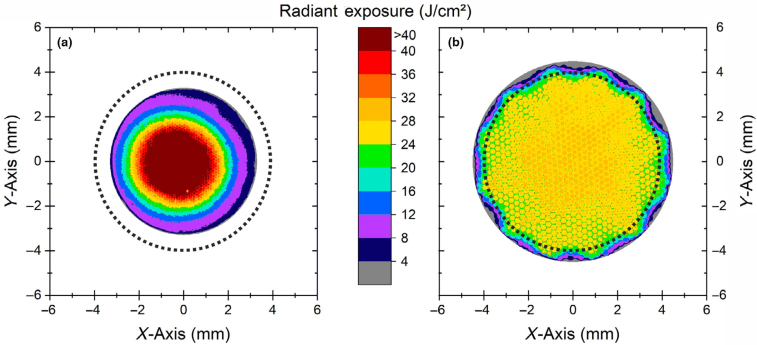
Beam profiling using a digital camera is used to examine the uniformity of light beams51., 52.. The beam-profiling software can produce both two-dimensional and three-dimensional images of the radiant exitance across the tip of the light source as well as numerical data about the light source51., 52.. The two images in Figure 3 illustrate the difference between the single averaged irradiance value provided by the ISO 10650 standard31 and the information provided by a beam profile from the same LCU. In Figure 3(a), the radiant power was divided by the optical tip area to produce an averaged radiant exitance of 1,822 mW/cm2. The image captured by the beam profile camera in Figure 3(b) shows why this information can be misleading. Although the average radiant exitance is still 1,822 mW/cm2, there are four ‘hot spots’of high radiant exitance that are above 12,600 mW/cm2, and other regions where the light output is lower. These four ‘hot spots’ deliver three times the maximum irradiance of 4,000 mW/cm2 allowed in the ISO 10650 standard31and six times more than the 2,000 mW/cm2 maximum value recommended in the 2014 consensus document22
Figure 3.
This light-curing unit (LCU) had an averaged radiant exitance of 1,822 mW/cm2. The figure depicts the anticipated beam profile (a) that was obtained from the quotient of the power and area (as per the ISO 10650 standard). (b) The actual scaled irradiance beam profile of the same LCU showing that although the average radiant exitance is still 1,822 mW/cm2, there are four ‘hot spots’ where the radiant exitance is above 12,600 mW/cm2 surrounded by regions of lower radiant exitance.
Light beam spectral uniformity
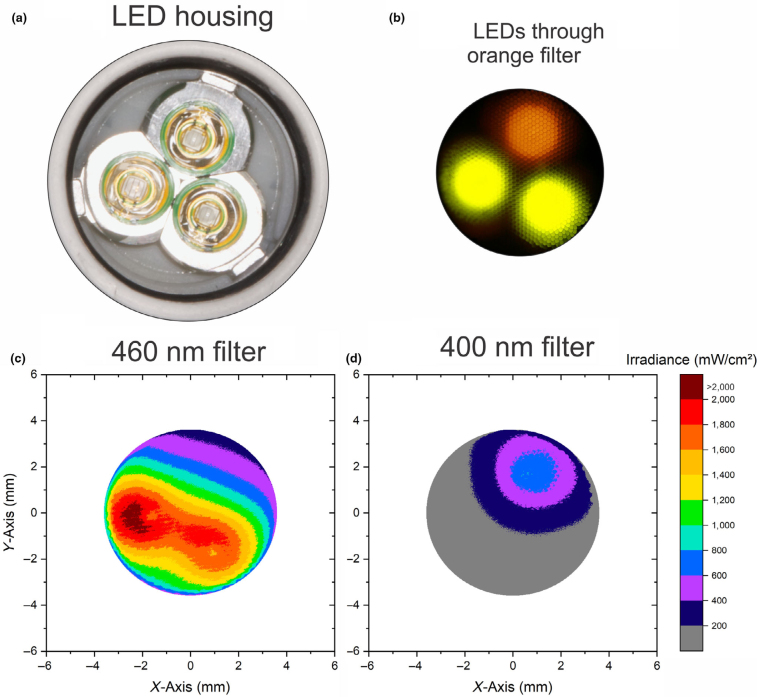
Figure 4 illustrates the beam profile of one dual-wavelength peak LED curing light that has one violet light and two blue LED emitters in the LCU. When the light output at the tip is viewed through blue-light-blocking orange glasses, the output from the one violet and two blue LEDs is visible, and ‘hot spots’ of high irradiance are also evident. The image clearly shows that the light is not well mixed. When the tip irradiance from the same LCU is viewed using a beam profiler camera through narrow bandpass filters that only allow either violet (400 ± 5 nm) or blue (460 ± 5 nm) wavelengths of light through, the spectral uniformity of the light emitted from the LCU in the violet and blue regions becomes quantifiable33., 36., 49.. Thus, dentists should look for a good optical design in the LCU that can homogenise the light so that both the irradiance and the emission spectrum are uniformly distributed across the light tip, that is there are no ‘hot spots’.
Figure 4.
This figure illustrates how the reader can view the light output from a dual-peak light-curing unit (LCU) through orange blue-light-blocking glasses. The distribution of the wavelengths and the tip irradiance are clearly not uniform (b). Instead, they correspond to the location (a) of the two blue and one violet light-emitting diode (LED) emitters in the LCU housing. When the same light is imaged through either (c) a 460 ± 5 nm or (d) a 400 ± 5 nm narrow bandpass filter into a beam profiler camera, the irradiance received in each region can be measured.
Active diameter of light beam
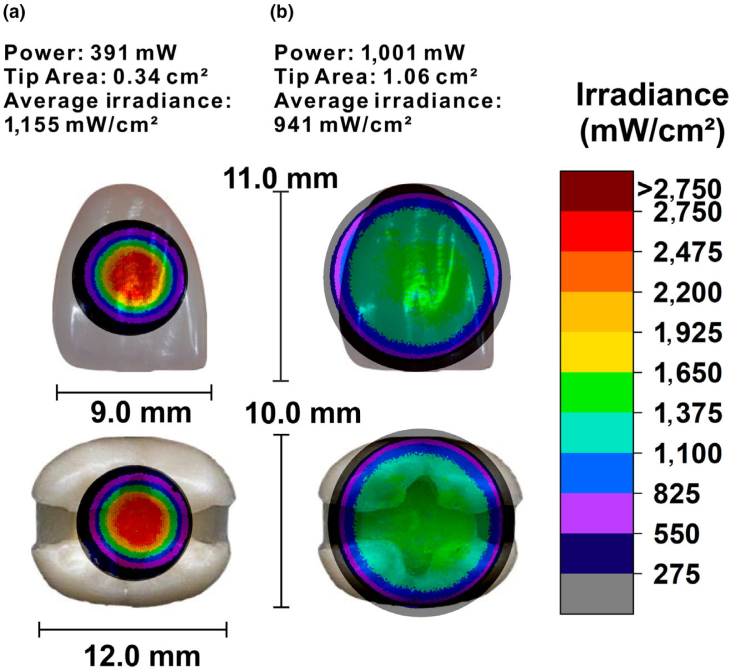
The beam profile also shows the active diameter of the tip from where light is emitted. This active tip diameter is important because any RBC that is not covered by the active region of the light tip will be less well polymerised53., 54., and most laboratory studies only evaluate the ability of the LCU to polymerise the resin that is directly under the centre 4-mm diameter region, not at the edges54. Based on a favourable report, clinicians may then attempt to light cure the entire adhesive layer in mesial-occlusal-distal (MOD) cavities using just one exposure and, if using a bulk-fill resin-composite, they may then also light cure the restoration as a whole using only one light exposure. The clinician may not realise that in order to adequately light cure the entire surface of the cavity preparation or restoration with a single exposure, the active light tip area should completely cover the whole surface. To be practical, an overlap of 1 mm beyond the restoration would be ideal, as this will allow for some small movements at the light tip. Because the active optical diameter of many LCU tips is smaller than a MOD preparation in a molar tooth14., 21., 32., 42., 43., 45., 55., the likely result will be that the adhesive and the resin at the bottom of the proximal boxes will be inadequately polymerised in just one exposure. Instead, multiple exposures from different locations are required. To illustrate this effect, the beam profiles of two different curing lights, one with an 11.6-mm active optical tip diameter and the other with a 6.6-mm active optical tip diameter, were superimposed over a maxillary central incisor and a mandibular first molar tooth (Figure 5). The differences in both the width and uniformity of light coverage over the teeth are striking. However, although a wide tip may appear to be preferred, if the light tip also covers the gingiva, the soft tissues may be burnt if the tip irradiance is too high, or the LCU is used incorrectly56., 57.. Consequently, a narrower tip (6–8 mm in diameter) is indicated for curing small increments of RBC, or Class V restorations that are close to the gingiva.
Figure 5.
Two-dimensional irradiance beam profile of the tip of (a) and (b) curing lights scaled to 2,750 mW/cm2 and superimposed over a maxillary central incisor or a mandibular first molar. Both lights deliver a similar average irradiance (1,155 mW/cm2 and 941 mW/cm2), but very different radiant power outputs and tip diameters. Light (a) has a small tip size and an undesirable irradiance hot spot of 2,750 mW/cm2 at the centre, whereas (b) has a lower, but more uniform, irradiance at about 1,200 mW/cm2 that covers most of the occlusal surface of the molar or the maxillary central incisor tooth.
Radiant exposure uniformity
It has been suggested that each 2-mm-thick increment of RBC should receive approximately 16 J/cm2 in order to be adequately photo-cured58. Consequently, a novel approach using the data acquired from beam profiling is to multiply the irradiance (mW/cm2) by the exposure time (seconds) to produce a map of the radiant exposure (J/cm2). When this is done, it can be seen that LCU (a) in Figure 6 does not deliver a uniform amount of energy across the light tip. Outside of the energy ‘hot spot’ at the centre, LCU (a) will emit less than 16 J/cm2 in 20 seconds, and here the resin will not be as well photo-cured as in the centre. Light (b) has a lower, but more uniform, irradiance at about 1,200 mW/cm2 that covers most of an 8-mm-diameter circle with over 24 J/cm2 in 20 seconds. Clinically, if the beam profile consists of a small region of high irradiance compared with a more even 8–10-mm diameter of uniform irradiance, this means that the light tip must be very accurately positioned over the target, and the resin at the edges may receive an insufficient amount of light54.
Figure 6.
Radiant exposure (J/cm2) delivered by two lights in 20 seconds. An 8-mm-diameter circle is drawn on both images. Note the smaller tip diameter and the uneven radiant exposure from light (a) compared with light (b) that emits more than 24 J/cm2 uniformly across the 8-mm-diameter circle. Light (b), in comparison, has a ‘hot spot’ of high irradiance at the centre. This information would not be revealed in ISO 10650.
Light-curing unit ergonomics
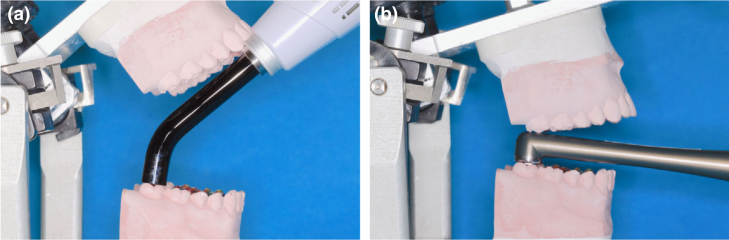
In most laboratory experiments, direct access to the material to be cured is rarely a factor1, and the light tip is precisely and rigidly positioned over the centre of the specimens. However, when used clinically, Figure 7(a) illustrates how the design of the LCU may prevent the light tip from achieving optimal access to all locations in the mouth42., 43.. This may cause the operator to increase the curing distance or angle the light tip. Doing so will reduce the amount of energy delivered and reduce the ultimate polymerisation of the RBC3., 59., 60.. Consequently, a low-profile head (Figure 7b) that will allow better access to the posterior teeth is recommended42., 43., 45.. The light tip should also be positioned both as close to the surface of the resin as is possible and perpendicular to the surface of the resin throughout the exposure cycle19., 61., 62., 63., 64., 65. (Figure 7b). Some manufacturers are now producing LCUs with sensing technologies that help the operator keep the LCU tip over the tooth66., 67.. If the light tip moves away from the tooth, the LCU first vibrates and then, if moved further away, the LCU turns off. This feature is similar to the ‘lane assist’ technology in cars, and should help the dentist keep the LCU tip on target and over the resin.
Figure 7.
Although the light-curing unit (LCU) may work well on the laboratory bench, the design of the LCU will affect access to some teeth (a). A low-profile head (b) is preferred as it will allow better access to the posterior teeth.
Blue light hazard
The dentist must protect the patient from harm, and employers should furnish a place of employment that is free from hazards that are causing or are likely to cause harm to their employees25., 68.. Most contemporary dental LED curing lights emit light between 430 and 480 nm, and the most damaging wavelengths of blue light to the retina are thought to be around 440 nm69. Exposure to blue light has also been reported to affect sleep patterns25., 70., 71.. Although a ‘blue light hazard’ to the retina has not yet been shown to occur in humans, dental personnel may be both chronically and acutely exposed to much greater high levels of blue light than the general population. Because this potential ‘blue light hazard’ can be prevented by using the appropriate blue-light-blocking eye protection, it is recommended that appropriate eye protection in the form of orange ‘blue-blocking’ paddles, shields or eyewear should be used whenever the dental LCU is used18., 25., 72., 73., 74., 75.. Watching the position of the light tip while photo-curing will help ensure that the tip is kept over and close to the resin so that the bottom of the restoration will be adequately polymerised19., 54., 61., 62., 63., 64., 65..
Infection control
It is important to recognise that the LCU can be a significant source of cross-contamination76., 77., and the manufacturer’s instructions for disinfecting the LCU between each patient should be followed. Ideally, the LCU should have removable, autoclavable light guides and easily disinfected surfaces. However, an autoclavable light guide is impractical for many LCUs that do not use a light guide and instead have the LED emitter at the light tip (Figure 1). Of note, repeated autoclaving of fibre optic light guides can reduce the light output78, and some surface disinfectants may both reduce the light transmission through the light guides and degrade the plastic LCU body79., 80.. In addition to wiping the LCU with the recommended surface disinfectants for the recommended time, plastic barriers or sleeves can be used to cover the LCU. However, the user must recognise that covering the light tip with an infection control barrier can reduce the irradiance delivered from the LCU by as much as 40%81., 82.. Thus, the output from the LCU should be regularly checked using a digital radiometer such as the Bluephase Meter II (Ivoclar Vivadent, Schaan, Liechtenstein) both without and with the same type of barrier that will be used on the LCU when treating patients. Then, depending on the percent decrease in the radiant exitance caused by the barrier, the clinician should increase the exposure times that they would use in the mouth81., 82., 83., 84.. The Bluephase Meter II has been shown to be an accurate (± 10%) dental radiometer that can measure the radiant power and, when the tip diameter is entered, this meter device can also report the radiant exitance85., 86.. As an added benefit, when the dentist measures the output from their LCU, they quickly realise the effects of battery discharge38., 39., 40., 41., 43., the barrier they use81., 82., 83., 84., and both tip angulation and distance23., 44., 45., 46., 60. have on the light received.
CONCLUSIONS
Globally there exists a large discrepancy between how long resin composite restorations are reported to last in well-controlled clinical trials4., 5., and how long they last when placed in most dental offices6., 7., 8., 9.. There may be many reasons for this discrepancy, but the general lack of understanding about the differences between LCUs, how to describe the output from the LCU, and how to use the LCU in everyday dentistry10., 11., 12., 13., 14., 15., 16., 17., 18., 19. may be contributing factors. The beam profile images (Figure 3., Figure 4., Figure 5., Figure 6.) show that the single averaged ‘irradiance’ value used in the ISO 10650-standard31 to describe the output from the LCU should be interpreted with caution. It is recommended that dental manufacturers and, where appropriate, the researcher should report the radiant power from the LCU, the spectral radiant power, information about the compatibility of the emission spectrum from the LCU with the photoinitiators used in dental resins, the active optical tip diameter from where the light is emitted, the radiant exitance at the light tip, the likely effect that distance from the tip will have on the irradiance received by a restoration, and the irradiance beam profile from the LCU. Clinicians should: (i) ensure that the LCU has been ‘cleared’/‘approved’ for use in their country; (ii) regularly monitor the output from the LCU and take corrective action should the LCU output start to fall; (iii) follow the instructions for use; (iv) use an appropriate light tip diameter for the size of the restoration; (v) keep the light tip close and perpendicular to the resin; (vi) use appropriate eye protection; and (vii) use appropriate disinfection procedures.
ACKNOWLEDGEMENTS
The authors wish to thank Dr S. Braga and Dr C. Soares for their assistance in generating the images, and Professors F. Rueggeberg and D. Labrie for their valuable input about how to describe dental curing lights.
Conflict of interest
The authors state that they have no conflict of interest. Richard Price is the inventor of the MARC patient simulator that is marketed by BlueLight Analytics, Halifax, Canada, but he has not been associated with the company since 2012. Jack Ferracane is listed on an external advisory board for BlueLight Analytics. This appointment was made years ago, and he has not performed any duties for the company within approximately the past 5 years. Reinhard Hickel declares no conflict of interest.
REFERENCES
- 1.Cadenaro M, Maravic T, Comba A, et al. The role of polymerization in adhesive dentistry. Dent Mater. 2019;35:e1–e22. doi: 10.1016/j.dental.2018.11.012. [DOI] [PubMed] [Google Scholar]
- 2.Rueggeberg FA, Giannini M, Arrais CAG, et al. Light curing in dentistry and clinical implications: a literature review. Braz Oral Res. 2017;31:e61. doi: 10.1590/1807-3107BOR-2017.vol31.0061. [DOI] [PubMed] [Google Scholar]
- 3.Maktabi H, Ibrahim M, Alkhubaizi Q, et al. Underperforming light curing procedures trigger detrimental irradiance-dependent biofilm response on incrementally placed dental composites. J Dent. 2019;88:103–110. doi: 10.1016/j.jdent.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 4.van Dijken JWV, Pallesen U. Bulk-filled posterior resin restorations based on stress-decreasing resin technology: a randomized, controlled 6-year evaluation. Eur J Oral Sci. 2017;125:303–309. doi: 10.1111/eos.12351. [DOI] [PubMed] [Google Scholar]
- 5.Opdam NJ, van de Sande FH, Bronkhorst E, et al. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dent Res. 2014;93:943–949. doi: 10.1177/0022034514544217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rho YJ, Namgung C, Jin BH, et al. Longevity of direct restorations in stress-bearing posterior cavities: a retrospective study. Oper Dent. 2013;38:572–582. doi: 10.2341/12-432-C. [DOI] [PubMed] [Google Scholar]
- 7.Astvaldsdottir A, Dagerhamn J, van Dijken JW, et al. Longevity of posterior resin composite restorations in adults - a systematic review. J Dent. 2015;43:934–954. doi: 10.1016/j.jdent.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Palotie U, Eronen AK, Vehkalahti K, et al. Longevity of 2- and 3-surface restorations in posterior teeth of 25- to 30-year-olds attending Public Dental Service-A 13-year observation. J Dent. 2017;62:13–17. doi: 10.1016/j.jdent.2017.05.012. [DOI] [PubMed] [Google Scholar]
- 9.Pummer A, Cieplik F, Nikolic M, et al. Longevity of posterior composite and compomer restorations in children placed under different types of anesthesia: a retrospective 5-year study. Clin Oral Investig. 2020;24:141–150. doi: 10.1007/s00784-019-02911-2. [DOI] [PubMed] [Google Scholar]
- 10.Swathi T, Madhusudhana K, Suneelkumar C, et al. A clinical survey of the output intensity of light curing units in dental offices across Nellore urban area. SRM J Res Dental Sci. 2016;7:64–68. [Google Scholar]
- 11.Kopperud SE, Rukke HV, Kopperud HM, et al. Light curing procedures - performance, knowledge level and safety awareness among dentists. J Dent. 2017;58:67–73. doi: 10.1016/j.jdent.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Ernst CP, Price RB, Callaway A, et al. Visible light curing devices - irradiance and use in 302 German dental offices. J Adhes Dent. 2018;20:41–55. doi: 10.3290/j.jad.a39881. [DOI] [PubMed] [Google Scholar]
- 13.Alqabbaa LM, Alsenani MS, Alsaif NS, et al. Light intensity output of visible light communication units and clinicians’ knowledge and attitude among Riyadh private clinics. J Conserv Dent. 2018;21:667–670. doi: 10.4103/JCD.JCD_252_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bansal R, Bansal M, Walia S, et al. Assessment of efficacy and maintenance of light-curing units in dental offices across Punjab: a clinical survey. Indian J Dental Sci. 2019;11:42–45. [Google Scholar]
- 15.de Oliveira DCRS, Rocha MG, Roulet J-F. Light curing matters: facts often overseen by dentists. Stomatology Edu Journal. 2018;5:236–242. [Google Scholar]
- 16.Omidi BR, Gosili A, Jaber-Ansari M, et al. Intensity output and effectiveness of light curing units in dental offices. J Clin Exp Dent. 2018;10:e555–e560. doi: 10.4317/jced.54756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee HA. Clinical considerations in the use of dental light curing unit. J Korean Dent Association. 2019;57:175–184. [Google Scholar]
- 18.Georgiev GP. Factors associated with light curing units: a questionnaire survey. Scripta Scientifica Medicinae Dentalis. 2019;5(2):41–47. [Google Scholar]
- 19.Suliman AA, Abdo AA, Elmasmari HA. Training and experience effect on light-curing efficiency by dental practitioners. J Dent Educ 2020. in press. 10.1002/jdd.12113. [DOI] [PubMed]
- 20.Jandt KD, Mills RW. A brief history of LED photopolymerization. Dent Mater. 2013;29:605–617. doi: 10.1016/j.dental.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Price RB, Ferracane JL, Shortall AC. Light-curing units: a review of what we need to know. J Dent Res. 2015;94:1179–1186. doi: 10.1177/0022034515594786. [DOI] [PubMed] [Google Scholar]
- 22.Price RB. Light curing guidelines for practitioners: a consensus statement from the 2014 symposium on light curing in dentistry, Dalhousie University, Halifax, Canada. J Can Dent Assoc. 2014;80:e61. [PubMed] [Google Scholar]
- 23.Price RB, Strassler H, Oxman JD, et al. Light curing: tips on choosing your next curing light. CDA Essentials. 2016;3:30–33. [Google Scholar]
- 24.Roulet JF, Price R. Light curing - guidelines for practitioners - a consensus statement from the 2014 symposium on light curing in dentistry held at Dalhousie University, Halifax, Canada. J Adhes Dent. 2014;16:303–304. doi: 10.3290/j.jad.a32610. [DOI] [PubMed] [Google Scholar]
- 25.Fluent MT, Ferracane JL, Mace JG, et al. Shedding light on a potential hazard: Dental light-curing units. J Am Dent Assoc. 2019;150:1051–1058. doi: 10.1016/j.adaj.2019.08.012. [DOI] [PubMed] [Google Scholar]
- 26.US Food and Drug Administration . US FDA; Silver Spring, MD: 2019. Sec. 872.6070 Ultraviolet Activator for Polymerization. Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=872.6070. Accessed 25 January 2020. [Google Scholar]
- 27.European Commission Manual on borderline and classification in the community regulatory framework for medical devices. 2019. Available from: https://ec.europa.eu/docsroom/documents/35582. Accessed 25 January 2020.
- 28.Watts DC, Kaiser C, O’Neill C, et al. Reporting of light irradiation conditions in 300 laboratory studies of resin-composites. Dent Mater. 2019;35:414–421. doi: 10.1016/j.dental.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 29.Kirkpatrick SJ. A primer on radiometry. Dent Mater. 2005;21:21–26. doi: 10.1016/j.dental.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 30.Price RB. Guest Editorial: Is your study reproducible? What "light" are you delivering to your specimens? J Adhes Dent. 2018;20:375. doi: 10.3290/j.jad.a41424. [DOI] [PubMed] [Google Scholar]
- 31.ISO 10650 . Second Edition. International Standards Organization; Geneva, Switzerland: 2018. Dentistry-Powered Polymerization Activators; p. 3. 5.2.2. [Google Scholar]
- 32.Michaud PL, Price RB, Labrie D, et al. Localised irradiance distribution found in dental light curing units. J Dent. 2014;42:129–139. doi: 10.1016/j.jdent.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 33.Price RB, Labrie D, Rueggeberg FA, et al. Irradiance differences in the violet (405 nm) and blue (460 nm) spectral ranges among dental light-curing units. J Esthet Restor Dent. 2010;22:363–377. doi: 10.1111/j.1708-8240.2010.00368.x. [DOI] [PubMed] [Google Scholar]
- 34.Laboratory evaluation of light-emitting diode curing lights. The ADA Professional Product Review. 2014:9. Sarrett D, editor. [Google Scholar]
- 35.Harlow JE, Sullivan B, Shortall AC, et al. Characterizing the output settings of dental curing lights. J Dent. 2016;44:20–26. doi: 10.1016/j.jdent.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 36.Soto-Montero J, Nima G, Rueggeberg FA et al. Influence of multiple peak light-emitting-diode curing unit beam homogenization tips on microhardness of resin composites. Oper Dent 2019. 10.2341/19-027-L [DOI] [PubMed]
- 37.Juckes SM, Sullivan B, Kostylev I, et al. Three-dimensional beam profiling used to characterize dental light-curing units. Appl Opt. 2019;58:9540–9547. doi: 10.1364/AO.58.009540. [DOI] [PubMed] [Google Scholar]
- 38.Tongtaksin A, Leevailoj C. Battery charge affects the stability of light intensity from light-emitting diode light-curing units. Oper Dent. 2017;42:497–504. doi: 10.2341/15-294-L. [DOI] [PubMed] [Google Scholar]
- 39.Ozkan S, Gollerli YY. Effects of declining battery voltage on light intensity and power consumption of light-curing. J Clin Orthod. 2017;51:411–418. [PubMed] [Google Scholar]
- 40.AlShaafi MM, Harlow JE, Price HL, et al. Emission characteristics and effect of battery drain in "Budget" curing lights. Oper Dent. 2016;41:397–408. doi: 10.2341/14-281-L. [DOI] [PubMed] [Google Scholar]
- 41.Cardoso IO, Machado AC, Teixeira D et al. Influence of different cordless light-emitting-diode units and battery levels on chemical, mechanical, and physical properties of composite resin. Oper Dent 2019. 10.2341/19-095-L [DOI] [PubMed]
- 42.Soares CJ, Rodrigues MP, Oliveira LRS, et al. An evaluation of the light output from 22 contemporary light curing units. Braz Dent J. 2017;28:362–371. doi: 10.1590/0103-6440201601466. [DOI] [PubMed] [Google Scholar]
- 43.Andre CB, Nima G, Sebold M, et al. Stability of the light output, oral cavity tip accessibility in posterior region and emission spectrum of light-curing units. Oper Dent. 2018;43:398–407. doi: 10.2341/17-033-L. [DOI] [PubMed] [Google Scholar]
- 44.Price RB, Derand T, Sedarous M, et al. Effect of distance on the power density from two light guides. J Esthet Dent. 2000;12:320–327. doi: 10.1111/j.1708-8240.2000.tb00241.x. [DOI] [PubMed] [Google Scholar]
- 45.Shortall AC, Price RB, MacKenzie L, et al. Guidelines for the selection, use, and maintenance of LED light-curing units - part 1. Br Dent J. 2016;221:453–460. doi: 10.1038/sj.bdj.2016.772. [DOI] [PubMed] [Google Scholar]
- 46.Almuallem Z, McDonnell S, Busuttil-Naudi A, et al. The effect of irradiation distance on light transmittance and vickers hardness ratio of two bulk-fill resin-based composites. Eur J Prosthodont Restor Dent. 2016;24:203–214. doi: 10.1922/EJPRD_1576Almuallem12. [DOI] [PubMed] [Google Scholar]
- 47.Moszner N, Fischer UK, Ganster B, et al. Benzoyl germanium derivatives as novel visible light photoinitiators for dental materials. Dent Mater. 2008;24:901–907. doi: 10.1016/j.dental.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 48.Burtscher P. Ivocerin in comparison to camphorquinone. 2013. Ivoclar Vivadent Report, No. 19, July.
- 49.Price RB, Labrie D, Rueggeberg FA, et al. Correlation between the beam profile from a curing light and the microhardness of four resins. Dent Mater. 2014;30:1345–1357. doi: 10.1016/j.dental.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 50.Issa Y, Watts DC, Boyd D, et al. Effect of curing light emission spectrum on the nanohardness and elastic modulus of two bulk-fill resin composites. Dent Mater. 2016;32:535–550. doi: 10.1016/j.dental.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 51.Dickey FM. 2nd edn. CRC Press, Taylor & Francis Group; Boca Raton: 2014. Laser Beam Shaping: Theory and Techniques. [Google Scholar]
- 52.ISO 11146–1:2005 . International Standards Organization; Geneva: 2005. Lasers and Laser-Related Equipment - Test Methods for Laser Beam Widths, Divergence Angles and Beam Propagation Ratios - Part 1: Stigmatic and Simple Astigmatic Beams; p. 16. [Google Scholar]
- 53.Li X, Pongprueksa P, Van Meerbeek B, et al. Curing profile of bulk-fill resin-based composites. J Dent. 2015;43:664–672. doi: 10.1016/j.jdent.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 54.Shimokawa C, Turbino ML, Giannini M et al. Effect of curing light and exposure time on the polymerization of bulk-fill resin-based composites in molar teeth. Oper Dent 2020. 10.2341/19-126-L [DOI] [PubMed]
- 55.Ash MM, Nelson SJ, Ash MM. 8th edn. W.B. Saunders; Philadelphia, PA: 2003. Wheeler’s Dental Anatomy, Physiology, and Occlusion. [Google Scholar]
- 56.Spranley TJ, Winkler M, Dagate J, et al. Curing light burns. Gen Dent. 2012;60:e210–e214. [PubMed] [Google Scholar]
- 57.Maucoski C, Zarpellon DC, Dos Santos FA, et al. Analysis of temperature increase in swine gingiva after exposure to a Polywave(®) LED light curing unit. Dent Mater. 2017;33:1266–1273. doi: 10.1016/j.dental.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 58.Anusavice KJ, Phillips RW, Shen C, et al. 12th edn. Elsevier/Saunders; St Louis, MO: 2013. Phillips’ Science of Dental Materials; p. 290. Chapter 13. [Google Scholar]
- 59.Price RB, McLeod ME, Felix CM. Quantifying light energy delivered to a Class I restoration. J Can Dent Assoc. 2010;76:a23. [PubMed] [Google Scholar]
- 60.Konerding KL, Heyder M, Kranz S, et al. Study of energy transfer by different light curing units into a class III restoration as a function of tilt angle and distance, using a MARC Patient Simulator (PS) Dent Mater. 2016;32:676–686. doi: 10.1016/j.dental.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 61.Soares CJ, Braganca GF, Pereira R, et al. Irradiance and radiant exposures delivered by LED light-curing units used by a left and right-handed operator. Braz Dent J. 2018;29:282–289. doi: 10.1590/0103-6440201802127. [DOI] [PubMed] [Google Scholar]
- 62.Samaha S, Bhatt S, Finkelman M, et al. Effect of instruction, light curing unit, and location in the mouth on the energy delivered to simulated restorations. Am J Dent. 2017;30:343–349. [PubMed] [Google Scholar]
- 63.Federlin M, Price R. Improving light-curing instruction in dental school. J Dent Educ. 2013;77:764–772. [PubMed] [Google Scholar]
- 64.Price RB, Felix CM, Whalen JM. Factors affecting the energy delivered to simulated class I and class v preparations. J Can Dent Assoc. 2010;76:a94. [PubMed] [Google Scholar]
- 65.Kojic DD, El-Mowafy O, Price R, et al. Efficacy of light-emitting diode light polymerization units used in private practices in Toronto, Ontario, Canada. J Am Dent Assoc. 2019;150:802–808. doi: 10.1016/j.adaj.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 66.Shortall AC, Palin WM, Jacquot B, et al. Advances in light-curing units: four generations of LED lights and clinical implications for optimizing their use: part 2. From present to future. Dent Update. 2012;39(13–17):20. doi: 10.12968/denu.2012.39.1.13. [DOI] [PubMed] [Google Scholar]
- 67.Ivoclar Vivadent Bluephase G4 Instructions for Use. 2019. Available from: http://www.ivoclarvivadent.com/en/p/all/bluephase-g4. Accessed 1 May 2019.
- 68.United States Department of Labor. Occupational Safety and Health Organization Act of 1970: General Duty Clause. Available from: https://www.osha.gov/laws-regs/oshact/section5-duties.
- 69.ACGIH; Cincinnati, OH: 2017. American Conference of Governmental Industrial Hygienists TLVs and BEIs Based on the Documentation for Threshold Limit Values for Chemical Substances and Physical Agents and Biological Exposure Indices. ISBN: 978-1-607260-90-5. [Google Scholar]
- 70.Nagai N, Ayaki M, Yanagawa T, et al. Suppression of blue light at night ameliorates metabolic abnormalities by controlling circadian rhythms. Invest Ophthalmol Vis Sci. 2019;60:3786–3793. doi: 10.1167/iovs.19-27195. [DOI] [PubMed] [Google Scholar]
- 71.Tosini G, Ferguson I, Tsubota K. Effects of blue light on the circadian system and eye physiology. Mol Vis. 2016;22:61–72. [PMC free article] [PubMed] [Google Scholar]
- 72.The effects of blue light on the retina and the use of protective filtering glasses. Council on Dental Materials, Instruments, and Equipment. J Am Dent Assoc. 1986;112:533–535. doi: 10.14219/jada.archive.1986.0038. [DOI] [PubMed] [Google Scholar]
- 73.Bruzell EM, Johnsen B, Aalerud TN, et al. Evaluation of eye protection filters for use with dental curing and bleaching lamps. J Occup Environ Hyg. 2007;4:432–439. doi: 10.1080/15459620701354218. [DOI] [PubMed] [Google Scholar]
- 74.Soares CJ, Rodrigues MP, Vilela AB, et al. Evaluation of eye protection filters used with broad-spectrum and conventional LED curing lights. Braz Dent J. 2017;28:9–15. doi: 10.1590/0103-6440201701380. [DOI] [PubMed] [Google Scholar]
- 75.Alasiri RA, Algarni HA, Alasiri RA. Ocular hazards of curing light units used in dental practice - a systematic review. Saudi Dent J. 2019;31:173–180. doi: 10.1016/j.sdentj.2019.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Caughman WF, O’Connor RP, Volkmann KR, et al. Visible-light-curing devices: a potential source of disease transmission. Oper Dent. 1987;12:10–14. [PubMed] [Google Scholar]
- 77.Janoowalla Z, Porter K, Shortall ACC, et al. Microbial contamination of light curing units: a pilot study. J Infect Prev. 2010;11:217–221. [Google Scholar]
- 78.Caughman GB, Caughman WF, Napier N, et al. Disinfection of visible-light-curing devices. Oper Dent. 1989;14:2–7. [PubMed] [Google Scholar]
- 79.Nelson SK, Caughman WF, Rueggeberg FA, et al. Effect of glutaraldehyde cold sterilants on light transmission of curing tips. Quintessence Int. 1997;28:725–730. [PubMed] [Google Scholar]
- 80.Kakaboura A, Tzoutzas J, Pitsinigos D, et al. The effect of sterilization methods on the light transmission characteristics and structure of light-curing tips. J Oral Rehabil. 2004;31:918–923. doi: 10.1111/j.1365-2842.2004.01314.x. [DOI] [PubMed] [Google Scholar]
- 81.McAndrew R, Lynch CD, Pavli M, et al. The effect of disposable infection control barriers and physical damage on the power output of light curing units and light curing tips. Br Dent J. 2011;210:E12. doi: 10.1038/sj.bdj.2011.312. [DOI] [PubMed] [Google Scholar]
- 82.Ajaj RA, Nassar HM, Hasanain FA. Infection control barrier and curing time as factors affecting the irradiance of light-cure units. J Int Soc Prev Community Dent. 2018;8:523–528. doi: 10.4103/jispcd.JISPCD_226_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Pollington S, Kahakachchi N, van Noort R. The influence of plastic light cure sheaths on the hardness of resin composite. Oper Dent. 2009;34:741–745. doi: 10.2341/09-024-L. [DOI] [PubMed] [Google Scholar]
- 84.Hwang IN, Hong SO, Lee BN, et al. Effect of a multi-layer infection control barrier on the micro-hardness of a composite resin. J Appl Oral Sci. 2012;20:576–580. doi: 10.1590/S1678-77572012000500014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Shimokawa CA, Harlow JE, Turbino ML, et al. Ability of four dental radiometers to measure the light output from nine curing lights. J Dent. 2016;54:48–55. doi: 10.1016/j.jdent.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 86.Giannini M, Andre CB, Gobbo VC, et al. Accuracy of irradiance and power of light-curing units measured with handheld or laboratory grade radiometers. Braz Dent J. 2019;30:397–403. doi: 10.1590/0103-6440201902430. [DOI] [PubMed] [Google Scholar]