Abstract
BACKGROUND
Atlanto-occipital dislocation (AOD) is a highly unstable injury of the osseoligamentous complex at the craniocervical junction that is more common in children. Its diagnosis remains a challenging process that must integrate clinical presentation and radiological criteria.
OBSERVATIONS
A 9-year-old child presented with severe craniocervical trauma (Glasgow Coma Scale score 6) and cardiorespiratory arrest on-site. Prompt resuscitation on-site and transfer to the university hospital were performed, and a computed tomography (CT) scan showed a subarachnoid hemorrhage around the brainstem and a retroclival hematoma. Most of the radiological criteria on CT scans for AOD were negative, except for the occipital condyle–C1 interval, and further imaging with magnetic resonance imaging permitted the diagnosis of AOD with rupture of both the tectorial membrane and the transverse ligament. Occipital-cervical Oc-C1–2 fixation was performed. The neurological outcome was excellent, with full recovery 6 months after the trauma.
LESSONS
AOD should be suspected in all high-intensity trauma in children, especially if the clinical presentation includes cardiorespiratory arrest and other brainstem and/or upper cervical cord symptoms along with premedullary subarachnoid hemorrhage. Understanding the ligamentous nature of the injury resulting in “normal” radiographs or CT scans is important to avoid underdiagnosing AOD, which can have detrimental consequences.
Keywords: atlanto-occipital dislocation, AOD, pediatric, cervical trauma, craniocervical junction, CCJ
ABBREVIATIONS : AOD = atlanto-occipital dislocation, BAI = basion–axis interval, CCI = condyle–C1 interval, CCJ = craniocervical junction, CN = cranial nerve, CSF = cerebrospinal fluid, CT = computed tomography, DBI = dens–basion interval, GCS = Glasgow Coma Scale, MRI = magnetic resonance imaging
Atlanto-occipital dislocation (AOD) is a severe ligamentous injury to the craniocervical junction (CCJ) that is thought to be fatal but the outcome of which is clearly improving due to advances in prehospital care.1–4 AOD is almost twice as frequent in children as in adults, probably because of the former’s disproportionately larger head-to-body ratio, flatter atlanto-occipital joints, and more flexible and weaker ligaments.5,6 The mechanism of injury is usually a high-energy trauma with a combination of forces with hyperextension and/or extreme lateral flexion resulting in the disruption of the tectorial membrane and alar ligaments.7
The clinical presentation ranges from severe cardiorespiratory arrest and hemodynamic instability to minor or no neurological deficits.7–9 Cranial nerve (CN) deficits are common, especially CNs VI, IX, X, and XII.10
It is important to understand that AOD is mostly a purely ligamentous injury; therefore, detailed knowledge of the ligamentous anatomy of the CCJ that is affected in AOD is pivotal.
Prompt AOD diagnosis is crucial and is even more important in the pediatric population because children survive AOD with a relatively good neurological outcome when it is detected and treated in a timely manner.11,12
Illustrative Case
A 9-year-old child was involved in a high-velocity ski accident with craniocervical trauma. On-site she was found with a Glasgow Coma Scale (GCS) score of 6, followed by cardiopulmonary arrest that was rapidly stabilized. She was brought to the emergency department intubated and sedated, and the cervical spine was secured with a rigid collar.
Imaging
A polytrauma computed tomography (CT) scan was rapidly performed, which showed a perimesencephalic and prepontine subarachnoid hemorrhage and retroclival epidural hematoma (Fig. 1A). Given the high-velocity trauma and cardiorespiratory arrest, we had a high clinical suspicion for AOD.
FIG. 1.
A: Axial CT scan showing the prepontine and premedullary subarachnoid hemorrhage. If careful analysis is done, we can appreciate an epidural component of the hematoma. B: Normal measurements criteria for AOD, Wholey DBI 7.85 mm, Harris BAI 11.54 mm, Powers ratio 0.75, and Sun C1–2/C2–3 interval 1.59. C and D: Coronal and sagittal CT; CCI with pathological value at 4.35 mm.
Careful analysis of the CCJ was performed with normal measurements for a Powers ratio of 0.75 (<1), Wholey distance between the apex of the dens and basion (dens–basion interval [DBI]) of 7.95 mm (<12 mm), Harris basion–axis interval (BAI) of 11.54 mm (normal 0–12 mm), and Sun C1–2/C2–3 interval of 1.25 (normal <2.5). The only ratio that suggested an AOD was the occipital condyle–C1 interval (CCI), measured at 4.5 mm (pathological if >4.3 mm) (Fig. 1B and C).
Further imaging with magnetic resonance imaging (MRI) confirmed subarachnoid hemorrhage, retroclival hematoma, and rupture of the tectorial membrane and transverse ligament increase in the C0–1 joint space on the left side (Fig. 2). In addition, there was a high suspicion of cerebrospinal fluid (CSF) leakage into the posterior cervical deep space (Fig. 2C) and C0–1 and C1–2 capsular tear.
FIG. 2.

MRI scans confirming AOD. A: Sagittal cut showing the retroclival hematome (yellow arrow), a sign of tectorial membrane rupture. B: Coronal view showing the C0–1 capsule rupture (yellow circle). C: Sagittal view of the C0–1 capsule distraction (yellow arrow) and suspicion of CSF leak (orange star). D: Axial view of the C0–1 joint (yellow arrow showing the ruptured joint).
Given all the above information and the clinical presentation, the diagnosis of AOD was retained, and surgical treatment was decided upon.
Surgical Technique
The patient underwent urgent surgical treatment with occipitocervical fixation at C0–2 with posterior transarticular 30 × 4–mm C1–2 screws with C0–1–2 joint opening and intracapsular bone grafting and an occipital plate (Fig. 3A and B).
FIG. 3.
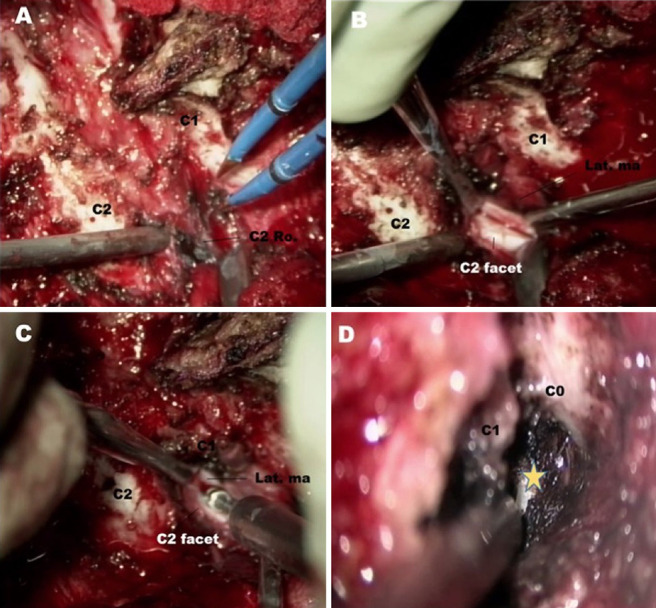
Intraoperative images. A: Dissection of the C2 root and subperiosteal coagulation of the plexus to avoid bleeding: B: C1–2 joint capsule that we can appreciate that is ruptured because of the trauma. C: Drilling of the cartilage of the articulation to achieve fusion. D: C0–1 capsule.
The patient was placed prone on the operating table, and the head was fixed in a Mayfield head holder in a neutral position under neurophysiological monitoring. There were no changes in recordings during the initial manipulation before the surgery, at the end of the positioning, or after surgery.
We used a standard posterior cervical approach with a midline incision. Identification of the C2 root, given sufficient facet distraction, which was already present preoperatively at C1–2, precluded the necessity to divide the C2 nerve roots to access the C1–2 joint. These joints were then entered where the articular cartilage and cortical surface were drilled off as preparation for bone grafting. The occipital condyle was identified due to surrounding soft tissue disruption, and joint distraction opening of the capsule was facilitated. Also, we like to follow a small ligament that attaches from the most medial part of the C1 vertebral groove of the atlas to the most medial posterior part of the condyle, because these structures “protect” the vertebral artery when dissecting it to open the capsule joint or place a screw, for example. The V3 segment of the vertebral artery was protected with a malleable spatula, whereas identical facet joint preparation was performed at the C0–1 level.
During dissection of the condyle, we could appreciate a CSF leak coming from the ventral and lateral parts of the foramen magnum due to the traumatic injury, which was repaired with a layer of fascia and glue.
Postoperative imaging confirmed the optimal positioning of the screws and stabilization of the joint (Fig. 4A and B).
FIG. 4.
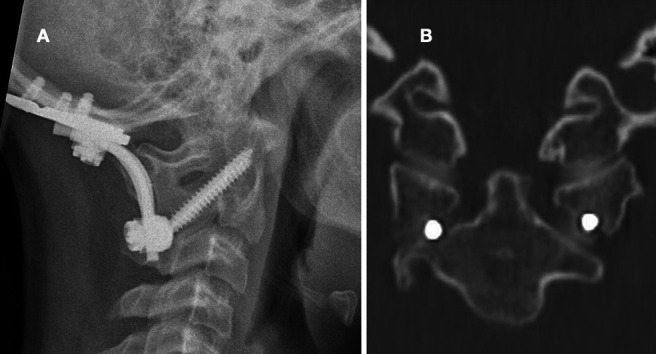
Postoperative images. A: Lateral radiograph confirming the optimal position of the screws and occipital plate. B: Coronal bone CT showing the transarticular screws. (Fusion achieved 9 months after surgery.)
Outcome
After 48 hours of neuroreanimation, she was successfully extubated, and neurological evaluation showed an excellent neurological recovery.
She had a GCS score of 15, was oriented on the three modes, and had no signs of upper cervical myelopathy, and the only neurological deficit was in CN VI on the left side.
CN VI palsy recovered within 6 months of the trauma.
Discussion
AOD is a rare injury that is associated with significant morbidity and mortality.2,3,13,14 The diagnosis of AOD is challenging, and it is important to always have a high clinical suspicion in all pediatric motor vehicle accidents of high-energy traumatism. The clinical presentation is highly variable, such as high cervical myelopathy, major brainstem dysfunction, and minor/no neurological deficits.
The problem with AOD is not so much its treatment but its timely recognition before irreversible damage is done to the cervicomedullary junction by unscrupulous handling.8 It has been proved that failure to diagnose AOD is the main predictor of mortality.12
Diagnosis can be made from plain lateral radiographs, and multiple measurements have been described for the diagnosis of AOD, such as Wholey DBI,15 Powers ratio,16 Harris BAI,17 Sun interspinous ratio,18 and the CCI.8 The CCI has the highest (100%) diagnostic sensitivity and specificity for AOD in the pediatric population8,10 compared with the other radiological criteria. Although these measurements are the standard for the diagnosis of AOD, MRI is essential to further analyze the integrity of the ligaments.19
It is not uncommon that due to correct patient positioning and handling at the time of the CT scan, the AOD is reduced, and therefore all the measurements will be falsely normal, concealing the true extent of the injury.18 This is represented by our case, which had normal measurements, except for the CCI, which was slightly increased.
Other clues for AOD that should raise a suspicion are a subarachnoid hemorrhage around the brainstem and retroclival epidural hematoma.8,20
MRI is vital in the diagnosis of AOD, especially in cases with unclear radiological criteria on CT scans or radiographs but strong clinical arguments for AOD. MRI usually confirms the rupture of the tectorial membrane, alar ligaments, and transverse ligaments.19
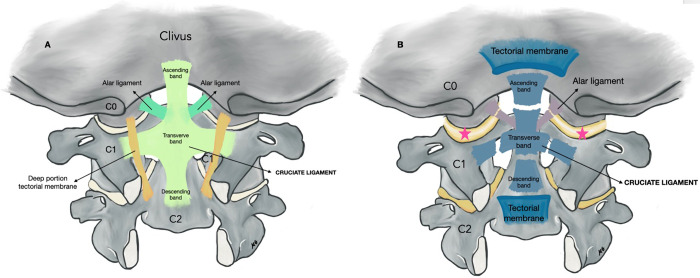
In Fig. 5, we highlight the ligamentous anatomy of the CCJ. As mentioned, AOD is almost purely a ligamentous injury, and therefore detailed knowledge of the ligamentous structures is crucial. In Fig. 5B, we can appreciate the rupture of the tectorial membrane and cruciate and alar ligaments, resulting in severe instability of the CCJ and increase of the C0–1 joint.
FIG. 5.
A: Normal anatomy of the CCJ. The cruciate ligament with the transverse, ascending and descending bands, the alar ligaments, are shown. B: AOD with disruption of the ligamentous structures; rupture of the tectorial membrane, cruciate ligament, and alar ligaments. Traumatic rupture of the C0–1 joint depicted with a pink star. Illustration by Marta Garvayo, published with permission.
The management of AOD is mainly surgery with internal fixation. Traction is contraindicated because it increases occipitocervical distraction.10 Surgical techniques may vary, but Oc-C–2 fixation remains the standard of care.21 Halo immobilization has been proposed as a treatment for AOD, but evidence indicates that it is not the appropriate management. This relies on the basis that it is a ligamentous injury and therefore is unlikely to heal with immobilization.1,10
The occipitoatlantal fusion technique we used is similar to that described by Jeszenszky et al.22 The use of this technique is facilitated by an already widened occipitoatlantal intra-articular distance in AOD. Moreover, based on Wolff’s law,23 osteogenesis is enhanced in the weight-bearing part of the spine.
Observations
Looking retrospectively at the case, the patient presented with basal cistern, prepontine, and prebulbar hemorrhages, and the CCI was abnormal. Given all these elements, the suspicion of AOD remains high, and all efforts must be made to rule out the need for CCJ fusion.
It is of critical importance to assess ligament integrity on MRI. A key anatomical feature is to confirm the integrity of the transverse ligament and tectorial membrane, which, when damaged, usually reflects significant trauma and instability of the upper cervical region and the CCJ.
MRI allowed confirmation of the AOD diagnosis in our case and was crucial in providing prompt identification and management.
Lessons
High-resolution MRI is recommended for patients for whom there is a suspicion of an underlying AOD, particularly those without significant C0–1 translation. This should be considered in the context of severe facial trauma, lower CN paresis (particularly CNs VI, X, and XII), traumatic high spinal cord injury, respiratory dysfunction, swelling of paravertebral soft tissue on imaging, and premedullary subarachnoid hemorrhage on the CT scan.
Once the appropriate diagnosis is made, including AOD with any associated atlantoaxial instability or subaxial spine injury, the choice for surgical fixation is crucial. The number of cases of AOD surviving until the hospital phase is increasing. A good surgical approach optimizes the fusion of the C0–1 joints while limiting the functional loss of movements across the CCJ.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Belouaer, Barges-Coll. Acquisition of data: Garvayo, Barges-Coll. Drafting the article: Garvayo, Belouaer. Critically revising the article: all authors. Reviewed submitted version of manuscript: Garvayo. Approved the final version of the manuscript on behalf of all authors: Garvayo. Statistical analysis: Garvayo.
Supplemental Information
Previous Presentations
This case has been presented as an abstract at the virtual Craniocervical Junction and Spine meeting, November 20, 2021.
References
- 1. Astur N, Klimo P, Jr, Sawyer JR, Kelly DM, Muhlbauer MS, Warner WC., Jr Traumatic atlanto-occipital dislocation in children: evaluation, treatment, and outcomes. J Bone Joint Surg Am. 2013;95(24):e194. doi: 10.2106/JBJS.L.01295. [DOI] [PubMed] [Google Scholar]
- 2. Chaput CD, Torres E, Davis M, Song J, Rahm M. Survival of atlanto-occipital dissociation correlates with atlanto-occipital distraction, injury severity score, and neurologic status. J Trauma. 2011;71(2):393–395. doi: 10.1097/TA.0b013e3181eb6a31. [DOI] [PubMed] [Google Scholar]
- 3. Mueller FJ, Kinner B, Rosskopf M, Neumann C, Nerlich M, Fuechtmeier B. Incidence and outcome of atlanto-occipital dissociation at a level 1 trauma centre: a prospective study of five cases within 5 years. Eur Spine J. 2013;22(1):65–71. doi: 10.1007/s00586-012-2543-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hale AT, Say I, Shah S, Dewan MC, Anderson RCE, Tomycz LD. Traumatic occipitocervical distraction injuries in children: a systematic review. Pediatr Neurosurg. 2019;54(2):75–84. doi: 10.1159/000496832. [DOI] [PubMed] [Google Scholar]
- 5. Klimo P, Jr, Ware ML, Gupta N, Brockmeyer D. Cervical spine trauma in the pediatric patient. Neurosurg Clin N Am. 2007;18(4):599–620. doi: 10.1016/j.nec.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 6. Alker GJ, Jr, Oh YS, Leslie EV. High cervical spine and craniocervical junction injuries in fatal traffic accidents: a radiological study. Orthop Clin North Am. 1978;9(4):1003–1010. [PubMed] [Google Scholar]
- 7. Steinmetz MP, Lechner RM, Anderson JS. Atlantooccipital dislocation in children: presentation, diagnosis, and management. Neurosurg Focus. 2003;14(2):ecp1. doi: 10.3171/foc.2003.14.2.11. [DOI] [PubMed] [Google Scholar]
- 8. Pang D, Nemzek WR, Zovickian J. Atlanto-occipital dislocation–part 2: the clinical use of (occipital) condyle-C1 interval, comparison with other diagnostic methods, and the manifestation, management, and outcome of atlanto-occipital dislocation in children. Neurosurgery. 2007;61(5):995–1015. doi: 10.1227/01.neu.0000303196.87672.78. [DOI] [PubMed] [Google Scholar]
- 9. Kenter K, Worley G, Griffin T, Fitch RD. Pediatric traumatic atlanto-occipital dislocation: five cases and a review. J Pediatr Orthop. 2001;21(5):585–589. [PubMed] [Google Scholar]
- 10. Theodore N, Aarabi B, Dhall SS, et al. The diagnosis and management of traumatic atlanto-occipital dislocation injuries. Neurosurgery. 2013;72(suppl 2):114–126. doi: 10.1227/NEU.0b013e31827765e0. [DOI] [PubMed] [Google Scholar]
- 11. Pang D, Wilberger JE., Jr Traumatic atlanto-occipital dislocation with survival: case report and review. Neurosurgery. 1980;7(5):503–508. doi: 10.1227/00006123-198011000-00017. [DOI] [PubMed] [Google Scholar]
- 12. Mendenhall SK, Sivaganesan A, Mistry A, Sivasubramaniam P, McGirt MJ, Devin CJ. Traumatic atlantooccipital dislocation: comprehensive assessment of mortality, neurologic improvement, and patient-reported outcomes at a level 1 trauma center over 15 years. Spine J. 2015;15(11):2385–2395. doi: 10.1016/j.spinee.2015.07.003. [DOI] [PubMed] [Google Scholar]
- 13. Bellabarba C, Mirza SK, West GA, et al. Diagnosis and treatment of craniocervical dislocation in a series of 17 consecutive survivors during an 8-year period. J Neurosurg Spine. 2006;4(6):429–440. doi: 10.3171/spi.2006.4.6.429. [DOI] [PubMed] [Google Scholar]
- 14. Horn EM, Feiz-Erfan I, Lekovic GP, Dickman CA, Sonntag VK, Theodore N. Survivors of occipitoatlantal dislocation injuries: imaging and clinical correlates. J Neurosurg Spine. 2007;6(2):113–120. doi: 10.3171/spi.2007.6.2.113. [DOI] [PubMed] [Google Scholar]
- 15. Wholey MH, Bruwer AJ, Baker HL., Jr The lateral roentgenogram of the neck; with comments on the atlanto-odontoid-basion relationship. Radiology. 1958;71(3):350–356. doi: 10.1148/71.3.350. [DOI] [PubMed] [Google Scholar]
- 16. Powers B, Miller MD, Kramer RS, Martinez S, Gehweiler JA., Jr Traumatic anterior atlanto-occipital dislocation. Neurosurgery. 1979;4(1):12–17. doi: 10.1227/00006123-197901000-00004. [DOI] [PubMed] [Google Scholar]
- 17. Harris JH, Jr, Carson GC, Wagner LK. Radiologic diagnosis of traumatic occipitovertebral dissociation: 1. Normal occipitovertebral relationships on lateral radiographs of supine subjects. AJR Am J Roentgenol. 1994;162(4):881–886. doi: 10.2214/ajr.162.4.8141012. [DOI] [PubMed] [Google Scholar]
- 18. Sun PP, Poffenbarger GJ, Durham S, Zimmerman RA. Spectrum of occipitoatlantoaxial injury in young children. J Neurosurg. 2000;93(1 suppl):28–39. doi: 10.3171/spi.2000.93.1.0028. [DOI] [PubMed] [Google Scholar]
- 19. Astur N, Sawyer JR, Klimo P, Jr, Kelly DM, Muhlbauer M, Warner WC., Jr Traumatic atlanto-occipital dislocation in children. J Am Acad Orthop Surg. 2014;22(5):274–282. doi: 10.5435/JAAOS-22-05-274. [DOI] [PubMed] [Google Scholar]
- 20. Diaz R, Zouros A, Stewart GM. Atlanto-occipital dislocation with retroclival hematoma in a pediatric patient presenting to the emergency department. Pediatr Emerg Care. 2010;26(11):843–847. doi: 10.1097/PEC.0b013e3181fb0e4c. [DOI] [PubMed] [Google Scholar]
- 21. Klepinowski T, Limanówka B, Sagan L. Management of post-traumatic craniovertebral junction dislocation: a PRISMA-compliant systematic review and meta-analysis of casereports. Neurosurg Rev. 2021;44(3):1391–1400. doi: 10.1007/s10143-020-01366-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jeszenszky D, Fekete TF, Lattig F, Bognár L. Intraarticular atlantooccipital fusion for the treatment of traumatic occipitocervical dislocation in a child: a new technique for selective stabilization with nine years follow-up. Spine (Phila Pa 1976) 2010;35(10):E421–E426. doi: 10.1097/BRS.0b013e3181c91fa1. [DOI] [PubMed] [Google Scholar]
- 23. Greer RB., 3rd Wolff’s law. Orthop Rev. 1993;22(10):1087–1088. [PubMed] [Google Scholar]