Abstract
Purpose and context
We report two cases of optic neuritis following Pfizer-BioNTech COVID-19 vaccination in patients with autoimmune diseases. Post-vaccine optic neuritis, although rare, is reported in the literature and an autoimmune mechanism seems to be involved, especially in genetically predisposed subjects.
Method
Report of two cases of optic neuritis following COVID-19 vaccination in patients with autoimmune diseases.
Key results
He novelty of this article is the fact that the two patients had a medical history of autoimmune diseases (Hashimoto thyroiditis and ankylosing spondylitis), a point of interest for research because it is not yet clear whether this could constitute a risk factor for adverse events after vaccination.
Conclusions
The reactogenicity of COVID-19 mRNA vaccine in individuals suffering from immune-mediated diseases is yet to be elucidated and it is being increasingly investigated. Our paper supports the hypothesis that patients who are already affected or predisposed to autoimmune or autoinflammatory disorders should be carefully evaluated for the benefits and risks of COVID-19 mRNA vaccination.
Keywords: Neuro ophthalmology, optic neuritis, optic neuropathy, neuro imaging, immunology
Introduction
COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), it emerged in December 2019 in Wuhan city, China, and it has been declared a pandemic by the WHO in March 2020. The Pfizer-BioNTech COVID-19 Vaccine BNT162b2 is a nucleoside-modified RNA vaccine that has shown to be safe and 95% effective against COVID-19. 1
Various systemic side effects have been reported after COVID-19 vaccines, most of them mild, including pain, redness or swelling at the site of vaccine shot, fever, fatigue, headache, muscle pain, nausea, vomiting, itching, chills, joint pain, and rarely anaphylactic shock.1,2
To date also many ocular complications have been described after COVID-19 vaccination, such as cranial nerves palsy, corneal graft rejection, vascular complications, retinopathies and anterior and posterior uveitis; the human body's immune response to vaccinations is thought to be involved in the pathogenesis of the ocular adverse effects post-COVID-19 vaccination. 3
Optic neuritis is an inflammation of the optic nerve. It is mostly idiopathic, but it may also result from a diverse number of inflammatory and infectious conditions. In literature some cases of optic neuritis after COVID-19 vaccine are described, in patients without relevant medical history.4–7
We report two cases of optic neuritis following Pfizer-BioNTech COVID-19 vaccination in patients with autoimmune diseases.
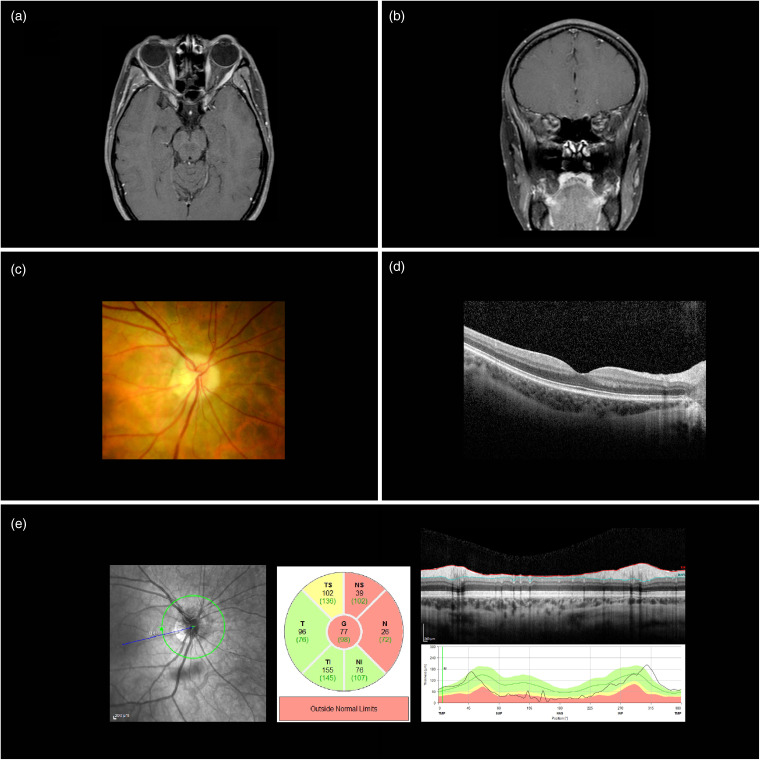
Case 1. A 31-year-old woman presented with visual loss in her right eye 6 days after the administration of the first dose of COVID-19 vaccine. Her medical history was remarkable for ankylosing spondylitis. Best-corrected visual acuity (BCVA) was 20/200 OD and 20/20 OS. Anterior segment examination was unremarkable OU, the fundoscopic examination (including OCT) revealed in the right eye an optic disc with peripapillary atrophy and mildly blurred margins. No pathological findings were found after neurological examination and in immunological and serological tests, including antibodies against aquaporin-4 and myelin oligodendrocyte glycoprotein. The visual field in the affected eye showed a subtotal scotoma and a normal retinal sensitivity in the fellow eye. MRI of the brain, orbits and spinal cord did not reveal lesions consistent with demyelination within the brain or spinal cord while T1-weighted MRI of brain and orbits, with fat suppression sequences and post gadolinium contrast, demonstrated enhancement of the retrobulbar right optic nerve near the optic foramen; a diagnosis of retrobulbar optic neuritis was therefore made (a summary of ocular imaging is shown in Figure 1).
Figure 1.
Ocular findings in case 1. (a) Axial T1 MRI of brain and orbits, with fat suppression sequences and post gadolinium contrast, demonstrating enhancement of the retrobulbar right optic nerve near the optic foramen. (b) Coronal T1 MRI of brain and orbits, with fat suppression sequences and post gadolinium contrast, demonstrating enhancement of the retrobulbar right optic nerve. (c) Fundus photo of right optic disc characterized by peripapillary atrophy and mildly blurred margins. (d) Macular OCT scan of the right eye. (e) Retinal nerve fiber layer (RNFL) thickness measurements of right eye using OCT.
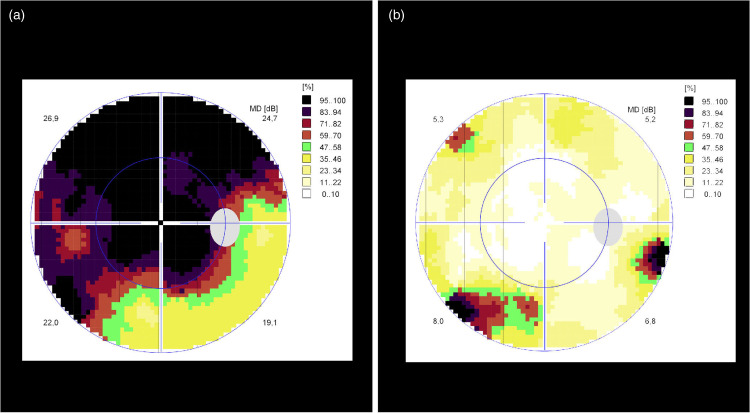
The patient was treated with a regimen of intravenous methylprednisolone 1000 mg/day for 5 days followed by a tapering dose of oral prednisone over the next 10 days. On the third day BCVA was found to be 20/20 OD with an improvement of retinal sensitivity after visual field testing (Figure 2).
Figure 2.
Visual field findings in case 1 before and after treatment. (a) Visual field findings before treatment, showing a subtotal scotoma. (b) Visual field findings after treatment, with resolution of visual field deficit.
Case 2. A 46-year-old woman presented with visual loss in the right eye for the previous 15 days. Her medical history included Hashimoto thyroiditis and a viral myocarditis 5 years before. The patient reported that her visual symptoms started 8 days after receiving the first dose of COVID-19 vaccine. BCVA was found to be 20/40 OD and 20/20 OS. Slit-lamp examination of both eyes was unremarkable. Computerized perimetry test and MRI, similarly to the previous case, confirmed the diagnosis of retrobulbar optic neuritis in the right eye. The patient was treated with corticosteroids with the same regimen as previously reported. Within one week BCVA improved to 20/25 OD and her visual field deficit resolved.
Discussion
SARS-CoV-2 infection is known to be linked to autoimmune and autoinflammatory sequelae; in fact, auto-antibodies are frequently detected in patients with COVID-19, possibly reflecting a pathogenetic role of immune dysregulation. 8
Since natural infection can result in autoimmune disorders, it is rational to question whether vaccines can also induce autoimmunity, given that autoimmune reactions to vaccinations may rarely be induced in predisposed individuals by molecular mimicry or bystander activation mechanisms. 9
In fact, new-onset autoimmune phenomena after COVID-19 vaccination are being increasingly reported, including immune thrombotic thrombocytopenia, autoimmune liver diseases, Guillain–Barré syndrome, IgA nephropathy, rheumatoid arthritis and systemic lupus erythematosus. Molecular mimicry, the production of particular autoantibodies and the role of certain vaccine adjuvants seem to contribute to the manifestation of these autoimmune phenomena. However, whether the association between COVID-19 vaccine and autoimmune manifestations is coincidental or causal remains to be elucidated. 10
In literature cases of post-viral and post-COVID-19 vaccination optic neuritis are reported;4–7,11 in all cases optic neuritis develops 1–3 weeks after the vaccination and usually has a good prognosis for visual recovery after an intravenous or oral steroid treatment. Our two reported cases are consistent with the literature, but it must be said that the main problem is to determine if the connection between vaccination and the optic nerve inflammation is not only temporal but also causal.
A review 11 seems to confirm this possible link between vaccine-induced immunization and autoimmune reaction at the level of optic nerve, especially in genetically susceptible individuals.
Since our patients do both suffer from autoimmune diseases (Hashimoto thyroiditis and ankylosing spondylitis) and optic neuritis was reported a few days after vaccination, it is possible that an autoimmune response may target the optic nerve after the vaccination.
Moreover, in the specific case of COVID-19 vaccination, an autoimmune and autoinflammatory response is thought to be the cause of several uveitic recurrences reported in the literature, in patient affected by quiescent inflammatory disease involving the eye and a history of autoimmunity.7,12
The reactogenicity of COVID-19 mRNA vaccine in individuals suffering from immune-mediated diseases (having therefore a pre-existent dysregulation of the immune response) is yet to be elucidated and it is being increasingly investigated.13–15 Our paper supports the hypothesis that patients who are already affected or predisposed (e.g. immunological and serological abnormalities in absence of clinical symptoms, familiarity for immune-mediated diseases) to autoimmune or autoinflammatory disorders should be carefully evaluated for the benefits and risks of COVID-19 mRNA vaccination.
Conclusions
Although the association between viral vaccine and the onset of optic neuritis in healthy patients is documented in the literature, our paper reports optic neuritis following COVID-19 vaccination in patients with a history of autoimmune diseases. We hope that our report may increase awareness about the possible adverse events that may present after COVID-19 vaccination, especially in patients suffering from autoimmune diseases where an already altered immune system could play a role. Further investigation is indicated to elucidate the pathophysiology of postvaccination optic neuritis and the interplay between environmental exposure and genetic predisposition in postvaccination optic neuritis warrants further research.
Acknowledgements
The Authors would like to thank Nathalie Herber, MD, from Clinic of Neuroradiology, Polytechnic University of Marche, Ancona, for her skillful contribution in clinical imaging evaluation; no compensation was received for her role.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written consent to publish the cases, including images, was gathered from the patients.
ORCID iDs: Paolo Pelliccioni https://orcid.org/0000-0002-6024-0183
Michele Nicolai https://orcid.org/0000-0001-8302-6107
Alessandro Franceschi https://orcid.org/0000-0001-8867-4488
References
- 1.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N Engl J Med 2020; 383: 2603–2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kadali RAK, Janagama R, Peruru S, et al. Side effects of BNT162b2 mRNA COVID-19 vaccine: a randomized, cross-sectional study with detailed self-reported symptoms from healthcare workers. Int J Infect Dis 2021; 106: 376–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng XL, Betzler BK, Testi I, et al. Ocular adverse events after COVID-19 vaccination. Ocul Immunol Inflamm 2021; 29: 1216–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.García-Estrada C, Gómez-Figueroa E, Alban L, et al. Optic neuritis after COVID-19 vaccine application. Clin Exp Neuroimmunol 2022; 13: 72–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elnahry AG, Asal ZB, Shaikh N, et al. Optic neuropathy after COVID-19 vaccination: a report of two cases. Int J Neurosci 2021; 14: 1–7. [DOI] [PubMed] [Google Scholar]
- 6.Pawar N, Maheshwari D, Ravindran M, et al. Ophthalmic complications of COVID-19 vaccination. Indian J Ophthalmol 2021; 69: 2900–2902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haseeb AA, Solyman O, Abushanab MM, et al. Ocular complications following vaccination for COVID-19: a one-year retrospective. Vaccines (Basel) 2022; 10: 342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pascolini S, Vannini A, Deleonardi G, et al. COVID-19 and immunological dysregulation: can autoantibodies be useful? Clin Transl Sci 2021; 14: 502–508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salemi S, D’Amelio R. Could autoimmunity be induced by vaccination? Int Rev Immunol 2010; 29: 247–269. [DOI] [PubMed] [Google Scholar]
- 10.Chen Y, Xu Z, Wang P, et al. New-onset autoimmune phenomena post-COVID-19 vaccination. Immunology 2022; 165: 386–401. [DOI] [PubMed] [Google Scholar]
- 11.Stübgen JP. A literature review on optic neuritis following vaccination against virus infections. Autoimmun Rev 2013; 12: 990–997. [DOI] [PubMed] [Google Scholar]
- 12.Bolletta E, Iannetta D, Mastrofilippo V, et al. Uveitis and other ocular complications following COVID-19 vaccination. J Clin Med 2021; 10: 5960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Briggs FBS, Mateen FJ, Schmidt H, et al. COVID-19 vaccination reactogenicity in persons with multiple sclerosis. Neurol Neuroimmunol Neuroinflamm 2022; 9: e1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang MM, Taylor KE, Paez D, et al. Reactogenicity of the mRNA SARS-CoV-2 vaccines associates with immunogenicity in patients with autoimmune and inflammatory disease. Arthritis Care Res (Hoboken). Epub ahead of print 12 April 2022. DOI: 10.1002/acr.24894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Talotta R. Do COVID-19 RNA-based vaccines put at risk of immune-mediated diseases? In reply to “potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases”. Clin Immunol 2021; 224: 108665. [DOI] [PMC free article] [PubMed] [Google Scholar]