Abstract
BACKGROUND
Intracranial air may become trapped inside the cranial vault after cranial surgery, causing tension pneumocephalus with a variety of possible neurological symptoms. The authors reported a unique case in which position-dependent tension pneumocephalus developed after standard pituitary adenoma resection, causing severe intermittent visual symptoms.
OBSERVATIONS
A tiny hole in the sellar floor after transsphenoidal surgery created a valve mechanism, allowing pressurized air accumulation inside the tumor capsule that periodically compressed the optic chiasm. This caused acute visual field defects only when the patient was in an upright position. Symptoms resolved when the patient lay down because pressurized air was allowed to escape from the cranial vault and compression of the optic chiasm was relieved. This phenomenon was verified with consecutive magnetic resonance imaging sequences demonstrating the relaxation of suprasellar space, after the intracranial air had escaped in a horizontal imaging position.
LESSONS
Imperfect sealing of the sellar floor after transsphenoidal surgery is not uncommon. Even a tiny defect may in rare cases work in a valve-like manner, leading to intermittent air accumulation in the suprasellar space and causing corresponding visual symptoms. Pressure pneumocephalus inside an empty tumor capsule should be kept in mind as a possible rare complication after transsphenoidal surgery.
Keywords: pneumocephalus, transsphenoidal surgery, pituitary adenoma
ABBREVIATIONS : CSF = cerebrospinal fluid, MRI = magnetic resonance imaging
Intracranial air (pneumocephalus) is a common finding after intracranial surgical procedures and is, in most cases, a self-limiting benign finding. However, in rare cases after trauma or cranial surgery, intracranial air may become trapped inside the cranial vault, causing tension pneumocephalus with a variety of possible neurological symptoms. Tension pneumocephalus after skull base surgery is extremely rare, with only a handful of presented cases.1 After transsphenoidal surgery, this condition usually occurs after the presentation of cerebrospinal fluid (CSF) leakage due to incomplete sealing of the sphenoid sinus. In all reported cases of tension pneumocephalus, the pressured air has cumulated in the subdural space, subarachnoid cisterns, or intraventricular space.2–6
Here, we report a unique case in which position-dependent tension pneumocephalus developed inside the empty tumor capsule after standard pituitary adenoma resection. A tiny hole in the sellar floor created a valve mechanism that allowed pressurized air accumulation inside the tumor capsule that periodically compressed the optic chiasm, causing acute visual field defects only when the patient was in an upright position. These symptoms were relieved when the patient laid down because pressurized air was allowed to escape from the cranial vault, and chiasm compression was relieved. The preceding phenomenon was accurately verified during magnetic resonance imaging (MRI) and discussed as a rare cause of postoperative visual field symptoms after transsphenoidal surgery, which may not be visible in postoperative MRI taken in a horizontal position.
Illustrative Case
An 82-year-old woman in good physical and mental health noticed problems in her visual field acuity. The left-side temporal visual field defect was verified by an ophthalmologist, and MRI showed chiasmal compression caused by typical pituitary macroadenoma without significant extension to the cavernous sinus on either side (Fig. 1). The hormonal evaluation showed a mild stalk effect but no significant hormonal activity. The primary operation was performed in a standard endoscopic fashion through the sphenoid sinus, and the tumor cavity was completely emptied with curettes and suction from soft adenoma tissue. No sign of CSF leakage was observed during the procedure, and the sellar floor was sealed with absorbable collagen fibrin sealant patch and fibrin glue. No immediate postoperative complications occurred, and the patient reported that her left side temporal visual field seemed wider after surgery. She was discharged on the third postoperative day.
FIG. 1.
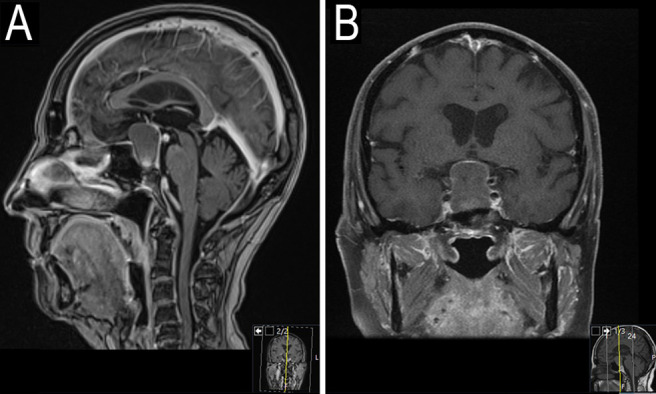
Contrast-enhanced T1-weighted MRI showing a typical pituitary macroadenoma that causes compression of the optic chiasm.
At the time of the standard 3-month postoperative outpatient clinic visit, the patient reported that her left visual field felt normal but there were now some symptoms on the right side that the ophthalmologist could not clearly verify in the visual field control check-up. The left-side temporal visual field had improved close to normal, and an MRI of the sella at 3 months postoperatively showed no remnant of contrast-enhancing tumor. Nevertheless, there was a significant amount of air inside the empty tumor capsule that was still extending upward and compressing the chiasm more on the right side (Fig. 2). Because the patient was elderly, there was no tumor remnant, the left-side visual field had improved, and the right-side defect could not be accurately verified. The treating neurosurgeon expected that the air inside the empty tumor capsule would resorb with time, and no further procedures were planned at that point. No hormonal deficiencies had developed postoperatively, and the patient was referred to an ophthalmologist for more frequent follow-ups.
FIG. 2.
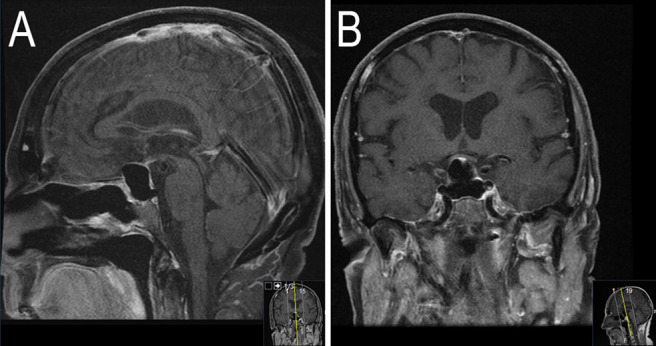
Postoperative MRI showing significant amount of air accumulated inside the empty tumor capsule. Air-filled tumor capsule is extending upward and compressing the optic chiasm more on the right side.
Position-Dependent Symptomatic Pressure Pneumocephalus Inside Empty Tumor Capsule
Five months after the primary surgery, the ophthalmologist noticed a severe visual field deficiency that had developed during the previous 2-month control interval. The temporal visual field was narrowing, and in particular, the patient was nearly blind on the right side. Her visual acuity also decreased significantly. Urgent MRI control imaging showed even more extensive air accumulation inside the empty tumor capsule with corresponding pressure on the optic nerves and chiasm. Interestingly, during the MRI procedure, when the patient laid down in a horizontal position for a while, intracranial air disappeared between the last two imaging sequences, and the optic chiasm and stalk returned to their normal position. This phenomenon was demonstrated in the following sagittal MRI sequences with corresponding imaging times (Fig. 3). When the patient was asked about any postural differences regarding these visual symptoms, she reported that her visual acuity had been getting blurred, and her temporal visual field quickly narrowed once she got up from a horizontal position in the mornings. However, these symptoms repeatedly and gradually were relieved when she lay down horizontally.
FIG. 3.
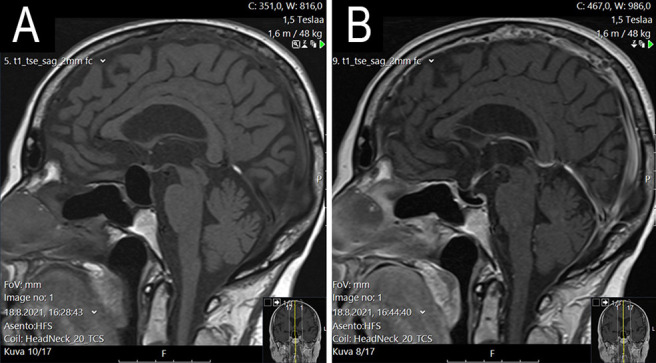
A: T1 MRI sequence taken at the time of 16.28 shows significant pneumocephalus inside the tumor capsule. B: T1 sequence taken 26 minutes later at 16.44 shows that the air has escaped from the suprasellar space during the imaging while patient has been in a horizontal position.
Treatment of Pressure Pneumocephalus
Closer investigation of the MRI showed a narrow, air-filled channel in the lower part of the sellar floor in a position that allows air to escape from intracranial space when the head is situated horizontally (Fig. 4). The tiny hole visible on MRI was visualized in the endoscopic transsphenoidal reoperation (Fig. 5) and sealed with fascia lata autograft and fibrin glue. Immediately after the operation, the patient reported clear relief of postural visual symptoms, and her temporal visual fields remained subjectively wider in an upright position. MRI on the second postoperative day showed only small air bubbles inside the sellar region and appropriate patching material against the sellar floor inside the sphenoidal sinus. At her 3-month follow-up by ophthalmologists, visual acuity had increased, but temporal visual fields had not improved significantly. The patient was in good health, and no further neurological symptoms had developed.
FIG. 4.
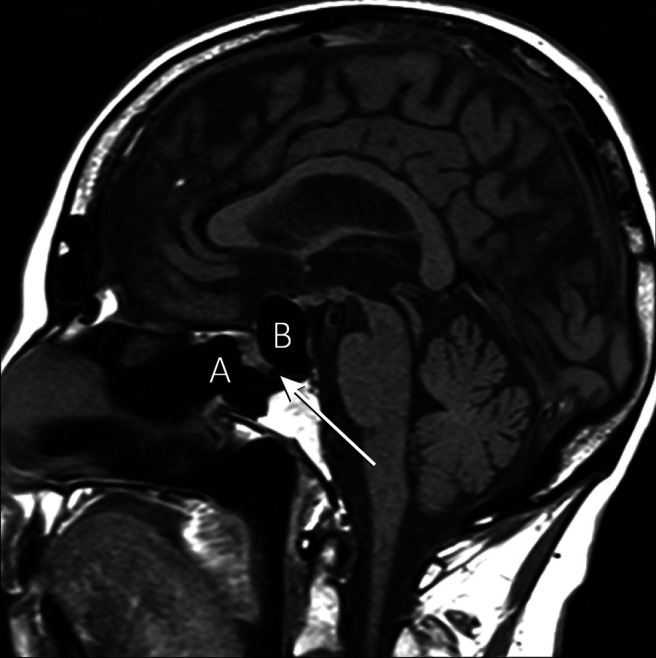
Sphenoid sinus (A) and empty adenoma capsule filled with air causing suprasellar extension and compression of optic chiasm (B). Arrow points to an air-filled small fistula canal in the lower part of sellar floor. Orientation of the fistula canal allows air accumulation inside cranial cavity when patient is in upright position.
FIG. 5.
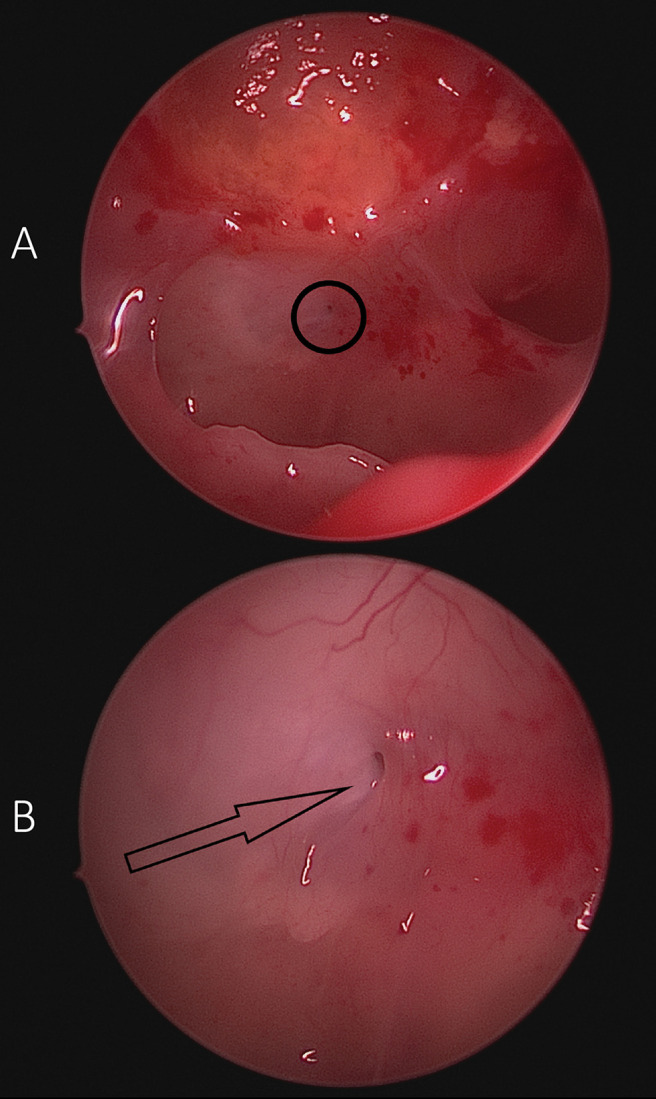
A: Endoscopic view from the sphenoid sinus. Upper part of image shows sealed tumor capsule with collagen-matrix remnants. Small fistula in lower part of sellar floor in a location corresponding to the MRI finding can be seen inside the black circle. B: Closer view from the area of the circle in (A) showing a tiny cavity-like opening as a cause of tension pneumocephalus (arrow).
Discussion
Observations
To our knowledge, this is the first report of intermittent symptomatic pneumocephalus inside an empty tumor capsule after transsphenoidal skull base surgery. It is the current standard in transsphenoidal pituitary surgery to empty the contents of an adenoma capsule without removing the capsule walls to avoid high-flow CSF leak, cranial nerve defects, and vascular injuries. Despite the appropriate sealing of the sellar floor, a tiny defect was left behind, which postoperatively created an air passage. This defect worked in a valve-like manner, leading to intermittent air accumulation in the suprasellar space and causing corresponding visual symptoms. This complication is most likely rare and can be difficult to diagnose if the pneumocephalus spontaneously resolves in a horizontal position, as was seen in this case. It is noteworthy that pneumocephalus after skull base surgery is thought to occur after CSF leakage. In our case, there was no evidence of CSF leakage, the subarachnoid spaces remained intact, and the air accumulated only inside the empty tumor capsule, causing severe symptoms.
Lessons
Imperfect sealing of the sellar floor after transsphenoidal surgery is not uncommon, and minor accumulation of air inside empty adenoma capsule postoperatively may be more frequent than previously thought. In symptomatic cases, the diagnosis may be delayed if air escapes in a horizontal position before verification with computed tomography scans or MRI. We believe it is important to bring the possibility of this rare complication to the attention of skull base surgeons.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: all authors. Acquisition of data: Kämäräinen, Penttilä. Analysis and interpretation of data: Kämäräinen, Kemppainen. Drafting the article: Kämäräinen, Kemppainen, Penttilä. Critically revising the article: all authors. Reviewed submitted version of manuscript: Kämäräinen, Kemppainen, Penttilä. Approved the final version of the manuscript on behalf of all authors: Kämäräinen. Administrative/technical/material support: Kämäräinen, Varis. Study supervision: Varis.
References
- 1. Biju RD, Wu J, Hussain Z. Tension pneumocephalus after skull base surgery. A case report and review of literature. J Clin Neurosci. 2020;75:218–220. doi: 10.1016/j.jocn.2020.03.041. [DOI] [PubMed] [Google Scholar]
- 2. Pendleton N, Persad AR, Meguro K. Tension pneumoventricle following transsphenoidal surgery. Can J Neurol Sci. 2021;48(3):419–420. doi: 10.1017/cjn.2020.172. [DOI] [PubMed] [Google Scholar]
- 3. Ruiz-Juretschke F, Mateo-Sierra O, Iza-Vallejo B, Carrillo-Yagüe R. Intraventricular tension pneumocephalus after transsphenoidal surgery: a case report and literature review. Article in Spanish. Neurocirugia (Astur) 2007;18(2):134–137. [PubMed] [Google Scholar]
- 4. McLaughlin DC, Chaichana KL, Freeman WD. Angel wing pneumocephalus sign following transsphenoidal surgery. Neurohospitalist. 2019;9(2):116–117. doi: 10.1177/1941874418786831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lin YH, Lin HL, Cho DY. Tension pneumoventricle after endoscopic transsphenoidal surgery for Rathke cleft cyst. World Neurosurg. 2020;135:228–232. doi: 10.1016/j.wneu.2019.12.065. [DOI] [PubMed] [Google Scholar]
- 6. Thavaraputta S, Attaya EN, Lado-Abeal J, Rivas AM. Pneumocephalus as a complication of transsphenoidal surgery for pituitary adenoma: a case report. Cureus. 2018;10(8):e3104. doi: 10.7759/cureus.3104. [DOI] [PMC free article] [PubMed] [Google Scholar]


