Abstract
Objectives
Respiratory syncytial virus (RSV) causes substantial morbidity and mortality in older adults. We assessed severe clinical outcomes among hospitalized adults that were associated with RSV infections.
Methods
We performed a nested retrospective study in 3 New York City hospitals during 2 respiratory viral seasons, October 2017–April 2018 and October 2018–April 2019, to determine the proportion of patients with laboratory-confirmed RSV infection who experienced severe outcomes defined as intensive care unit (ICU) admission, mechanical ventilation, and/or death. We assessed factors associated with these severe outcomes and explored the effect of RSV-associated hospitalizations on changes in the living situations of surviving patients.
Results
Of the 403 patients studied (median age, 69 years), 119 (29.5%) were aged ≥80. Severe outcomes occurred in 19.1% of patients, including ICU admissions (16.4%), mechanical ventilation (12.4%), and/or death (6.7%). Patients admitted from residential living facilities had a 4.43 times higher likelihood of severe RSV infection compared with patients who were living in the community with or without assistance from family or home health aides. At discharge, 56 (15.1%) patients required a higher level of care than at admission.
Conclusions
RSV infection was associated with severe outcomes in adults. Living in a residential facility at admission was a risk factor for severe outcomes and could be a proxy for frailty rather than an independent risk factor. Our data support the development of prevention strategies for RSV infection in older populations, especially older adults living in residential living facilities.
Keywords: respiratory syncytial virus, epidemiology, assisted-living facilities, frailty, in-hospital mortality
Respiratory syncytial virus (RSV) causes substantial morbidity and mortality in older adults. RSV infects an estimated 3% to 10% of adults each year 1 and contributes to more than 14 000 adult deaths annually in the United States. 2 People with chronic heart or lung disease and people with immunocompromising conditions are at increased risk of severe illness from RSV infection; RSV causes exacerbations of asthma, chronic obstructive pulmonary disease, and cardiovascular comorbidities. 3 -5 National mortality and viral surveillance data for respiratory and cardiac deaths estimate that 78% of RSV-associated deaths occur among people aged >65 years, 6 suggesting that age is a risk factor for mortality. 5 However, the associations between risk factors such as older age, obesity, and heart, lung, and neurological comorbid conditions with severe clinical outcomes during hospitalization are better understood for influenza than for RSV infection. 4
Because the RSV season typically coincides with seasonal influenza, generally from October to May, 7 and both viruses can cause lower respiratory tract infections and pneumonia, it can be difficult to ascertain the relative contribution of RSV without comprehensive screening and testing for both viruses. 8 We performed this nested retrospective study using data derived from a prospective surveillance study for RSV-related hospitalizations in which patients with symptoms of acute respiratory illness (ARI) were routinely tested for respiratory viruses. We identified hospitalized adults with laboratory-confirmed RSV infection who had severe clinical outcomes, defined as intensive care unit (ICU) admission, mechanical ventilation, and/or in-hospital death. We compared the demographic characteristics, clinical factors, and living situation at admission of patients with and without severe clinical outcomes. We hypothesized that even among patients with similar comorbidities, baseline living situation at admission could serve as an indicator of a patient’s underlying health status and predict severe outcomes. Finally, we explored the effect of RSV-associated hospitalizations on the level of care required by surviving patients by assessing changes in their living situations from hospital admission to discharge.
Methods
Study Design, Sites, and Participants
From October 2017 through April 2018 (Year 1) and from October 2018 through April 2019 (Year 2), we performed prospective surveillance among hospitalized adults aged ≥18 who had laboratory-confirmed RSV infection. Surveillance occurred at 3 academically affiliated hospitals from the same multicampus institution. The hospitals are in northern Manhattan and included a ~750-bed tertiary care hospital for adult patients, a ~200-bed community hospital for adult patients, and a ~250-bed children’s hospital. The Columbia University Irving Medical Center Institutional Review Board approved this study with a waiver of documentation of consent.
As per the standard of care in these hospitals, patients with ARI and anticipated hospitalization are tested for viral respiratory pathogens to inform treatment (eg, the administration of oseltamivir for influenza) and decision-making on the potential need for implementing transmission precautions in the hospital (eg, contact precautions for RSV). These tests are most often performed in the emergency department during evaluation for hospitalization. Nasopharyngeal swabs are processed in the clinical microbiology laboratories affiliated with these hospitals using a multiplex reverse transcription polymerase chain reaction assay (FilmArray Respiratory Panel V1.7, BioFire Diagnostics, Inc) that includes RSV; this assay was used throughout the study period. We identified potential patients during the prospective surveillance study by monitoring admissions from the emergency department (Monday through Friday) and by reviewing the Department of Infection Prevention and Control’s internal database of epidemiologically important pathogens in hospitalized patients. To detect patients missed by active surveillance, when the surveillance seasons ended, we queried the electronic medical record (EMR) for all positive RSV test results in hospitalized adults during the study period.
Eligible patients for the current study were adults aged ≥18 who had laboratory-confirmed RSV infection, had ≥2 symptoms consistent with ARI (ie, presence of fever [≥37.8 °C] or feeling feverish, new or worsening cough, new or worsening sputum production, new or worsening dyspnea, sore throat, runny nose/nasal congestion, and/or body aches) documented in the EMR, were hospitalized for at least 24 hours, and lived in New York City as per their residential zip code.
Study Outcomes and Risk Factors Associated With Severe Clinical Outcomes
The primary outcome of interest was the proportion of patients with severe clinical outcomes, defined as being admitted to an ICU, receiving mechanical ventilation, and/or dying during the RSV-associated hospitalization. We used the Centers for Disease Control and Prevention National Notifiable Diseases Surveillance System case definition for RSV-related death. 2
Potential factors associated with severe clinical outcomes included demographic characteristics, comorbid conditions, study hospital, study year, and living situation at the time of admission as described in the EMR. We categorized the baseline living situations of patients by implied level of functional independence. Level 1 included patients living without assistance in the community; Level 2 included those living in the community with the assistance of friends, family, and/or a home health aide; and Level 3 included those living in a facility such as assisted living, a skilled nursing or long-term care facility, rehabilitation facility, or hospice. We excluded from analysis patients who reported being homeless at admission or who were transferred from another acute care facility.
Among the patients who survived and were discharged from the hospital, we explored changes in living situation from admission to discharge that implied the need for a higher level of care at discharge than at admission. For example, living with assistance on admission (Level 2) and discharge to a skilled nursing home (Level 3) represented the need for a higher level of care. We excluded from analysis patients transferred to another acute care facility.
Data Collection and Analysis
We extracted data for outcomes and factors associated with severe clinical outcomes from the EMR and entered these data into standardized electronic case report forms maintained on a secure server. We also collected data on living situation at admission and at discharge from the EMR; these data were generally in the form of notes by social workers.
We used the χ2 test of proportions to determine differences in the distribution of severe clinical outcomes by month and by surveillance year. We used the Fisher exact test to determine differences when cell sizes were ≤5. We used odds ratios (ORs) and 95% CIs to estimate the odds of severe clinical outcomes by demographic characteristics, comorbid conditions, and living situation. We built a multivariate logistic regression model using bidirectional elimination to evaluate characteristics associated with severe clinical outcomes. Variables included in the model were hypothesized to be associated with severe illness, including older age; obesity; heart, lung, and neurologic comorbidities; and any factors significantly associated with severe clinical outcomes in the bivariate analysis. We selected the final model by minimizing the Akaike information criterion and maximizing the coefficient of determination (r 2).
We explored whether severe clinical outcomes affected the level of care needed at discharge, using living situation as a proxy for level of care. To do so, we compared the pre-admission and discharge living situation for each surviving patient. We categorized changes in the patient’s living situation as increased (eg, living independently before hospitalization and discharged to a nursing home), decreased (eg, living in the community with family before hospitalization and discharged to living independently), or unchanged. We used ORs and 95% CIs to estimate the odds of a change in living situation among patients with and without severe clinical outcomes.
We considered a P value < .05 to be significant. We used RStudio version 1.2.5001 (RStudio, PBC) packages and procedures for data analysis.
Results
Study Population
During the 2-year study period, 403 patients fulfilled the eligibility criteria for RSV-associated hospitalization. The median age of patients was 69.0 (interquartile range [IQR], 57.2-82.1); 29.5% of patients were aged ≥80, and 58.3% were female (Table 1). The most common comorbid conditions were cardiac conditions (47.6%), respiratory conditions (45.9%), and diabetes (41.4%). Only 4.7% of patients had no comorbid conditions. Fewer than half (41.9%) were living independently at admission.
Table 1.
Comparison of demographic and clinical factors among adults hospitalized with laboratory-confirmed respiratory syncytial virus with and without severe clinical outcomes, including intensive care unit admission, mechanical ventilation, and/or death, October 2017 through April 2018 and October 2018 through April 2019, New York City a
| Factor | All (N = 403) | Severe clinical outcomes | ||
|---|---|---|---|---|
| No (n = 326) | Yes (n = 77) | Odds ratio (95% CI) | ||
| Age, median (IQR), y | 69.0 (57.2-82.1) | 69.3 (56.4-81.9) | 68.4 (57.9-82.3) | — |
| Age group, y | ||||
| 18-49 | 62 (15.4) | 47 (14.4) | 15 (19.5) | 1.44 (0.75-2.73) |
| 50-64 | 110 (27.3) | 96 (29.4) | 14 (18.2) | 0.53 (0.28-1.00) |
| 65-79 | 112 (27.8) | 88 (27.0) | 24 (31.2) | 1.22 (0.71-2.10) |
| ≥80 | 119 (29.5) | 95 (29.1) | 24 (31.2) | 1.10 (0.64-1.89) |
| Female sex | 235 (58.3) | 201 (61.7) | 44 (57.1) | 0.83 (0.50-1.37) |
| Race | ||||
| White | 106 (26.3) | 89 (27.3) | 17 (22.1) | 0.75 (0.42-1.36) |
| Black or African American | 80 (19.9) | 61 (18.7) | 19 (24.7) | 1.42 (0.79-2.56) |
| Asian | 5 (1.2) | 5 (1.5) | 0 | 0.38 (0.02-6.89) b |
| Other c | 8 (2.0) | 8 (2.5) | 0 | 0.24 (0.01-4.23) b |
| Unknown | 204 (50.6) | 163 (50.0) | 41 (53.2) | 1.14 (0.69-1.87) |
| Ethnicity | ||||
| Hispanic | 129 (32.0) | 110 (33.7) | 19 (24.7) | 0.64 (0.37-1.13) |
| Non-Hispanic | 73 (18.1) | 57 (17.5) | 16 (20.8) | 1.24 (0.67-2.30) |
| Unknown | 201 (49.9) | 159 (48.8) | 42 (54.5) | 1.26 (0.77-2.07) |
| Comorbid conditions | ||||
| Any cardiac d | 192 (47.6) | 159 (48.8) | 33 (42.9) | 0.79 (0.48-1.30) |
| Congestive heart failure | 111 (27.5) | 88 (27.0) | 23 (30.0) | 1.15 (0.67-1.99) |
| Any respiratory e | 185 (45.9) | 147 (45.1) | 38 (49.4) | 1.19 (0.72-1.95) |
| Chronic obstructive pulmonary disease | 91 (22.6) | 67 (20.6) | 24 (31.2) | 1.75 (1.01-3.04) |
| Asthma | 103 (25.6) | 82 (25.2) | 21 (27.3) | 1.12 (0.64-1.95) |
| Diabetes | 167 (41.4) | 133 (40.8) | 34 (44.2) | 1.15 (0.69-1.89) |
| Any neurologic f | 113 (28.0) | 93 (28.5) | 20 (26.0) | 0.88 (0.50-1.54) |
| Obesity | 107 (26.6) | 91 (27.9) | 16 (20.8) | 0.68 (0.37-1.24) |
| Immunosuppressive conditions g | 101 (25.1) | 83 (25.5) | 18 (23.4) | 0.89 (0.50-1.60) |
| None | 19 (4.7) | 14 (4.3) | 5 (6.5) | 1.55 (0.54-4.44) |
| Hospital | ||||
| A | 289 (71.7) | 235 (72.1) | 54 (70.1) | 0.91 (0.53-1.57) |
| B | 107 (26.6) | 85 (26.1) | 22 (28.6) | 1.13 (0.56-1.97) |
| C | 7 (1.7) | 6 (1.8) | 1 (1.3) | 0.70 (0.08-5.92) b |
| Study year | ||||
| Year 1 (October 2017 through April 2018) | 184 (45.7) | 151 (46.3) | 33 (42.9) | 0.87 (0.53-1.43) |
| Year 2 (October 2018 through April 2019) | 219 (54.3) | 175 (53.7) | 44 (57.1) | 1.15 (0.70-1.90) |
| Living situation at admission h | ||||
| Level 1 | 169 (41.9) | 141 (43.3) | 28 (36.4) | 0.75 (0.45-1.25) |
| Level 2 | 193 (47.9) | 164 (50.3) | 29 (37.7) | 0.60 (0.36-0.99) |
| Level 3 | 39 (9.7) | 21 (6.4) | 18 (23.4) | 4.43 (2.23-8.82) |
| Excluded i | 2 (0.5) | 0 | 2 (2.6) | — |
aData were extracted by the research team from the electronic medical records of 3 academically affiliated hospitals in northern Manhattan. All values are number (percentage) unless otherwise indicated; percentages may not add to 100 because of rounding.
bFisher exact test used when cell size ≤5; otherwise, χ2 test of proportions used.
c“Other” includes Native Hawaiian/Other Pacific Islander or American Indian/Alaska Native.
dAny cardiac condition includes congestive heart failure, coronary artery disease, and/or hypertension.
eAny respiratory condition includes asthma, chronic obstructive pulmonary disease, sleep apnea, cystic fibrosis, interstitial lung disease, bronchiectasis, pulmonary fibrosis, and/or pulmonary hypertension.
fAny neurologic condition includes seizure disorder, cerebral palsy, dementia, stroke, and/or Guillain-Barre syndrome.
gImmunosuppressive conditions include HIV infection, transplant recipient, and/or chemotherapy for cancer within past 6 months.
hHypothesized as an indicator of a patient’s underlying health status. Level 1, independent; Level 2, assistance of family, friends, or home health aide; Level 3, assisted living, skilled nursing or long-term care facility, rehabilitation facility, or hospice.
iTwo patients were excluded from analysis; one was homeless at admission, and one was transferred from another hospital.
Patients With Severe Clinical Outcomes
Overall, 77 (19.1%) of the 403 patients had severe clinical outcomes; 66 (16.4%) were admitted to an ICU, 50 (12.4%) received mechanical ventilation, and 27 (6.7%) died during hospitalization. The median length of ICU stay was 7 days (IQR, 3.5-12.0), and the median duration of mechanical ventilation was 3.0 days (IQR, 2.0-9.5).
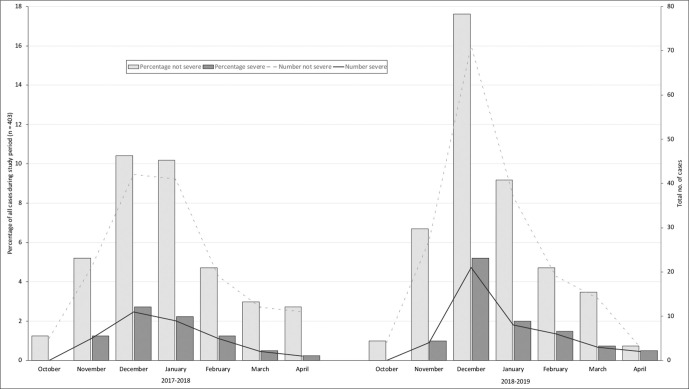
For each month of admission, the number of patients hospitalized with laboratory-confirmed RSV infection ranged from 4 to 92, and the number of patients with severe clinical outcomes ranged from 0 to 21 (Figure). In both surveillance years, the number of patients hospitalized with RSV infection was highest in December and January. The proportion of patients with severe clinical outcomes each year and each month was similar.
Figure.
Adults hospitalized with laboratory-confirmed respiratory syncytial virus infection, with and without severe clinical outcomes (intensive care unit admission, mechanical ventilation, and/or death), by admission month and year, October 2017 through April 2018 and October 2018 through April 2019, New York City. Data were extracted by the research team from the electronic medical records of 3 academically affiliated hospitals in northern Manhattan.
Factors Associated With Severe Clinical Outcomes
In the bivariate analysis of factors associated with severe clinical outcomes, neither age nor any of the comorbid conditions assessed were associated with increased odds of having severe clinical outcomes (Table 1). Patients who resided in assisted living, skilled nursing, long-term care, rehabilitation, or hospice facilities at admission (Level 3) had a 4.43 times higher likelihood of severe clinical outcomes compared with patients who had other living situations at admission.
In the final logistic regression model, which controlled for age, sex, and comorbidities, patients with a Level 3 living situation at admission had 6.64 times higher odds of severe clinical illness compared with patients admitted from other living situations (Table 2).
Table 2.
Regression analysis for factors associated with severe clinical outcomes, including intensive care unit admission, mechanical ventilation, and/or death, in adults hospitalized with laboratory-confirmed respiratory syncytial virus infection, October 2017 through April 2018 and October 2018 through April 2019, New York City a
| Variable | Estimated odds ratio (95% CI) | β | P value |
|---|---|---|---|
| Intercept b | 0.15 (0.07-0.31) | −1.92 | <.001 |
| Age, y | |||
| 18-49 | 1.73 (0.75-4.00) | 0.55 | .20 |
| 50-64 | 1 [Reference] | ||
| 65-79 | 1.76 (0.86-3.61) | 0.57 | .12 |
| ≥80 | 1.25 (0.58-2.70) | 0.23 | .56 |
| Male sex | 1.20 (0.70-2.07) | 0.18 | .51 |
| Comorbid conditions | |||
| Respiratory condition | 1.36 (0.80-2.33) | 0.31 | .26 |
| Cardiac condition | 0.73 (0.42-1.27) | −0.31 | .27 |
| Immunosuppressive condition | 0.89 (0.48-1.68) | −0.11 | .74 |
| Neurologic condition | 0.60 (0.30-1.18) | −0.51 | .14 |
| Living in a facility at admission c | 6.64 (2.92-15.08) | 1.89 | <.001 |
aData were extracted by the research team from the electronic medical records of 3 academically affiliated hospitals in northern Manhattan.
bThe final model is as shown: Logit(sRSV) = intercept + β1(Age 18-49) + β2(Age 65-79) + β3(Age 80+) + β4(male) + β5(Lung Condition) + β6(Cardio Condition) + β7(Immunosuppressive Condition) + β8(Neurological Condition) + β9(living in a facility at admission). Final correlation coefficient (r 2) = 0.098; Akaike information criterion = 384.47.
cIncludes assisted living, skilled nursing or long-term care facility, rehabilitation facility, or hospice.
Changes in Living Situation From Admission to Discharge
Of the 372 surviving patients who were discharged, 56 (15.1%) required a higher level of care at discharge than at admission (Table 3). Patients who returned to living independently in the community (Level 1, n = 127) or returned to living in the community with assistance (Level 2, n = 156) were less likely to have had severe clinical outcomes than to not have them (OR = 0.48 and 0.33, respectively). Patients who lived in a facility and returned to a facility (Level 3, n = 30) were 4.92 times more likely to have had severe clinical outcomes than to not have them. Severe outcomes were significantly more likely to have occurred (than to not have occurred) among patients whose level of care increased at discharge, especially among patients whose care increased from Level 1 to Level 3 (OR = 5.41) or from Level 2 to Level 3 (OR = 3.17).
Table 3.
Changes in living situation from admission to discharge among adults hospitalized with laboratory-confirmed respiratory syncytial virus infection, October 2017 through April 2018 and October 2018 through April 2019, New York City a
| Change from admission to discharge b | Total, no. (%) (n = 372) c | Severe clinical outcomes | |||
|---|---|---|---|---|---|
| No, no. (%) (n = 325) | Yes, no. (%) (n = 47) | Odds ratio (95% CI) | P value | ||
| Unchanged: Level 1 | 127 (34.1) | 117 (36.0) | 10 (21.3) | 0.48 (0.23-1.00) | .05 |
| Unchanged: Level 2 | 156 (41.9) | 146 (44.9) | 10 (21.3) | 0.33 (0.16-0.69) | .003 |
| Unchanged: Level 3 | 30 (8.1) | 19 (5.8) | 11 (23.4) | 4.92 (2.17-11.16) | <.001 |
| Increased: Level 1 to Level 2 | 20 (5.4) | 17 (5.2) | 3 (6.4) | 1.24 (0.35-4.39) | .73 |
| Increased: Level 1 to Level 3 | 12 (3.2) | 7 (2.2) | 5 (10.6) | 5.41 (1.64-17.81) | .005 |
| Increased: Level 2 to Level 3 | 24 (6.5) | 17 (5.2) | 7 (14.9) | 3.17 (1.24-8.12) | .02 |
| Any increase in level of care | 56 (15.1) | 41 (12.6) | 15 (31.9) | 3.25 (1.62-6.51) | .001 |
| Any decrease in level of care | 3 (0.8) | 2 (0.6) | 1 (2.1) | 3.51 (0.31-39.49) | .33 |
aData were extracted by the research team from the electronic medical records of 3 academically affiliated hospitals in northern Manhattan.
bLevel 1, independent; Level 2, assistance of family, friends, or home health aide; Level 3, assisted living, skilled nursing or long-term care facility, rehabilitation facility, or hospice.
cAnalysis included 372 surviving patients. Excluded patients included 1 patient who was homeless at admission, 3 patients discharged to another acute care facility, and 27 patients who died.
Discussion
We found that 19.1% of patients with RSV-associated hospitalization had severe clinical outcomes, including 6.7% who died during hospitalization. The proportion of deaths associated with RSV infection is consistent with previous studies of similar populations ranging from 5.6% 4 to 7.6%. 1 Previous studies compared morbidity and mortality among adult patients with RSV-related and influenza-related hospitalizations. 1,9 Adults hospitalized with RSV or influenza in Rochester, New York, had similar lengths of stay, rates of pneumonia, need for ICU care, and mortality. 1 In Hong Kong, compared with hospitalized adults with influenza, hospitalized adults with RSV infection had similar 30- and 60-day mortality but significantly higher rates of mechanical ventilation (11.1% vs 6.2%; P = .003) and higher rates of extended care in subacute hospitals after discharge (25.2% vs 19.7%; P = .03). 10 Analysis of Medicaid data in Tennessee found that RSV infection and influenza accounted for a similar estimated number of hospitalizations. 11
Nearly half of the patients in our study who were admitted from assisted living, a skilled nursing or long-term care facility, rehabilitation facility, or hospice had severe clinical outcomes. Although age and selected comorbidities were not associated with severe clinical outcomes, patients living in a facility before admission had 4.43 times the odds of severe clinical outcomes compared with patients living independently or with assistance in the community. Similarly, when we controlled for age and comorbidities, patients who lived in a facility had 6.64 times the odds of severe clinical outcomes compared with patients living independently or with assistance. Another study reported increased mortality associated with RSV infections among patients admitted from long-term care facilities (33% mortality) compared with patients admitted from the community (3% mortality). 1 These findings suggest that living situation may be a proxy measure of frailty and, in turn, a risk for severe clinical outcomes. 12 Chronic disease, multiple comorbidities, and functional disability are associated with frailty, and frailty can contribute to older adults’ vulnerability to adverse outcomes from influenza. 13,14 Other studies showed that people in assisted living have higher rates of frailty compared with people living independently, 15 although frailty can be measured in different ways. Future interventions for RSV, such as vaccines or antiviral therapy, should target this population at high risk for RSV.
Fifteen percent of adults who survived hospitalization required a higher level of care at discharge than at admission. Overall, 36 (9.7%) patients went from living in the community to living in a facility. Other researchers have reported that 5% of patients hospitalized with RSV infection required a higher level of care at discharge than at admission 1 and that hospitalization is an independent risk factor for declines in functional status among older adults that can be associated with a need for a higher level of care. 16 The yearly median cost of assisted living was estimated to be $48 612 in 2019. 17 Thus, studies of health care costs associated with RSV hospitalizations should include costs incurred after discharge, including the need for a higher level of care, ambulatory health care, 18 and management of worsening comorbidities associated with RSV infection. 19,20
Limitations
This study had several limitations. First, we conducted the study in an urban, academically affiliated medical center; as such, our findings may not be generalizable to other populations. Second, although patients had laboratory-confirmed RSV infection and at least 2 symptoms of ARI, severe clinical outcomes may have been secondary to exacerbations of their comorbid conditions. Third, some patients admitted with an ARI may not have been tested for RSV by treating health care providers. Fourth, we assessed comorbidities as reported in the admission notes, but we did not verify comorbidities by relevant medications or treatment, nor did we account for the severity of these comorbid conditions or their management during hospitalization. Fifth, living situation was self-reported or reported by a family member; we did not verify living situation by other means. Lastly, living situation might not be determined by health-related issues; for example, patients could be living with a family member because of financial constraints or to assist with child care.
Conclusions
Adults hospitalized with laboratory-confirmed RSV infection can have severe clinical outcomes, including the need for ICU care, mechanical ventilation, and/or death. Our data support the development of vaccines and antiviral agents for RSV. Living in a facility at admission was a risk factor for severe clinical outcomes and could be a proxy for frailty, rather than an independent risk factor. Because therapies and vaccines for the prevention of RSV infection in adults are lacking, prevention strategies are needed. Our data support the development of prevention strategies for RSV infection in older populations, especially older adults living in residential living facilities. Furthermore, older adults may have a diminished capacity to respond to vaccines; as such, prevention of RSV transmission in congregate settings is highly desirable and feasible. Infection prevention strategies combined with vaccination could reduce morbidity, mortality, and health care costs. Future studies should further assess the association of living situation and adverse clinical outcomes and the association of RSV-related hospitalizations and longer-term deterioration in functional status.
Footnotes
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: M.P. and L.F. are employees of Merck Sharp & Dohme Corp, a subsidiary of Merck & Co, Inc, Kenilworth, NJ, USA. L.S. has received research funding from and served on an advisory board for Merck Sharp & Dohme Corp.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a research grant from Merck Sharp & Dohme Corp.
ORCID iD
Lisa Saiman, MD, MPH https://orcid.org/0000-0002-7231-8451
References
- 1. Falsey AR., Hennessey PA., Formica MA., Cox C., Walsh EE. Respiratory syncytial virus infection in elderly and high-risk adults. N Engl J Med. 2005;352(17):1749-1759. 10.1056/NEJMoa043951 [DOI] [PubMed] [Google Scholar]
- 2. Centers for Disease Control and Prevention . Respiratory syncytial virus–associated mortality (RSV-associated mortality) 2019 case definition. Accessed April 27, 2020. https://wwwn.cdc.gov/nndss/conditions/respiratory-syncytial-virus-associated-mortality/case-definition/2019
- 3. Centers for Disease Control and Prevention . RSV in older adults and adults with chronic medical conditions. Accessed April 26, 2020. https://www.cdc.gov/rsv/high-risk/older-adults.html
- 4. Ackerson B., Tseng HF., Sy LS. et al. Severe morbidity and mortality associated with respiratory syncytial virus versus influenza infection in hospitalized older adults. Clin Infect Dis. 2019;69(2):197-203. 10.1093/cid/ciy991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nam HH., Ison MG. Respiratory syncytial virus infection in adults. BMJ. 2019;366:15021. 10.1136/bmj.l5021 [DOI] [PubMed] [Google Scholar]
- 6. Thompson WW., Shay DK., Weintraub E. et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179-186. 10.1001/jama.289.2.179 [DOI] [PubMed] [Google Scholar]
- 7. Rose EB., Wheatley A., Langley G., Gerber S., Haynes A. Respiratory syncytial virus seasonality—United States, 2014-2017. MMWR Morb Mortal Wkly Rep. 2018;67(2):71-76. 10.15585/mmwr.mm6702a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Piedimonte G., Perez MK. Respiratory syncytial virus infection and bronchiolitis. Pediatr Rev. 2014;35(12):519-530. 10.1542/pir.35-12-519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dasgupta S., Das S., Chawan NS., Hazra A. Nosocomial infections in the intensive care unit: incidence, risk factors, outcome and associated pathogens in a public tertiary teaching hospital of Eastern India. Indian J Crit Care Med. 2015;19(1):14-20. 10.4103/0972-5229.148633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lee N., Lui GCY., Wong KT. et al. High morbidity and mortality in adults hospitalized for respiratory syncytial virus infections. Clin Infect Dis. 2013;57(8):1069-1077. 10.1093/cid/cit471 [DOI] [PubMed] [Google Scholar]
- 11. Griffin MR., Coffey CS., Neuzil KM., Mitchel EF Jr., Wright PF., Edwards KM. Winter viruses: influenza- and respiratory syncytial virus–related morbidity in chronic lung disease. Arch Intern Med. 2002;162(11):1229-1236. 10.1001/archinte.162.11.1229 [DOI] [PubMed] [Google Scholar]
- 12. Chen X., Mao G., Leng SX. Frailty syndrome: an overview. Clin Interv Aging. 2014;9:433-441. 10.2147/CIA.S45300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. McElhaney JE., Zhou X., Talbot HK. et al. The unmet need in the elderly: how immunosenescence, CMV infection, co-morbidities and frailty are a challenge for the development of more effective influenza vaccines. Vaccine. 2012;30(12):2060-2067. 10.1016/j.vaccine.2012.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lees C., Godin J., McElhaney JE. et al. Frailty hinders recovery from influenza and acute respiratory illness in older adults. J Infect Dis. 2020;222(3):428-437. 10.1093/infdis/jiaa092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lutomski JE., Baars MAE., Boter H. et al. Frailty, disability and multi-morbidity: the relationship with quality of life and healthcare costs in elderly people. Ned Tijdschr Geneeskd. 2014;158: [PubMed] [Google Scholar]
- 16. Boyd CM., Landefeld CS., Counsell SR. et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56(12):2171-2179. 10.1111/j.1532-5415.2008.02023.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Genworth . Cost of care survey. Accessed June 25, 2020. https://www.genworth.com/aging-and-you/finances/cost-of-care.html
- 18. Amand C., Tong S., Kieffer A., Kyaw MH. Healthcare resource use and economic burden attributable to respiratory syncytial virus in the United States: a claims database analysis. BMC Health Serv Res. 2018;18(1): 10.1186/s12913-018-3066-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Openshaw PJ. Antiviral immune responses and lung inflammation after respiratory syncytial virus infection. Proc Am Thorac Soc. 2005;2(2):121-125. 10.1513/pats.200504-032AW [DOI] [PubMed] [Google Scholar]
- 20. Wilkinson TMA., Donaldson GC., Johnston SL., Openshaw PJM., Wedzicha JA. Respiratory syncytial virus, airway inflammation, and FEV1 decline in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173(8):871-876. 10.1164/rccm.200509-1489OC [DOI] [PubMed] [Google Scholar]