Abstract
BACKGROUND
This report describes an unusual meningioma with a large left frontal component and extensive growth within the sagittal sinus and its successful treatment with a staged approach: left frontal craniotomy followed by a sagittal craniotomy and intrinsic removal of the tumor from the sagittal sinus.
OBSERVATIONS
A previously healthy 27-year-old presented with 6 months of progressively worsening bilateral headaches, visual changes, and nausea. On examination she had a left cranial nerve VI palsy and severe papilledema. Magnetic resonance imaging revealed a 5.1 × 3.8 × 4.1 cm homogenously enhancing left superior frontal parafalcine extra-axial mass with surrounding vasogenic edema and growth through the sagittal sinus extending just short of the torcula.
LESSONS
This case report describes a fast-growing meningioma with a unique pattern of spread, growing through the sagittal sinus as if it were a conduit and resulting in complete occlusion of flow in the sinus. An important recognition in this case was that a robust parasagittal venous plexus had developed on either side of the falx cerebri with drainage to the inferior sagittal sinus. This collateral drainage pattern allowed for an extradural opening of the sagittal sinus from front to back and intrinsic resection of the tumor from the sinus with preservation of the lateral walls of the sinus.
Keywords: case report, meningioma, sagittal sinus, sinus surgery
ABBREVIATIONS : CT = computed tomography, MRI = magnetic resonance imaging
Meningiomas account for about one-third of all central nervous system tumors.1 The most common locations are the cerebral convexity (35%) and parasagittal (20%).2 Meningiomas present a particular challenge when they involve bridging veins and major dural sinuses, as surgical removal may lead to venous congestion, brain swelling, and venous infarction. Parasagittal meningiomas have a grading classification described by Sindou.3,4 Type I describes meningiomas that are attached to the outer surface of the sinus wall. In higher grades, types V and VI, the sinus is totally occluded.3,4 After resection, the prognosis for recurrence is graded by the Simpson scale. A Simpson grade I resection denotes complete removal of the tumor with excision of the dural attachment and any abnormal bone. Complete removal results in a lower rate of recurrence.5 If the tumor arises from the wall of a dural venous sinus, a complete resection requires removal of the affected sinus wall, which can lead to venous congestion, brain swelling and venous infarction. This report describes an unusual meningioma with a large left frontal component and extensive growth within the sagittal sinus and its successful treatment with a staged approach: left frontal craniotomy followed by a sagittal craniotomy and intrinsic removal of the tumor from the sagittal sinus.
Illustrative Case
A previously healthy 27-year-old presented to the emergency department with 6 months of progressively worsening bilateral headaches, visual changes, and nausea. She was previously evaluated at another hospital where computed tomography (CT) was read as negative (Fig. 1). On examination she had a left cranial nerve VI palsy and severe papilledema. Head CT (Fig. 1) was obtained followed by magnetic resonance imaging (MRI) that revealed a 5.1 × 3.8 × 4.1 cm homogenously enhancing left superior frontal parafalcine extraaxial mass with surrounding vasogenic edema and growth through the sagittal sinus extending just short of the torcula (Fig. 2A).
FIG. 1.
Noncontrast coronal CT scan (A) obtained 19 months prior to presentation (obtained for evaluation following motor vehicle accident) showing no abnormalities. CT scan (B) 5 months prior to presentation was interpreted as normal, however, the sagittal sinus is enlarged and hyperdense. No left frontal mass is present. CT scan at presentation (C) shows left frontal edema and mass effect from the left frontal component of the tumor and involvement of the sagittal sinus.
FIG. 2.
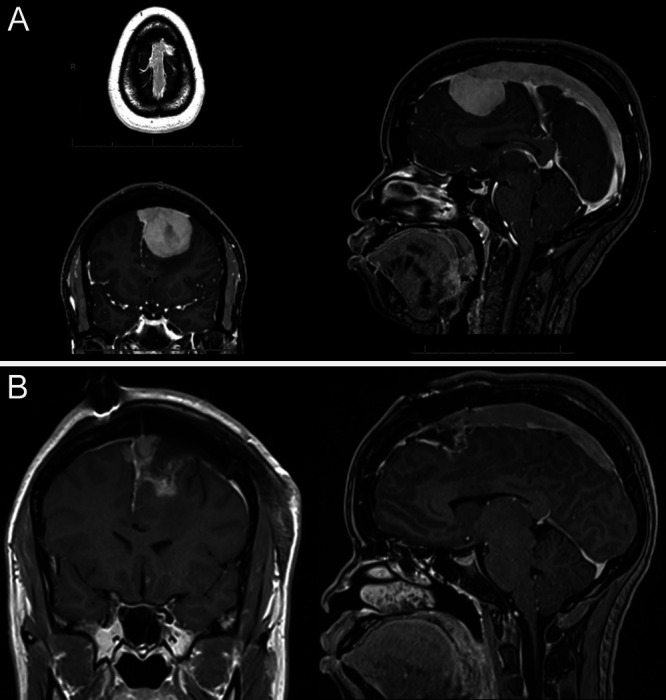
A: Axial, coronal, and sagittal brain MRI with gadolinium contrast demonstrating contrast enhancing dural growth in the left frontal lobe with extension through the superior sagittal sinus. B: Postoperative coronal and sagittal gadolinium enhanced MRI performed after the first surgery, demonstrating resection of the left frontal mass and continued sagittal sinus involvement.
Considering the significant mass effect from the left frontal component of the lesion and rapid development of this large lesion in 5 months, a left frontal craniotomy was performed for resection of the left frontal component of the tumor. The margins of the tumor were well-circumscribed and noninvasive to the surrounding brain tissue. However, the bone overlying the tumor was noted to be hypervascular. Intraoperative pathology was reported as “lesional tissue.” Postoperative MRI showed complete resection of the left frontal component of the tumor (Fig. 2B). Her preoperative headache improved, and she continued to have intermittent headaches, blurred vision related to her sixth nerve palsy, and papilledema. She was discharged home on postoperative day 3.
The final pathology description was: “The specimens consist of a predominately spindled meningothelial lesion. There are epithelioid features with meningothelial whorls and rare psammoma bodies. Increase mitotic activity (4/10 HPFs) is noted, as well as macronucleoli and hypercellularity. There is no evidence of brain invasion, small cell change, or loss of pattern noted. Lesional tissue show patchy positivity for EMA and Ki67 highlights scattered cells showing nuclear positivity for an overall mildly increased (20%) proliferation rate. Staining for S100 is negative. Final Diagnosis: Atypical meningioma, WHO grade II.”
The patient was admitted 4 weeks later for the second surgery. Careful review of imaging studies revealed persistent filling of bilateral bridging veins with development of rich parasagittal venous anastomoses traveling on the lateral dura of the sagittal sinus despite the complete occlusion of the sinus itself (Fig. 3). Therefore, extrinsic resection with removal of the sinus would not be possible and an intrinsic approach with opening of the dorsal surface (extradural) of sinus in the midline was the best method for preservation of venous drainage. A central venous catheter was inserted and using a laser level the central venous pressure transducer was leveled to the midpoint of the sagittal sinus. Head position was adjusted until the CVP transducer read 0. Scalp incision was made along the previous incision and extended sagittally in the midline to the torcula. Burr holes were drilled on either side of the sagittal sinus and a sagittal craniotomy was cut and elevated. An incision was made in the midline at the most rostral portion of the sinus, exposing tumor underneath. The tumor was resected in a segmental fashion by opening, resecting, and closing the sinus in small sections from rostral to caudal until the tumor had been completely removed and the sinus repaired (Fig. 4). The interior dural surface of the sinus was coagulated as the resection progressed and the sinus was irrigated with heparinized saline. In removing the final posterior portion of the tumor, a pediatric Foley catheter was placed into the posterior sinus just above the torcula and inflated to temporarily occlude the distal sinus. Only retrograde blood flow from the posterior sagittal sinus was noted. There was no bleeding from bridging veins feeding into the sinus. The patient was heparinized for the first 12 hours following resection, but this was discontinued after postoperative MRI failed to show recanalization of the sinus.
FIG. 3.
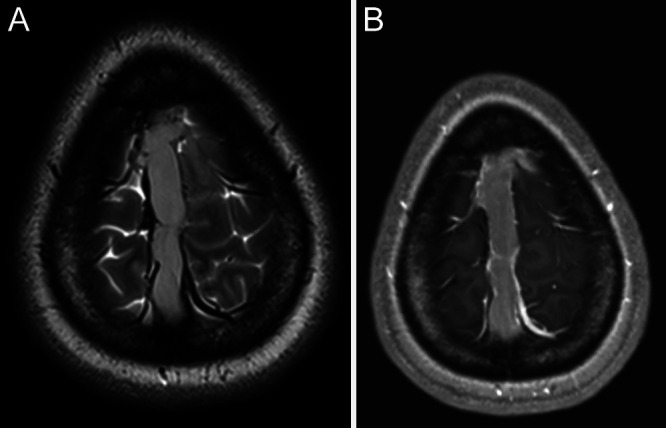
Axial T2-weighted (A) and postcontrast T1-weighted (B) magnetic resonance images demonstrate collateral venous drainage on the lateral (external) walls of the sinus with complete occlusion of sinus with tumor.
FIG. 4.
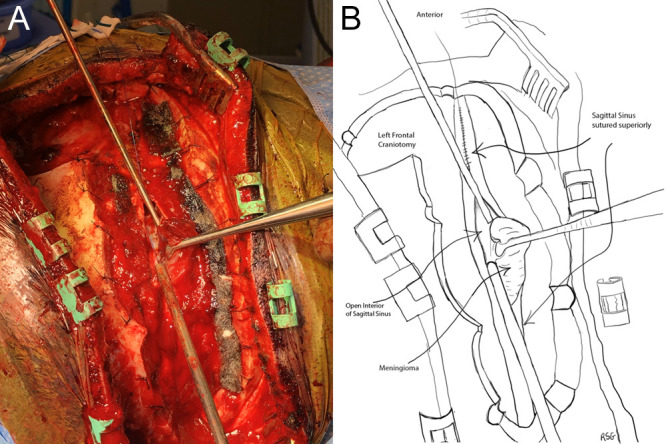
Intraoperative image demonstrating resection of the meningioma inside the superior sagittal sinus (A). Line drawing (B).
She was discharged on postoperative day 3, and at follow-up had resolution of all symptoms. Later she was treated with radiation. MRI at 18 months showed no evidence of residual or recurrent tumor (Fig. 5). MRI follow-up has been temporarily suspended due to pregnancy.
FIG. 5.
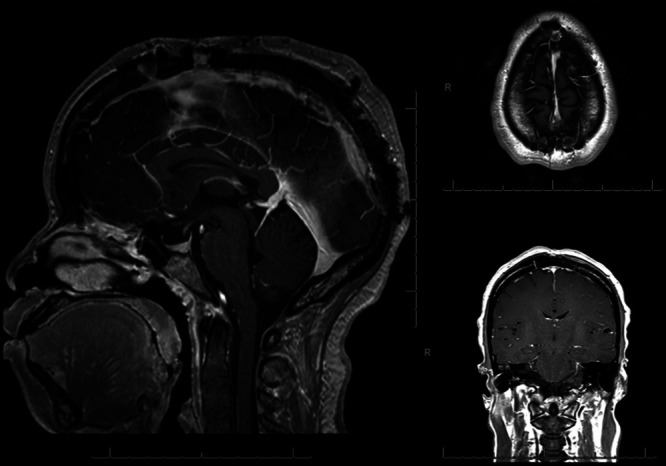
Eighteen-month postoperative MRI shows no residual or recurrent tumor. Significant recanalization of the sagittal sinus with persistent deep venous compensation via inferior sagittal sinus and deep venous drainage. Less prominent compared to immediately postoperative MRI.
Discussion
Observations
This report describes an unusual, fast-growing meningioma with a large left frontal component and extensive growth within the sagittal sinus. To the authors’ knowledge, this is a unique growth pattern for a meningioma with spread through the sagittal sinus as if it were a tube or conduit. In addition to the unique spread of this tumor and occlusion of venous drainage within the sinus, imaging revealed an interesting pattern of collateral venous drainage. T2 MRI demonstrates the parasagittal bridging veins remain patent and a rich anastomotic network developed on the lateral dural surface of the sinus bilaterally (Fig. 4). These veins, in turn, drain through falcine collaterals to the inferior sagittal sinus. Tubbs et al.6 described persistent falcine sinus as an embryologic communication between the superior and inferior sagittal sinus and others have demonstrated recruitment of these anastomosing structures with pathologies which occlude sinus drainage.7–9
Prior authors have described and classified meningiomas invading and occluding dural sinuses.10,11 Additionally, authors have characterized venous collateral drainage and many strategies for managing venous obstruction including ligation/resection of occlude portions of dural sinuses, intradural suturing the recessed edges, use of patch grafts to repair dural sinus and creation of sinus bypass with vein grafts.3,4,12 None of the previously described techniques would be applicable to the unique features of this tumor. However, the extradural intrinsic sinus approach described here was successful in obtaining complete resection with excellent neurological outcome.
Lessons
This case report describes a fast-growing meningioma with a unique pattern of spread, namely growing through the sagittal sinus as if it were a conduit and resulting in complete occlusion of flow in the sinus. An important recognition in this case was that a robust parasagittal venous plexus had developed on either side of the falx cerebri, with drainage to the inferior sagittal sinus. This collateral drainage pattern allowed for an extradural opening of the sagittal sinus from front to back and intrinsic resection of the tumor from the sinus with preservation of the lateral walls of the sinus.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: all authors. Acquisition of data: all authors. Analysis and interpretation of data: Rajagopal, Graham. Drafting the article: all authors. Critically revising the article: Rajagopal, Graham. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Rajagopal. Administrative/technical/material support: Rajagopal, Graham. Study supervision: Graham.
References
- 1. Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010;99(3):307–314. doi: 10.1007/s11060-010-0386-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haddad GF, Al-Mefty O, Aboulrauf SI. Youmans Neurological Surgery. 5th ed. Saunders; 2004. pp. 1099–1131. [Google Scholar]
- 3. Sindou MP, Alvernia JE. Results of attempted radical tumor removal and venous repair in 100 consecutive meningiomas involving the major dural sinuses. J Neurosurg. 2006;105(4):514–525. doi: 10.3171/jns.2006.105.4.514. [DOI] [PubMed] [Google Scholar]
- 4. Sindou M. Meningiomas invading the sagittal or transverse sinuses, resection with venous reconstruction. J Clin Neurosci. 2001;8(1) suppl 1:8–11. doi: 10.1054/jocn.2001.0868. [DOI] [PubMed] [Google Scholar]
- 5. Simpson D. The recurrence of intracranial meningiomas after surgical treatment. J Neurol Neurosurg Psychiatry. 1957;20(1):22–39. doi: 10.1136/jnnp.20.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tubbs RS, Loukas M, Louis RG, Jr, et al. Anatomy of the falcine venous plexus. J Neurosurg. 2007;107(1):155–157. doi: 10.3171/JNS-07/07/0155. [DOI] [PubMed] [Google Scholar]
- 7. Manjila S, Bazil T, Thomas M, Mani S, Kay M, Udayasankar U. A review of extraaxial developmental venous anomalies of the brain involving dural venous flow or sinuses: persistent embryonic sinuses, sinus pericranii, venous varices or aneurysmal malformations, and enlarged emissary veins. Neurosurg Focus. 2018;45(1):E9. doi: 10.3171/2018.5.FOCUS18107. [DOI] [PubMed] [Google Scholar]
- 8. Strub WM, Leach JL, Tomsick TA. Persistent falcine sinus in an adult: demonstration by MR venography. AJNR Am J Neuroradiol. 2005;26(4):750–751. [PMC free article] [PubMed] [Google Scholar]
- 9. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016;131(6):803–820. doi: 10.1007/s00401-016-1545-1. [DOI] [PubMed] [Google Scholar]
- 10. Oka K, Go Y, Kimura H, Tomonaga M. Obstruction of the superior sagittal sinus caused by parasagittal meningiomas: the role of collateral venous pathways. J Neurosurg. 1994;81(4):520–524. doi: 10.3171/jns.1994.81.4.0520. [DOI] [PubMed] [Google Scholar]
- 11. Wei Z, Mallela A, Faramand A, Niranjan A, Lunsford L. Long-term survival in patients with long-segment complex meningiomas occluding the dural venous sinuses: illustrative cases. J Neurosurg Case Lessons. doi: 10.3171/CASE21116. Published online May 17, 2021. doi: 10.3171/CASE21116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. DiMeco F, Li KW, Casali C, et al. Meningiomas invading the superior sagittal sinus: surgical experience in 108 cases. Neurosurgery. 2004;55(6):1263–1274. doi: 10.1227/01.neu.0000143373.74160.f2. [DOI] [PubMed] [Google Scholar]



