Abstract
In this era of confronting racism in public space, it is critical to keep addressing the covert systemic racism in the healthcare system. We want to bring attention to the continued unscientific practice of race-based medicine and the absurdity of treating race as a biological indicator in the 21st century. We believe race is a social construct that does not qualify as a scientific biological indicator for predicting health outcomes. In this paper, we first present arguments for inappropriate use of race in health research and then discuss alternative explanations for health disparity findings that use race as a predictor. Our main concern centers on two specific aspects of the concept of "race": (1) its fundamental lack of scientific basis as a predictor for health outcomes, (2) the misguided narrative that the term creates, placing the onus of racial discrimination on the victim, instead of highlighting the act of discrimination and the role researchers play in actively reinforcing racism when using "race" as a variable. We conclude by proposing that "race" be replaced by the variable "racism" in health.
Keywords: Race, racism, health outcomes, social construct
Race is a compounded, socially constructed variable that lacks a concrete and standardized conceptual definition (Fuller, 2003; Kahn, 2003; Lee, 2009; Sankar et al., 2007). It appears as a predictor for the likelihood of disease development and a risk factor for health outcomes in many publications including textbooks and clinical guidelines. In these publications, race is often captured as skin color (i.e., black or white) but at times, study participants are categorized by skin color and ancestral origin, (i.e. black/African-American), while others are classified by their country of origin (i.e. Chinese) and most recently as Indigenous. Studies that combine physical characteristics with the place of origin, i.e. black/African-American, appear to imply some interactions between skin color, ancestral origin and the outcome of interest – making race a compounded variable. This ambiguity of an indicator can lead clinicians to make incorrect assumptions about patients they see by giving credence to their implicit biases (Godsil et al., 2014). In this way, research can promote "scientific racism" - the ideology that lends support to the early century practice that categorizes people based on anthropologic characteristics, which are believed to make people of European descent superior to non-Europeans (Fuentes et al., 2019; Umek & Fischer, 2020).
Scientists, particularly those in the field of genetics and social sciences, continue to warn researchers about the inappropriate use of race in health research because the heterogeneity that exists within populations - particularly those classified as black – do not correlate with human biology or behavior beyond the physical characteristics (Cooper et al., 2003; Fuentes et al., 2019; Ioannidis et al., 2021; Keeton, 2020; Race, Ethmicity, and Genetics Working Group, 2005; Umek & Fischer, 2020; Wagner et al., 2017). While it is apparent that the dichotomy between black and white predominates the literature, these race-related inequalities exist between and within populations (Fuller, 2003), which supports the immediate need to examine what race is measuring when used in health outcome research. For the purpose of this theoretical essay, we focus on people classified as black/African* to discuss the inappropriate usage of race in health research and then discuss racism as the alternative explanations for health disparity findings that use race as a predictor. We conclude by proposing that "race" be replaced by the variable "racism" in health outcomes research and offer a theoretical definition and a tool to collect such data.
History of race in health research
Race appeared in the scientific literature in the field of anthropology to advance the discourse of the time that portrayed nature not nurture as the foundation of human behavior, and to argue for multiple racial origins of the Homo sapiens (Smedley & Smedley, 2012). This discourse resulted in the creation of three to five classifications of humankind (Morning, 2011; Rupke & Lauer, 2018). Race started to appear in biological textbooks, solidifying the "scientific" reasoning that supported nature as the root of human behaviors (Morning, 2011). Overtime, science advanced this misguided notion by incorporating race into clinical practice. For example, while there are five equations to estimate glomerular filtration rate, three of these equations adjust for the black race (Jo et al., 2019); incentive spirometry corrects for the black race (Braun, 2015); and Bidil was marketed as the first race-based drug for patients with heart failure (Kahn, 2003). These clinical practices assume black people are biologically different from other races thus physiological measures need to be adjusted accordingly. The consequences of these scientific racist practices in the health system partly explain the differences in the health outcomes of black people. For example, adjusting glomerular filtration rate for the black race may seem inconsequential, but this practice has resulted in some people of African descent - even those of mixed ancestry who are deemed as black by their healthcare providers, to be ineligible for kidney transplant (Tsai, 2021). Proponents argue that dropping this adjustment would lead to overdiagnosis of kidney disease among black people. But doing so, can also shift the number of black people with early disease to advance disease status who could potentially receive advanced therapies. Some institutions are beginning to stop the practice but how this has impacted kidney disease related health outcomes for black people have yet to be fully elucidated (Madhusoodanan, 2020).
Over time, much of the health research community leaned further into the nature of biology as the roots of health disparities, even though genomic evidence refutes the notion of biological race. Disparities in cardiovascular outcomes between blacks and whites is well documented, however a recent meta-analysis of 47 articles found only three single nucleotide polymorphisms (SNP) that were associated with cardiovascular outcomes: C825T (hypertension), rs10455872 (aortic valve calcification) and rs12425791 (stroke) (Kaufman et al., 2015). Interestingly, only the SNP C825T was associated with an increased risk for hypertension but it only potentially explains some of the observed variance in the disparity associated with hypertension. Meta-analysis to examine the association between the SNP and outcomes of ischemic stroke among African and European ancestries failed to support that ischemic stroke differs among black and white patients. Overall, the study by Kaufman et al. (2015) concluded that genomic evidence does not support the biological or genetic contribution to the disparities seen in blacks compared to white people. This aligns well with the findings from the human genome project, which disputed the idea of a biological race back in early 2000 (Collins & Fink, 1995; Cooper et al., 2003). Despite this compelling 21st century evidence, race continues to be used to highlight health disparities.
Challenges in studying differences in health outcomes between various subpopulations have been widely discussed for decades. In some cases, these differences have been attributed to impacts of racism (Williams et al., 1997) while in others, a combination of genetics, environment, behavior, poverty, or even access to care (Olden & White, 2005). Overall, a major challenge is the insufficient socio-economic data for populations who face negative impacts of racism (Nazroo, 2003). Numbers of peer-reviewed publications on the health impacts of racism have been increasing exponentially since the early 2000s (Brondolo et al., 2009). Life course approach is an example of the proposed mechanisms for studying complex health determinants connected to racial health inequities (Gee et al., 2012). Similarly, epigenetic changes associated with transgenerational trauma have been brought forward as one of the new potential partial explanations for differential health outcomes (Brockie et al., 2013; Sullivan, 2013). The appropriate way to quantify and evaluate the contributions of these factors to health outcomes and health disparities have yet to be elucidated.
To date, studies continue to include race in research designs as a variable to examine health outcomes. When used researchers frequently fail to provide a theoretical rationale for using it but the conclusion they provide conflate race to be a biological variable which underpins their observations rather than as the social construct of the slavery era created to justify the inhumane treatment of people based on skin pigmentation. As a social construct, race appeared on the census in the United States initially with three categories – white, slave and others (Best & Chenault, 2014). The slave category evolved into black, or as prefixed with Afro. Nevertheless, this racial categorization became the basis for allocation of human rights – that is people of white race are seen as superior and endowed with basic human rights while blacks (the original slave category) were inferior thus unfairly dispossessed of their human rights.
Based on this premise, race is correctly operationalized in health research as self-identified criterion of belonging to groups. However, using this self-identified criterion to convey the experiences people endure in society as a proxy for biological predisposition is scientifically problematic. Firstly, the categories of race used in health research are inconsistent. In Canada, the racial categories include black, white, South Asian, Chinese, Filipino, Latin American, Arab, Southeast Asian, west Asian, Korean, Japanese, others (Statistics Canada, 2019). Mixing of skin color, geographic regions of origin, and ethnicity, is not consistently apply to all the racial categories. Moreover, black and white do not correspond to any geographic regions. The assumption might be that people of black and white races come from Africa and Europe respectively but this is an assumption which lacks scientific foundation. Genomic evidence suggests life began on the continent of Africa hence the biodiversity outside of the continent represents only a fraction of what is seen within the continent (Cooper et al., 2003). This supports the reality in which Africans are people with varying skin pigmentation. Thus, a person who may present with a darker complexion may have a predominantly European genetic heritage because the gene that codes for the white skin pigmentation is recessive (Ju & Mathieson, 2021; Sabeti et al., 2007). Similarly, sickle cell anemia – previously presumed an African disease – is now known to be a disease common throughout large areas in sub-Saharan Africa, the Mediterranean Basin, the Middle East, and India, likely because the heterozygosity for the sickle cell mutation protects against severe malaria (Lonergan et al., 2001). The dangers of racial assumptions highlight the critical need to be explicit about the sound theoretical foundations for using race in health research for scientific credibility. The failure to provide this conceptual definition is thus a major threat to the validity of research findings because of inadequate explication of construct and inadequate adjustment in statistical models (Kahn, 2003; Sankar et al., 2007; Shadish et al., 2002).
In summary, race is a concept that was socially constructed to privilege one group over another based on physical characteristics like skin pigmentation. Although the categories have evolved and increased over the years in North America, it is a fact that racism leads to differential treatment of people in society. Using "race" as a proxy in health research reinforces and solidifies the unequal treatment. It also shifts the focus from discrimination, which can be reduced, to something as unchangeable as skin color; hence removing the responsibility from society, including the researchers, to act upon findings. The more accurate term referring to health determinant that describes this preferential treatment based on skin pigmentation is racism. To take an action-oriented approach to addressing health disparities, we propose that “racism” replace “race” in health outcome research thus forth.
Racism
Racism is often used generically to refer to societal discrimination. However, without belittling the harmful effects of any kind of discrimination, we propose that racism be separated from other types of discrimination (i.e. homophobia, islamophobia, sexism and alike) and should be used to refer to discrimination based purely on skin pigmentation. Not only is one's skin color visible at all times but in societies with varying skin pigmentation, people with a darker complexion still tend to suffer worse outcomes. Discrimination based on skin pigmentation influences several socio-economic health determinants. As such people experience cumulative impacts of different types of discrimination, which further exacerbate health disparities – an idea referred to as intersectionality (Crenshaw, 1991; Levine-Rasky, 2011). Thus we do not suggest that skin pigmentation is the sole source of health disparities; only to say that skin pigmentation adds a foundational layer upon which other types of disparities – education, financial, home ownership, mortality, morbidity etc., often stem from.
Measuring racism
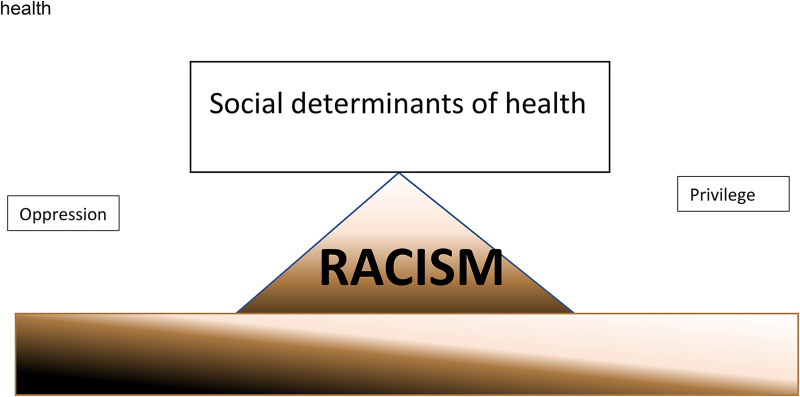
The challenge in measuring racism cannot be understated. Conceptually we define racism as a continuum with oppression and privilege on either side, which coincides with darker to lighter skin pigmentation, respectively (Figure 1).
Figure 1.
Conceptual diagram of racism and its relationship to social determinants of health.
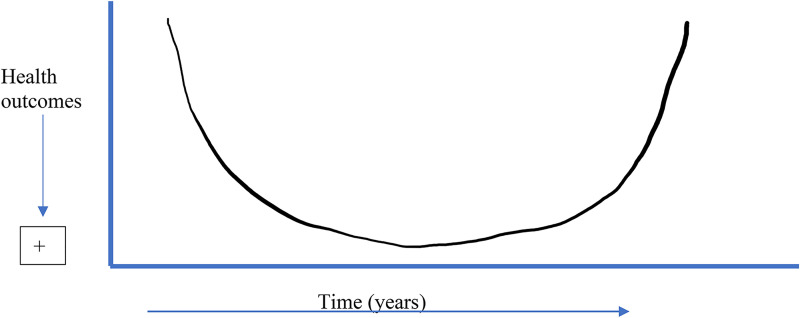
Based on this view, every human being within a racist society occupies space on the continuum. Thus, the ideal tool to measure racism must ask subjective questions about skin pigmentation but must also take into consideration frequency of racist encounter, intensity (e.g., energy expenditure physically, emotionally etc) during these encounters and the length of time the individual has been experiencing these encounters. This conceptualization of racism is based on few observations: 1) black people who endure infrequent but high intense racist encounter experience worse outcomes (e.g., higher mortality and morbidity). The transatlantic slavey trade killed an estimated 12.5 million Africans while countless other black people have died during high intensity encounters with police officers and in the health care system that resulted in their demise. These are considered infrequent but high intense at the person level – the outcomes of these encounters are so dire that individuals who experience them do so infrequently because it ultimately leads to their untimely demise, disability, or incarceration. Second, the higher the frequency at which a person experiences racist encounters, the worse their health outcomes. The assumption here is that black people who experience low intensity racism on daily basis would have worse health outcomes compared to those who experience low intensity racism on an infrequent basis. Lastly, the effects of low intensity racist encounters over a long duration may be equivalent to the effects seen among black people with infrequent, high intense racist encounters. This suggests a “U shaped curve” distribution with regards to the time dependent relationship between racism and health outcomes (Figure 2). Black people that fit premise 1 and 3 as describe above represent the higher end of the racism curve with those meeting premise 2 as their anchor. Consistent with the continuum conception of racism, the health impacts of racism on black people's health is also hypothesized to exist on a continuum.
Figure 2.
Relationship between racism and health outcomes.
Based on the available evidence, racism has an inverse relationship with health outcomes; specifically, higher reports of racism results in poorer health outcomes (Bailey et al., 2017; Smedley, 2012; Williams et al., 2008; Williams et al., 2019). It also operates on various levels within a society, which includes institutional, societal, and individual levels (Smedley, 2012; Walker et al., 2016; Williams, 2012; Williams et al., 2016, 2019; Williams & Mohammed, 2013; Williams & Rucker, 2000). Within each of these levels are factors, some quantifiable, that act as confounders either mediating or moderating the relationship between racism and health outcomes (Smedley, 2012). This current proposed conceptualization of racism retains the inverse relationship but due to the intricate relationship between racism and social determinants of health such as education, employment etc, it is hypothesized that while anti-racist approach would be beneficial to society as a whole, the health of black people meeting premise 1 and 3 would benefit the most. This is based on the assumption that if racist barriers can be removed, individuals would be capable of addressing their own social determinant of health by leveraging their social networks. Thus, the current race-focused approaches that lean heavily on addressing social determinant of health to improve the health of black people would mostly benefit black people who meet premise 2.
Proposed racism index tool
Building on the everyday discrimination scale by Williams et al. (1997), we proposed the racism index (Table 1) as a tool that can be used to quantify the experiences of black people within societies which can be used to correlate health outcomes. The responses to these questions would be summarized into a perceived racism score that can be incorporated in statistical models to predict health outcomes.
Table 1.
Racism index Tool.
| Instruction: Racism is the belief that human beings possess different characteristics, abilities, or qualities that make them inferior or superior to one another. This belief influences the way people treat one another, as well as how policies of institutions are created to disadvantage one group of people and advantage others. We are interested in knowing your experiences of racism in society and the effects on social determinants of health (i.e., adequate employment, education, housing etc.). Please answer the following questions about your outer physical appearance, place of origin and experiences of racism. |
| 1. Are you a descent of a slave? [Yes/No] |
| 1a. If no, what is your ancestral origin? [choices should reflect geographical location; note middle east can be different depending on who you ask, so for consistencies either select countries or continents, although heterogeneity on the continent of Africa will not be captured—i.e., non-black African] |
| 2. What is your skin color? [dark, light, black, white…] |
| 3. Do you consider yourself an immigrant to the country where you currently reside? [N (born in an area where I currently live) /Y] |
| 4. If yes to question 3, are you…1st 2nd 3rd etc. generation [please complete] |
| 5. Do you believe you speak with an accent that is different from those around you? [Y/N] |
| 6. Do you feel respected or treated with courtesy in your interactions with people where you live or work? [Yes//No] |
| 7. How often would you say you encounter these experiences you indicated in question 6? [Daily/1-2 times per week/3-5 times per week/ Monthly/very infrequently] |
| 8. If no to question 6, why do you think you are treated with less courtesy or respect? [open ended] |
The proposed tool is a state measurement instrument which in theory should change to reflect the implementation of meaningful strategies that aim to dismantle white supremacy - addressing racism in a way that helps people heal from its harmful effects. Though this tool is aimed at capturing the experience of racism among black people, due to the heterogeneity of their experiences, we hope it can provide a foundation that can be used and validated in other populations. Ongoing research is underway to gather qualitative data about the tool with planned quantitative studies to gather psychometric properties to determine its validity in measuring racism and its association with health outcomes.
Conclusion
We are in an era where many concepts in society and research are reassessed and redefined, this includes marriage and the differentiation of sex from gender. However, similar discourse involving race and racism has not occurred despite the mounting evidence that support racism - and not race - as a major determinant of black people's health. The irony of this discussion about racism is that it may well be the thing that is preventing us in the scientific community from embarking on the journey to define, measure and mitigate it. To this end, we proposed the racism index tool for consideration. Although, it is not yet validated, we invite the scientific community to re-ignite the discourse that will results in the incorporation of racism analysis analogous to the gender/sex analysis that is currently required by funding agencies. If this proposed conceptualization of racism is adopted and operationalized with the use of this tool, additional work will be needed because including the variable racism into the research design require advanced hierarchical statistical modeling with appropriate interaction terms for it to be meaningful in health outcomes research (Fuller, 2003; Gee, 2002). Furthermore, due to potential multicollinearity in statistical models, the academic community needs to consider which variables need to be adjusted for within statistical models. Lastly, government agencies may need to set some standards and facilitate access to some of the data at the population level that need to be adjusted for since it will be difficult for individual researchers to collect these data points. Ultimately, we believe this approach to remove race from health outcome research encourages constructive discourse on structural inequalities and interventions on the upstream causes of health disparities.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Dzifa Dordunoo https://orcid.org/0000-0002-0290-8261
References
- Bailey Z. D., Krieger N., Agénor M., Graves J., Linos N., Bassett M. T. (2017). Structural racism and health inequities in the USA: Evidence and interventions. Lancet (London, England), 389(10077), 1453–1463. 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- Best L. E., Chenault J. (2014). Racial classifications, biomarkers, and the challenges of health disparities research in the african diaspora. The Journal of Pan African Studies, 7(1), 74–98. [PMC free article] [PubMed] [Google Scholar]
- Braun L. (2015). Race, ethnicity and lung function: A brief history. Canadian journal of respiratory therapy: CJRT= Revue Canadienne de la therapies respiratoire: RCTR, 51(4), 99–101. [PMC free article] [PubMed] [Google Scholar]
- Brockie T. N., Heinzelmann M., Gill J. (2013). A framework to examine the role of epigenetics in health disparities among native Americans. Nursing Research and Practice, 2013, 1–9. 10.1155/2013/410395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondolo E., Gallo L. C., Myers H. F. (2009). Race, racism and health: Disparities, mechanisms, and interventions. Journal of Behavioural Medicine, 32(1), 1. 10.1007/s10865-008-9190-3 [DOI] [PubMed] [Google Scholar]
- Collins F. S., Fink L. (1995). The human genome project. Alcohol Health and Research World, 19(3), 190–195. [PMC free article] [PubMed] [Google Scholar]
- Cooper R. S., Kaufman J. S., Ward R. (2003). Race and genomics. New England Journal of Medicine, 348(12), 1166–1170. 10.1056/NEJMsb022863 [DOI] [PubMed] [Google Scholar]
- Crenshaw K. (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review, 43(6), 1241–1299. 10.2307/1229039 [DOI] [Google Scholar]
- Fuentes A., Ackermann R. R., Athreya S., Bolnick D., Lasisi T., Lee S.-H., McLean S.-A., Nelson R. (2019). AAPA statement on race and racism. American Journal of Physical Anthropology, 169(3), 400–402. 10.1002/ajpa.23882 [DOI] [PubMed] [Google Scholar]
- Fuller K. E. (2003). Health disparities: Reframing the problem. Medical Science Monitor, 9(3), 9–16. [PubMed] [Google Scholar]
- Gee G. C. (2002). A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. American Journal of Public Health, 92(4), 615–623. 10.2105/AJPH.92.4.615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G. C., Walsemann K. M., Brondolo E. (2012). A life-course perspective on how racism may be related to health inequities. American Journal of Public Health, 102(5), 967–974. 10.2105/AJPH.2012.300666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godsil, R. D., Tropp, L. R., Goff, P. A., & Powell, J. A. (2014). Addressing implicit bias, racial anxiety and stereotype threat in education and healthcare. The Science of Equality, 1(Nov), 1–90.
- Ioannidis J. P. A., Powe N. R., Yancy C. (2021). Recalibrating the use of race in medical research. JAMA, 325(7), 623. 10.1001/jama.2021.0003 [DOI] [PubMed] [Google Scholar]
- Jo J. Y., Ryu S. A., Kim J. I., Lee E. H., Choi I. C. (2019). Comparison of five glomerular filtration rate estimating equations as predictors of acute kidney injury after cardiovascular surgery. Scientific Reports, 9(1), 11072. 10.1038/s41598-019-47559-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ju D., Mathieson I. (2021). The evolution of skin pigmentation-associated variation in West Eurasia. Proceedings of the National Academy of Sciences of the United States of America, 118(1), e2009227118. 10.1073/pnas.2009227118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn J. (2003). Getting the numbers right: Statistical mischief and racial profiling in heart failure research. Perspectives in Biology and Medicine, 46(4), 473–483. 10.1353/pbm.2003.0087 [DOI] [PubMed] [Google Scholar]
- Kaufman J. S., Dolman L., Rushani D., Cooper R. S. (2015). The contribution of genomic research to explaining racial disparities in cardiovascular disease: A systematic review. American Journal of Epidemiology, 181(7), 464–472. 10.1093/aje/kwu319 [DOI] [PubMed] [Google Scholar]
- Keeton V. F. (2020). What's race got to do with It? A close look at the misuse of race in case-based nursing education. Nurse Educator, 45(3), 122–124. 10.1097/NNE.0000000000000707 [DOI] [PubMed] [Google Scholar]
- Lee C. (2009). "Race" and "ethnicity" in biomedical research: How do scientists construct and explain differences in health? Social Science & Medicine, 68(6), 1183–1190. 10.1016/j.socscimed.2008.12.036 [DOI] [PubMed] [Google Scholar]
- Levine-Rasky C. (2011). Intersectionality theory applied to whiteness and middle-classness. Social Identities, 17(2), 239–253. 10.1080/13504630.2011.558377 [DOI] [Google Scholar]
- Lonergan G. J., Cline D. B., Abbondanzo S. L. (2001). Sickle cell anemia. Radiographics, 21(4), 971–994. 10.1148/radiographics.21.4.g01jl23971. PMID: 11452073. [DOI] [PubMed] [Google Scholar]
- Madhusoodanan J. (2020). Is a racially-biased algorithm delaying health care for one million Black people?. Nature, 588(7839), 546–547. 10.1038/d41586-020-03419-6 [DOI] [PubMed] [Google Scholar]
- Morning A. (2011). The nature of race: How scientists think and teach about human difference. Berkeley: University of California Press. [Google Scholar]
- Nazroo J. Y. (2003). The structuring of ethnic inequalities in health: Economic position, racial discrimination, and racism. American Journal of Public Health, 93(2), 277–284. 10.2105/AJPH.93.2.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olden K., White S. L. (2005). Health-related disparities: Influence of environmental factors. The Medical Clinics of North America, 89(4), 721–738. 10.1016/j.mcna.2005.02.001 [DOI] [PubMed] [Google Scholar]
- Race, Ethnicity and Genetics Working Group (2005). The use of racial, ethnic, and ancestral categories in human genetics research. American Journal of Human Genetics, 77(4), 519–532. 10.1086/491747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rupke N., Lauer G. (Eds.). (2018). Johann Friedrich Blumenbach: Race and natural history, 1750–1850 (1st ed.). Routledge. https://doi-org.ezproxy.library.uvic.ca/10.4324/9781315184777 [Google Scholar]
- Sabeti P. C., Varilly P., Fry B., Lohmueller J., Hostetter E., Cotsapas C., Xie X., Byrne E. H., McCarroll S. A., Gaudet R., Schaffner S. F., Lander E. S., International HapMap Consortium, Frazer, K. A., Ballinger, D. G., Cox, D. R., Hinds, D. A., Stuve, L. L., Gibbs, R. A., & Belmont, J. W., … Stewart, J. (2007). Genome-wide detection and characterization of positive selection in human populations. Nature, 449(7164), 913–918. 10.1038/nature06250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sankar P., Cho M. K., Mountain J. (2007). Race and ethnicity in genetic research. American Journal of Medical Genetics Part A, 143A(9), 961–970. 10.1002/ajmg.a.31575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadish W. R., Cook T. D., Campbell D. T. (2002). Experimental and quasi-experimental designs for generalized causal inference. Houghton Mifflin Company. [Google Scholar]
- Smedley A., Smedley B. D. (2012). Race in North America: Origin and evolution of a worldview (4th ed.). Westview Press. 10.4324/9780429494789 [DOI] [Google Scholar]
- Smedley B. D. (2012). The lived experience of race and its health consequences. American Journal of Public Health, 102(5), 933–935. 10.2105/AJPH.2011.300643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada (2019, Jan, 03). Visible minority and population group reference guide, census of population, 2016. https://www12.statcan.gc.ca/census-recensement/2016/ref/guides/006/98-500-x2016006-eng.cfm
- Sullivan S. (2013). Inheriting racist disparities in health: Epigenetics and the transgenerational effects of white racism. Critical Philosophy of Race, 1(2), 190–218. 10.5325/critphilrace.1.2.0190 [DOI] [Google Scholar]
- Tsai J. (2021). Jordan Crowley would be in line for a kidney – if he were deemed white enough. https://slate.com/technology/2021/06/kidney-transplant-dialysis-race-adjustment.html
- Umek W., Fischer B. (2020). We should abandon "race" as a biological category in biomedical research. Female Pelvic Medicine & Reconstructive Surgery, 26(12), 719–720. 10.1097/SPV.0000000000000979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner J. K., Yu J. H., Ifekwunigwe J. O., Harrell T. M., Bamshad M. J., Royal C. D. (2017). Anthropologists’ views on race, ancestry, and genetics. American Journal of Physical Anthropology, 162(2), 318–327. 10.1002/ajpa.23120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker R. J., Williams J. S., Egede L. E. (2016). Influence of race, ethnicity and social determinants of health on diabetes outcomes. The American Journal of the Medical Sciences, 351(4), 366–373. 10.1016/j.amjms.2016.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R. (2012). Miles to go before we sleep: Racial inequities in health. Journal of Health & Social Behavior, 53(3), 279–295. 10.1177/0022146512455804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Lawrence J. A., Davis B. A. (2019). Racism and health: Evidence and needed research. Annual Review of Public Health, 40(1), 105–125. 10.1146/annurev-pubhealth040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Mohammed S. A. (2013). Racism and health I: Pathways and scientific evidence. American Behavioral Scientist, 57(8), 1152–1173. 10.1177/0002764213487340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Neighbors H. W., Jackson J. S. (2008). Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health, 98(9 Suppl), S29–S37. 10.2105/ajph.98.supplement_1.s29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Priest N., Anderson N. B. (2016). Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Heal Psychology, 35(4), 407–411. 10.1037/hea0000242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Rucker T. D. (2000). Understanding and addressing racial disparities in health care. Health Care Finance Rev, 21(4), 75–90. [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., Yu Y., Jackson J. S., Anderson N. B. (1997). Racial differences in physical and mental health: Socioeconomic status, stress and discrimination. Journal of Health Psychology, 2(3), 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]