Abstract
Background
Atrial fibrillation (AF) is a complex disease. The management of AF requires continuous patient engagement and integrative healthcare.
Objectives
To explore the association between adverse AF-related clinical outcomes and the following two sociodemographic factors: educational attainment and insurance plan.
Design
A nationwide, prospective, multicenter, cohort trial.
Setting
National registry of 3402 patients with non-valvular AF in Thailand.
Participants
All patients enrolled in the registry, except those with missing information on educational attainment or insurance plan. Finally, data from 3026 patients (mean age 67 years, SD 11.3; 59% male sex) were analysed.
Primary outcomes
Incidences of all-cause mortality, ischaemic stroke and major bleeding during the 36-month follow-up period. Survival analysis was performed using restricted mean survival time (RMST) and adjusted for multiple covariates. The levels of the educational attainment were as follows: no formal education, elementary (grade 1–6), secondary (grade 7–12) and higher education (tertiary education).
Results
The educational attainment of the majority of patients was elementary (N=1739, 57.4%). The predominant health insurance plans were the Civil Servant Medical Benefit Scheme (N=1397, 46.2%) and the Universal Coverage Scheme (N=1333, 44.1%). After 36 months of follow-up, 248 patients died (8.2%), 95 had ischaemic stroke (3.1%) and 136 had major bleeding (4.5%). Patients without formal education died 1.78 months earlier (adjusted RMST difference −1.78; 95% CI, −3.25 to −0.30; p=0.02) and developed ischaemic stroke 1.04 months sooner (adjusted RMST difference −1.04; 95% CI, −2.03 to −0.04; p=0.04) than those attained a level of higher education. There were no significant differences in RMSTs for all three clinical outcomes when considering the type of health insurance plan.
Conclusion
Educational attainment was independently associated with all-cause mortality and ischaemic stroke in patients with AF, but adverse clinical outcomes were not related to the types of health insurance in Thailand.
Trial registration number
Thai Clinical Trial Registration; Study ID: TCTR20160113002.
Keywords: Health policy, PUBLIC HEALTH, Adult cardiology, Thromboembolism
Strengths and limitations of this study.
This study explored the association between two sociodemographic factors (ie, educational attainment and health insurance plan) and the occurrences of adverse clinical outcomes in patients with atrial fibrillation.
Data were derived from a large prospective and nationwide cohort.
Causal relationships cannot be assumed from the outcomes of a cohort trial.
Some patients were excluded because of missing information, which might have contributed to selection bias.
Introduction
Atrial fibrillation (AF) is a common cardiovascular disease that increases the risks of death and stroke. Over the past two decades, there has been a twofold, global increase in the prevalence of AF, regardless of a country’s sociodemographic index.1 AF is a chronic, complex and multifaceted condition. Treatment of AF requires patients to change their lifestyle and adhere to chronic therapy.2 Healthcare providers from multiple specialty have to work together to optimise treatment strategy. Patients themselves need to understand the disease and their responsibilities in their own care.
Education is an important factor for understanding one’s own illness.3 Indeed, education has been shown to be a major determinant of cardiovascular and cancer mortality.4 5 In the case of a complex and chronic disease such as AF, long-term commitments from patients are necessary to adhere to medications and lifestyle adjustments. Patients with low educational attainment were shown to be associated with treatment non-compliance,6 worsened symptom severity7 and poorer prognosis.6 8
The quality and accessibility of healthcare are crucial factors that affects clinical outcomes. Worldwide, achieving universal access to healthcare has been a goal. Accordingly, a health medical plan called universal coverage scheme (UCS) was implemented in Thailand.9 UCS is a propoor and unremarkable medical scheme offered to all Thai citizens not eligible for other government based medical plans, namely Civil Servant Medical Benefit Scheme (CSMBS) and compulsory social security scheme (SSS). UCS is currently the most common health insurance plan across Thailand, covering more than 70% of the population.10 After first being implemented in 2002, UCS is now globally regarded as a highly successful policy.9 11 By 2018, uninsured population numbers had been dramatically reduced from approximately 47 million (30% of the total population) to less than 400 000 people (0.06% of the total population).9 10 Life expectancy improved from 70.6 years in 2000 to 74.6 years in 2015.9 However, the path to achieve universal access to healthcare in Thailand is fraught with challenges. Similar to healthcare reform in many low-income and middle-income countries, UCS faces problems with financial sustainability and quality of services.9 11 The benefit package of UCS is less comprehensive than that of CSMBS because of budget limitation.9 Previous studies have shown that the clinical outcomes of CSMBS beneficiaries are better than those of UCS beneficiaries.12 13 Over the last decade, UCS has responded by strengthening its primary healthcare system and expanding its benefit packages.9 However, the impact of these improvements has yet to be investigated. Both education and health coverage are among the major determinants of clinical outcomes. In a middle-income country such as Thailand, services provided by the government in both areas are still developing. In the present cohort trial, we prospectively analysed the AF patients enrolled in the national registry of Thailand. We aimed to explore whether the two sociodemographic factors (ie, educational attainment and insurance plan) were associated in adverse clinical outcomes of all-cause mortality, ischaemic stroke and major bleeding in these patients independent of other comorbidities. We believe that the results of this study can provide new insights into disparities of the education and insurance plan in Thailand as well as in other low and middle-income countries that implemented similar policies.
Methods
Participant selection
Between 2014 and 2017, patients with AF across Thailand were consecutively enrolled in the cohort of antithrombotic use and optimal international normalised ratio (INR) level in patients with non-valvular atrial fibrillation in Thailand (COOL-AF) registry. Details of the COOL-AF study have been reported elsewhere.14 Briefly, patients age>18 year with electrocardiography confirmed AF were eligible for the enrolment. The exclusion criteria14 were as follows: (1) ischaemic stroke within 3 months, (2) haematologic disorders that can increase the risk of bleeding, (3) mechanical prosthetic valve or valve repair, (4) rheumatic valve disease or severe valve disease, (5) AF associated with transient reversible cause, (6) current participation in a clinical trial, (7) life expectancy<3 years, (8) pregnancy, (9) inability to attend follow-up visits and (10) refusal to participate in the study. Written informed consent was obtained from all enrolled patients.14
This study included all patients enrolled in the registry, except those with missing information on educational attainment or insurance plan. Those who were excluded from the present study remained in the main registry until the end of follow-up (online supplemental appendix figure 1).
bmjopen-2021-053166supp001.pdf (411KB, pdf)
Data collection
Baseline data including demographics, educational attainment level, insurance plan, medical history and administered medications taken were obtained from medical records and patient interviews at the enrolment. For educational attainment, data were self-report. Patient or their families completed the educational attainment questionnaire in the hospital registration form. The insurance plan information was centrally linked to the government database and available in the patients’ medical record. All patients were prospectively followed for the endpoints of death from any causes, ischaemic stroke or major bleeding. Data on adverse outcomes were collected from medical records and telephonic interviews every 6 months until the end of the 36-month follow-up period. All adverse outcome events were validated by an adjudication committee. Ischaemic stroke and major bleeding were defined according to the standard criteria.15 16
Data classifications
The levels of educational attainment were defined as follows: no formal education, elementary education (grades 1–6), secondary education (grades 7–12) and higher education (ie, tertiary education or education beyond secondary education). The categories of the insurance plans were as follows: (1) SSS, a contributory and compulsory scheme for non-government employees; (2) CSBMS, a fringe benefit provided for government employees; (3) UCS, a non-contributory insurance scheme provided for all citizens of Thailand who were not covered by (1) or (2); and (4) non-government-based scheme (NGS), which included private insurance, opt-out of the plan and out-of-pocket payments.
According to standard guidelines,2 stroke and bleeding risks were assessed using congestive heart failure, hypertension, age≥75 (doubled), diabetes, stroke (doubled), vascular disease, age 65–74, and sex (female) (CHA2DS2VASc) and hypertension, abnormal renal/liver function (1 point each), stroke, bleeding history or predisposition, labile INR, elderly (>65 years), drugs/alcohol concomitantly (1 point each) (HASBLED) scores, respectively. In general, patients without clinical stroke risk factors do not typically require anticoagulation therapy, while patients with stroke risk factors (ie, CHA2DS2VASc≥2) are likely to benefit from anticoagulant.2 The HASBLED is a bleeding risk score. A higher HASBLED score is related to a higher risk of bleeding.2
The types of anticoagulants were grouped as follows: none, vitamin K antagonist (VKA) and direct oral anticoagulant (DOAC).
Statistical analysis
All analyses were performed using SAS software, V.9.4_M6 of the SAS OnDemand for Academics (SAS Institute). Categorical variables are expressed as numbers and percentages, and continuous variables are expressed as means and SDs. Chi-square and one-way analyses of variance were used to compare differences in baseline characteristics.
Event probabilities were assessed by restricted mean survival time (RMST) analyses using LIFETEST and RMSTREG procedures in the SAS/STAT software V.15.1. We initially chose to use a Cox proportional hazard model for the analyses. However, the proportionality hazard assumption of all three primary outcomes was violated (ie, p<0.05 based on the weighted Schoenfeld residual (online supplemental appendix table 1)). RMST analysis was selected as an alternative method. The RMST is equivalent to the area under the entire survival curve up to a fixed time point. It is widely advocated as an alternative to the Cox proportional hazard model, especially when proportionality is violated.17 18
Here, we computed RMST to the time horizon of 36 months using Kaplan-Meier method for survival probability estimation. We then adjusted RMST with multiple covariates using pseudovalue linear regression model.19 The model consisted of age, sex, educational attainment, insurance plan, types of anticoagulant, CHA2DS2VASc and HASBLED scores. We also calculated adjusted RMST to ischaemic stroke and major bleeding among patients who were still alive at the end of the follow-up, to account for the competing risk of death.20 The results were presented as the differences of RMSTs and 95% CI for each covariate.
The RMST difference estimated months gain or loss of event-free time over a period of 36 months. P values were reported for all between-group comparisons. A p value<0.05 was considered significant.
Results
Participants
The COOL-AF registry comprises of 3402 patients. Of these, 376 patients had incomplete data and were excluded from the study (online supplemental appendix figure 1 and table 2). Finally, data from 3026 patients were included in the analyses. None of the patients were lost to follow-up. The participant population (table 1) was approximately 67 years old and primarily male (N=1779, 58.8%). The most common comorbidity was hypertension (N=2061, 68.1%), followed by congestive heart failure (N=829, 27.4%) and diabetes (n=730, 24.1%). The mean CHA2DS2VASc and HASBLED scores were 3.0 (SD 1.7) and 1.5 (SD 1.0), respectively.
Table 1.
Baseline characteristics by insurance plans (N=3026)
| All (N=3026) | UHC (N=1333) | SSS (N=142) | NGS (N=154) | CSMBS (N=1397) | P value | |
| Age, mean (SD), years | 67.3 (11.3) | 66.7 (11.2) | 56.6 (10.5) | 65.4 (11.9) | 69.2 (10.6) | <0.001 |
| Male, No. (%) | 1779 (58.8%) | 732 (54.9%) | 100 (70.4%) | 91 (59.1%) | 856 (61.3%) | <0.001 |
| CHA2DS2-VASc, mean (SD) | 3.0 (1.7) | 3.0 (1.6) | 2.1 (1.7) | 2.8 (1.7) | 3.2 (1.7) | <0.001 |
| HASBLED, mean (SD) | 1.5 (1.0) | 1.5 (1.0) | 1.2 (1.1) | 1.3 (1.0) | 1.6 (1.0) | <0.001 |
| CAD, No. (%) | 478 (15.8%) | 198 (14.9%) | 19 (13.4%) | 21 (13.6%) | 240 (17.2%) | 0.255 |
| CHF, No. (%) | 829 (27.4%) | 419 (31.4%) | 33 (23.2%) | 33 (21.4%) | 344 (24.6%) | <0.001 |
| Hypertension, No. (%) | 2061 (68.1%) | 865 (64.9%) | 81 (57.0%) | 109 (70.8%) | 1006 (72.0%) | <0.001 |
| Dyslipidaemia, No. (%) | 1703 (56.3%) | 616 (46.2%) | 77 (54.2%) | 102 (66.2%) | 908 (65.0%) | <0.001 |
| Diabetes, No. (%) | 730 (24.1%) | 278 (20.9%) | 36 (25.4%) | 47 (30.5%) | 369 (26.4%) | 0.002 |
| Stroke/TIA, No. (%) | 530 (17.5%) | 237 (17.8%) | 25 (17.6%) | 20 (13.0%) | 248 (17.8%) | 0.512 |
| Vascular disease, No. (%) | 510 (16.9%) | 209 (15.7%) | 20 (14.1%) | 24 (15.6%) | 257 (18.4%) | 0.200 |
| Current smoker, No. (%) | 98 (3.2%) | 60 (4.5%) | 8 (5.6%) | 4 (2.6%) | 26 (1.9%) | <0.001 |
| Alcohol use, No. (%) | 129 (4.3%) | 53 (4.0%) | 9 (6.3%) | 10 (6.5%) | 57 (4.1%) | 0.289 |
| History of bleeding, No. (%) | 304 (10.0%) | 127 (9.5%) | 19 (13.4%) | 6 (3.9%) | 152 (10.9%) | 0.022 |
| Abnormal renal function, No. (%) | 90 (3.0%) | 39 (2.9%) | 6 (4.2%) | 2 (1.3%) | 43 (3.1%) | 0.507 |
| Abnormal liver function, No. (%) | 67 (2.2%) | 29 (2.2%) | 6 (4.2%) | 3 (1.9%) | 29 (2.1%) | 0.418 |
| Antiplatelets, No. (%) | 802 (26.5%) | 343 (25.7%) | 39 (27.5%) | 42 (27.3%) | 378 (27.1%) | 0.863 |
| Anticoagulants | <0.001 | |||||
| VKA, No. (%) | 2075 (68.6%) | 995 (74.6%) | 93 (65.5%) | 107 (69.5%) | 880 (63.0%) | |
| DOAC, No. (%) | 182 (6.0%) | 5 (0.4%) | 1 (0.7%) | 10 (6.5%) | 166 (11.9%) | |
| None, No. (%) | 769 (25.4%) | 333 (25.0%) | 48 (33.8%) | 37 (24.0%) | 351 (25.1%) | |
| Educational attainment | <0.001 | |||||
| No formal education, No. (%) | 213 (7.0%) | 152 (11.4%) | 2 (1.4%) | 11 (7.1%) | 48 (3.4%) | |
| Elementary, No. (%) | 1526 (50.4%) | 921 (69.1%) | 54 (38.0%) | 59 (38.3%) | 492 (35.2%) | |
| Secondary, No. (%) | 639 (21.1%) | 206 (15.5%) | 40 (28.2%) | 42 (27.3%) | 351 (25.1%) | |
| Higher education, No. (%) | 648 (21.4%) | 54 (4.1%) | 46 (32.4%) | 42 (27.3%) | 506 (36.2%) | |
CAD, coronary artery disease; CHA2DS2-VASc, congestive heart failure, hypertension, age≥75 years, diabetes mellitus, stroke or transient ischaemic attack (TIA), vascular disease, age 65–74 years, sex category; CHF, congestive heart failure; CSMBS, civil servant medical benefit scheme; DOAC, direct oral anticoagulant; HASBLED, hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile INR, elderly (>65 years), drugs/alcohol concomitantly; NGS, non-government-based scheme; SSS, social-security scheme; UCS, universal coverage scheme; VKA, vitamin K antagonist.
Insurance plan
The participant population was predominantly insured by either CSMBS (N=1397, 46.2%) or UCS (N=1333, 44.1%). Patients insured by CSMBS were at greater risk of stroke and bleeding as assessed by CHA2DS2VASc (CSMBS, 3.2; UCS, 3.0; NGS, 2.8; SSS, 2.1; p<0.001) and HASBLED (CSMBS, 1.6; UCS, 1.5; NGS, 1.3; SSS, 1.2; p<0.001) scores.
Educational attainment
More than one-third of the patients attained at least a secondary education level (N=1287, 42.5%). Among these patients, the male sex was predominant (N=948, 73.7%). Age, CHA2DS2VASc and HASBLED scores (online supplemental appendix table 3) were higher in those patients with no formal education (mean age, 74 years; CHA2DS2VASc, 3.9; HASBLED, 1.7) compared with those who attained an elementary (mean age, 69 years; CHA2DS2VASc, 3.3; HASBLED, 1.6), secondary (mean age, 64 years; CHA2DS2VASc, 2.7; HASBLED, 1.5) or higher level of education (mean age, 63 years; CHA2DS2VASc, 2.6; HASBLED, 1.4; p<0.001 for all comparisons).
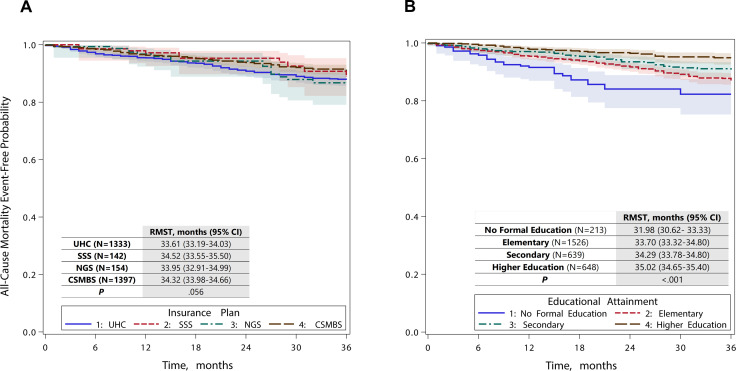
Adverse outcomes
During the 36 months follow-up, 248 patients died (8.2%), 95 had ischaemic stroke (3.1%) and 136 had major bleeding (4.5%). There were no significant differences in the rates of adverse events between those with missing information who were initially excluded and those patients whose data were included in the final analysis (online supplemental appendix table 2). Figure 1A, B shows the Kaplan-Meier survival curves of all-cause mortality by insurance plan and educational attainment, respectively. Patients with higher levels of educational attainment survived longer than those with lower levels (RMST for higher education vs secondary vs elementary vs no formal education, 35.02 vs 34.29 vs 33.70 vs 31.98 months; p<0.001). They also experienced longer event-free time to ischaemic stroke (RMST for higher education vs secondary vs elementary vs no formal education, 35.58 vs 35.46 vs 35.11 vs 34.15 months; p=0.004) and major bleeding (RMST for higher education vs secondary vs elementary vs no formal education, 35.31 vs 34.72 vs 37.82 vs 34.18 months; p=0.03) than those with lower educational attainment (online supplemental appendix table 4). The RMSTs of all three adverse outcomes did not differ among patients with different insurance plans (online supplemental appendix table 5).
Figure 1.
Kaplan-Meier curve for all-cause mortality with 95% confidence limits. (A) Kaplan-Meier curve for all-cause mortality by insurance plans. (B) Kaplan-Meier curve for all-cause mortality by educational attainment. CSMBS, civil servant medical benefit scheme; NGS, non-government-based scheme; SSS, social-security scheme; UCS, universal coverage scheme.
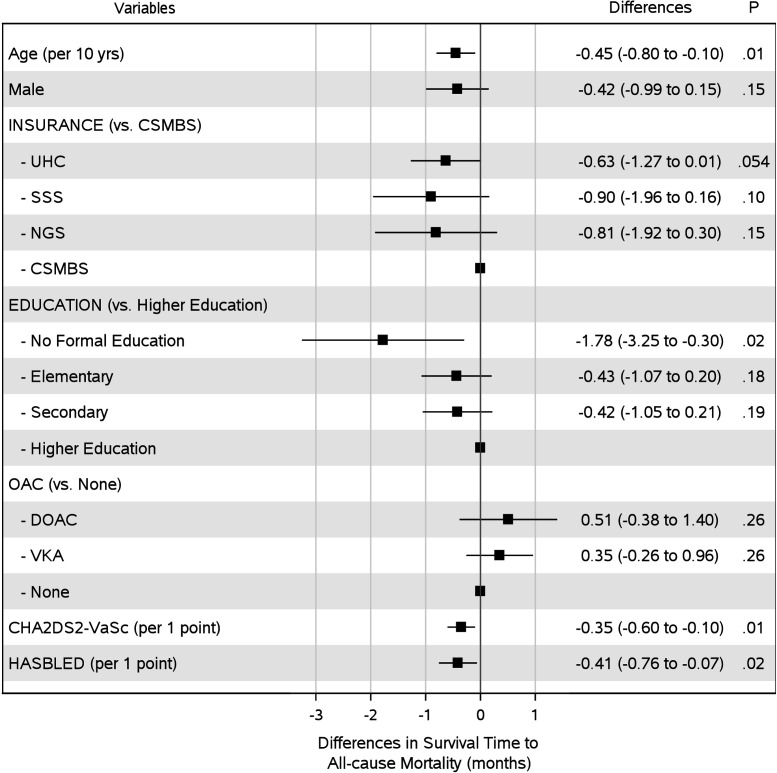
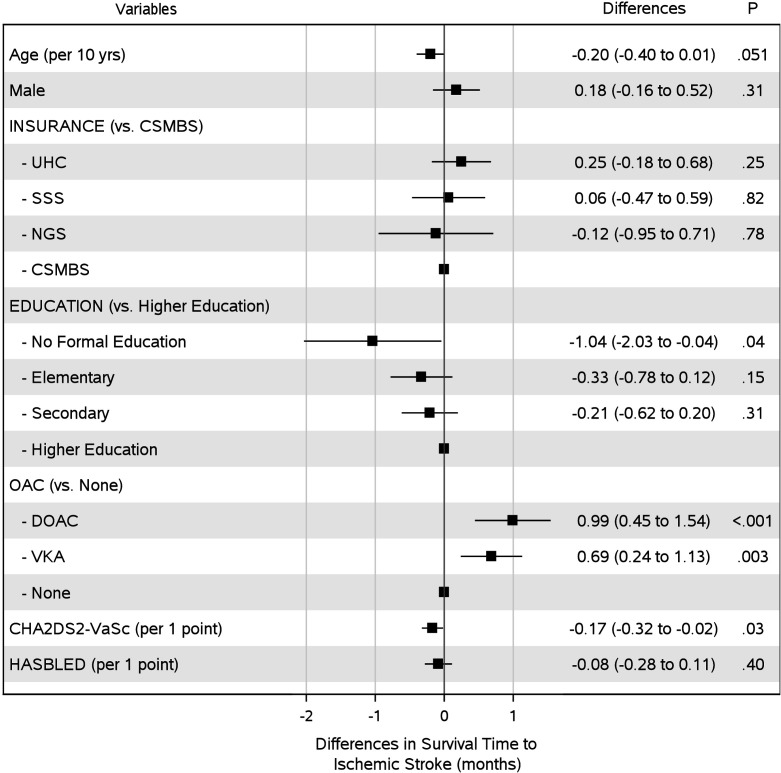
In the multivariate analyses, educational attainment was associated with all-cause mortality and ischaemic stroke, independently of comorbidities (figures 2 and 3). After adjusting for death as a competing risk of ischaemic stroke, educational attainment remained independently associated with ischaemic stroke (online supplemental appendix table 6). Over the 36-month follow-up, patients with AF and no formal education lost 1.78 months before they died (RMST difference −1.78; 95% CI, −3.25 to −0.30; p=0.02) and 1.04 months before they developed ischaemic stroke (RMST difference −1.04; 95% CI, −2.03 to −0.04; p=0.04) compared with those attained a level of higher education.
Figure 2.
Differences in adjusted restricted median survival time to all-cause mortality over a period of 36 months. The model was adjusted for of age, sex, educational attainment, insurance plan, types of anticoagulant, CHA2DS2VASc, and HASBLED scores. CAD, coronary artery disease; CHA2DS2-VASc, congestive heart failure, hypertension, age≥75 years, diabetes mellitus, stroke or transient ischaemic attack (TIA), vascular disease, age 65–74 years, sex category; CHF, congestive heart failure; CSMBS, civil servant medical benefit scheme; DOAC, direct oral anticoagulant; HASBLED, hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile INR, elderly (>65 years), drugs/alcohol concomitantly; NGS, non-government-based scheme; SSS, social-security scheme; UCS, universal coverage scheme; VKA, vitamin K antagonist.
Figure 3.
Differences in adjusted restricted median survival time to ischaemic stroke over a period of 36 months. The model was adjusted for of age, sex, educational attainment, insurance plan, types of anticoagulant, CHA2DS2VASc and HASBLED scores. CAD, coronary artery disease; CHA2DS2VASc, congestive heart failure, hypertension, age≥75 years, diabetes mellitus, stroke or transient ischaemic attack (TIA), vascular disease, age 65–74 years, sex category; CHF, congestive heart failure; CSMBS, civil servant medical benefit scheme; DOAC, direct oral anticoagulant; HASBLED, hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile INR, elderly (>65 years), drugs/alcohol concomitantly; NGS, non-government-based scheme; SSS, social-security scheme; UCS, universal coverage scheme; VKA, vitamin K antagonist.
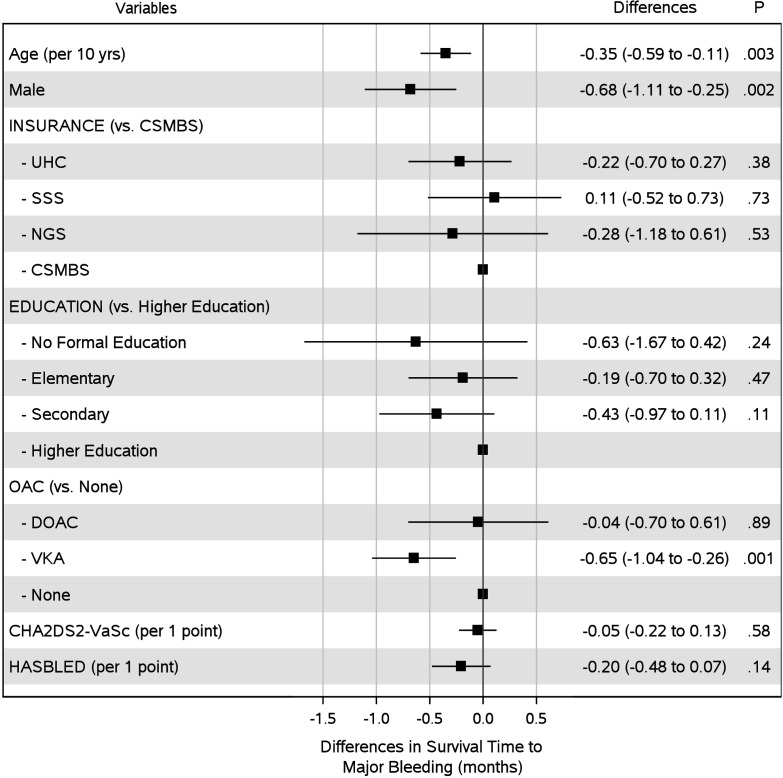
Older age and higher CHA2DS2VASc score also shortened the survival time to all-cause mortality. Survival time was lost by 0.45 months for every 10 year increase in age (RMST difference, −0.45; 95% CI, −0.8 to −0.1; p=0.01), and 0.35 months for every single point increase in CHA2DS2VASc score (RMST difference, −0.35; 95% CI, −0.6 to −0.1; p=0.01). Time to major bleeding (figure 4) was lost in patients with older age (RMST difference per 10 years, −0.35; 95% CI, −0.59 to −0.11; p=0.003), those of male sex (RMST difference, −0.68; 95% CI, −1.11 to –0.25; p=0.002) and with the use of VKA (RMST difference, −0.65; 95% CI, −1.04 to −0.26; p=0.001). For all three major outcomes, the type of insurance plan was not associated with a gain or loss in survival times (figures 2–4), even after adjusting for the competing risk of death (online supplemental appendices tables 6 and 7).
Figure 4.
Differences in adjusted restricted median survival time to major bleeding over a period of 36 months. The model was adjusted for of age, sex, educational attainment, insurance plan, types of anticoagulant, CHA2DS2VASc and HASBLED scores. CAD, coronary artery disease; CHA2DS2VASc, congestive heart failure, hypertension, age≥75 years, diabetes mellitus, stroke or transient ischaemic attack (TIA), vascular disease, age 65–74 years, sex category; CHF, congestive heart failure; CSMBS, civil servant medical benefit scheme; DOAC, direct oral anticoagulant; HASBLED, hypertension, abnormal renal/liver function, stroke, bleeding history or predisposition, labile INR, elderly (>65 years), drugs/alcohol concomitantly; NGS, non-government-based scheme; SSS, social-security scheme; UCS, universal coverage scheme; VKA, vitamin K antagonist.
Discussion
In the COOL-AF registry of patients with AF across Thailand, educational attainment was associated with all-cause mortality and ischaemic stroke, independently of age, sex, stroke and bleeding risks, anticoagulant use, and types of insurance. Over the 36-month follow-up period, those with no formal education died approximately 1.8 months sooner and suffered stroke 1 month sooner than those attained the level of higher education. UCS, the propoor medical scheme, was not linked to elevated risks of all-cause mortality, ischaemic stroke or major bleeding.
The significant impact of education on cardiovascular outcome has been demonstrated globally.8 21–23 Among Asian population, data from the Asia Pacific Cohort Studies Collaboration23 reported that Asians attained the lowest level of education had a 54% higher risk of stroke and 78% higher risk of cardiovascular mortality than those with a tertiary education. Among patients with AF, a large-scale study in Norway reported an educational gradient in mortality between patients who attained higher education level and those who attained a high school education or less.8 Findings from a patient survey showed that higher levels of educational attainment were associated with a better understanding of anticoagulant therapy and lower incidence of bleeding.24 In this prospective cohort study, we explored the association between educational attainment and three adverse outcomes, namely all-cause mortality, ischaemic stroke and major bleeding. We reported educational disparities in all-cause mortality and ischaemic stroke but not major bleeding. Disparities were detected between the educational attainment level of no formal education and higher education, independently of age, sex, bleeding and stroke risk, type of insurance plan, and anticoagulant use. Patients with no formal education are more likely to be having a reduced health literacy, which subsequently lead to poorer outcomes especially for chronic disease such as AF.4 24
Low-education and low-income statuses often coincide. Low income could lead to a lack or poor choice of health insurance. In Thailand, these consequences have been ameliorated with the implementation of UCS. The UCS provides healthcare coverage to the unemployed, who primarily are in the low-income group. According to the 2004 national health insurance data, half of UCS beneficiaries were from the two poorest quintiles while half of CSMBS insurers were in the richest quintile.25 Unlike other insurance plans for the poor, UCS provides extensive and comprehensive benefit packages.10 High-cost services, such as percutaneous cardiac intervention, heart transplantation or catheter ablation, are currently covered by UCS.9 10 A remaining discrepancy between the UCS and CSMBS packages is the drug plan. UCS restricts access to medications outside the National List of Essential Medicines, notably DOAC. In contrast, CSMBS covers the use of DOACs for some conditions.9 In this cohort of patients with AF, discrepancies in the coverages provided by different types of insurance plans did not result in outcome disparities. UCS beneficiaries had RMSTs for all-cause mortality, ischaemic stroke and major bleeding similar to beneficiaries of other plans.
However, outcome disparities between UCS and CSMBS have been previously reported.12 13 In a retrospective analysis from 2010 National Insurance Database, 5-year mortality after AF admission was higher in UCS beneficiaries than in CSMBS beneficiaries.13 In contrast to previous studies, patients in our cohort were prospectively enrolled and subjected to structured followed up. The enrolment process took place after the third strategic plan of the UCS began in 2012.10 With the implementation of the plan, the benefits were expanded to seasonal influenza vaccination, screening of complications from diabetes and hypertension, and long-term care for dependent elderly. The differences in trial designs and timing of enrolment periods could explain the discrepancies between our results and those of previous trials focusing on outcome disparities between UCS and CSMBS beneficiaries.
In this study, we reported the effect size of educational disparities using months loss. The reported value may appear small, but they indicate a time loss over a fixed period of 36 months. For those patients with no formal education, losing 1.8 months of survival time equates to losing 5% of their lifetime during follow-up. In the health production function analyses conducted in 35 members countries of Organisation for Economic Co-operation and Development countries,4 a 10% increase in education of the population was associated with a gain of 3.2 months in life expectancy and a 100% increase in education of the population was associated with a gain of 23.8 months.
Our results provide some insights to the national health insurance policy in Thailand. We have shown that in a moderate-to-high income country such as Thailand, the disparity in insurance coverage could be reduced or even removed by a well maintained, propoor health insurance, such as the UCS. Our findings also emphasise the utmost importance of national education level. Education can keep people healthier.4 For a chronic condition such as AF, adherence to the therapy requires some understanding towards the disease, which entails education.24 In our cohort, the educational attainment level of higher education was associated with better clinical outcomes, but this level is only attained in a minority of Thai population. According to the government reports,26 less than 25% of the working age population have attained higher education, and more than 20% of students left schools after completion of the compulsory, lower secondary level. Clearly, there is ample of room for improvement to make education more inclusive and accessible.
Our trial is prospective and nationwide in nature. The enrolment and follow-up were well structured and validated. To accurately analyse the outcomes that occurred at non-constant rates, we chose to use an RMST approach rather than the log-rank test or Cox proportional hazard model for the survival analysis. The truncation time for the analysis was the prespecified follow-up time, which was optimal for the performance of the test.18
Approximately 10% of patients were excluded from the present analysis because of missing educational attainment data. However, the event rates of the excluded patients were not different from those remained in the present trial. Another potential bias is that patients enrolled in the registry were more likely to have a high socioeconomic status. However, 44% of patients in this cohort were insured by the UCS indicating that these participants were more likely to have low socioeconomic statuses.
Differences were observed in the numbers of baseline comorbidities. Even after adjustment were made in the multivariate analyses, some confounders may have remained. Owing to the non-randomised nature of the trial, only assumptions about associations and not causal relationships can be made. Causal links between educational attainment, types of insurance plans and adverse clinical outcomes cannot be guaranteed by our analyses.
Conclusions
In a large nationwide prospective cohort of patients with AF in Thailand, educational attainment was independently associated with all-cause mortality and ischaemic stroke. Over a period of 36 months, RMSTs to all-cause mortality and ischaemic stroke of those patients who attained higher education levels were extended by 1.8 and 1 months, respectively, compared with those who attained no formal education. UCS beneficiaries had the same incidences of all-cause mortality, ischaemic stroke and major bleeding as beneficiaries of other insurance plans.
Supplementary Material
Footnotes
Collaborators: List of COOL-AF investigators: Buddhachinaraj Hospital: Tomorn Thongsri, Central Chest Institute of Thailand: Kriengkrai Hengrussamee, Charoen Krung Pracha Rak Hospital: Pattraporn Srirattana, Chiangrai Prachanukroh Hospital: Wattana Wongtheptien, Chonburi Hospital: Pornchai Ngamjanyaporn, Faculty of Medicine, Chiang Mai University: Arintaya Phrommintikul, Faculty of Medicine, Chulalongkorn University: Smonporn Boonyaratavej, Faculty of Medicine, Naresuan University: Pongpun Jittham, Faculty of Medicine, Prince of Songkla University: Treechada Wisartpong, Faculty of Medicine Ramathibodi Hospital, Mahidol University: Sirin Apiyasawat, Faculty of Medicine Siriraj Hospital, Mahidol University: Arjbordin Winijkul, and Rungroj Krittayaphong, Faculty of Medicine, Thammasat University (Rangsit Campus): Roj Rojretamphai, Faculty of Medicine Vajira Hospital, Navamindradhiraj University: Kulyot Jongpiputvanich, Golden Jubilee Medical Center: Somchai Dutsadeevettakul, Khon Kaen Hospital: Chaisit Wongwipaporn, Lampang Hospital: Tanita Bunyapipat, Nakorn Ratchasima Hospital: Weerapan Wiwatworapan, Nakornping Hospital: Khanchai Siriwattana, Phramongkutklao College of Medicine: Tharanit Chantrarat, Police General Hospital: Kasem Rattanasumawong, Prapokklao Hospital (Chanthaburi): Wiwat Kanjanarutjawiwat, Queen Savang Vadhana Memorial Hospital: Sakaorat Kornbongkotmas; Ratchaburi Hospital: Thanasak Patmuk, Sapphasitthiprasong Hospital: Praprut Thanakitcharu, Surat Thani Hospital: Suchart Arunsiriwattana, Surin Hospital: Thaworn Choochunklin; Udon Thani Hospital: Sumon Tangsuntornwiwat
Contributors: SA and RK had the idea for and designed the study and were responsible for the overall content as guarantors. All authors collected the data. SA performed the statistical analysis. SA mainly wrote the manuscript with support from TT, KJ and RK. All authors provided critical feedback and contributed to the final manuscript.
Funding: This study was funded by grants from the Health Systems Research Institute (grant no. 59-053), the Heart Association of Thailand under the Royal Patronage of H.M. the King and the Royal College of Physicians of Thailand.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The individual anonymised data supporting the analyses contained in the manuscript will be made available upon reasonable written request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants. The study was approved by Siriraj lnstitutional Review Board (COA no. Si 317/2014) and Central Research Ethics Committee (COA-CREC 003/2014). Participants gave informed consent to participate in the study before taking part.
References
- 1. Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge. Int J Stroke 2021;16:217–21. 10.1177/1747493019897870 [DOI] [PubMed] [Google Scholar]
- 2. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893–962. 10.1093/eurheartj/ehw210 [DOI] [PubMed] [Google Scholar]
- 3. Agård A, Hermerén G, Herlitz J. When is a patient with heart failure adequately informed? A study of patients' knowledge of and attitudes toward medical information. Heart Lung 2004;33:219–26. 10.1016/j.hrtlng.2004.02.003 [DOI] [PubMed] [Google Scholar]
- 4. James C, Devaux M, Sassi F. "Inclusive growth and health", OECD Health Working Papers, No. 103. Paris: OECD Publishing, 2017. [Google Scholar]
- 5. Kilander L, Berglund L, Boberg M, et al. Education, lifestyle factors and mortality from cardiovascular disease and cancer. A 25-year follow-up of Swedish 50-year-old men. Int J Epidemiol 2001;30:1119–26. 10.1093/ije/30.5.1119 [DOI] [PubMed] [Google Scholar]
- 6. Hernández Madrid A, Potpara TS, Dagres N, et al. Differences in attitude, education, and knowledge about oral anticoagulation therapy among patients with atrial fibrillation in Europe: result of a self-assessment patient survey conducted by the European heart rhythm association. Europace 2016;18:463–7. 10.1093/europace/euv448 [DOI] [PubMed] [Google Scholar]
- 7. Goli NM, Thompson T, Sears SF, et al. Educational attainment is associated with atrial fibrillation symptom severity. Pacing Clin Electrophysiol 2012;35:1090–6. 10.1111/j.1540-8159.2012.03482.x [DOI] [PubMed] [Google Scholar]
- 8. Akerkar R, Ebbing M, Sulo G, et al. Educational inequalities in mortality of patients with atrial fibrillation in Norway. Scand Cardiovasc J 2017;51:82–7. 10.1080/14017431.2016.1268711 [DOI] [PubMed] [Google Scholar]
- 9. Tangcharoensathien V, Witthayapipopsakul W, Panichkriangkrai W, et al. Health systems development in Thailand: a solid platform for successful implementation of universal health coverage. Lancet 2018;391:1205–23. 10.1016/S0140-6736(18)30198-3 [DOI] [PubMed] [Google Scholar]
- 10. National Health Security Office . NHSO annual report, fiscal year 2018. Bangkok: NHSO, 2018. https://eng.nhso.go.th/assets/portals/1/files/annual_report/Annual%20report_final%202018.pdf [Google Scholar]
- 11. Glassman A, Temin M. “Health Access for All: Thailand’s Universal Coverage Scheme.”. In: Millions saved: new cases of proven success in global health. Washington DC: Brookings Institution Press, 2016: 89–96. [Google Scholar]
- 12. Siwachat S, Lertprasertsuke N, Tanatip N, et al. Effect of insurance type on stage at presentation, surgical approach, tumor recurrence and cancer-specific survival in resectable non-small lung cancer patients. Risk Manag Healthc Policy 2020;13:559–69. 10.2147/RMHP.S244344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Apiyasawat S, Tangcharoen T, Wisaratapong T, et al. CHA₂DS₂-VASc scores predict mortality after hospitalization for atrial fibrillation. Int J Cardiol 2015;185:293–6. 10.1016/j.ijcard.2015.03.180 [DOI] [PubMed] [Google Scholar]
- 14. Krittayaphong R, Winijkul A, Methavigul K, et al. Risk profiles and pattern of antithrombotic use in patients with non-valvular atrial fibrillation in Thailand: a multicenter study. BMC Cardiovasc Disord 2018;18:174. 10.1186/s12872-018-0911-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sacco RL, Kasner SE, Broderick JP, et al. An updated definition of stroke for the 21st century. Stroke 2013;44:2064–89. 10.1161/STR.0b013e318296aeca [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schulman S, Kearon C, Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost 2005;3:692–4. 10.1111/j.1538-7836.2005.01204.x [DOI] [PubMed] [Google Scholar]
- 17. Royston P, Parmar MKB. Restricted mean survival time: an alternative to the hazard ratio for the design and analysis of randomized trials with a time-to-event outcome. BMC Med Res Methodol 2013;13:152. 10.1186/1471-2288-13-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. McCaw ZR, Yin G, Wei L-J. Using the restricted mean survival time difference as an alternative to the hazard ratio for analyzing clinical cardiovascular studies. Circulation 2019;140:1366–8. 10.1161/CIRCULATIONAHA.119.040680 [DOI] [PubMed] [Google Scholar]
- 19. Andersen PK, Hansen MG, Klein JP. Regression analysis of restricted mean survival time based on pseudo-observations. Lifetime Data Anal 2004;10:335–50. 10.1007/s10985-004-4771-0 [DOI] [PubMed] [Google Scholar]
- 20. Shi S, Gouskova N, Najafzadeh M, et al. Intensive versus standard blood pressure control in type 2 diabetes: a restricted mean survival time analysis of a randomised controlled trial. BMJ Open 2021;11:e050335. 10.1136/bmjopen-2021-050335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mackenbach JP, Cavelaars AE, Kunst AE, et al. Socioeconomic inequalities in cardiovascular disease mortality; an international study. Eur Heart J 2000;21:1141–51. 10.1053/euhj.1999.1990 [DOI] [PubMed] [Google Scholar]
- 22. Hamad R, Nguyen TT, Bhattacharya J, et al. Educational attainment and cardiovascular disease in the United States: a quasi-experimental instrumental variables analysis. PLoS Med 2019;16:e1002834. 10.1371/journal.pmed.1002834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Woodward M, Peters SAE, Batty GD, et al. Socioeconomic status in relation to cardiovascular disease and cause-specific mortality: a comparison of Asian and Australasian populations in a pooled analysis. BMJ Open 2015;5:e006408. 10.1136/bmjopen-2014-006408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hernández Madrid A, Potpara TS, Dagres N, et al. Differences in attitude, education, and knowledge about oral anticoagulation therapy among patients with atrial fibrillation in Europe: result of a self-assessment patient survey conducted by the European heart rhythm association. Europace 2016;18:463–7. 10.1093/europace/euv448 [DOI] [PubMed] [Google Scholar]
- 25. Prakongsai P, Limwattananon S, Tangcharoensathien V. The equity impact of the universal coverage policy: Lessons from thailand. In: Chernichovsky D, Hanson K, eds. Innovations in health system finance in developing and transitional economies. Emerald group publishing limited, 2009: 57–81. [PubMed] [Google Scholar]
- 26. Office of the Education Council . Education in Thailand 2018. Bangkok: Office of the Education Council, Ministry of Education, 2019. http://backoffice.onec.go.th/uploads/Book/1676-file.pdf [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053166supp001.pdf (411KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The individual anonymised data supporting the analyses contained in the manuscript will be made available upon reasonable written request.